What is escitalopram
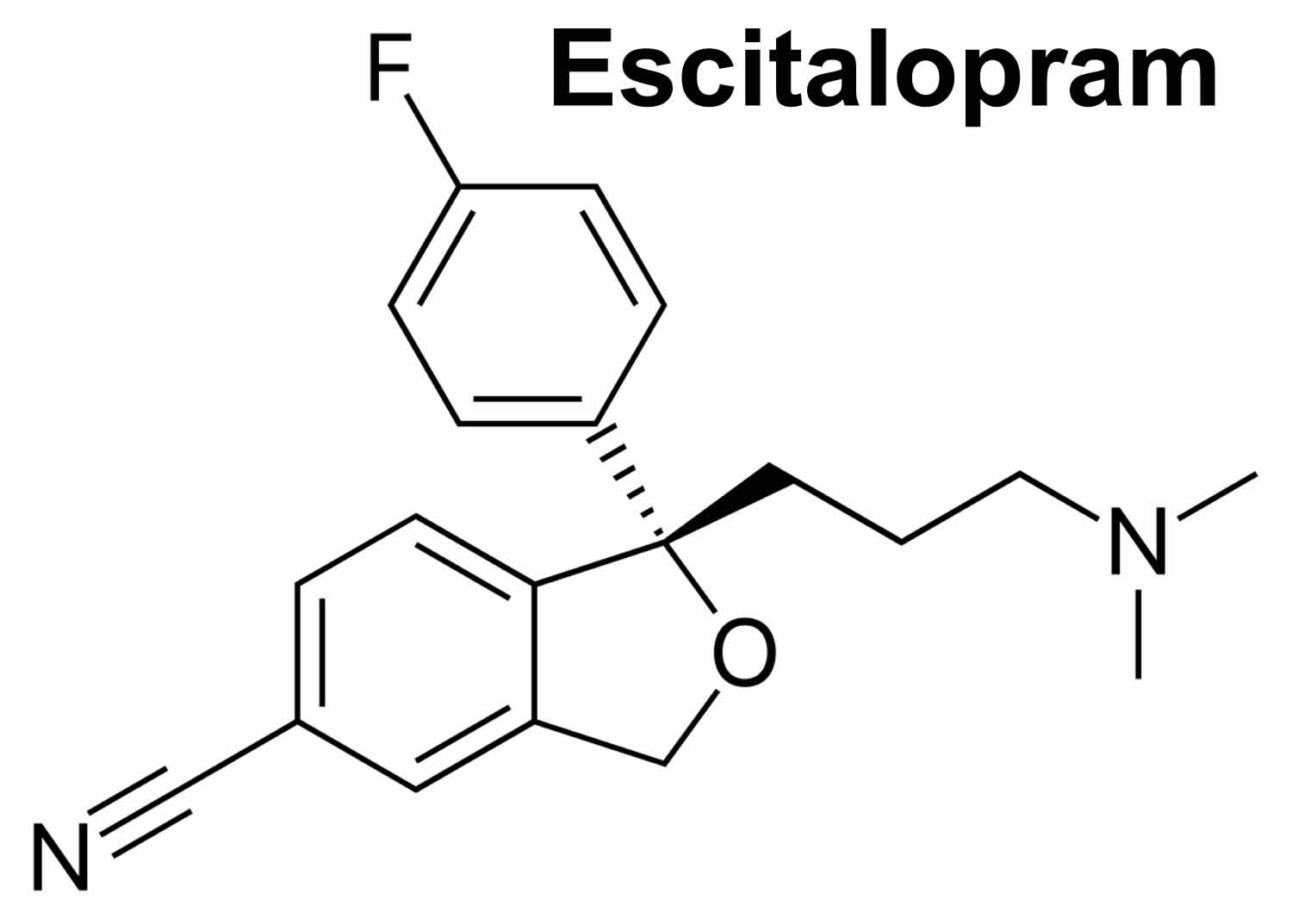
Escitalopram is a medication used to treat depression and generalized anxiety disorder (GAD). Escitalopram belongs to the class of antidepressants known as selective serotonin reuptake inhibitors or SSRIs. Escitalopram is the S-isomer of the antidepressant, citalopram, which is metabolized to 2 metabolites, each having antidepressant activity considered to be about 13% that of citalopram 1. The exact way escitalopram works for the treatment of depression or anxiety is not known but is thought to be related an increase in serotonin, a chemical transmitter, in nerve synapses (the spaces between nerves) in the brain. Serotonin is involved in the regulation of mood, appetite, and sleep. Escitalopram is available on prescription. It comes as tablets and as liquid drops that you put in a drink.
How and when to take escitalopram
- Take escitalopram once a day. You can take it with or without food.
- You can take escitalopram at any time of day, as long as you stick to the same time every day. If you have trouble sleeping, it’s best to take it in the morning.
Key facts
- It usually takes 4 to 6 weeks for escitalopram to work.
- Side effects such as nausea and headache are common. They are usually mild and go away after a couple of weeks.
- Escitalopram can cause withdrawal symptoms so don’t stop taking it without talking to your doctor.
- Escitalopram is called by the brand name Lexapro or Cipralex.
A small number of children, teenagers, and young adults (up to 24 years of age) who took antidepressants (‘mood elevators’) such as escitalopram during clinical studies became suicidal (thinking about harming or killing oneself or planning or trying to do so). Children, teenagers, and young adults who take antidepressants to treat depression or other mental illnesses may be more likely to become suicidal than children, teenagers, and young adults who do not take antidepressants to treat these conditions. However, experts are not sure about how great this risk is and how much it should be considered in deciding whether a child or teenager should take an antidepressant. Children younger than 12 years of age should not normally take escitalopram, but in some cases, a doctor may decide that escitalopram is the best medication to treat a child’s condition.
You should know that your mental health may change in unexpected ways when you take escitalopram or other antidepressants even if you are an adult over 24 years of age. You may become suicidal, especially at the beginning of your treatment and any time that your dose is increased or decreased. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: new or worsening depression; thinking about harming or killing yourself, or planning or trying to do so; extreme worry; agitation; panic attacks; difficulty falling asleep or staying asleep; aggressive behavior; irritability; acting without thinking; severe restlessness; and frenzied abnormal excitement. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Your healthcare provider will want to see you often while you are taking escitalopram, especially at the beginning of your treatment. Be sure to keep all appointments for office visits with your doctor.
The doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with escitalopram. Read the information carefully and ask your doctor or pharmacist if you have any questions. You also can obtain the Medication Guide from the FDA website: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm.
No matter your age, before you take an antidepressant, you, your parent, or your caregiver should talk to your doctor about the risks and benefits of treating your condition with an antidepressant or with other treatments. You should also talk about the risks and benefits of not treating your condition. You should know that having depression or another mental illness greatly increases the risk that you will become suicidal. This risk is higher if you or anyone in your family has or has ever had bipolar disorder (mood that changes from depressed to abnormally excited) or mania (frenzied, abnormally excited mood) or has thought about or attempted suicide. Talk to your doctor about your condition, symptoms, and personal and family medical history. You and your doctor will decide what type of treatment is right for you.
WARNINGS
Increased Risk of Suicidal Thoughts and Behavior in Children and Adolescents with Depression or Other Mood Disorders.
Escitalopram, like other antidepressants, has been associated with an increased risk of suicidal thoughts and behavior in children, adolescents, and adults under the age of 24. Beyond the age of 24 no increase in risk was noted, and over the age of 65 there was a reduction in risk. Monitor behavior.
Serotonin Syndrome
Serotonin syndrome is the name given to a potentially life-threatening collection of symptoms that occur if serotonin levels in the nerve synapses
Withdrawal Symptoms Following Abrupt Discontinuation
Some people have experienced withdrawal symptoms when they have stopped taking escitalopram suddenly. Symptoms have included a low mood, agitation, confusion, dizziness, electric shock sensations or a feeling of burning or prickling on their skin, insomnia, and lethargy. Do not stop taking escitalopram suddenly, unless your doctor tells you to. When it comes time to discontinue escitalopram, your doctor will tell you how to do it slowly.
Risk of Very Low Sodium Levels (Hyponatremia)
Escitalopram may cause low sodium levels (hyponatremia) because of continued and inappropriate secretion of a hormone from the pituitary gland that is responsible for concentrating urine. This is known as the syndrome of inappropriate antidiuretic hormone secretion (SIADH), and it reverses when escitalopram is discontinued. The risk is higher in seniors and in people who are dehydrated or taking diuretics. Symptoms include a headache, confusion, unsteadiness resulting in falls, and weakness; and in severe cases, it may cause death. Seek urgent medical help if you develop symptoms.
Increased Risk of Bleeding
Escitalopram, like other selective serotonin reuptake inhibitors (SSRIs), has been associated with an increased risk of bleeding events, particularly gastrointestinal (related to the stomach and intestine) bleeding. The risk is increased in people who also aspirin, nonsteroidal anti-inflammatory drugs, warfarin, or other anticoagulants. Talk to your doctor if you notice it takes longer for you to stop bleeding from a cut or if you notice blood in your stools (feces).
When will I feel better?
You may not notice much improvement in your symptoms for a week or 2 until escitalopram begins to take effect. It usually takes between 4 and 6 weeks before you feel the full benefits.
Don’t stop taking escitalopram after a week or two just because you feel it is not helping your symptoms. Give escitalopram at least 6 weeks to work.
What is the difference between escitalopram and citalopram?
Escitalopram and citalopram are both medicines used to treat depression. They may sound similar but they’re different medicines.
Differences include:
- escitalopram doses are half that of citalopram
- the type and frequency of side effects you may get are different with each medicine
- escitalopram can be used for a wider range of health problems than citalopram
How will escitalopram make me feel?
Antidepressants like escitalopram help to jump start your mood so you feel better. You may notice that you sleep better and get on with people more easily because you’re less anxious. You will hopefully take little things that used to worry you in your stride.
Escitalopram won’t change your personality or make you feel euphorically happy. It will simply help you feel like yourself again.
Don’t expect to feel better overnight though. Some people feel worse during the first few weeks of treatment before they begin to feel better.
Is escitalopram better than other antidepressants?
Escitalopram isn’t any better or worse than other antidepressants. However, sometimes people respond better to one antidepressant than to another. Talk to your doctor if you aren’t feeling any better after 6 weeks.
Are there other treatments that will help?
Antidepressants, including escitalopram, are just one of several approaches to treating depression. Other potential treatments include:
- talking therapy (such as cognitive behavioral therapy or CBT)
- exercise programmes
- help to get a good night’s sleep
Choosing a treatment that’s most suitable for you depends on how long you have had depression, your symptoms, whether you have had any previous bouts of depression, whether previous treatment has worked, how likely you are to stick with your treatment, the potential side effects and your preferences and priorities.
How long will I take escitalopram for?
Once you’re feeling better it’s likely that you will continue to take escitalopram for several more months to prevent the symptoms returning.
You’ll need to discuss with your doctor the pros and cons of continuing to take escitalopram for longer than a few months. The decision will depend on the type and severity of your symptoms, whether it’s a one-off problem or one that keeps coming back, how well escitalopram works for you and whether you have had any bad side effects.
What will happen when I stop taking escitalopram?
Some people get side effects when they stop taking escitalopram, especially if they stop taking it suddenly.
To help prevent this, your doctor might recommend reducing your dose of escitalopram gradually over several weeks.
Don’t stop taking escitalopram, suddenly, or without talking to your doctor.
Is it safe to take escitalopram for a long time?
Escitalopram is safe to take for a long time. There don’t seem to be any lasting harmful effects from taking it for many months and years.
Will I gain or lose weight?
Escitalopram can make you feel less hungry, so you may lose weight when you first start taking it.
Later on, you may gain a little weight as your appetite returns.
If you start to have problems with your weight while taking escitalopram, talk to your doctor or pharmacist.
Can I drive or ride a bike?
Some people find they can’t concentrate properly while they’re taking escitalopram. It might be best to stop driving and cycling for the first few days of treatment until you know how this medicine makes you feel.
Will escitalopram affect my sex life?
The good effects of escitalopram may, after a while, improve your sex life as your mood lifts and you become interested in life and relationships again.
Some of the possible negative effects include:
- men getting painful erections, problems with getting an erection and problems with ejaculating
- women having some vaginal bleeding and might not reach orgasm the same way as before
- a lower sex drive
Sexual side effects should pass after the first couple of weeks. If they don’t, and this is a problem for you, go back to your doctor to see if there’s another antidepressant you can try.
Will escitalopram affect my contraception?
For women, escitalopram will not affect contraceptive pills or the morning after pill.
Is there any food or drink I need to avoid?
You can eat and drink normally while taking escitalopram.
Can I drink alcohol with escitalopram?
You can drink alcohol while taking escitalopram but it may make you feel sleepy. It might be best to stop drinking alcohol until you see how the medicine makes you feel.
Will recreational drugs affect escitalopram?
The sleep-inducing effects of cannabis can add to those of escitalopram, especially in people who have just started taking it. Cannabis with escitalopram can also give you a fast heartbeat.
Methadone can increase the risk of side effects in people taking escitalopram.
It can be potentially dangerous to take escitalopram with:
- stimulants like MDMA (ecstasy) or cocaine
- hallucinogens like LSD
- novel psychoactive substances (which used to be known as legal highs) like mephedrone
Escitalopram hasn’t been properly tested with recreational drugs. Talk to your doctor if you think you might use recreational drugs while taking escitalopram.
How should escitalopram be used?
Escitalopram comes as a tablet and a solution (liquid) to take by mouth. It is usually taken once a day with or without food. To help you remember to take escitalopram, take it at around the same time every day, in the morning or in the evening. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take escitalopram exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor may start you on a low dose of escitalopram and increase your dose after 1 week.
It may take 1 to 4 weeks or longer before you feel the full benefit of escitalopram. Continue to take escitalopram even if you feel well. Do not stop taking escitalopram without talking to your doctor. If you suddenly stop taking escitalopram, you may experience withdrawal symptoms such as mood changes, irritability, agitation, dizziness, numbness or tingling in the hands or feet, anxiety, confusion, headache, tiredness, and difficulty falling asleep or staying asleep. Your doctor will probably decrease your dose gradually.
Who can and can’t take escitalopram
Escitalopram can be taken by adults over the age of 18.
Escitalopram isn’t suitable for some people. Check with your doctor before starting to take escitalopram if you:
- have had an allergic reaction to escitalopram or any other medicines in the past
- have epilepsy – as escitalopram can increase your seizures
- have a heart problem – as escitalopram can speed up or change your heartbeat
- have a low heart rate plus you have had severe diarrhoea and vomiting for a long time or take water tablets
- have liver or kidney problems – your doctor may need to change your dose
- have been told you have low sodium (salt) levels
- bruise or bleed easily
- are having electroconvulsive treatment
- have ever taken any other medicines for depression – some rarely used antidepressants can interact with escitalopram to cause very high blood pressure
- even when they’ve been stopped for a few weeks
- are trying to become pregnant, are already pregnant or are breastfeeding
- have an eye problem called glaucoma because escitalopram can increase the pressure in your eye
If you have diabetes, escitalopram can make it more difficult to keep your blood sugar stable. Monitor your blood sugar more often for the first few weeks of treatment with escitalopram and adjust your diabetes treatment if necessary.
Escitalopram special precautions
Before taking escitalopram:
- tell your doctor or pharmacist if you are allergic to escitalopram, citalopram (Celexa), or any other medications.
- tell your doctor if you are taking pimozide (Orap) or a monoamine oxidase (MAO) inhibitor such as isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate), or if you have stopped taking an MAO inhibitor within the past 14 days. Your doctor will probably tell you not to take escitalopram. If you stop taking escitalopram, you should wait at least 14 days before you start to take an MAO inhibitor.
- you should know that escitalopram is very similar to another SSRI, citalopram (Celexa). You should not take these two medications together.
- tell your doctor or pharmacist what prescription and nonprescription medications and vitamins you are taking or plan to take. Be sure to mention any of the following: anticoagulants (‘blood thinners’) such as warfarin (Coumadin); antihistamines; aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve, Naprosyn); carbamazepine (Tegretol); cimetidine (Tagamet); ketoconazole (Sporanox); lithium (Eskalith, Lithobid, Lithotabs); linezolid (Zyvox); medications for anxiety, mental illness, or seizures; medications for migraine headaches such as almotriptan (Axert), eletriptan (Relpax), frovatriptan (Frova), naratriptan (Amerge), rizatriptan (Maxalt), sumatriptan (Imitrex), and zolmitriptan (Zomig); metoprolol (Lopressor, Toprol XL); other antidepressants such as desipramine (Norpramin); sedatives; sibutramine (Meridia); sleeping pills; tramadol; methylene blue; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what nutritional supplements and herbal products you are taking, especially products containing St. John’s wort or tryptophan.
- tell your doctor if you have recently had a heart attack and if you have or have ever had seizures or liver, kidney, thyroid, or heart disease.
- tell your doctor if you are pregnant, especially if you are in the last few months of your pregnancy, or if you plan to become pregnant or are breast-feeding. If you become pregnant while taking escitalopram, call your doctor. Escitalopram may cause problems in newborns following delivery if it is taken during the last months of pregnancy.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking escitalopram.
- you should know that escitalopram may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by this medication.
- you should know that escitalopram may cause angle-closure glaucoma (a condition where the fluid is suddenly blocked and unable to flow out of the eye causing a quick, severe increase in eye pressure which may lead to a loss of vision). Talk to your doctor about having an eye examination before you start taking this medication. If you have nausea, eye pain, changes in vision, such as seeing colored rings around lights, and swelling or redness in or around the eye, call your doctor or get emergency medical treatment right away.
Cautions with other medicines
Some medicines and escitalopram can interfere with each other and increase the chances of you having side effects.
Tell your doctor if you’re taking these medicines before you start escitalopram:
- any medicines that affect your heartbeat – as escitalopram can speed up or change your heartbeat
- any other medicines for depression – some rarely used antidepressants can interact with escitalopram to cause very high blood pressure even when they have been stopped for a few weeks
These are not all the medicines that can interfere with escitalopram. For a full list see the leaflet inside your medicine packet or check with your pharmacist.
Mixing escitalopram with herbal remedies and supplements
Don’t take St John’s wort, the herbal remedy for depression, while you are being treated with escitalopram as this will increase your risk of side effects.
Tell your doctor or pharmacist if you’re taking any other medicines, including herbal remedies, vitamins or supplements.
Pregnancy and breastfeeding
It’s important for you and your baby that you stay well during your pregnancy. If you become pregnant while taking escitalopram speak to your doctor. Do not stop taking your medicine unless your doctor tells you to.
Escitalopram has been linked to a very small increased risk of problems for your unborn baby. However if your depression is not treated during pregnancy this can also increase the chance of problems.
You may need to take escitalopram during pregnancy if you need it to remain well. Your doctor can explain the risks and the benefits, and will help you decide which treatment is best for you and your baby.
Escitalopram and breastfeeding
If your doctor or health visitor says your baby is healthy, escitalopram can be used during breastfeeding.
Escitalopram passes into breast milk in small amounts, and has been linked with side-effects in very few breastfed babies.
It is important to continue taking escitalopram to keep you well. Breastfeeding will also benefit both you and your baby.
If you notice that your baby isn’t feeding as well as usual, or seems unusually sleepy, or if you have any other concerns about your baby, then talk to your health visitor or doctor as soon as possible.
Summary of escitalopram use during breastfeeding
Limited information indicates that maternal doses of escitalopram up to 20 mg daily produce low levels in milk and would not be expected to cause any adverse effects in breastfed infants, especially if the infant is older than 2 months. One case of necrotizing enterocolitis was reported in an breastfed newborn whose mother was taking escitalopram during pregnancy and lactation, but causality was not established. A seizure-like event occurred in an infant who was also exposed to bupropion in milk. Other minor behavioral problems have also been reported. Monitor the infant for drowsiness, especially in younger, exclusively breastfed infants and when using combinations of psychotropic drugs. Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state 2. These mothers may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants.
Eight women taking escitalopram in an average dosage of 199 mcg/kg daily (10 to 20 mg daily) had 6 to 8 milk steady-state milk samples analyzed over the 24-hour interval after their single daily dose. The average dosage that an exclusively breastfed infant would receive was calculated to be 7.6 mcg/kg of escitalopram and 3 mcg/kg of desmethylcitalopram daily which were 3.9% and 1.7% of the maternal weight-adjusted dosages, respectively. The absolute dosage was about 40% less than a previous study by the same authors with racemic citalopram 3.
A woman taking escitalopram had milk escitalopram concentrations measured twice. While taking a dosage of 5 mg daily, milk escitalopram was 24.9 mcg/L at 20 hours after the dose. While taking 10 mg escitalopram daily and valproic acid 1200 mg daily, milk escitalopram was 76.1 mcg/L at 15 hours after the dose. Using these two data points, the authors estimated that the infant received 5.1 and 7.7% of the maternal weight-adjusted dosage of escitalopram on these days, respectively 4.
One woman was taking escitalopram 20 mg daily and reboxetine 4 mg daily orally while nursing her 9.5-month-old infant. She collected milk samples before each breastfeeding session over a 1-day period. The authors estimated that the infant would receive 4.6% of the maternal-weight-adjusted dosage of escitalopram plus desmethylescitalopram 5.
A nursing mother was taking escitalopram 20 mg daily. Foremilk and hindmilk samples taken at 1 week postpartum, 12 hours after a dose contained 173 mcg/L and 195 mcg/L, respectively. The samples also contained 21 mcg/L and 24 mcg/L of S -desmethylcitalopram in foremilk and hindmilk, respectively 6.
Eighteen lactating women taking escitalopram in a mean daily dosage of 10 mg (range 2.5 to 30 mg [mean 0.2 mg/kg daily]) donated 3 to 5 random milk samples over a 24-hour period (n = 104 samples). The mean peak milk levels were 84.3 and 84.7 mcg/L for the 10 and 20 mg daily doses, respectively. Women taking 30 mg daily had an average peak milk level of 202 mcg/L. The average milk levels were 32.9 mcg/L with a dose of 10 mg daily, 49.8 mcg/L with a 20 mg dose and 136 mcg/L with 30 mg daily. Hindmilk concentrations averaged 10% higher than foremilk values. With a dose of 20 mg daily, the infant dosage was calculated to be 0.0078 mg/kg daily or 2.6% of the weight-adjusted maternal dosage 7.
Infant Levels
One study found that racemic citalopram serum levels in infants were determined by their CYP2C19 genotype, with slow metabolizers more likely to have detectable serum levels 8. Pharmacogenetics likely plays a part in determining the exposure of breastfed infants to escitalopram also.
In 8 breastfed infants whose mothers were taking an average of 199 mcg/kg daily of escitalopram (10 or 20 mg daily), escitalopram and desmethylescitalopram were undetectable in the serum of 3 infants (<1 mcg/L). The drug and metabolite serum levels were less than 5 mcg/L in all the other infants. Their mothers’ serum levels of the drug and metabolite averaged 24 and 20 mcg/L, respectively 3.
Eighteen lactating women taking escitalopram in a mean daily dosage of 10 mg (range 2.5 to 30 mg [mean 0.2 mg/kg daily]) donated 3 to 5 random milk samples over a 24-hour period (n = 104 samples). The data were used to construct a physiologically based pharmacokinetic model simulating 1600 infant serum levels whose mothers received a dose of 20 mg daily. The predicted average infant serum concentrations were 1.7% (range, 0.5 to 5.9%) of the average maternal serum concentrations. Age of the infant from birth to 1 year did not substantially impact the results 7.
Escitalopram effects in breastfed infants
Eight breastfed infants whose mothers were taking escitalopram in an average dose of 199 mcg/kg daily for postpartum depression were evaluated by a pediatric specialist using the Denver developmental scale. Their mothers had taken escitalopram for a median of 55 days postpartum (range 23 to 240 days). The infants’ scores on this scale was 110% of normal 3.
A woman began taking escitalopram 5 mg daily immediately after birth. Her dosage was increased to 10 mg daily and valproic acid 1200 mg daily was added by 7 weeks postpartum. Her breastfed infant was judged to be healthy and have normal neuropsychological development by a general practitioner at 7.5 weeks of age 9.
One woman was taking escitalopram 20 mg daily and reboxetine 4 mg daily orally while nursing her infant (extent not stated). She had taken reboxetine for 1.5 months, but the start of her escitalopram therapy was not stated. At 9.5 months of age, her breastfed infant had normal weight gain and a Denver developmental score of 105% of chronological age 5.
A nursing mother was given escitalopram 10 mg daily for depression beginning at 3 weeks postpartum and increasing to 20 mg daily thereafter. At 4 months of age, her exclusively breastfed infant was admitted to the hospital for irritability, vomiting and fever of 4 days duration. He had been irritable with prolonged periods of crying for the past 3 months according to his mother and had gained only 400 grams per month since birth. Liver enzymes were moderately elevated. The infant was discharged after 5 days and breastfeeding was continued, but only twice daily for 2 weeks, then discontinued at 4.5 months of age. At 5 months, symptom improvement was noted and at 6 months, serum liver enzymes had normalized. The author noted that the time course of the adverse effects were consistent with the treatment with escitalopram 10.
A mother began taking escitalopram 20 mg daily in the morning on day 15 postpartum. She exclusively breastfed her infant on demand. At 3 months of age, no adverse effects had been reported in the infant by his pediatrician 11.
At 5 days of age, an infant was readmitted to the neonatal intensive care unit with a diagnosis of necrotizing enterocolitis. The infant had spent the first 2 days of life in intensive care because of respiratory distress. The infant’s mother had taken escitalopram 20 mg daily throughout pregnancy and while breastfeeding (extent not stated). The authors hypothesized that escitalopram might have been responsible for the enterocolitis because of its effect on platelet aggregation 12. The drug was possibly a cause of the reaction.
One author reported on the newborn infant of a mother who was taking escitalopram (dose and duration not stated). The hyperirritable infant had high-pitched crying 2 hours after breastfeeding every afternoon which was 5 to 6 hours after maternal dose of escitalopram. Changing the time of the mother’s escitalopram dose resulted in a shift in the time of the infant’s crying at the same time interval after the dose. The infant’s symptoms improved with partial substitution of formula and ceased on day 11 of life with complete formula feeding 13.
An uncontrolled online survey compiled data on 930 mothers who nursed their infants while taking an antidepressant. Infant drug discontinuation symptoms (e.g., irritability, low body temperature, uncontrollable crying, eating and sleeping disorders) were reported in about 10% of infants. Mothers who took antidepressants only during breastfeeding were much less likely to notice symptoms of drug discontinuation in their infants than those who took the drug in pregnancy and lactation 14.
A 6.5-month-old infant developed severe vomiting and an apparent tonic seizure after being breastfed by her mother. The mother had been taking escitalopram 10 mg daily since birth and had begun extended-release bupropion 150 mg daily 3 weeks earlier. The seizure occurred 8 hours after the mother’s morning dose of bupropion. The infant’s mother had noted disturbances in sleep behavior, unusual movements, and unresponsiveness followed by sleep on several previous occasions. The baby was partially breastfed, also receiving pumped breastmilk, formula, and solid foods. Breastfeeding was discontinued and the baby was discharged after being asymptomatic for 48 hours. The seizure was probably drug-related, most likely caused by bupropion and hydroxybupropion in breastmilk, but a contribution by escitalopram cannot be ruled out 15.
A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation. Of the 247 infants, 154 developed poor neonatal adaptation. Infants who were exclusively given formula had about 3 times the risk of developing poor neonatal adaptation as those who were exclusively or partially breastfed. None of the infants were exposed to escitalopram in utero, but 51 were exposed to citalopram, the racemic form of the drug 16.
A case-control study in Israel compared 280 infants of nursing mothers taking long-term psychotropic drugs to the infants of 152 women taking antibiotics. Infant sleepiness at 3 days of age was reported by 1 mother taking escitalopram and none taking antibiotics. The sleepiness resolved within 24 hours with no developmental effect 17.
Can taking escitalopram during my pregnancy cause birth defects?
Unlikely. Citalopram has not been associated with an increase in birth defects in human studies. One study showed citalopram might cross the placenta in lower amounts than some of the other SSRI medications. There are no large studies looking at the chance of birth defects when escitalopram is used during pregnancy. Since it is very similar to citalopram, escitalopram is also unlikely to increase the chance of birth defects over a background risk.
I need to take escitalopram throughout my entire pregnancy. Will it cause withdrawal symptoms in my baby?
If you are taking escitalopram at the end of your pregnancy, your baby may need some extra care for the first few days of life. Babies exposed to any SSRI may have breathing problems, jitteriness, increased muscle tone, irritability, problems sleeping, tremors and difficulty feeding. These symptoms are usually mild and should go away by two weeks of age.
Will taking escitalopram have any long-term effect on my baby’s behavior and development?
One small study followed eleven babies of mothers who took citalopram during pregnancy. At one year of age there was no difference in their development compared to children who were not exposed. More studies are needed before we will know if there are any long-term effects on the baby’s brain development.
Are there any other problems escitalopram can cause when used in the third trimester?
Some studies suggested that babies whose mothers take SSRIs like citalopram or escitalopram during the third trimester might have a small increased chance for persistent pulmonary hypertension of the newborn, however, other studies have not. Persistent pulmonary hypertension of the newborn is a serious lung problem. The background risk for persistent pulmonary hypertension of the newborn is about 1 to 2 babies in 1,000 births, around 0.12%. This is a less than 1% chance. If there is an increased chance for persistent pulmonary hypertension of the newborn from SSRIs, it is still less than 1%; maybe around 0.30%. Further study is needed. Tell your health care providers and your baby’s pediatrician that you are taking escitalopram, and they will exam your baby at birth.
I am taking escitalopram, but I would like to stop taking it before becoming pregnant.
You should not make any changes in your medication without first talking to your health care providers. You and your health care provider should discuss the benefits of taking escitalopram for your specific situation and the potential risks to the baby before making a decision. If you are going to stop taking escitalopram, you should talk to your health care provider about cutting back on the dose slowly. Gradually cutting back might help to avoid withdrawal symptoms.
Studies have shown that when depression is left untreated during pregnancy, there could be an increased chance for pregnancy complications. Some women remain well after stopping their antidepressant medication during pregnancy. For other women, stopping their medication can be more harmful than the risks of staying on it. After delivery, untreated depression can lead to difficulty bonding with your newborn and an increased chance for postpartum depression.
Can taking escitalopram make it more difficult for me to become pregnant?
It is not known if taking escitalopram will make it harder to get pregnant. Studies in animals found that citalopram might have caused some reduced fertility. So far, there have been no reports of humans having a harder time getting pregnant while taking these medicines.
Can taking escitalopram cause a miscarriage?
Probably not. There have been some studies that suggested taking antidepressant medications may slightly increase the chance for miscarriage. However, a study on escitalopram did not find an increased chance for miscarriage in women taking these medications.
Can I take escitalopram while breastfeeding?
Several studies have shown that small amounts of citalopram and escitalopram are found in breast milk. There have been a few cases of sleepiness and weight loss, but in most studies no harmful effects were seen in the breastfed babies. Some studies also showed no difference in the intellectual development of babies whose mothers took citalopram or escitalopram while breastfeeding. The risk to the breastfed infant appears to be small, and the benefits of breastfeeding are well known. Be sure to talk to your health care provider about all your breastfeeding questions.
What is escitalopram used for?
Escitalopram is a type of antidepressant known as an SSRI (selective serotonin reuptake inhibitor) that is often used to treat depression and is sometimes used for anxiety, obsessive compulsive disorder or panic attacks.
Escitalopram helps many people recover from depression, and it has fewer unwanted effects than older antidepressants.
Escitalopram dosage
Escitalopram tablets come in different strengths ranging from 5mg to 20mg.
The usual dose of escitalopram is 10mg a day in adults. However, you may start on a lower dose and increase to a maximum dose of 20mg a day. If you have liver problems, the maximum recommended dose is 10mg a day.
With liquid drops of escitalopram, 1 drop is equivalent to 1mg, 10 drops is 10mg, 20 drops is 20mg.
Dose adjustments
- Treatment withdrawal: A gradual dose reduction is recommended instead of abrupt cessation where possible
- Switching between MAOI (monoamine oxidase inhibitor) and escitalopram: At least 14 days should elapse between ceasing one of these medicines and starting the other.
Adult Dose for Generalized Anxiety Disorder
Use: Acute treatment of generalized anxiety disorder
- Initial dose: 10 mg orally once a day; increase if necessary after at least 1 week of treatment to 20 mg once a day
- Maintenance dose: 10 to 20 mg orally once a day
- Maximum dose: 20 mg orally once a day
Comment: Treatment should be periodically reassessed to determine the need for ongoing treatment; efficacy beyond 8 weeks has not been systematically studied.
Adult Dose for Depression
Use: Acute and maintenance treatment of major depressive disorder
- Initial dose: 10 mg orally once a day; increase if necessary after at least 1 week of treatment to 20 mg once a day
- Maintenance dose: 10 to 20 mg orally once a day
- Maximum dose: 20 mg orally once a day
Comments:
- Acute episodes may require several months or longer of sustained pharmacological therapy beyond response to the acute episode.
- Patients should be periodically reassessed to determine the need for maintenance treatment.
Geriatric Dose for Depression
Use: Acute and maintenance treatment of major depressive disorder
- Recommended dose: 10 mg orally once a day
Pediatric Dose for Depression
Use: Acute and maintenance treatment of major depressive disorder
12 years and older:
- Initial dose: 10 mg orally once a day; increase if necessary after at least 3 weeks of treatment to 20 mg once a day
- Maintenance dose: 10 to 20 mg orally once a day
- Maximum dose: 20 mg orally once a day
Comments:
- Acute episodes may require several months or longer of sustained pharmacological therapy beyond response to the acute episode.
- Patients should be periodically reassessed to determine the need for maintenance treatment.
Renal Dose Adjustments
- Mild to moderate renal dysfunction: No adjustment recommended
- Severe renal dysfunction: Use with caution
Liver Dose Adjustments
- Liver dysfunction: 10 mg orally once a day
What should I do if I forget a dose?
Do not take a double dose to make up for forgotten doses. If you do forget to take a dose, and you remember before you go to bed, take it straight away. Carry on as usual the next day. If you only remember during the night, or the next day, leave out the missed dose and carry on as usual.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
Ask your doctor for advice straight away. An overdose can lead to potentially serious symptoms such as:
- agitation
- being sick (vomiting)
- shaking
- fast heart rate
- seizures
Escitalopram side effects
Like all medicines, escitalopram can cause side effects in some people, but many people have no side effects or only minor ones. Some of the common side effects of escitalopram will gradually improve as your body gets used to it.
Common side effects
Common side effects may happen in more than 1 in 10 people. Keep taking the medicine but talk to your doctor or pharmacist if these side effects bother you or don’t go away:
- dry mouth
- sweating a lot
- being unable to sleep
- feeling sleepy
- feeling tired or weak
Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- diarrhea
- constipation
- changes in sex drive or ability
- drowsiness
- increased sweating
- dizziness
- heartburn
- stomach pain
- excessive tiredness
- dry mouth
- increased appetite
- flu-like symptoms
- runny nose
- sneezing
Serious side effects
Serious side effects are rare and happen in less than 1 in 1,000 people. Tell a doctor straight away if you get:
- headache, trouble focusing, memory problems, not thinking clearly, weakness, seizures or losing your balance – these can be signs of low sodium levels
thoughts about harming yourself or ending your life - a high temperature (above 38C) with agitation, confusion, trembling and twitching
- severe dizziness or passing out
- weight gain or loss without trying to
- changes in your periods such as heavy bleeding, spotting or bleeding between periods
- painful erections that last longer than 4 hours – this may happen even when you are not having sex
Or, if you develop any signs of abnormal bleeding including:
- vomiting blood or dark vomit, coughing up blood, blood in your pee, black or red poo – these can be signs of bleeding from the gut
- bleeding from the gums or bruises that appear without a reason or that get bigger
- any bleeding that is very bad or that you cannot stop
Some side effects can be serious. If you experience either of the following symptoms or those listed in the IMPORTANT WARNING or SPECIAL PRECAUTIONS sections, call your doctor immediately:
- unusual excitement
- seeing things or hearing voices that do not exist (hallucinating)
- fever, sweating, confusion, fast or irregular heartbeat, and severe muscle stiffness
Serious allergic reaction
In rare cases, it’s possible to have a serious allergic reaction to escitalopram. A serious allergic reaction is an emergency. Contact a doctor straight away if you think you or someone around you is having a serious allergic reaction.
The warning signs of a serious allergic reaction are:
- getting a skin rash that may include itchy, red, swollen, blistered or peeling skin
- wheezing
- tightness in the chest or throat
- having trouble breathing or talking
- swelling of the mouth, face, lips, tongue, or throat
These are not all the side effects of escitalopram. For a full list see the leaflet inside your medicines packet.
Escitalopram may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
How to cope with side effects
What to do about:
- feeling sleepy – cut down the amount of alcohol you drink
- dry mouth – chew sugar-free gum or sugar-free sweets
- being unable to sleep – take escitalopram first thing in the morning
Except for problems getting to sleep, you can reduce the chance of having a side effect that bothers you if you take escitalopram in the evening. That way you’re asleep when the level of medicine in your body is highest.
Escitalopram withdrawal
Case reports of escitalopram discontinuation syndrome involved 2 patients 18. One subject gradually reduced escitalopram (over 3 weeks) 18, while the other first missed a few doses and then reduced the drug very gradually (over 9 months) 19. Both experienced electric-shock sensations a few days after drug stoppage, which lasted from 5 days 18 to 4 weeks 19.
Despite the limited literature available, the results of this systematic review indicate that withdrawal symptoms may occur with any type of SSRI (citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline), even though they are exceedingly more frequent with paroxetine 20.
The pathophysiological mechanisms of withdrawal phenomena are still hypothetical and in need of proper neurobiological investigations 20. A number of mechanisms have been suggested: a decrease in serotonin availability when treatment ends 21, a behavioral stress response that is associated with increased hippocampal N-methyl-D-aspartate (NMDA) receptor density 22, and genetic vulnerabilities 23. Animal studies concerned with the long-term use of antidepressant drug have limited implications, since clear discontinuation-like behaviors in animal models are not available 24. Fava and Offidani 25 have interpreted the withdrawal phenomena according to the oppositional model of tolerance. Continued drug treatment may recruit processes that oppose the initial acute effects of a drug and may lead to a loss of efficacy and/or to a treatment-unresponsive course. When drug treatment ends, oppositional processes may operate for some time, resulting in the appearance of withdrawal symptoms and/or an increased vulnerability to relapse and/or resistance to treatment (if it is reinstituted) and/or switching to a bipolar course 25. The appearance of withdrawal symptoms after SSRI discontinuation may thus be potentially related to a number of important clinical phenomena 26.
Escitalopram overdose
In clinical trials of escitalopram, there were reports of escitalopram overdose, including overdoses of up to 600 mg, with no associated fatalities. During the postmarketing evaluation of escitalopram, escitalopram oxalate overdoses involving overdoses of over 1000 mg have been reported. As with other SSRIs, a fatal outcome in a patient who has taken an overdose of escitalopram has been rarely reported.
Symptoms most often accompanying escitalopram overdose, alone or in combination with other drugs and/or alcohol, included convulsions, coma, dizziness, hypotension, insomnia, nausea, vomiting, sinus tachycardia, somnolence, and ECG changes (including QT prolongation and very rare cases of torsade de pointes). Acute renal failure has been very rarely reported accompanying overdose.
Symptoms of overdose may include:
- dizziness
- sweating
- nausea
- vomiting
- tremor
- drowsiness
- fast or pounding heartbeat
- seizures
- confusion
- forgetfulness
- fast breathing
- coma (loss of consciousness for a period of time)
Management of escitalopram overdose
Establish and maintain an airway to ensure adequate ventilation and oxygenation. Gastric evacuation by lavage and use of activated charcoal should be considered. Careful observation and cardiac and vital sign monitoring are recommended, along with general symptomatic and supportive care. Due to the large volume of distribution of escitalopram, forced diuresis, dialysis, hemoperfusion, and exchange transfusion are unlikely to be of benefit. There are no specific antidotes for escitalopram oxalate.
In managing overdosage, consider the possibility of multiple-drug involvement. The physician should consider contacting a poison control center for additional information on the treatment of any overdose.
References- Weissman AM, Levy BT, Hartz AJ et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry. 2004;161:1066-78. https://doi.org/10.1176/appi.ajp.161.6.1066
- Grzeskowiak LE, Leggett C, Costi L et al. Impact of serotonin reuptake inhibitor use on breast milk supply in mothers of preterm infants: A retrospective cohort study. Br J Clin Pharmacol. 2018;84:1373-9 https://www.ncbi.nlm.nih.gov/pubmed/29522259
- Rampono J, Hackett LP, Kristensen JH et al. Transfer of escitalopram and its metabolite demethylescitalopram into breastmilk. Br J Clin Pharmacol. 2006;3:316-22 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1885141/
- Castberg I, Spigset O. Excretion of escitalopram in breast milk. J Clin Psychopharmacol. 2006;26:536-8 https://www.ncbi.nlm.nih.gov/pubmed/16974204
- Hackett LP, Ilett KF, Rampono J et al. Transfer of reboxetine into breastmilk, its plasma concentrations and lack of adverse effects in the breastfed infant. Eur J Clin Pharmacol. 2006;62:633-8. https://www.ncbi.nlm.nih.gov/pubmed/16699799
- Weisskopf E, Panchaud A, Nguyen KA et al. Simultaneous determination of selective serotonin reuptake inhibitors and their main metabolites in human breast milk by liquid chromatography-electrospray mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2017;1057:101-9. https://www.ncbi.nlm.nih.gov/pubmed/28511118
- Delaney SR, Malik PRV, Stefan C et al. Predicting escitalopram exposure to breastfeeding infants: Integrating analytical and in silico techniques. Clin Pharmacokinet. 2018 https://www.ncbi.nlm.nih.gov/pubmed/29651785
- Berle JO, Steen VM, Aamo TO et al. Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: infant exposure, clinical symptoms, and cytochrome P450 genotypes. J Clin Psychiatry. 2004;65:1228-34 https://www.ncbi.nlm.nih.gov/pubmed/15367050
- Castberg I, Spigset O. Excretion of escitalopram in breast milk. J Clin Psychopharmacol. 2006;26:536-8. https://www.ncbi.nlm.nih.gov/pubmed/16974204
- Merlob P. Use of escitalopram during lactation. BELTIS Newsl. 2005;Number 13:40-4.
- Gentile S. Escitalopram late in pregnancy and while breast-feeding. Ann Pharmacother. 2006;40:1696-7. https://www.ncbi.nlm.nih.gov/pubmed/16912243
- Potts AL, Young KL, Carter BS, Shenai JP. Necrotizing enterocolitis associated with in utero and breast milk exposure to the selective serotonin reuptake inhibitor, escitalopram. J Perinatol. 2007;27:120-2
- Schaefer C, Peters P, Miller RK, eds. Drugs during pregnancy and lactation. Treatment options and risk assessment, 2nd ed. Amsterdam; Boston: Elsevier Academic Press. 2007:714-5.
- Hale TW, Kendall-Tackett K, Cong Z et al. Discontinuation syndrome in newborns whose mothers took antidepressants while pregnant or breastfeeding. Breastfeed Med. 2010;5:283-8.
- Neuman G, Colantonio D, Delaney S et al. Bupropion and escitalopram during lactation. Ann Pharmacother. 2014;48:928-31
- Kieviet N, Hoppenbrouwers C, Dolman KM et al. Risk factors for poor neonatal adaptation after exposure to antidepressants in utero. Acta Paediatr. 2015;104:384-91
- Kronenfeld N, Ziv Baran T, Berlin M et al. Chronic use of psychotropic medications in breastfeeding women: Is it safe? PLoS One. 2018;13:e0197196
- Feth N, Cattapan-Ludewig K, Jaquenoud-Sirot E: Electric sensations: neglected symptom of escitalopram discontinuation. Am J Psychiatry 2006;163:160.
- Prakash O, Dhar V: Emergence of electric shock-like sensations on escitalopram discontinuation. J Clin Psychopharmacol 2008;28:359-360.
- Withdrawal Symptoms after Selective Serotonin Reuptake Inhibitor Discontinuation: A Systematic Review. Psychother Psychosom 2015;84:72-81 https://doi.org/10.1159/000370338
- Blier P, Tremblay P: Physiologic mechanisms underlying the antidepressant discontinuation syndrome. J Clin Psychiatry 2006;67:8-13.
- Harvey BH, McEwen BS, Stein DJ: Neurobiology of antidepressant withdrawal: implications for longitudinal outcome of depression. Biol Psychiatry 2003;54:1105-1117.
- Murata Y, Kobayashi D, Imuta N, Haraguchi K, Ieiri I, Nishimura R, Koyama S, Mine K: Effects of serotonin 1A, 2A, 2C, 3A and 3B and serotonin transporter gene polymorphisms on the occurrence of paroxetine discontinuation syndrome. J Clin Psychopharmacol 2010;30:11-17.
- Renoir T: Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Front Pharmacol 2013;4:1-10.
- Fava GA, Offidani E: The mechanisms of tolerance in antidepressant action. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:1593-1602.
- Fava GA: Rational use of antidepressant drugs. Psychother Psychosom 2014;83:197-204.