What is fatty liver disease
Fatty liver disease is a condition in which fat (triglycerides) builds up in your liver. Fatty liver or hepatic steatosis, is the accumulation of fat within liver cells, is a common histological finding in human liver biopsy specimens and affects 10–24% of the general population 1. There are two main types of fatty liver disease 2:
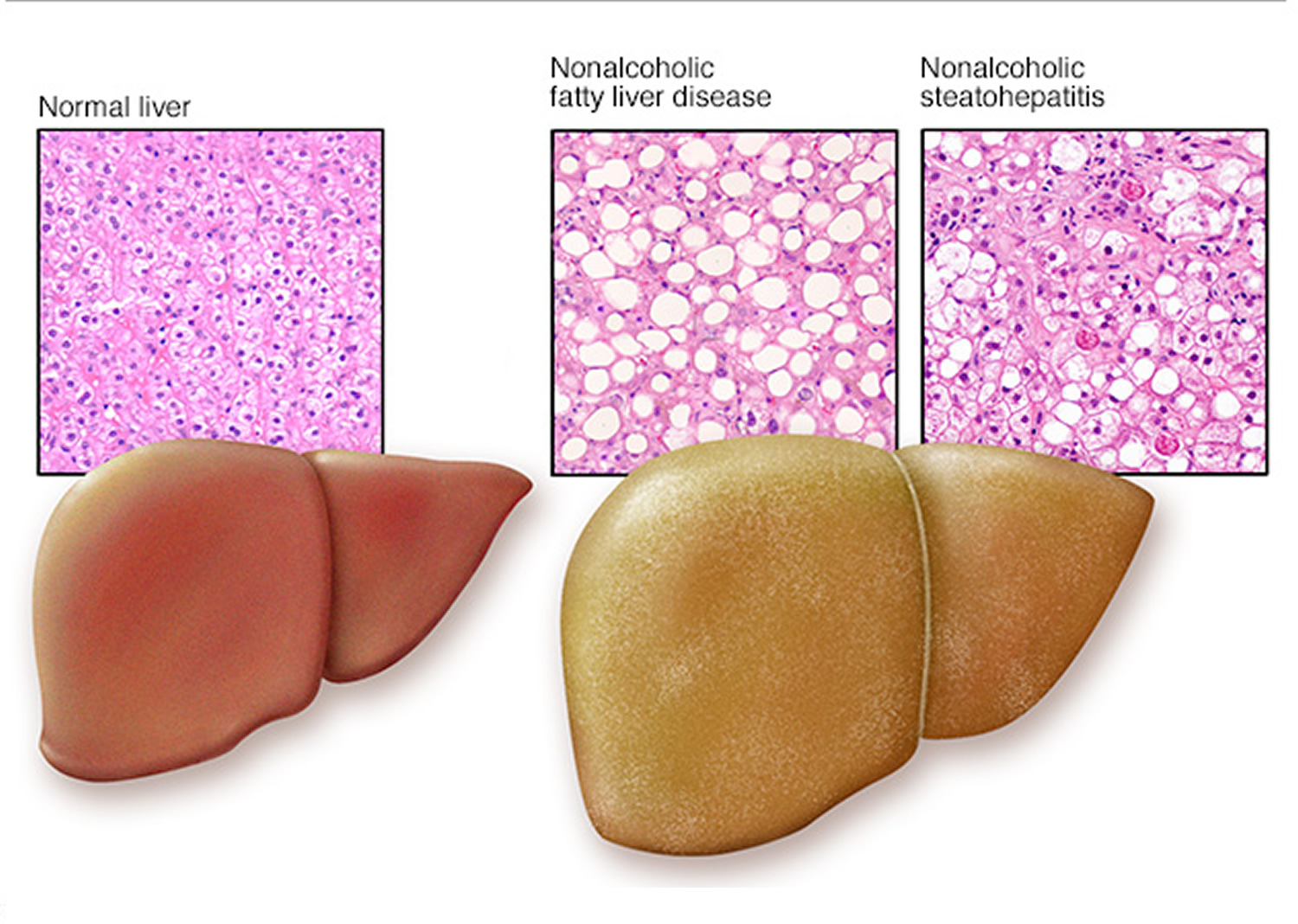
- Nonalcoholic fatty liver disease (NAFLD). Nonalcoholic fatty liver disease (NAFLD) is a type of fatty liver disease that is not related to heavy alcohol use. Nonalcoholic fatty liver disease (NAFLD) is the most common form of liver disease in the United States, affecting up to 30% of adults 3. There are two kinds of NAFLD 4:
- Simple fatty liver also called nonalcoholic fatty liver (NAFL): Simple fatty liver is a form of nonalcoholic fatty liver disease (NAFLD) in which you have fat in your liver but little or no inflammation or liver cell damage. Simple fatty liver or nonalcoholic fatty liver (NAFL) is defined as 5% or greater hepatic steatosis without hepatocellular injury or fibrosis 3. Simple fatty liver typically does not progress to cause liver damage or complications 5.
- Nonalcoholic steatohepatitis (NASH): Nonalcoholic steatohepatitis (NASH) is a form of nonalcoholic fatty liver disease (NAFLD) in which you have inflammation and liver cell damage, in addition to fat in your liver. Nonalcoholic steatohepatitis (NASH) is defined as 5% or greater hepatic steatosis plus hepatocellular injury and inflammation, with or without fibrosis 3. This form of liver injury carries a 20%-50% risk for progressive liver fibrosis, 30% risk for cirrhosis, and 5% risk for hepatocellular carcinoma (liver cancer) 6. Nonalcoholic steatohepatitis (NASH) may lead to cirrhosis or liver cancer 5.
- Alcoholic fatty liver disease also called alcoholic steatohepatitis. Alcoholic fatty liver disease (alcoholic steatohepatitis) is due to heavy alcohol use. Your liver breaks down most of the alcohol you drink, so it can be removed from your body. But the process of breaking it down can generate harmful substances. These substances can damage liver cells, promote inflammation, and weaken your body’s natural defenses. The more alcohol that you drink, the more you damage your liver. Alcoholic fatty liver disease is the earliest stage of alcohol-related liver disease. The next stages are alcoholic hepatitis and cirrhosis.
Your liver is the largest organ inside your body and it is a vital organ that performs many essential functions. Your liver filters out harmful substances from your blood, makes bile to digest food, stores energy and nutrients, and manufactures hormones, proteins, and enzymes your body uses to function, remove poisons and ward off disease 7.
The fatty liver may or may not be inflamed. Inflammation of the liver due to fatty liver is called steatohepatitis. This inflammation may develop into scarring (fibrosis). Fibrosis often progresses to cirrhosis (scarring that distorts the structure of the liver and impairs its function).
Fatty liver (with or without fibrosis) due to any condition except consumption of large amounts of alcohol is called nonalcoholic fatty liver disease (NAFLD). NAFLD develops most often in people with at least one of the components of metabolic syndrome:
- Excess body weight
- High fat levels in the blood (triglyceride and cholesterol)
- Insulin resistance
Inflammation of the liver due to NAFLD is called nonalcoholic steatohepatitis (NASH). This inflammation may develop into scarring (fibrosis) and cirrhosis.
People with fatty liver may feel tired or have mild abdominal discomfort but otherwise have no symptoms. Sometimes fatty liver causes advanced liver disease such as fibrosis and cirrhosis.
A liver biopsy may be needed to confirm the diagnosis and to determine the cause and extent of the damage.
There are no medicines to treat fatty liver disease. Treatment of fatty liver focuses on controlling or eliminating the cause of fatty liver. Treatment involves making changes to your lifestyle. This can improve the condition and even reverse it. Doctors focus on controlling or eliminating the cause of fatty liver, such as metabolic syndrome or consumption of large amounts of alcohol.
Liver anatomy
Your liver is essential to your life. You cannot live without your liver. Your liver is the largest internal organ in your body. Your liver is about the size of a football and weighs about 3 to 3.5 pounds (1.36–1.59kg). Your liver lies under your right ribs just beneath your right lung. Your liver has two lobes (sections). Your liver is made up mainly of liver cells called hepatocytes. It also has other types of cells, including cells that line its blood vessels and cells that line small tubes in the liver called bile ducts. The bile ducts carry bile from the liver to the gallbladder or directly to the intestines.
Your liver has many important functions:
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It delivers bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
Figure 1. Liver anatomy
Fatty liver of pregnancy
Nonalcoholic fatty liver disease (NAFLD) is considered the liver manifestation of the metabolic syndrome, and is tightly linked with obesity and type 2 diabetes 8. The obesity epidemic has affected reproductive-aged women, with obesity present in over one third of U.S. women ages 20–39 years 9. Pregnancy itself is a relative insulin resistant state and concurrent maternal obesity further increases the risk for gestational diabetes 10.
In the U.S., a study was conducted from 2012 to 2016 on a total of 18.5 million pregnant women 11. The aim was to find out how high certain pregnancy risks are in comparison groups 11. In the evaluation, a distinction was made between 3 groups of pregnant women. The first group consisted of women without liver disease. The second group had chronic liver disease (n = 115,210). The third group were women with NAFLD (n = 5,640). It was shown that pregnant women with nonalcoholic fatty liver disease (NAFLD) have a higher risk of developing pregnancy-associated (gestational) diabetes compared to the control group (23 in 100 compared to 7-8 in 100) 11. It was also found that pregnant women with NAFLD are also more frequently affected by severe pregnancy-induced increases in blood pressure (16 out of 100 compared to 4 out of 100 if there was no liver disease), of which the HELLP (hemolysis-elevated liver tests-low platelet count) syndrome is the most severe complication. HELLP syndrome is a rare life-threatening condition during pregnancy, the course of which is difficult to predict. This leads to a breakdown of the red blood cells, increased liver enzymes and a drop in red blood platelets. HELLP syndrome can result in immediate termination of pregnancy.
Your gynaecologist should contact the doctor treating your fatty liver disease and make an assessment of your possible individual risks of pregnancy. You should be informed in detail. In addition, physicians should support you in reducing metabolic risk factors, such as the existence of fatty liver, during a planned pregnancy.
Fatty liver causes
Fat accumulates in the liver for several reasons. Most commonly, fatty liver involves increased delivery of free fatty acids to the liver, increased synthesis of fatty acids in the liver, decreased oxidation of free fatty acid, or decreased synthesis or secretion of very-low-density lipoprotein (VLDL) 12. Oxidative stress in the liver cells can activate stellate cells and lead to the production of collagen and inflammation 13.
The most common causes of fatty liver in the United States and other Western countries are 14:
- Consumption of large amounts of alcohol
- Obesity
- Type 2 diabetes and prediabetes
- Metabolic abnormalities, such as excess body weight, insulin resistance (as can occur in diabetes), and high levels of fats (triglycerides and cholesterol) in the blood
- Metabolic syndrome (insulin resistance, high blood pressure, high cholesterol and high triglyceride levels).
- Polycystic ovary syndrome (PCOS).
- Obstructive sleep apnea.
- Hypothyroidism (underactive thyroid).
- Hypopituitarism (low pituitary gland hormones).
- Hypogonadism (low sex hormones).
- Exposure to some toxins
- Certain drugs, including corticosteroids, amiodarone, diltiazem, tamoxifen, HIV treatment, estrogens, and certain chemotherapy drugs and others
- Hereditary metabolic disorders called lipodystrophies, that cause your body to use or store fat improperly
- Pregnancy
Other factors that may contribute to fatty liver disease include:
- The use of medications (e.g., tamoxifen, amiodarone, methotrexate)
- Metabolic disorders (e.g., metabolic syndrome, glycogen storage disorders, homocystinuria)
- Nutritional status (e.g., total parenteral nutrition, severe malnutrition, overnutrition, or a starvation diet)
- Rapid weight loss or malnutrition
- Rare genetic diseases like Wilson disease, celiac disease and hypobetalipoproteinemia
- Middle aged or older (although children can also get it)
- Hispanic, followed by non-Hispanic whites. It is less common in African Americans.
- High blood pressure
- Hepatitis C.
The combination of excess body weight, insulin resistance, and high triglyceride levels is called metabolic syndrome. All of these conditions cause fat to accumulate in liver cells by causing the body to synthesize more fat or by processing (metabolizing) and excreting fat more slowly. As a result, fat accumulates and is then stored inside liver cells. Just consuming a high-fat diet does not result in fatty liver.
Alcoholic fatty liver disease only happens in people who are heavy drinkers, especially those who have been drinking for a long period of time. The risk is higher for heavy drinkers who are women, have obesity, or have certain genetic mutations.
Rarely, fat accumulates in the liver during late pregnancy. This disorder, called fatty liver of pregnancy or microvesicular steatosis, is usually considered a different disorder from fatty liver.
Fatty liver prevention
The way to prevent non-alcoholic fatty liver disease (NAFLD) is to follow the same lifestyle advice given to people who already have the condition, including:
- Eat a healthy diet. Eat a healthy diet that’s rich in fruits, vegetables, whole grains and healthy fats.
- Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks like soda, sports drinks, juices and sweet tea. Drinking alcohol can damage your liver and should be avoided or minimized.
- Keep a healthy weight. If you are overweight or obese, work with your health care team to gradually lose weight. If you are a healthy weight, work to keep it by eating a healthy diet and exercising.
- Exercise. Be active most days of the week. Get an OK from your health care team first if you haven’t been exercising regularly.
Fatty liver symptoms
Fatty liver usually causes no symptoms. Some people may feel tired or generally unwell or have vague abdominal discomfort in the upper right part of their abdomen. The liver tends to enlarge and can be detected by doctors during a physical examination.
More commonly, people notice symptoms once fatty liver has progressed to cirrhosis of the liver. When cirrhosis develops, you may experience:
- Nausea.
- Loss of appetite.
- Unexplained weight loss.
- Yellowish skin and whites of the eyes (jaundice).
- Swelling in your abdomen (ascites)
- Swelling in your legs, feet or hands (edema).
- Bleeding (that your doctor finds in your esophagus, stomach or rectum).
Fatty liver disease complications
In many people, fatty liver by itself doesn’t cause too many problems. But in some people the fatty liver gets inflamed, causing a more serious condition called non-alcoholic steatohepatitis, or NASH. Ongoing inflammation may scar the liver, which can lead to cirrhosis. This is a serious illness. A few people who get cirrhosis of the liver develop liver cancer. Some people who develop severe cirrhosis of the liver need to have a liver transplant.
People with fatty liver have an increased risk of heart attack and stroke.
Fatty liver diagnosis
If your doctor suspects fatty liver, he may ask about your alcohol use. This information is crucial. Continued and excessive alcohol use can cause severe liver damage.
Your doctor will also ask about your diet and lifestyle factors that may make you more likely to develop non-alcoholic fatty liver disease (NAFLD), such as a lack of physical activity, eating a diet high in sugar, or drinking sugary beverages.
However, because fatty liver causes no symptoms in most cases, it frequently comes to medical attention when tests done for other reasons point to a liver problem. This can happen if your liver looks unusual on ultrasound or if you have an abnormal liver enzyme test.
Tests done to pinpoint the diagnosis and determine disease severity include:
Blood tests
- Complete blood count
- Liver enzyme and liver function tests. Your doctor may suspect you have NAFLD if your blood test shows increased levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST).
- Tests for chronic viral hepatitis (hepatitis A, hepatitis C and others)
- Celiac disease screening test
- Fasting blood sugar
- Hemoglobin A1C (HbA1c), which shows how stable your blood sugar is
- Lipid profile, which measures blood fats, such as cholesterol and triglycerides
Your doctor may use the results of routine blood tests to calculate special scores, such as the FIB-4 or APRI. These scores can help doctors identify or rule out advanced liver fibrosis, or scarring.
Imaging procedures
Imaging procedures used to diagnose fatty liver include:
- Abdominal ultrasound, which is often the initial test when liver disease is suspected.
- Computerized tomography (CT) scanning or magnetic resonance imaging (MRI) of the abdomen. These techniques lack the ability to distinguish NASH from NAFLD, but still may be used.
- Transient elastography, an enhanced form of ultrasound that measures the stiffness of your liver. Liver stiffness indicates fibrosis or scarring.
- Magnetic resonance elastography, works by combining MRI imaging with sound waves to create a visual map (elastogram) showing the stiffness of body tissues.
Liver biopsy
If other tests are inconclusive, your doctor may recommend a procedure to remove a sample of tissue from your liver (liver biopsy). Liver biopsy is the only test that can prove a diagnosis of NASH and show clearly how severe the disease is. For liver biopsy, a doctor gives a local anesthetic to lessen any pain, then inserts a long hollow needle through the skin and into the liver to obtain a small piece of liver tissue for examination under a microscope. The tissue sample is examined in a laboratory to look for signs of inflammation and scarring.
A liver biopsy can be uncomfortable, and it does have small risks that your doctor will review with you in detail.
A liver biopsy can help determine whether fatty liver is present, whether it resulted from alcohol or certain other specific causes, and how severe the liver damage is.
Fatty liver treatment
There are no medicines to treat fatty liver disease. Treatment of fatty liver focuses on controlling or eliminating the cause of fatty liver. Lifestyle modifications and weight loss are the mainstays of the treatment 15. Treatment also involves glycemic (blood sugar) and lipid control. For patients with significant obesity, gastric bypass or other weight loss surgical modalities should be considered. Weight loss is proven to reduce fatty liver. Evidence available suggests that weight loss of 3% to 5% of body weight is necessary to notice an improvement in fatty liver, but a greater loss (up to 10%) is necessary to improve liver inflammation 16, 17.
Patients should also abstain from alcohol or liver toxic drugs.
If your fatty liver is caused by alcohol, then the most important thing to do is give up alcohol. This will prevent you from developing a more serious condition.
If you have non-alcoholic fatty liver disease (NAFLD), you will probably be advised to:
- Drink no or very little alcohol
- Follow a healthy diet and avoid sugar. Eat a healthy diet that’s rich in fruits, vegetables and whole grains, and keep track of all calories you take in.
- Lose weight. If you’re overweight or obese, reduce the number of calories you eat each day and increase your physical activity in order to lose weight. Calorie reduction is the key to losing weight and managing this disease. If you have tried to lose weight in the past and have been unsuccessful, ask your doctor for help.
- Exercise regularly. Aim for at least 30 minutes of exercise most days of the week. If you’re trying to lose weight, you might find that more exercise is helpful. But if you don’t already exercise regularly, get your doctor’s OK first and start slowly.
- Control your blood sugar. Follow your doctor’s instructions to stay in control of your diabetes. Take your medications as directed and closely monitor your blood sugar.
- Treat high cholesterol if you have it. A healthy plant-based diet, exercise and medications can help keep your cholesterol and your triglycerides at healthy levels.
- Avoid medicines that can affect your liver
- Quit smoking
Your doctor can help you. They may refer you to a dietitian, drug and alcohol counselor or specialist.
Avoiding all fat in your diet is not necessary. However, your doctor may recommend that you avoid certain foods, such as those that contain fructose (the sugar in fruit) and trans fats (a type of fat).
There is no specific medicine for fatty liver disease. However, depending on your situation, your doctor may advise that you take medicine to lower your lipid levels, or improve the way your body manages glucose.
No medicines have been approved to treat nonalcoholic fatty liver disease (NAFLD) by the US Food and Drug Administration or by the European Medicines Agency. However, researchers are studying medicines that may improve these conditions. Medicine options include Metformin, Vitamin E, fish oil, Orlistat (an inhibitor of gastric and pancreatic lipase), and Sibutramine. It is important to notice that the evidence behind these pharmacological modalities is weak 13.
According to the European Association for the Study of the Liver guidelines 18, drug therapy should be reserved for: Progressive NASH (bridging fibrosis and cirrhosis); early-stage NASH at high risk for disease progression (age > 50 years, metabolic syndrome, diabetes mellitus or increased ALT) 19; active NASH with high necroinflammatory activities 20. Similarly, in the American Association for the Study of Liver Diseases and Asian Pacific Association for the Study of the Liver guidelines, a pharmacological approach is recommended only for patients with NASH and fibrosis 8. In the National Institute for Health and Care Excellence guidance, just people with an advanced liver fibrosis (enhanced liver fibrosis [ELF] test > 10.51) are proposed for drug treatment 21. In the Italian Association for the Study of the Liver position paper, drug therapy is suggested for patients who are at high risk for disease progression22.
All guidelines acknowledge that any medicines prescribed explicitly for nonalcoholic fatty liver disease should be considered as an off-label treatment and that the decision should be discussed with the patient, carefully balancing the benefits and the safety. However, there are wide disagreement among the guidelines with regard to possibly helpful drugs.
- Metformin: Due to the evidence of its limited efficacy in improving the histological features of nonalcoholic fatty liver disease 23, metformin is not recommended by any guidelines to specifically treat NAFLD 15.
- Pioglitazone: Pioglitazone, a thiazolidinedione, is a peroxisome proliferator-activated receptor (PPAR) gamma agonist with insulin-sensitising effects. Treatment with pioglitazone improves insulin sensitivity, aminotransferases, steatosis, inflammation, and ballooning in patients with nonalcoholic steatohepatitis (NASH) and prediabetes or type 2 diabetes 24. The PIVENS trial (a large multicenter randomized control trial) compared low dose pioglitazone (30 mg/d) vs vitamin E (800 UI/d) vs placebo for two years in patients without overt diabetes 25. Pioglitazone improved all histological features (except for fibrosis) and achieved resolution of NASH more often than placebo 25. The histological benefit occurred together with ALT improvement and partial correction of insulin resistance. The main side effects of glitazones are weight gain 26 and bone fractures in women 27. The use of pioglitazone for the treatment of NAFLD is endorsed both by the National Institute for Health and Care Excellence and American Association for the Study of Liver Diseases guidelines, with significant limitations. According to the National Institute for Health and Care Excellence, pioglitazone should be prescribed only in second and third level centers, after a careful evaluation 21. Whereas the American Association for the Study of Liver Diseases, pioglitazone is reserved for patients with biopsy-proven NASH 8. The European Association for the Study of the Liver guidelines are more cautious, generically suggesting to consider pioglitazone for the treatment of diabetes in patients with a concurrent NAFLD 18. Even the Asia-Pacific and the Italian guidelines acknowledge the potential benefits of pioglitazone, however, suggest that more evidence should be available before a firm recommendation can be made 28, 22.
- Vitamin E: Vitamin E is an anti-oxidant and has been investigated to treat nonalcoholic steatohepatitis (NASH). In the PIVENS trial, vitamin E at a dose of 800 IU/d of α-tocopherol for 96 wk was associated with a decrease in serum aminotransferases and histological improvement in steatosis, inflammation, and ballooning and resolution of steatohepatitis in adults with NASH 25. Long-term safety of vitamin E is under dispute, with two different meta-analyses leading to conflicting results when analysing the all-cause mortality in patients treated with t doses of > 800 IU/d 29, 27. Similarly to pioglitazone, vitamin E is recommended by the National Institute for Health and Care Excellence and American Association for the Study of Liver Diseases guidelines (limited to biopsy-proven NASH in the latter case) 21, 8. Italian Association for the Study of the Liver and European Association for the Study of the Liver guidelines call for more evidence before any recommendation, while Asia-Pacific guidelines advice against the use of vitamin E which is described as not beneficial by the current evidence 28.
- Glucagon-like peptide-1 (GLP-1) analogues: Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist. Glucagon is an important hormone in the regulation of energy handling in your body. Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of drugs that improve control of your blood sugar, cause weight loss and improve blood lipids. They also improve cardiovascular outcomes 30. Therefore, they are approved for the treatment of diabetes and obesity. Liraglutide is one of these GLP-1 receptor agonists and has been tested in a randomized, placebo-controlled trial consisting of 52 patients with biopsy-proven NASH at a daily dose of 1.8 mg in 1-year study 31. NASH resolved significantly more frequently in liraglutide-treated patients than placebo-treated patients. Treatment with liraglutide also led to a trend in improvement of fibrosis stage. The same holds true for semaglutide, which was already shown to improve liver blood tests in patients with type 2 diabetes and obesity 32. Semaglutide was tested at several dose regimens for a treatment period of 1.5 years. NASH resolved significantly more frequently in patients treated with the higher doses of semaglutide than in patients that received placebo 33. Fibrosis also tended to improve, but this result was not strong enough to be considered as a positive endpoint of the study. However, both the American Association for the Study of Liver Diseases and National Institute for Health and Care Excellence recommendations state that there is still too few evidence to support the use of GLP-1 analogues to specifically treat liver disease in patients with NAFLD 21, 8. The remaining guidelines also agree on this point, however also state that further evidence are needed to prove the efficacy of these drugs. In particular, the Asian Pacific Association for the Study of the Liver guidelines consider some more elements in their recommendations. On the one hand, glucagon-like peptide-1 (GLP-1) agonists appeared to reduce glycated hemoglobin more efficiently in Asian patients with type 2 diabetes mellitus 34. On the other hand, there has been no study on Asian NASH patients, even if the pharmacokinetics of GLP-1 agonists do not appear to differ between Asian and non-Asian patients according to preliminary evidence 35. You can consider using these drugs if you meet the diagnosis for which these drugs are approved by the regulatory authorities. For example, if you are living with type 2 diabetes, it could be worthwhile to consider including pioglitazone or glucagon-like peptide-1 (GLP-1) receptor agonists in the treatment of your type 2 diabetes, as they are also beneficial for your liver. This needs to be discussed with the doctors that treat your diabetes.
- Statins: Historically, the use of statins in patients with chronic liver diseases has been considered as potentially troublesome due to the risk of hepatotoxicity. At the same time, a considerable portion of NAFLD patients usually receives statins because of their multiple cardiovascular risk factors. Consequently, the primary concern of the guidelines is the safety of statins. In this regard, a recent review underlined the safety of statin and their efficacy in reducing the associated cardiovascular morbidity in patients with NAFLD, including those with slightly elevated alanine transaminases (up to 3 × reference upper limit) 36. All of the guidelines agree about the safety of prescribing statins (or continuing an ongoing statin therapy) in patients with NAFLD, even with compensated cirrhosis. However, routine prescription of a statin is not recommended in patients with decompensated cirrhosis and acute liver failure 37.
- Silymarin: Silymarinis a complex mixture of six major flavonolignans (silybins A and B, isosilybins A and B, silychristin, and silydianin), as well as other minor polyphenolic compounds 38. In a randomized, double-blinded, placebo-controlled study on patients with biopsy-proven NASH, silymarin dosage of 700 mg three times daily for 48 wk resulted in a significantly higher percentage of fibrosis reduction compared with placebo (22.4% vs 6.0%) 39. The dosage was safe and well tolerated 39. Silymarin is mentioned as a potentially useful treatment for NASH in Asia-Pacific guidelines only. However, optimal dose and duration still require further studies before a full recommendation 28.
For patients with advanced disease and cirrhosis, liver transplantation might have to be considered.
What food should I eat for healthy liver function?
Eating a healthy diet and being a healthy weight can often help avoid damage to your liver.
Eating the right types of food helps you and your liver stay healthy. So, try to eat a mix of:
- Milk, yogurt and cheese
- Meat and fish (fresh or tinned low salt) and/or eggs, tofu, nuts and seeds
- Fruits (fresh or tinned low sugar)
- Vegetables, beans and legumes (fresh or tinned low salt)
- Grains (like breads, cereals, rice and pasta)
- And drinking lots of water.
Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease (NAFLD) now called metabolic dysfunction-associated steatotic liver disease (MASLD) is a liver disease in which too much fat builds up in your liver and this buildup of fat is not caused by heavy alcohol use 40, 41. It is normal for your liver to contain some fat. However, if more than 5% to 10% percent of your liver’s weight is fat, then it is called a fatty liver (steatosis). Non-alcoholic fatty liver disease (NAFLD) is the most common form of liver disease in the world, with the highest rates being reported in South America and the Middle East, followed by Asia, the USA, and Europe; NAFLD is less common in Africa 42, 43, 44, 45. This study found that approximately 900 million people suffered from NAFLD in 2017 43. When heavy alcohol use causes fat to build up in your liver, this condition is called alcoholic fatty liver disease (AFLD). NAFLD is a growing cause of end-stage liver disease and has been recognized as a cause of liver cancer (hepatocellular cancer [HCC]), even in the absence of underlying cirrhosis 46.
Non-alcoholic fatty liver disease (NAFLD) is seen most often in people who are overweight or obese. NAFLD is becoming more common, especially in North African and Middle Eastern countries (including Qatar, Libya and Kuwait) and Western nations as the number of people with obesity and type 2 diabetes rises 47, 48. Global reports relating to the epidemiology of NAFLD have estimated a global prevalence of NAFLD between 25% and 35%, with Europe as high as 30%, 35% in South American countries and 35% in North America 49, 50, 51, 52, 49, 53.
Well-established risk factors for NAFLD include obesity, type 2 diabetes, an unhealthy diet (eg, high intake of red meat and processed meat) and physical inactivity 54, 55, 56, 57, 58. Of these, an unhealthy lifestyle is deemed to be the most important contributor to NAFLD 59. Key lifestyle factors include an increased intake of glucose, fructose, and saturated fat, induced hepatic de novo lipogenesis, subclinical inflammation in the adipose tissue and liver, and insulin resistance in adipose tissue, the liver, and skeletal muscle 60. These lifestyle factors are also accompanied by an increased risk of type 2 diabetes 60.
Non-alcoholic fatty liver disease (NAFLD) ranges in severity from nonalcoholic fatty liver (NAFL) to a more severe form of the disease called nonalcoholic steatohepatitis (NASH) 41.
- Nonalcoholic fatty liver (NAFL). Nonalcoholic fatty liver (NAFL) is a form of NAFLD in which you have fat in your liver but little or no inflammation or liver damage. Nonalcoholic fatty liver (NAFL) typically does not progress to cause liver damage or complications. However, nonalcoholic fatty liver (NAFL) can cause pain from enlargement of the liver and have a higher risk for other health problems 61.
- Nonalcoholic steatohepatitis (NASH). Nonalcoholic steatohepatitis (NASH) is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH can cause fibrosis, or scarring, of the liver. NASH may lead to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer. Furthermore, people with NASH have an increased chance of dying from liver-related causes 62. It is hard to tell apart NAFLD from NASH without a clinical evaluation and testing.
Scientists are not sure why some people with NAFLD have NASH while others have nonalcoholic fatty liver (NAFL) 63. People typically develop one type of NAFLD or the other, although sometimes people with one form are later diagnosed with the other form of NAFLD. The majority of people with NAFLD have nonalcoholic fatty liver (NAFL). Only a small number of people with NAFLD have NASH. Experts guess that about 10% to 24% of Americans have nonalcoholic fatty liver disease (NAFLD) and about 1.5% to 6.5% have nonalcoholic steatohepatitis (NASH) 61, 64.
Non-alcoholic fatty liver disease (NAFLD) is more common in people who have certain diseases and conditions, including obesity, and conditions that may be related to obesity, such as type 2 diabetes 63. Studies suggest that one-third to two-thirds of people with type 2 diabetes have NAFLD 61. Research also suggests that NAFLD is present in up to 75% of people who are overweight and in more than 90% of people who have severe obesity 65, 66.
NAFLD can affect people of any age, including children. Research suggests that close to 10% of U.S. children ages 2 to 19 have NAFLD 67. However, people are more likely to develop NAFLD as they age.
While NAFLD occurs in people of all races and ethnicities, it is most common among Hispanic individuals, followed by non-Hispanic whites and Asian Americans, including those of East Asian and South Asian descent 62, 68. NAFLD is less common among non-Hispanic Blacks 62. On average, Asian Americans with NAFLD have a lower body mass index (BMI) than non-Hispanic whites with NAFLD 68. Experts think that genes may help explain some of the racial and ethnic differences in NAFLD 63.
Non-alcoholic fatty liver disease (NAFLD) usually is a silent disease with few or no symptoms 69. When it does, they may include:
- Fatigue.
- Not feeling well, or malaise.
- Pain or discomfort in the upper right belly area.
People with non-alcoholic fatty liver disease (NAFLD) have a higher risk for certain health problems, including:
- Cardiovascular disease, which is the most common cause of death in people who have NAFLD 62
- Type 2 diabetes
- Metabolic syndrome
- Conditions that may be part of metabolic syndrome, such as high blood pressure and abnormal levels of fats—cholesterol and triglycerides—in the blood.
Early-stage NAFLD does not usually cause any harm, but it can lead to serious liver damage, including cirrhosis, if it gets worse.
Having high levels of fat in your liver is also associated with an increased risk of serious health problems, such as type 2 diabetes, high blood pressure and kidney disease.
If you already have diabetes, NAFLD increases your chance of developing heart problems.
If detected and managed at an early stage, it’s possible to stop NAFLD getting worse and reduce the amount of fat in your liver.
Doctors recommend weight loss, done through a combination of calorie reduction, exercise, and healthy eating, to treat nonalcoholic fatty liver disease (NAFLD) 70, 71, 72. Weight loss can reduce fat, inflammation, and fibrosis or scarring in your liver 73.
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve nonalcoholic fatty liver disease (NAFLD). Losing at least 3% to 5% of your body weight can reduce fat in the liver 74, 62. You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis 75, 72, 76, 62. Physical activity alone, even without weight loss, is also beneficial.
The best way to lose weight is done by:
- Reducing the number of calories you eat. Keeping track of the calories you consume every day and employing portion control can help.
- Eating a healthy diet that’s rich in fruits and vegetables, whole grains and low in saturated fats. Limit animal-based foods, like red meat which is high in saturated fats, and eat more plant-based foods like beans, legumes, and nuts. Use good fats like olive oil. This is the basis for the Mediterranean diet – which isn’t a diet in the traditional sense, but a healthy way of eating inspired by the eating habits of people living in the Mediterranean area and is often recommended by doctors as a way to reduce some of the risk factors associated with fatty liver disease.
- Limiting the amount of salt and sugar in your diet, particularly sugar-sweetened beverages, like soda, juices, sports drinks, and sweetened tea. High consumption of fructose, one of the main sweeteners in these beverages, increases your odds of developing obesity, type 2 diabetes, metabolic syndrome, and NAFLD.
- Limit your intake of saturated fats, which are found in meat, poultry skin, butter, shortening, milk and dairy products (except fat-free versions). Replace them with monounsaturated fats (olive, canola, and peanut oils) and polyunsaturated fats (corn, safflower, soybean oils, and many types of nuts). Particularly helpful in reducing heart disease are omega-3 fatty acids, a type of polyunsaturated fat found in oily fish such as salmon, flaxseed oil, and walnuts. Healthy eating combined with exercise – and taking cholesterol-lowering medications if prescribed by your doctor – will help keep your cholesterol and triglyceride levels where they need to be.
- Exercise and be more active – exercise is important for many reasons; it can help with weight control, boost your immune system, and alleviate stress and depression. Aim for at least 150 minutes of exercise a week. Depending on how much weight you’re trying to lose, you may need to up that amount. Getting exercise doesn’t mean you have to go to a gym – walking, gardening, and even housework counts. However, if you don’t already exercise, get your doctor’s okay first and build slowly. The goal is to participate in exercise of a moderate intensity (examples include light jogging, biking, swimming or playing a sport that boosts your heart rate and results in sweating).
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
If you’ve tried to lose weight in the past without success, talk to your dietitian about getting help. You may also be a candidate for a medically-supervised weight loss program that employs medication along with diet and exercise. Alternatively, there are weight-loss (bariatric) surgical procedures and endoscopic therapies that work by either physically limiting the amount of food your stomach can hold, or reducing the amount of nutrients and calories your body absorbs. Talk to your doctor about which option may be best for you.
Figure 2. Nonalcoholic fatty liver disease (NAFLD)
Figure 3. Non-alcoholic fatty liver disease progression
Footnotes: Non-alcoholic fatty liver disease (NAFLD) encompasses a range of liver damage, from simple accumulation of fat in liver cells, named steatosis, to more severe forms of the diseases such as nonalcoholic steatohepatitis (NASH), involving inflammation which can lead to fibrosis and cirrhosis. In the “multiple-hit” theory of progression, the first cause or “first-hit” in NAFLD is insulin resistance, obesity, type 2 diabetes, and metabolic syndrome. As the first hit occurs, free fatty acids are stored in the liver as triglycerides, resulting in simple steatosis. Disease progresses when multiple factors, or “multi-hits”, such as oxidative stress, inflammatory mediators, apoptosis, and mitochondrial dysfunction cause liver damage.
[Source 70 ]Non-alcoholic fatty liver disease causes
Scientists don’t know exactly why fat builds up in some livers and not others. They also don’t fully understand why some fatty livers turn into non-alcoholic fatty liver disease (NAFLD).
Non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) are both linked to the following 77, 78, 79, 80, 81:
- Genetics. Researchers have found that certain genes may make you more likely to develop NAFLD. These genes may help explain why NAFLD is more common in certain racial and ethnic groups. Studies have identified many genetic changes that may be associated with the development of NAFLD and NASH. Among these is a particular variation in the PNPLA3 gene 82. The PNPLA3 gene provides instructions for making a protein called adiponutrin, which is found in fat cells (adipocytes) and liver cells (hepatocytes). The function of this protein is not well understood, but it is thought to help regulate the production and breakdown of fats (lipogenesis and lipolysis) and the development of adipocytes. Studies indicate that the activity (expression) of the PNPLA3 gene decreases during periods without food (fasting) and increases after eating, suggesting that the amount of adiponutrin protein produced is regulated as needed to help process and store fats in the diet. The PNPLA3 gene variation associated with NAFLD is thought to lead to increased production and decreased breakdown of fats in the liver. Research is ongoing to determine how this and other genetic changes contribute to the development of NAFLD and its complications.
- Overweight or obesity.
- Insulin resistance, which happens when your cells don’t take up sugar in response to the hormone insulin.
- Type 2 diabetes, sometimes called high blood sugar or hyperglycemia.
- High levels of fats (abnormal levels of cholesterol—high total cholesterol, high LDL cholesterol, or low HDL cholesterol), especially triglycerides, in the blood.
These combined health problems may contribute to a fatty liver. However, some people get NAFLD even if they do not have any risk factors.
Risk factors for developing non-alcoholic fatty liver disease
Many diseases and health problems can increase your risk of non-alcoholic fatty liver disease (NAFLD), including:
- Family history of fatty liver disease or obesity.
- Growth hormone deficiency, which means the body doesn’t make enough hormones to grow.
- High cholesterol.
- High levels of triglycerides in the blood.
- Insulin resistance.
- Metabolic syndrome. Metabolic syndrome is a group of traits and medical conditions linked to overweight and obesity. Doctors define metabolic syndrome as the presence of any three of the following:
- large waist size
- high levels of triglycerides in your blood
- low levels of HDL cholesterol in your blood
- high blood pressure
- higher than normal blood glucose levels or a diagnosis of type 2 diabetes
- Obesity, especially when fat is centered in the waist.
- Polycystic ovary syndrome (PCOS).
- Obstructive sleep apnea.
- Type 2 diabetes.
- Underactive thyroid, also called hypothyroidism.
- Underactive pituitary gland, or hypopituitarism.
If you have risks for NAFLD and also drink alcohol excessively, you could have both NAFLD and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Nonalcoholic steatohepatitis (NASH) is more likely in these groups:
- People older than 50.
- People with certain genetic risk factors.
- People with obesity.
- People with diabetes or high blood sugar.
- People with symptoms of metabolic syndrome, such as high blood pressure, high triglycerides and a large waist size.
Having more of these health conditions increases your chances of developing NASH. Losing weight may cause nonalcoholic steatohepatitis (NASH) to switch to nonalcoholic fatty liver (NAFL) and regaining weight may cause nonalcoholic fatty liver (NAFL) to switch to nonalcoholic steatohepatitis (NASH).
Non-alcoholic fatty liver disease prevention
You may be able to prevent non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) by being physically active regularly, eating a healthy diet, limiting your portion sizes, and maintaining a healthy weight.
To reduce your risk of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH):
- Eat a healthy diet. Eat a healthy diet that’s rich in fruits, vegetables, whole grains and healthy fats.
- Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks like soda, sports drinks, juices and sweet tea. Drinking alcohol can damage your liver and should be avoided or minimized.
- Keep a healthy weight. If you are overweight or obese, work with your health care team to gradually lose weight. If you are a healthy weight, work to keep it by eating a healthy diet and exercising.
- Exercise. Be active most days of the week. Get an OK from your health care team first if you haven’t been exercising regularly.
Non-alcoholic fatty liver disease stages
Staging and grading systems have been developed to characterize the histological changes in non-alcoholic fatty liver disease (NAFLD), mainly as a tool for clinical research.
Non-alcoholic fatty liver disease (NAFLD) Grades 83, 84, 85, 86, 87:
- Grade 0 (Normal) is defined as a normal liver containing fat in less than 5% of liver cells (hepatocytes)
- Grade 1 (Mild): Fatty liver (steatosis) up to 66%, occasional ballooning in zone 3, scattered polymorphs with or without lymphocytes, mild or no portal inflammation
- Grade 2 (Moderate): Any degree of steatosis, obvious ballooning predominantly in zone 3, intralobular inflammation with polymorphs and chronic inflammation, and mild to moderate portal inflammation
- Grade 3 (Severe): Panacinar steatosis, ballooning, and obvious disarray predominantly in zone 3, intralobular inflammation with scattered polymorphs with or without mild chronic and mild to moderate portal inflammation
Non-alcoholic fatty liver disease (NAFLD) Stages 83, 84, 85, 86, 87, 88, 89, 90:
- Stage 0: No fibrosis
- Stage 1: Zone 3 perisinusoidal fibrosis only
- Stage 2: Zone 3 perisinusoidal and periportal fibrosis
- Stage 3: Bridging fibrosis
- Stage 4: Cirrhosis
Progression of the fibrosis stage to a cirrhotic scarred liver can vary between individuals, with cirrhosis occurring up to 15 to 20 years after initial diagnosis 89, 91. The median survival rate for patients with compensated cirrhosis is approximately 9 to 12 years, however, patients with decompensated cirrhosis have a significantly lower median survival rate of approximately 2 years 92. Patients in the compensated stage are frequently asymptomatic, and often remain undiagnosed 92. Therefore, early detection of cirrhotic patients who are still in the compensated stage is crucial, as early diagnosis could prevent or slow down disease progression 70.
Non-alcoholic fatty liver disease symptoms
Often, there are no symptoms of non-alcoholic fatty liver disease (NAFLD) in its early stages. It is more common for symptoms to develop once significant damage to the liver has occurred. Some symptoms of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) may include:
- Discomfort or pain in the abdomen (belly area)
- Fatigue (feeling very tired)
- Irritability
- Headaches
- Difficulty concentrating
- Depression and anxiety
- Changes in skin color near joints and the back of the neck/upper back
If cirrhosis develops, the following symptoms may be present:
- Jaundice (yellowing of the skin and whites of the eyes)
- Itchy skin
- Swelling of the lower stomach
- Bruising easily
- Dark urine
Non-alcoholic fatty liver disease complications
Severe liver scarring, or cirrhosis, is the main complication of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). Cirrhosis happens because of liver injury, such as the damage caused by inflammation in NASH. As the liver tries to stop inflammation, it creates areas of scarring, also called fibrosis. With ongoing inflammation, fibrosis spreads and takes up more liver tissue.
If nothing is done to stop the scarring, cirrhosis can lead to:
- Fluid buildup in the stomach area, called ascites.
- Swollen veins in your esophagus, or esophageal varices, which can rupture and bleed.
- Confusion, sleepiness and slurred speech, also called hepatic encephalopathy.
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- Liver cancer.
- End-stage liver failure, which means the liver has stopped working.
Non-alcoholic fatty liver disease diagnosis
Doctors use your medical history, a physical exam, and tests to diagnose nonalcoholic fatty liver disease (NAFLD) including nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). Because nonalcoholic fatty liver disease (NAFLD) typically causes no symptoms, it is often found when tests done for other reasons point to a liver problem. For example, your blood work may show high levels of liver enzymes, or an ultrasound of your abdomen might reveal that your liver looks enlarged, which can lead to more testing. Doctors use blood tests, imaging tests, and sometimes liver biopsy to diagnose NAFLD and to tell the difference between nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH).
Medical history
Your doctor will ask if you have a history of health conditions or diseases that make you more likely to develop NAFLD, such as:
- overweight or obesity
- insulin resistance or type 2 diabetes
- high levels of triglycerides or abnormal levels of cholesterol in your blood
- metabolic syndrome
Your doctor will ask about your diet and lifestyle factors that may make you more likely to develop liver disease or fat in your liver.
- What medicines you take to determine whether a medicine might be causing your fatty liver.
- Your doctor will ask about your alcohol intake to find out whether fat in your liver is a sign of alcohol-associated liver disease or NAFLD. Medical tests cannot show whether alcohol is the cause of fat in the liver, so it’s important to be honest with your doctor.
- What your diet is like (eating a diet high in sugar, or drinking sugary beverages), your level of physical activity, and other lifestyle factors that can contribute to the likelihood of developing NAFLD.
Physical exam
During a physical exam, a doctor usually examines your body and checks your weight and height to calculate your body mass index (BMI). Your BMI estimates how much you should weigh based on your height. Most experts say that a BMI greater than 30 (obesity) is unhealthy. If you want to figure out your BMI on your own, there are many websites that calculate it for you when you enter your height and weight. If you have more or less muscle than is normal, your BMI may not be a perfect measure of how much body fat you have. Your doctor may also take your waist circumference and waist-to-hip ratio into consideration.
Your doctor will look for signs of nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH), such as:
- an enlarged liver
- signs of insulin resistance, such as darkened skin patches over your knuckles, elbows, and knees
- signs of cirrhosis, such as an enlarged spleen, ascites, spiderlike blood vessels on your skin, yellowing of your skin and whites of your eyes (jaundice) and muscle loss
Blood tests
Your doctor may take a blood sample from you and send the sample to a lab.
Your blood tests may include:
- Complete blood count.
- Iron studies, which show how much iron is in your blood and other cells.
- Liver enzyme and liver function tests.
- Tests for chronic viral hepatitis (hepatitis A, hepatitis C and others).
- Celiac disease screening test.
- Fasting blood sugar.
- Hemoglobin A1C, which shows how stable your blood sugar is.
- Lipid profile, which measures blood fats, such as cholesterol and triglycerides.
Your doctor may suspect you have NAFLD if your blood test shows increased levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST). The cells in your liver contain proteins called enzymes, which are chemicals that help the liver do its work. When liver cells are damaged or destroyed, the enzymes in the cells leak out into the blood where they can be measured by blood tests. Liver enzyme testing usually checks the blood for two main enzymes 75, 93:
- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
If your liver is damaged due to inflammation, the level of these enzymes may be higher than normal. However, ALT and AST levels do not tell you how much scarring (fibrosis) may be present in your liver or predict how much liver damage will develop. In some people with NAFLD these liver enzymes may be normal as well.
Fibrosis assessment tests
These blood tests result in a score that estimates your level of liver scarring or fibrosis. They include:
- AST-to-Platelet Ratio Index (APRI) score
- Fibrosis-4 (Fib-4) score. The fibrosis-4 scoring system uses a patients age, platelet count, AST (aspartate aminotransferase) and ALT (alanine aminotransferase) to determine a liver fibrosis score and can help to predict advanced fibrosis.
These scores can help doctors identify or rule out advanced liver fibrosis, or scarring.
Your doctor may perform additional blood tests to find out if you have other health conditions that may increase your liver enzyme levels.
Imaging tests
Your doctor may order tests that take images, or pictures, of your liver to help make the diagnosis of liver disease. Different types of images can be obtained by using various types of equipment. However, these tests can’t show inflammation or fibrosis, so your doctor can’t use these tests to find out whether you have nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). If you have cirrhosis, routine imaging tests may show nodules, or lumps, in your liver.
Your doctor may use the following imaging tests to help diagnose NAFLD:
- Abdominal ultrasound, which uses a device called a transducer that bounces safe, painless sound waves off your organs to create an image of their structure. Abdominal ultrasoundis often the first test used when liver disease is suspected.
- Computed tomography (CT) scan, which uses a combination of x-rays and computer technology to create images of your liver.
- Magnetic resonance imaging (MRI), which uses radio waves and magnets to produce detailed images of organs and soft tissues without using x-rays.
- Transient elastography, a newer type of ultrasound that measures the stiffness of your liver to determine if you have advanced liver fibrosis. Liver stiffness is a sign of fibrosis or scarring. Commonly used types of elastography are:
- Vibration-controlled transient elastography, a special type of ultrasound
- Sheer wave elastography, another type of ultrasound to detect increased liver stiffness
- Magnetic resonance elastography (MRE), is a newer, noninvasive test that combines features of ultrasound and MRI imaging to create a visual map showing gradients of stiffness throughout the liver. MRE has been shown to be a more reliable measure of liver stiffness in severely obese patients.
Liver biopsy
If other tests show signs of more-advanced liver disease or nonalcoholic steatohepatitis (NASH), or if your test results are unclear, your doctor may suggest a liver biopsy. Liver biopsy is a procedure to remove a small piece of tissue from your liver. It is usually done using a needle through the abdominal wall. The tissue sample is looked at in a lab for signs of inflammation and scarring. Liver biopsy is the only test that can prove a diagnosis of NASH and clearly shows the amount of liver damage.
Liver biopsy can show fibrosis at earlier stages than elastography can. However, doctors don’t recommend liver biopsy for everyone with suspected NAFLD. Your doctor may recommend a liver biopsy if you are more likely to have nonalcoholic steatohepatitis (NASH) with advanced fibrosis or if your other tests show signs of advanced liver disease or cirrhosis. In some cases, doctors may recommend a liver biopsy to rule out other liver diseases.
During a liver biopsy, a doctor using a needle that is passed through the abdominal wall and into the liver will take small pieces of tissue from your liver. A pathologist will examine the tissue under a microscope to look for signs of damage or disease.
A liver biopsy can be uncomfortable, and it does have risks that your doctor will go over with you in detail.
Non-alcoholic fatty liver disease treatments
Doctors recommend weight loss, done through a combination of calorie reduction, exercise, and healthy eating, to treat nonalcoholic fatty liver disease (NAFLD) 70, 71, 72, 73. Weight loss can reduce fat, inflammation, and fibrosis or scarring in your liver 73.
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve nonalcoholic fatty liver disease (NAFLD). Losing at least 3% to 5% of your body weight can reduce fat in the liver 74, 62. You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis 75, 72, 76, 62. Physical activity alone, even without weight loss, is also beneficial.
The best way to lose weight is done by:
- Reducing the number of calories you eat. Keeping track of the calories you consume every day and employing portion control can help.
- Eating a healthy diet that’s rich in fruits and vegetables, whole grains and low in saturated fats. Limit animal-based foods, like red meat which is high in saturated fats, and eat more plant-based foods like beans, legumes, and nuts. Use good fats like olive oil. This is the basis for the Mediterranean diet – which isn’t a diet in the traditional sense, but a healthy way of eating inspired by the eating habits of people living in the Mediterranean area and is often recommended by doctors as a way to reduce some of the risk factors associated with fatty liver disease.
- Limiting the amount of salt and sugar in your diet, particularly sugar-sweetened beverages, like soda, juices, sports drinks, and sweetened tea. High consumption of fructose, one of the main sweeteners in these beverages, increases your odds of developing obesity, type 2 diabetes, metabolic syndrome, and NAFLD.
- Limit your intake of saturated fats, which are found in meat, poultry skin, butter, shortening, milk and dairy products (except fat-free versions). Replace them with monounsaturated fats (olive, canola, and peanut oils) and polyunsaturated fats (corn, safflower, soybean oils, and many types of nuts). Particularly helpful in reducing heart disease are omega-3 fatty acids, a type of polyunsaturated fat found in oily fish such as salmon, flaxseed oil, and walnuts. Healthy eating combined with exercise – and taking cholesterol-lowering medications if prescribed by your doctor – will help keep your cholesterol and triglyceride levels where they need to be.
- Exercise and be more active – exercise is important for many reasons; it can help with weight control, boost your immune system, and alleviate stress and depression. Aim for at least 150 minutes of exercise a week. Depending on how much weight you’re trying to lose, you may need to up that amount. Getting exercise doesn’t mean you have to go to a gym – walking, gardening, and even housework counts. However, if you don’t already exercise, get your doctor’s okay first and build slowly. The goal is to participate in exercise of a moderate intensity (examples include light jogging, biking, swimming or playing a sport that boosts your heart rate and results in sweating).
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
If you’ve tried to lose weight in the past without success, talk to your dietitian about getting help. You may also be a candidate for a medically-supervised weight loss program that employs medication along with diet and exercise. Alternatively, there are weight-loss (bariatric) surgical procedures and endoscopic therapies that work by either physically limiting the amount of food your stomach can hold, or reducing the amount of nutrients and calories your body absorbs. Talk to your doctor about which option may be best for you.
Patients with NASH are to be followed by liver specialists or gastroenterologists. NASH with cirrhosis requires hepatocellular carcinoma (HCC) surveillance with an ultrasound every six months 77.
Non-alcoholic fatty liver disease diet
If you have NAFLD, your doctor may suggest changes to your diet such as:
- Limiting your intake of fats, which are high in calories and increase your chance of developing obesity.
- Replacing saturated fats and trans fats in your diet with unsaturated fats, especially omega-3 fatty acids, which may reduce your chance of heart disease if you have NAFLD.
- Eating more low-glycemic (low GI) index foods such as most fruits, vegetables, and whole grains. These foods affect your blood glucose less than high-glycemic index foods, such as white bread, white rice, and potatoes.
- Avoiding foods and drinks that contain large amounts of simple sugars, especially fructose. Fructose is found in sweetened soft drinks, sports drinks, sweetened tea, and juices. Table sugar, called sucrose, is rapidly changed to glucose and fructose during digestion and is therefore a major source of fructose.
If you have NAFLD, you should minimize alcohol use, which can further damage your liver.
Evidence has suggested that the ketogenic diet (diet with very low in carbohydrate and very high in fat = 75-80% fat, 10-15% protein and ≤ 5% carbohydrate) is an effective treatment for NAFLD 95, 73, 96, 70. Ketogenesis is a metabolic process resulting in the production of ketone bodies, namely acetoacetate, beta-hydroxybutyrate and acetone, which act as alternative energy sources 97, 95. The ketogenic diet has been shown to change hepatic mitochondrial fluxes and redox state as well as significantly reducing liver fat content and liver insulin resistance 98. These changes were found to be accompanied by an increase in the net hydrolysis of liver triglycerides, a decrease in endogenous glucose production, and lower serum insulin levels 98. Beta-hydroxybutyrate has also been shown to interact with inflammasomes 99, 100 and neutralize reactive oxygen species (ROS) 101, leading to a reduction in inflammatory cytokines and oxidative damage via its antioxidant capacity. These findings suggest a ketogenic diet can contribute to the reversal of NAFLD through improvement of insulin resistance and cellular redox function 70.
Non-alcoholic fatty liver disease medication
No medicines have been approved to treat nonalcoholic fatty liver disease (NAFLD) 102, 77, 70.
Weight loss surgery
Weight loss surgery also called bariatric surgery been shown to be an effective treatment for nonalcoholic fatty liver disease (NAFLD) by improving overall liver health via facilitating weight loss, improving insulin sensitivity, and subsiding inflammation 103, 104. Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy are the most prevalent weight loss surgical procedures, which lead to significant weight loss and metabolic health improvements 105.
Several research studies have investigated the impact of weight loss surgery in NAFLD and have shown positive results. Studies have indicated that weight loss surgery resulted in significant improvements in liver enzymes and histology, with a decrease in liver fat and fibrosis. Results from two meta-analyses have shown that treatment of NAFLD using weight loss surgery resulted in a biopsy-confirmed resolution of steatosis (56%-66%), inflammation (45%-50%), ballooning degeneration (49%-76%), and fibrosis (25%-40%), as well as showing a decrease in NAS scoring 105, 106, 107. Weight loss surgery has therefore proven to be effective in ameliorating NAFLD, however, it is important to clarify which type of weight loss surgery is most effective. A study by Baldwin et al 108 compared Roux-en-Y gastric bypass (RYGB) and laparoscopic sleeve gastrectomy against its effectiveness at improving AST and ALT concentration, NAS and NAFLD fibrosis score. Overall, both procedures reduce AST and ALT levels, however, laparoscopic sleeve gastrectomy showed slightly more favourable results 104. Another study has shown NAS scoring reduced significantly in patients who underwent both surgery types 12-mo after the surgery 104. Roux-en-Y gastric bypass patients had a more significantly decreased steatosis and superior improvement in plasma lipid profile 109. Furthermore, weight loss surgery has been demonstrated to lower the risk of liver-related complications and death in individuals with NAFLD. Weight loss surgery can therefore be considered as a promising treatment option for those with NAFLD who are overweight or obese.
Protect your liver
Don’t do things that put extra stress on your liver:
- Avoid drinking alcohol.
- Take medications and over-the-counter drugs only as instructed by your doctor.
- Be cautious about taking dietary supplements. Certain vitamins and minerals – like vitamins A, iron, and niacin – can be harmful to your liver in higher doses than necessary or prescribed.
Check with your doctor before trying any herbal remedies. Just because a product is called “natural,” does not mean it’s safe. - Get vaccinated for hepatitis A and hepatitis B. If you get hepatitis A or B, along with fatty liver, it’s more likely to lead to liver failure.
- Manage your diabetes. Follow your doctor’s advice to manage your diabetes. Take your medicines as told by your care team and watch your blood sugar closely.
- Lower your cholesterol and blood pressure. Improve your cholesterol levels and blood pressure if they are high. A healthy diet, exercise and medicines can help keep your cholesterol, triglycerides and blood pressure at healthy levels.
Vitamin E, which is an antioxidant, in theory could help protect the liver by reducing or canceling out the damage caused by inflammation. But more research is needed. Some evidence suggests vitamin E supplements may be helpful for people with liver damage due to NAFLD and NASH who don’t have type 2 diabetes. Researchers in one study found that a daily dose of the natural form of vitamin E – the kind that comes from food sources and isn’t made in a laboratory – improved NASH in study participants overall by reducing fat and inflammation although not scarring. This medication is not for everyone and may have potential side effects as well. Vitamin E has been linked with a slightly increased risk of heart disease and prostate cancer. Discuss the potential benefits and side effects of vitamin E with your doctor.
Some studies suggest that coffee may benefit the liver by reducing the risk of liver diseases like NAFLD and lowering the chance of scarring. It’s not yet clear how coffee may prevent liver damage. But certain compounds in coffee are thought to lower inflammation and slow scar tissue growth. If you already drink coffee, these results may make you feel better about your morning cup. But if you don’t already drink coffee, this probably isn’t a good reason to start. Discuss the possible benefits of coffee with your health care team.
Non-alcoholic fatty liver disease prognosis
Patients with nonalcoholic fatty liver disease (NAFLD) have a decreased survival as compared to the general population 110. Individuals with non-alcoholic fatty liver disease (NAFLD) exhibit increased mortality rates when compared to the general population 111, 112, 77. People with non-alcoholic fatty liver disease (NAFLD) have a high risk of mortality from cardiovascular causes as these patients have metabolic derangements, followed by cancers and only then liver disease 110, 113, 111, 77. Cardiovascular causes of mortality are higher in non-alcoholic fatty liver disease (NAFLD) patients than liver causes 114, 115. NAFLD patients die 9 times more often from liver disease than the general population 113.
NAFLD is a slowly progressive disease 116, 117; simple faty liver (steatosis) is reversible and non-progressive, whereas nonalcoholic steatohepatitis (NASH) can progress to cirrhosis 115. The main risk factors for having advanced liver fibrosis are older age 118, 119, presence of obesity and central obesity 120, as well as type 2 diabetes 121 and hypertension 122. In a 13 year follow-up study by Ekstedt et al 117 the progression of cirrhosis were seen in 41% subjects. These subjects more often had a weight gain exceeding 5 kg, they were more insulin resistant and they exhibited more pronounced hepatic fatty infiltration at follow-up 117. Most NAFLD patients will develop diabetes or impaired glucose tolerance in the long term 117. A meta-analysis on 17 studies done by White et al. 123 showed that in cohorts of NAFLD or NASH with few or no cases of cirrhosis, the risk of developing liver cancer (hepatocellular carcinoma [HCC]) was minimal at 0 to 3% over a 20 year follow up, and in cohorts with NASH with cirrhosis, the risk was high at 2.4 to 12.8% after 3 to 12 years of follow up. In fact, NAFLD-associated cirrhosis accounts for 15%-30% of cases of hepatocellular carcinoma (HCC) 124. Patients with NAFLD can also progress to hepatocellular carcinoma (HCC), even without cirrhosis 125. Some cases of hepatocellular carcinoma (HCC) were reported in patients with simple steatosis, without NASH or fibrosis 126, 127.
Nonalcoholic steatohepatitis
Nonalcoholic steatohepatitis also called NASH or metabolic dysfunction associated steatohepatitis (MASH) is a fatty liver disease characterized by fatty changes with lobular hepatitis in people who drink little or no history of excessive alcohol consumption 128, 129, 130, 131, 132, 133. Jurgen Ludwig and colleagues in July 1980, at Mayo Clinic in Rochester, Minnesota, published the first article to identify non-alcoholic steatohepatitis (NASH) 128. At the time, steatohepatitis, which is a term to describe an inflammation of the liver that is accompanied by the abnormal accumulation of fat, was thought to be caused by excessive alcohol consumption. But the Mayo study described 20 people with fatty and inflamed livers — none of whom was a heavy alcohol drinker 128. Most had some liver scarring, also known as fibrosis 128. Three of the patients had cirrhosis, liver damage that results from such scarring. The study also noted that “most patients were moderately obese, and many had obesity-associated diseases” 128. Obesity and type 2 diabetes, two conditions associated with insulin resistance, are major risk factors for the development of NASH. Accumulating evidence suggests that the hyperinsulinemia associated with insulin resistance may be important in the pathogenesis of NASH.
Nonalcoholic steatohepatitis (NASH) is a severe form of nonalcoholic fatty liver disease (NAFLD) now called metabolic dysfunction-associated steatotic liver disease (MASLD) a term applied to a liver disease involving the presence of too much fat in the liver cells with or without inflammation and cellular injury that is not caused by alcohol 134, 135. Nonalcoholic steatohepatitis (NASH) is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH may lead to serious liver scarring, called cirrhosis. NASH may progress to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer.
Experts guess that about 10% to 24% of Americans have nonalcoholic fatty liver disease (NAFLD) and about 1.5% to 6.5% have nonalcoholic steatohepatitis (NASH) 61, 64.
A diagnosis of nonalcoholic steatohepatitis (NASH) is established by the presence of morphologic changes on liver biopsy similar to those seen in alcoholic hepatitis, including hepatocellular fat accumulation, evidence of lobular inflammation and cell injury, and in some cases, progressive fibrosis, but are found in the absence of alcohol abuse. Nonalcoholic steatohepatitis (NASH) is typically identified during the evaluation of elevated ALT (alanine aminotransferase) or AST (aspartate aminotransferase) levels after exclusion of viral, metabolic, and other causes of liver disease.
Nonalcoholic steatohepatitis (NASH) is increasingly recognized as a relatively common disorder occurring in 3% of adults that may progress to hepatic fibrosis, a precursor to cirrhosis in 15% to 40% of nonalcoholic steatohepatitis (NASH) patients 132. Cirrhosis is a condition in which your liver is scarred and permanently damaged. Scar tissue replaces healthy liver tissue and prevents your liver from working normally. Scar tissue also partly blocks the flow of blood through your liver. As cirrhosis gets worse, your liver begins to fail. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH).
If you have nonalcoholic steatohepatitis (NASH), you may have symptoms that could take years for them to develop. If liver damage from nonalcoholic steatohepatitis (NASH) leads to permanent scarring and hardening of your liver, this is called cirrhosis.
Symptoms from nonalcoholic steatohepatitis (NASH) may include:
- Severe tiredness
- Weakness
- Weight loss
- Yellowing of the skin or eyes (jaundice)
- Spiderlike blood vessels on your skin
- Long-lasting itchy skin.
Nonalcoholic steatohepatitis (NASH) that turns into cirrhosis could cause symptoms like fluid retention, abdominal swelling (ascites), shortness of breath, swelling of the legs, enlarged spleen, red palms, internal bleeding, muscle wasting, and confusion. People with cirrhosis over time may develop liver failure and need a liver transplant.
If you have nonalcoholic steatohepatitis (NASH), no medication is available to reverse the fat buildup in your liver. In some cases, the liver damage stops or even reverses itself. But in others, nonalcoholic steatohepatitis (NASH) continues to progress. If you have nonalcoholic steatohepatitis (NASH), it’s important to control any conditions that may contribute to fatty liver disease.
Nonalcoholic steatohepatitis (NASH) treatments and lifestyle changes may include:
- Losing weight
- Medication to reduce cholesterol or triglycerides
- Medication to reduce blood pressure
- Medication to control diabetes
- Limiting over-the-counter (OTC) drugs
- Avoiding alcohol
- Seeing a liver specialist
Some medications are being studied as possible treatments for nonalcoholic steatohepatitis (NASH). These include antioxidants like vitamin E. Scientists are also studying some new diabetes medications for nonalcoholic steatohepatitis (NASH) that may be given even if you don’t have diabetes. However, you should only take these medicines after consulting with a liver specialist.
Nonalcoholic steatohepatitis causes
Scientists don’t know exactly why fat builds up in some livers and not others. They also don’t fully understand why some fatty livers turn into nonalcoholic steatohepatitis (NASH).
Non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) are both linked to the following 77, 78, 79, 80, 81:
- Genetics. Researchers have found that certain genes may make you more likely to develop NAFLD. These genes may help explain why NAFLD is more common in certain racial and ethnic groups. Studies have identified many genetic changes that may be associated with the development of NAFLD and NASH. Among these is a particular variation in the PNPLA3 gene 82. The PNPLA3 gene provides instructions for making a protein called adiponutrin, which is found in fat cells (adipocytes) and liver cells (hepatocytes). The function of this protein is not well understood, but it is thought to help regulate the production and breakdown of fats (lipogenesis and lipolysis) and the development of adipocytes. Studies indicate that the activity (expression) of the PNPLA3 gene decreases during periods without food (fasting) and increases after eating, suggesting that the amount of adiponutrin protein produced is regulated as needed to help process and store fats in the diet. The PNPLA3 gene variation associated with NAFLD is thought to lead to increased production and decreased breakdown of fats in the liver. Research is ongoing to determine how this and other genetic changes contribute to the development of NAFLD and its complications.
- Overweight or obesity.
- Insulin resistance, which happens when your cells don’t take up sugar in response to the hormone insulin.
- Type 2 diabetes, sometimes called high blood sugar or hyperglycemia.
- High levels of fats (abnormal levels of cholesterol—high total cholesterol, high LDL cholesterol, or low HDL cholesterol), especially triglycerides, in the blood.
These combined health problems may contribute to a fatty liver. However, some people get NAFLD even if they do not have any risk factors.
Risk factors for developing nonalcoholic steatohepatitis
Many diseases and health problems can increase your risk of non-alcoholic fatty liver disease (NAFLD), including:
- Family history of fatty liver disease or obesity.
- Growth hormone deficiency, which means the body doesn’t make enough hormones to grow.
- High cholesterol.
- High levels of triglycerides in the blood.
- Insulin resistance.
- Metabolic syndrome. Metabolic syndrome is a group of traits and medical conditions linked to overweight and obesity. Doctors define metabolic syndrome as the presence of any three of the following:
- large waist size
- high levels of triglycerides in your blood
- low levels of HDL cholesterol in your blood
- high blood pressure
- higher than normal blood glucose levels or a diagnosis of type 2 diabetes
- Obesity, especially when fat is centered in the waist.
- Polycystic ovary syndrome (PCOS).
- Obstructive sleep apnea.
- Type 2 diabetes.
- Underactive thyroid, also called hypothyroidism.
- Underactive pituitary gland, or hypopituitarism.
If you have risks for NAFLD and also drink alcohol excessively, you could have both NAFLD and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Nonalcoholic steatohepatitis (NASH) is more likely in these groups:
- People older than 50.
- People with certain genetic risk factors.
- People with obesity.
- People with diabetes or high blood sugar.
- People with symptoms of metabolic syndrome, such as high blood pressure, high triglycerides and a large waist size.
Having more of these health conditions increases your chances of developing NASH. Losing weight may cause nonalcoholic steatohepatitis (NASH) to switch to nonalcoholic fatty liver (NAFL) and regaining weight may cause nonalcoholic fatty liver (NAFL) to switch to nonalcoholic steatohepatitis (NASH).
Nonalcoholic steatohepatitis prevention
You may be able to prevent non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) by being physically active regularly, eating a healthy diet, limiting your portion sizes, and maintaining a healthy weight.
To reduce your risk of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH):
- Eat a healthy diet. Eat a healthy diet that’s rich in fruits, vegetables, whole grains and healthy fats.
- Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks like soda, sports drinks, juices and sweet tea. Drinking alcohol can damage your liver and should be avoided or minimized.
- Keep a healthy weight. If you are overweight or obese, work with your health care team to gradually lose weight. If you are a healthy weight, work to keep it by eating a healthy diet and exercising.
- Exercise. Be active most days of the week. Get an OK from your health care team first if you haven’t been exercising regularly.
Nonalcoholic steatohepatitis symptoms
If you have nonalcoholic steatohepatitis (NASH), you may have symptoms that could take years for them to develop. If liver damage from nonalcoholic steatohepatitis (NASH) leads to permanent scarring and hardening of your liver, this is called cirrhosis. You may not have symptoms even if you develop cirrhosis due to NASH.
Symptoms from nonalcoholic steatohepatitis (NASH) may include:
- Severe tiredness
- Weakness
- Weight loss
- Yellowing of the skin or eyes (jaundice)
- Spiderlike blood vessels on your skin
- Long-lasting itchy skin.
Nonalcoholic steatohepatitis (NASH) that turns into cirrhosis could cause symptoms like fluid retention, abdominal swelling (ascites), shortness of breath, swelling of the legs, enlarged spleen, red palms, internal bleeding, muscle wasting, and confusion. People with cirrhosis over time may develop liver failure and need a liver transplant.
If nothing is done to stop the scarring, cirrhosis can lead to:
- Fluid buildup in the stomach area, called ascites.
- Swollen veins in your esophagus, or esophageal varices, which can rupture and bleed.
- Confusion, sleepiness and slurred speech, also called hepatic encephalopathy.
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- Liver cancer.
- End-stage liver failure, which means the liver has stopped working.
Nonalcoholic steatohepatitis complications
The main complication of nonalcoholic steatohepatitis (NASH) is the progression of NASH to cirrhosis. Cirrhosis means permanent scarring and hardening of the liver. Cirrhosis is a condition in which your liver is scarred and permanently damaged. Your liver performs many vital functions, including filtering toxins from your blood, managing blood clotting, making bile to digest fat, storing sugar for energy, turning extra glucose into glycogen, making protein for blood plasma, and helping with digestion. Scar tissue replaces healthy liver tissue and prevents your liver from working normally. Scar tissue also partly blocks the flow of blood through your liver. As cirrhosis gets worse, your liver begins to fail and you’ll need a liver transplant. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH). Moreover, people with NASH have an increased chance of dying from liver-related causes 62.
Liver fibrosis and cirrhosis
The inflammation and liver cell damage that happen with nonalcoholic steatohepatitis (NASH) can cause serious health problems. The inflamed liver will start to scar, a process called fibrosis (scar tissue is a kind of fibrous tissue). If left untreated, scar tissue will continue to replace healthy liver tissue leading to cirrhosis, which is advanced, late-stage scarring. About 20% of people with NASH will progress to cirrhosis over several years typically decades. Once you’ve been diagnosed with cirrhosis, treatment will focus on keeping your condition from getting worse. It may be possible to stop or slow the liver damage. Doctors can treat the health problems caused by cirrhosis with medications, operations, and other medical procedures. It’s important to protect the healthy liver tissue you have left.
Liver failure
If cirrhosis is not treated, the liver will not be able to work well or work at all. Liver failure means that your liver is losing or has lost all of its function. When liver failure occurs as a result of cirrhosis, it usually means that your liver has been failing gradually for some time, possibly for years. If cirrhosis leads to liver failure, you may need a liver transplant.
Liver cancer
One of the complications of cirrhosis is liver cancer. Liver cancer is the growth and spread of unhealthy cells in the liver. Cancer that starts in the liver is called primary liver cancer or hepatocellular carcinoma (HCC). Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer. NAFLD is now considered the third-most common cause of hepatocellular carcinoma (HCC) in the United States behind hepatitis C and alcohol induced liver disease although it is increasing more rapidly than from other conditions.
Cardiovascular disease and type 2 diabetes
The association between NAFLD and NASH with both cardiovascular disease and type 2 diabetes is bidirectional. This means that people with cardiovascular disease and/or type 2 diabetes are more likely to have NAFLD and NASH. And conversely, people with NAFLD or NASH are more likely to have cardiovascular disease and/or type 2 diabetes. In fact, cardiovascular disease is the most common cause of death in people who have either form of NAFLD.
Nonalcoholic steatohepatitis diagnosis
Doctors use your medical history, a physical exam, and tests to diagnose nonalcoholic fatty liver disease (NAFLD) including nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). Because nonalcoholic fatty liver disease (NAFLD) typically causes no symptoms, it is often found when tests done for other reasons point to a liver problem. For example, your blood work may show high levels of liver enzymes, or an ultrasound of your abdomen might reveal that your liver looks enlarged, which can lead to more testing. Doctors use blood tests, imaging tests, and sometimes liver biopsy to diagnose NAFLD and to tell the difference between NAFL and NASH.
Medical history
Your doctor will ask if you have a history of health conditions or diseases that make you more likely to develop NAFLD, such as:
- overweight or obesity
- insulin resistance or type 2 diabetes
- high levels of triglycerides or abnormal levels of cholesterol in your blood
- metabolic syndrome
Your doctor will ask about your diet and lifestyle factors that may make you more likely to develop liver disease or fat in your liver.
- What medicines you take to determine whether a medicine might be causing your fatty liver.
- Your doctor will ask about your alcohol intake to find out whether fat in your liver is a sign of alcohol-associated liver disease or NAFLD. Medical tests cannot show whether alcohol is the cause of fat in the liver, so it’s important to be honest with your doctor.
- What your diet is like (eating a diet high in sugar, or drinking sugary beverages), your level of physical activity, and other lifestyle factors that can contribute to the likelihood of developing NAFLD.
Physical exam
During a physical exam, a doctor usually examines your body and checks your weight and height to calculate your body mass index (BMI). Your BMI estimates how much you should weigh based on your height. Most experts say that a BMI greater than 30 (obesity) is unhealthy. If you want to figure out your BMI on your own, there are many websites that calculate it for you when you enter your height and weight. If you have more or less muscle than is normal, your BMI may not be a perfect measure of how much body fat you have. Your doctor may also take your waist circumference and waist-to-hip ratio into consideration.
Your doctor will look for signs of nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH), such as:
- an enlarged liver
- signs of insulin resistance, such as darkened skin patches over your knuckles, elbows, and knees
- signs of cirrhosis, such as an enlarged spleen, ascites, spiderlike blood vessels on your skin, yellowing of your skin and whites of your eyes (jaundice) and muscle loss
Blood tests
Your doctor may take a blood sample from you and send the sample to a lab.
Your blood tests may include:
- Complete blood count.
- Iron studies, which show how much iron is in your blood and other cells.
- Liver enzyme and liver function tests.
- Tests for chronic viral hepatitis (hepatitis A, hepatitis C and others).
- Celiac disease screening test.
- Fasting blood sugar.
- Hemoglobin A1C, which shows how stable your blood sugar is.
- Lipid profile, which measures blood fats, such as cholesterol and triglycerides.
Your doctor may suspect you have NAFLD if your blood test shows increased levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST). The cells in your liver contain proteins called enzymes, which are chemicals that help the liver do its work. When liver cells are damaged or destroyed, the enzymes in the cells leak out into the blood where they can be measured by blood tests. Liver enzyme testing usually checks the blood for two main enzymes 75, 93:
- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
If your liver is damaged due to inflammation, the level of these enzymes may be higher than normal. However, ALT and AST levels do not tell you how much scarring (fibrosis) may be present in your liver or predict how much liver damage will develop. In some people with NAFLD these liver enzymes may be normal as well.
Fibrosis assessment tests
These blood tests result in a score that estimates your level of liver scarring or fibrosis. They include:
- AST-to-Platelet Ratio Index (APRI) score
- Fibrosis-4 (Fib-4) score. The fibrosis-4 scoring system uses a patients age, platelet count, AST (aspartate aminotransferase) and ALT (alanine aminotransferase) to determine a liver fibrosis score and can help to predict advanced fibrosis.
These scores can help doctors identify or rule out advanced liver fibrosis, or scarring.
Your doctor may perform additional blood tests to find out if you have other health conditions that may increase your liver enzyme levels.
Imaging tests
Your doctor may order tests that take images, or pictures, of your liver to help make the diagnosis of liver disease. Different types of images can be obtained by using various types of equipment. However, these tests can’t show inflammation or fibrosis, so your doctor can’t use these tests to find out whether you have nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). If you have cirrhosis, routine imaging tests may show nodules, or lumps, in your liver.
Your doctor may use the following imaging tests to help diagnose NAFLD:
- Abdominal ultrasound, which uses a device called a transducer that bounces safe, painless sound waves off your organs to create an image of their structure. Abdominal ultrasoundis often the first test used when liver disease is suspected.
- Computed tomography (CT) scan, which uses a combination of x-rays and computer technology to create images of your liver.
- Magnetic resonance imaging (MRI), which uses radio waves and magnets to produce detailed images of organs and soft tissues without using x-rays.
- Transient elastography, a newer type of ultrasound that measures the stiffness of your liver to determine if you have advanced liver fibrosis. Liver stiffness is a sign of fibrosis or scarring. Commonly used types of elastography are:
- Vibration-controlled transient elastography, a special type of ultrasound
- Sheer wave elastography, another type of ultrasound to detect increased liver stiffness
- Magnetic resonance elastography (MRE), is a newer, noninvasive test that combines features of ultrasound and MRI imaging to create a visual map showing gradients of stiffness throughout the liver. MRE has been shown to be a more reliable measure of liver stiffness in severely obese patients.
Liver biopsy
If other tests show signs of more-advanced liver disease or NASH, or if your test results are unclear, your doctor may suggest a liver biopsy. Liver biopsy is a procedure to remove a small piece of tissue from your liver. It is usually done using a needle through the abdominal wall. The tissue sample is looked at in a lab for signs of inflammation and scarring. Liver biopsy is the only test that can prove a diagnosis of NASH and clearly shows the amount of liver damage.
Liver biopsy can show fibrosis at earlier stages than elastography can. However, doctors don’t recommend liver biopsy for everyone with suspected NAFLD. Your doctor may recommend a liver biopsy if you are more likely to have NASH with advanced fibrosis or if your other tests show signs of advanced liver disease or cirrhosis. In some cases, doctors may recommend a liver biopsy to rule out other liver diseases.
During a liver biopsy, a doctor using a needle that is passed through the abdominal wall and into the liver will take small pieces of tissue from your liver. A pathologist will examine the tissue under a microscope to look for signs of damage or disease.
A liver biopsy can be uncomfortable, and it does have risks that your doctor will go over with you in detail.
Nonalcoholic steatohepatitis treatment
Doctors recommend weight loss, done through a combination of calorie reduction, exercise, and healthy eating, to treat nonalcoholic fatty liver disease (NAFLD), either nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). Weight loss can reduce fat, inflammation, and fibrosis or scarring in your liver.
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve NAFLD either nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). Losing at least 3% to 5% of your body weight can reduce fat in the liver 62. You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis 62. Physical activity alone, even without weight loss, is also beneficial.
The best way to lose weight is done by:
- Reducing the number of calories you eat. Keeping track of the calories you consume every day and employing portion control can help.
- Eating a healthy diet that’s rich in fruits and vegetables, whole grains and low in saturated fats. Limit animal-based foods, like red meat which is high in saturated fats, and eat more plant-based foods like beans, legumes, and nuts. Use good fats like olive oil. This is the basis for the Mediterranean diet – which isn’t a diet in the traditional sense, but a healthy way of eating inspired by the eating habits of people living in the Mediterranean area and is often recommended by doctors as a way to reduce some of the risk factors associated with fatty liver disease.
- Limiting the amount of salt and sugar in your diet, particularly sugar-sweetened beverages, like soda, juices, sports drinks, and sweetened tea. High consumption of fructose, one of the main sweeteners in these beverages, increases your odds of developing obesity, type 2 diabetes, metabolic syndrome, and NAFLD.
- Limit your intake of saturated fats, which are found in meat, poultry skin, butter, shortening, milk and dairy products (except fat-free versions). Replace them with monounsaturated fats (olive, canola, and peanut oils) and polyunsaturated fats (corn, safflower, soybean oils, and many types of nuts). Particularly helpful in reducing heart disease are omega-3 fatty acids, a type of polyunsaturated fat found in oily fish such as salmon, flaxseed oil, and walnuts. Healthy eating combined with exercise – and taking cholesterol-lowering medications if prescribed by your doctor – will help keep your cholesterol and triglyceride levels where they need to be.
- Exercise and be more active – exercise is important for many reasons; it can help with weight control, boost your immune system, and alleviate stress and depression. Aim for at least 150 minutes of exercise a week. Depending on how much weight you’re trying to lose, you may need to up that amount. Getting exercise doesn’t mean you have to go to a gym – walking, gardening, and even housework counts. However, if you don’t already exercise, get your doctor’s okay first and build slowly. The goal is to participate in exercise of a moderate intensity (examples include light jogging, biking, swimming or playing a sport that boosts your heart rate and results in sweating).
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
If you’ve tried to lose weight in the past without success, talk to your dietitian about getting help. You may also be a candidate for a medically-supervised weight loss program that employs medication along with diet and exercise. Alternatively, there are weight-loss (bariatric) surgical procedures and endoscopic therapies that work by either physically limiting the amount of food your stomach can hold, or reducing the amount of nutrients and calories your body absorbs. Talk to your doctor about which option may be best for you.
Nonalcoholic steatohepatitis diet
If you have NAFLD, your doctor may suggest changes to your diet such as:
- Limiting your intake of fats, which are high in calories and increase your chance of developing obesity.
- Replacing saturated fats and trans fats in your diet with unsaturated fats, especially omega-3 fatty acids, which may reduce your chance of heart disease if you have NAFLD.
- Eating more low-glycemic (low GI) index foods such as most fruits, vegetables, and whole grains. These foods affect your blood glucose less than high-glycemic index foods, such as white bread, white rice, and potatoes.
- Avoiding foods and drinks that contain large amounts of simple sugars, especially fructose. Fructose is found in sweetened soft drinks, sports drinks, sweetened tea, and juices. Table sugar, called sucrose, is rapidly changed to glucose and fructose during digestion and is therefore a major source of fructose.
If you have NAFLD, you should minimize alcohol use, which can further damage your liver.
Nonalcoholic steatohepatitis medicine
A new medicine called Resmetirom (Rezdiffra) can help reduce the amount of fat that collects in the liver is available to treat people who have NASH with moderate to severe liver scarring. In March 2024, the US Food and Drug Administration (FDA) approved the use of resmetirom (Rezdiffra) for people with NASH and stage 2 or 3 fibrosis (but not cirrhosis) along with eating a healthy diet and participating in regular exercise. This is the first drug approved for NASH in the United States and the approval was based on resolution of NASH and improvement in fibrosis in about a quarter of the patients treated in a large international trial 136. Resmetirom (Rezdiffra) is not recommended for people with cirrhosis. For those who have cirrhosis due to NASH, a liver transplant may be needed.
Resmetirom (Rezdiffra) drug works by revving up the thyroid hormone pathway in the liver to increase the metabolism of liver fat. The most common side effects of treatment are nausea and diarrhea. Gallstones and gallbladder inflammation also developed in some patients in the trials. It can also interact with other medications such as statins, gemfibrozil (Lopid) and clopidogrel (Plavix), so be sure that your doctor has a full list of your medications before prescribing resmetirom (Rezdiffra). A liver biopsy is not essential to start resmetirom (Rezdiffra) because other tests that can show the accumulation of liver fibrosis such as Fibroscan or other measures of liver stiffness can provide the necessary information. Resmetirom (Rezdiffra) is not for people who do not have evidence of significant liver fibrosis.
Protect your liver
Don’t do things that put extra stress on your liver:
- Avoid drinking alcohol.
- Take medications and over-the-counter drugs only as instructed by your doctor.
- Be cautious about taking dietary supplements. Certain vitamins and minerals – like vitamins A, iron, and niacin – can be harmful to your liver in higher doses than necessary or prescribed.
Check with your doctor before trying any herbal remedies. Just because a product is called “natural,” does not mean it’s safe. - Get vaccinated for hepatitis A and hepatitis B. If you get hepatitis A or B, along with fatty liver, it’s more likely to lead to liver failure.
- Manage your diabetes. Follow your doctor’s advice to manage your diabetes. Take your medicines as told by your care team and watch your blood sugar closely.
- Lower your cholesterol and blood pressure. Improve your cholesterol levels and blood pressure if they are high. A healthy diet, exercise and medicines can help keep your cholesterol, triglycerides and blood pressure at healthy levels.
Vitamin E, which is an antioxidant, in theory could help protect the liver by reducing or canceling out the damage caused by inflammation. But more research is needed. Some evidence suggests vitamin E supplements may be helpful for people with liver damage due to NAFLD and NASH who don’t have type 2 diabetes. Researchers in one study found that a daily dose of the natural form of vitamin E – the kind that comes from food sources and isn’t made in a laboratory – improved NASH in study participants overall by reducing fat and inflammation although not scarring. This medication is not for everyone and may have potential side effects as well. Vitamin E has been linked with a slightly increased risk of heart disease and prostate cancer. Discuss the potential benefits and side effects of vitamin E with your doctor.
Some studies suggest that coffee may benefit the liver by reducing the risk of liver diseases like NAFLD and lowering the chance of scarring. It’s not yet clear how coffee may prevent liver damage. But certain compounds in coffee are thought to lower inflammation and slow scar tissue growth. If you already drink coffee, these results may make you feel better about your morning cup. But if you don’t already drink coffee, this probably isn’t a good reason to start. Discuss the possible benefits of coffee with your health care team.
Nonalcoholic steatohepatitis prognosis
Patients with non-alcoholic fatty liver disease (NAFLD) exhibit increased mortality rates when compared to the general population. These patients have a high risk of mortality from cardiovascular causes as these patients have metabolic derangements. Cardiovascular causes of mortality are higher in these patients than liver causes 114. NAFLD is a slowly progressive disease; simple steatosis is reversible and non-progressive, whereas nonalcoholic steatohepatitis (NASH) can progress to cirrhosis. It is unclear why some people develop NASH. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH). Over a 13 year follow-up, the progression of cirrhosis presented in 41% in a study by Ekstedt et al 117. A meta-analysis done by White et al 123 showed that in cohorts of NAFLD or NASH with few or no cases of cirrhosis, the risk of developing hepatocellular carcinoma (HCC) was minimal at 0 to 3% over 20 years, and in cohorts with NASH with cirrhosis, the risk was high at 2.4 % over seven years. Losing weight and managing diabetes can slow or sometimes reverse the deposit of fat in your liver.
Alcoholic liver disease
Alcoholic fatty liver disease (AFLD) is a fatty liver disease caused to heavy alcohol (ethanol) consumption 137. Alcoholic fatty liver disease (AFLD) is characterized by the excessive accumulation of triglycerides and cholesterol in liver cells 138. If you have a history of heavy alcohol use and fat in your liver, your doctor may determine you have alcohol-associated liver disease instead of nonalcoholic fatty liver disease (NAFLD). If you have risks for nonalcoholic fatty liver disease (NAFLD) and also drink alcohol (ethanol) excessively, you could have both nonalcoholic fatty liver disease (NAFLD) and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Your liver breaks down most of the alcohol (ethanol) you drink using liver enzymes – alcohol dehydrogenase (ADH), aldehyde dehydrogenase (ALDH), and Cytochrome P450 2E1 (CYP2E1), so it can be removed from your body 138, 139, 140. But the process of breaking alcohol down can generate harmful substances: (1) acetaldehyde accumulation; (2) an alteration in the nicotinamide adenine dinucleotide (NAD)H/NAD+ ratio; and/or (3) generation of reactive oxygen species (ROS) 137. These substances can damage liver cells, promote liver inflammation (hepatitis), and weaken your body’s natural defenses 138, 140, 141, 142, 143. The more alcohol that you drink, the more you damage your liver. Alcoholic fatty liver disease is the earliest stage of alcohol-related liver disease. The next stages are alcoholic hepatitis and cirrhosis. Alcohol is a toxin and a psychoactive and dependence-producing substance and has been classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC) decades ago – this is the highest risk group, which also includes asbestos, radiation and tobacco 144, 145, 144, 146. According to the latest 2023 report from the World Health Organization (WHO), alcohol (ethanol) is a major factor in the development of around 200 diseases, and no amount of alcohol consumption is considered safe 147. Alcohol consumption is the third major cancer risk factor after tobacco use and excess body weight and alcohol consumption is an established cause of at least 7 types of cancer, such as oral cavity cancer, pharyngeal cancer, laryngeal cancer, esophageal cancer, liver cancer, colorectal cancer, and female breast cancer 148, 149, 150, 151, 152, 153, 154. The risk of developing cancer increases substantially the more alcohol you consumed 147, 155.
Alcoholic fatty liver disease stages
There are 3 histologic stages of alcoholic liver disease 156, 157:
- Alcoholic fatty liver (steatosis): At this stage, small fat droplets accumulate around liver cells, specifically around the venules, and approaches the portal tracts. Fatty liver is generally considered a reversible condition.
- Alcoholic hepatitis: Inflammation of liver cells takes place at this stage and the outcome depends on the severity of the damage. Eosinophilic fibrillar material (Mallory hyaline or Mallory-Denk bodies) forms in swollen (ballooned) hepatocytes. Alcohol abstinence, nutritional support, treatment of infection, and prednisolone therapy in severe cases can help in the treatment of alcoholic hepatitis, but more severe cases lead to liver failure.
- Alcoholic cirrhosis: The end-stage of liver disease is alcoholic cirrhosis. At this stage, fibrotic septae surround regenerative nodules in the liver 157. The deposition of collagen typically occurs around the terminal hepatic vein (perivenular fibrosis) and along the sinusoids, leading to a peculiar “chicken wire” pattern of fibrosis in alcoholic cirrhosis. Liver damage at this stage is irreversible and leads to complications of cirrhosis and portal hypertension.
People do not necessarily progress sequentially through the three stages of alcohol-related liver disease. Some may advance from fatty liver disease to alcoholic hepatitis but others will first present with cirrhosis.
Alcoholic fatty liver (steatosis)
Alcoholic fatty liver also called steatosis is the earliest stage of alcohol-related liver disease and the most common alcohol-related liver disorder 158. Alcoholic fatty liver is characterized by an excessive accumulation of fat inside liver cells, which makes it harder for the liver to function. Usually there are no symptoms, although the liver can be enlarged and you may experience upper abdominal discomfort on the right side. Fatty liver occurs fairly soon in almost all people who drink heavily. The condition will usually go away if you stop drinking.
Alcoholic hepatitis
Alcoholic hepatitis is an inflammation, or swelling, of the liver accompanied by the destruction of liver cells. Up to 35 percent of heavy drinkers develop alcoholic hepatitis, which can be mild or severe 158. Symptoms may include fever, jaundice, nausea, vomiting, abdominal pain and tenderness. In its mild form, alcoholic hepatitis can last for years and will cause progressive liver damage, although the damage may be reversible over time if you stop drinking. In its severe, acute form the disease may occur suddenly – after binge drinking for instance – and can quickly lead to life-threatening complications. Alcohol abstinence, nutritional support, treatment of infection, and prednisolone therapy in severe cases can help in the treatment of alcoholic hepatitis, but more severe cases lead to liver failure.
Alcoholic cirrhosis
Alcoholic cirrhosis is the most serious type of alcohol-related liver disease. Cirrhosis refers to the replacement of normal liver tissue with nonliving scar tissue. Between 10 and 20 percent of heavy drinkers develop cirrhosis, usually after 10 or more years of drinking 158. Anything that damages the liver over many years can lead the liver to form scar tissue. Fibrosis is the first stage of liver scarring. When scar tissue builds up and takes over most of the liver, it’s referred to as cirrhosis. Research has shown that cirrhosis can be reversed, although this may not occur for all patients. Cirrhosis caused by alcohol can be a life-threatening disease 158. Many individuals with advanced cirrhosis will experience complications such as fluid retention (ascites), gastrointestinal bleeding from abnormal veins (varices), confusion (hepatic encephalopathy) or development of liver cancer. Some individuals will benefit from a liver transplant but may not be eligible until a period of abstinence has been attained.
Alcoholic liver disease causes
In the United States, alcohol is the leading cause of liver disease. It involves 61 percent of the American population, and among the 61 percent, 10 to 12 percent are heavy drinkers 159. Drinking too much alcohol, either on a single occasion known as binge drinking or drinking a lot over time, can take a serious toll on your health and well-being. In addition to injuring your liver, alcohol has many effects on your body including:
- Lessening your ability to think clearly and move with coordination; it can change your mood and behavior.
- Disrupting the processes involved in digestion, leading to malnutrition and weight loss.
- Weakening your immune system and the ability to fight infections. Increasing your risk of developing certain cancers including cancers of the colon, liver, esophagus, mouth, and breast (for women).
In the United States, one standard drink is one that contains about 14 grams of pure alcohol (ethanol), which is found in:
- 12 ounces (355 ml) of regular beer (5% alcohol content)
- 8 to 9 ounces (237 to 266 ml) of malt liquor (about 7% alcohol)
- 5 ounces (148 ml) of wine (12% alcohol content)
- 1.5 ounces (44 milliliters) or a “shot” of distilled spirits (e.g., gin, whiskey, vodka) or liquor (40% alcohol content)
As of 2023, the National Institutes of Health defines heavy alcohol use as:
- For men, consuming 5 or more drinks on any day or 15 or more drinks per week
- For women, consuming 4 or more drinks on any day or 8 or more drinks per week
Daily consumption of 30 to 50 grams of alcohol for over five years can cause alcoholic liver disease 159. Alcoholic fatty liver or steatosis can occur in 90% of patients who drink over 60 g/day, and cirrhosis occurs in 30% of individuals with long-standing consumption of more than 40 g/day 159.
Alcoholic liver disease occurs after years of heavy drinking. Over time, scarring and cirrhosis of the liver can occur. Cirrhosis is scarring of the liver and poor liver function. It is the last stage of chronic liver disease including alcoholic liver disease 160.
Alcoholic liver disease does not occur in all heavy drinkers. The chances of getting liver disease go up the longer you have been drinking and more alcohol you consume. You do not have to get drunk for the disease to happen 160.
Alcoholic liver disease seems to be more common in some families 160. Women may be more likely to have this problem than men 160.
The liver tolerates mild alcohol consumption, but as the consumption of alcohol increases, it leads to disorders of the metabolic functioning of the liver. The initial stage involves the accumulation of fat in the liver cells, commonly known as alcoholic fatty liver or steatosis. If the consumption of alcohol does not stop at this stage, it sometimes leads to alcoholic hepatitis, which is an inflammation, or swelling, of the liver accompanied by the destruction of liver cells. With continued alcohol consumption, the alcoholic liver disease progresses to severe damage to liver cells known as “alcoholic cirrhosis”. Alcoholic cirrhosis is the stage described by progressive hepatic fibrosis and nodules.
Quantity and duration of the patient’s alcohol intake are the highest risk factors for the development of liver disease. The beverage type plays a minimal role. Women are more susceptible than men. Obesity and high-fat diet also increase the risk of alcoholic liver disease. Concurrent hepatitis C infection is associated with younger age of onset, more advanced histological damage, and decreased survival. Patatin-like phospholipase domain-containing protein 3 (PNPLAP3) is associated with alcoholic liver cirrhosis 159.
The amount of alcohol you consume is the most important risk factor for developing alcohol-related liver disease 158. The risk increases with the length of time and amount of alcohol you drink. However, because many people who drink heavily or binge drink do not develop alcohol-related liver disease, we know there are other factors that affect a person’s susceptibility.
Additional risk factors that play a role in someone developing alcohol-related liver disease include:
- Obesity: Obesity is a contributing factor to fatty liver disease. The combined effect of obesity and alcohol together is worse than the effect of either one of them alone.
- Malnutrition: Many people who drink heavily are malnourished, either because they eat poorly due to loss of appetite and nausea or because alcohol and its toxic byproducts prevent the body from breaking down and absorbing nutrients. In both cases, the lack of nutrients contributes to liver cell damage.
- Genetic factors: Genetics can influence how the body processes alcohol and may predispose someone to alcoholism and alcohol-related liver disease. Race and ethnicity: A higher risk of liver injury appears to be associated with one’s racial and ethnic heritage. For example, rates of alcoholic cirrhosis are higher in African-American and Hispanic males compared with Caucasian males.
- Your sex: Women are more susceptible than men to the adverse effects of alcohol.
- Pattern of drinking: It’s worse to drink outside of meal times and binge drink, defined as five drinks for men and four drinks for women in one sitting.
- Chronic viral hepatitis, particularly hepatitis C: The combined effect of alcohol and viral hepatitis on the liver results in more advanced disease than either of them alone.
Many heavy drinkers will progress from fatty liver disease to alcoholic hepatitis to alcoholic cirrhosis over time. However, some heavy drinkers may develop cirrhosis without first having alcoholic hepatitis first 7. Others may have alcoholic hepatitis but never have symptoms. Additionally, alcohol consumption may worsen liver injury caused by non-alcoholic liver diseases such as chronic hepatitis C.
Since an individual’s susceptibility to the toxic effects of alcohol may vary by many factors including age, gender, genetics and coexistent medical conditions, it is reasonable for you to review alcohol use with your physician.
Alcoholic liver disease pathophysiology
Your liver breaks down most of the alcohol (ethanol) you drink using liver enzymes – alcohol dehydrogenase (ADH), aldehyde dehydrogenase (ALDH), and Cytochrome P450 2E1 (CYP2E1), so it can be removed from your body 138, 139, 140. But the process of breaking alcohol down can generate harmful substances: (1) acetaldehyde accumulation; (2) an alteration in the nicotinamide adenine dinucleotide (NAD)H/NAD+ ratio; and/or (3) generation of reactive oxygen species (ROS) 137. These substances can damage liver cells, promote liver inflammation (hepatitis), and weaken your body’s natural defenses 138, 140, 141, 142, 143. The more alcohol that you drink, the more you damage your liver.
Alcohol dehydrogenase converts alcohol into acetaldehyde, and aldehyde dehydrogenase converts acetaldehyde into acetate. The metabolism of alcohol increases the production of NADH by reducing NAD in the body. This shifting of metabolic balance toward the production of NADH leads to the formation of glycerol phosphate, which combines with the fatty acids and becomes triglycerides, which accumulate within the liver. When lipid oxidation (lipolysis) stops due to alcohol consumption, fats accumulate in the liver and lead to “fatty liver disease.” Continued alcohol consumption brings the immune system into play. Interleukins with the help of neutrophils attack the hepatocytes, and swelling of the hepatocytes known as the “alcoholic hepatitis” takes place. Ongoing liver injury leads to irreversible liver damage, the cirrhosis of the liver.
Alcoholic liver disease symptoms
There may be no symptoms, or symptoms may come on slowly, depending on how well your liver is working. Symptoms tend to be worse after a period of heavy drinking.
Early symptoms include:
- Fatigue and loss of energy
- Poor appetite and weight loss
- Nausea or belly pain
- Small, red spider-like blood vessels on the skin.
As liver function worsens, symptoms may include:
- Fluid buildup of the legs (edema) and in the abdomen (ascites)
- Yellow color in the skin, mucous membranes, or eyes (jaundice)
- Redness on the palms of the hands
- In men, impotence, shrinking of the testicles, and breast swelling
- Easy bruising and abnormal bleeding
- Behavior changes and confusion or problems thinking
- Pale or clay-colored stools
Alcoholic liver disease complications
Possible complications of alcoholic liver disease:
- Bleeding disorders (coagulopathy)
- Buildup of fluid in the abdomen (ascites) and infection of the fluid (bacterial peritonitis)
- Ascites: This is the most common complication of alcoholic liver disease in which there is an accumulation of fluid in the peritoneal cavity. The patient usually presents with abdominal distension and pedal edema. It can be managed with sodium restriction, diuretics, paracentesis, and transjugular intrahepatic portosystemic shunt placement (TIPS).
- Spontaneous Bacterial Peritonitis: It is an infection of ascitic fluid with no evidence of any other intraabdominal source (e.g., a perforated viscus) of infection. The diagnosis can be confirmed by positive ascitic fluid bacterial culture and ascitic fluid absolute neutrophil count of over 250/mm³. The preferred antibiotic is cefotaxime, but ciprofloxacin can be an option if the patient is not able to take cefotaxime.
- Enlarged veins in the esophagus, stomach, or intestines that bleed easily (esophageal varices).
- Variceal hemorrhage: The presentation is usually with vomiting blood (hematemesis) or melena (black tarry stool). Management options include endoscopic band ligation, sclerotherapy, and placement of transjugular intrahepatic portosystemic shunt placement (TIPS). TIPS increases the risk of hepatic encephalopathy.
- Increased pressure in the blood vessels of the liver (portal hypertension)
- Kidney failure (hepatorenal syndrome): This is the development of renal failure owing to advanced alcoholic liver disease after having excluded other causes of kidney failure. Characteristically, it demonstrates a progressive rise in creatinine, low sodium excretion rate, oliguria, benign urinary sediment, and absence of proteinuria.
- Type 1 hepatorenal syndrome is a more severe type with at least a two-fold increase in creatinine in less than two weeks. It correlates with a high mortality rate.
- Type 2 hepatorenal syndrome is slower in onset and has a relatively better prognosis. Treatment for a critically ill patient includes norepinephrine and albumin. For noncritically ill patients treatment includes midodrine ( oral alpha agonist), octreotide, and albumin. The ultimate treatment is liver transplantation
- Hepatopulmonary syndrome: Hepatopulmonary syndrome characteristically presents with elevated alveolar-arterial oxygen gradient on room air and evidence of intrapulmonary vascular abnormalities. The patient typically presents with shortness of breath and hypoxia. There is no treatment option except liver transplantation.
- Hepatic hydrothorax: Hepatic hydrothorax is the presence of pleural effusion, and excludes other causes of pleural effusion. Treatment is diuretics, thoracentesis, and transjugular intrahepatic portosystemic shunt placement (TIPS).
- Mental confusion, change in the level of consciousness, or coma (hepatic encephalopathy). Hepatic encephalopathy is characterized by reversible neuropsychiatric abnormalities. Treatment includes lactulose, rifaximin, and correction of precipitating factors like infection, GI bleeding, etc.
Other rare complications are cirrhotic cardiomyopathy, liver cancer (hepatocellular carcinoma), portal gastropathy, portopulmonary hypertension, and portal vein thrombosis.
Alcoholic liver disease diagnosis
Alcoholic liver disease is caused by heavy use of alcohol.
Your doctor will do a physical exam to look for:
- An enlarged liver or spleen
- Excess breast tissue
- Swollen abdomen, as a result of too much fluid
- Reddened palms
- Red spider-like blood vessels on the skin
- Small testicles
- Widened veins in the abdomen wall
- Yellow eyes or skin (jaundice)
Tests you may have include:
- Complete blood count (CBC): Complete blood count to rule out the infection, look for complications of cirrhosis: anemia, thrombocytopenia, a leukemoid reaction in alcoholic hepatitis.
- Basic metabolic profile (BMP) should be ordered to look for renal failure and electrolyte disturbance (low levels of potassium, magnesium, and phosphorus).
- Liver function tests: AST (aspartate aminotransferase) is markedly raised as opposed to ALT (alanine aminotransferase) in alcoholic liver disease. There is hypoalbuminemia, hyperbilirubinemia, and hypertriglyceridemia. Also, GGTP (gamma-glutamyl transpeptidase) is usually raised.
- Coagulation studies: Prothrombin time (PT) and international normalized ratio (INR) to assess liver synthetic function (i.e., clotting (coagulation) factors). A prothrombin time (PT) test measures how many seconds it takes for a clot to form in a blood sample. Since the results of this test can vary with different labs or test methods, your results may be used to create an INR (international normalized ratio). An elevated value indicates more severe disease.
- Liver biopsy: A liver biopsy can lead to a definitive diagnosis in cases where the diagnosis is uncertain. More often than not, it is used for evaluation of severity, prognosis, staging, and treatment monitoring. For an accurate diagnosis of fibrosis, at least a 1.5 to 2 cm long sample of liver tissue is necessary. Liver biopsy has a risk of complication, including life-threatening hemorrhage, so it is reserved for cases where the results of a biopsy can make a difference in the treatment plan.
Tests to rule out other diseases include:
- Abdominal CT scan
- Blood tests for other causes of liver disease. Elevated CA-125 levels were noted in 85% of patients with cirrhosis in one study. The more advanced the degree of decompensation based on MELD score, Child’s Turcotte-Pugh classification, and ALBI score, the higher the elevation in CA-125 161.
- Ultrasound of the abdomen. Abdominal ultrasonography is useful in looking for biliary obstruction and liver tumors.
- Endoscopy to look for esophageal varices due to portal hypertension in patients with cirrhosis.
Alcoholic liver disease treatment
Lifestyle Changes
Some things you can do to help take care of your liver disease are:
- Abstinence: If you’ve been diagnosed with alcohol-related liver disease, the single most important thing you can do for yourself is to stop drinking. Abstinence is the only way of possibly reversing liver damage, or in more advanced cases, preventing it from becoming worse. Discuss treatment options with your healthcare provider; these can include counseling, medications, an outpatient treatment program or a residential inpatient stay. If you are physically addicted to alcohol, medical supervision in a detoxification (or detox) program may be required to safely reduce your alcohol levels. It can be dangerous to stop drinking very suddenly. A rapid reduction in alcohol can lead to withdrawal symptoms including anxiety, agitation, hallucinations and seizures. Your doctor can recommend a program that best meets your needs.
- Nutrition therapy: Nutritional deficiencies are very common in people with alcohol-related liver disease. Your doctor will likely recommend a special diet, as well as vitamin and nutritional supplements, to combat the effects of malnutrition and help you gain weight if needed. You may be referred to a nutritionist who can assist you with meal planning. If you have trouble eating enough to get the vitamins and nutrients you need, your doctor may recommend giving you a special nutrient-rich liquid intravenously or via tube feeding. Eat a healthy diet that is low in salt.
- Get vaccinated for diseases such as influenza, hepatitis A and hepatitis B, and pneumococcal pneumonia.
- Talk to your doctor about all medicines you take, including herbs and supplements and over-the-counter medicines.
Medicines from your doctor
- “Water pills” (diuretics) to get rid of fluid build-up
- Vitamin K or blood products to prevent excess bleeding
- Medicines for mental confusion
- Antibiotics for infections
- Depending on the severity of your disease, your doctor may recommend medications to help reduce liver inflammation. These drugs have shown some short-term benefit in increasing survival. Steroid treatment with prednisolone is usually the first-line medication, followed by pentoxifylline, if steroid therapy doesn’t work. No alternative medicine treatments have been found to cure alcoholic hepatitis.
Other Treatments
- Endoscopic treatments for enlarged veins in the throat (bleeding varices)
- Removal of fluid from the abdomen (paracentesis)
- Placement of a transjugular intrahepatic portosystemic shunt (TIPS) to repair blood flow in the liver
When cirrhosis progresses to end-stage liver disease, a liver transplant may be needed in those who have shown a commitment to continued alcohol abstinence.
Alcoholic liver disease prognosis
Anyone with alcohol-related liver disease will improve their health and life expectancy if they stop drinking. However, up to 20% of patients with fatty liver may still progress to cirrhosis 162. People with alcoholic hepatitis or alcoholic cirrhosis should stop drink completely.
For alcohol-related liver disease people who do not stop drinking the outlook is poor. Continued excessive drinking can shorten your lifespan. Your risk for complications such as bleeding, brain changes, and severe liver damage go up. The outcome will likely be poor if you keep drinking.
Cirrhosis is caused by scarring of the liver and the prognosis is poor. In most cases, the liver cannot heal or return to normal function once the damage is severe. Cirrhosis can lead to serious complications. Screening for hepatocellular carcinoma is important at this stage. The presence of ascites, variceal bleeding, severe encephalopathy, and hepatorenal syndrome also indicate poor prognosis.
Model for End-Stage Liver Disease (MELD) score is calculated as a 3.8 x log (serum bilirubin [mg/dL]) + 11.2 x log (INR) + 9.6 x log (serum creatinine [mg/dL]) + 6.4.
The Model for End-Stage Liver Disease (MELD) score was adopted by the United Network for Organ Sharing (UNOS) to prioritize patients waiting for a liver transplant due to its ability to predict 90-day mortality 163, 164. In 2016 the Organ Procurement and Transplantation Network (OPTN) in conjunction with United Network for Organ Sharing (UNOS) announced the inclusion of sodium into the MELD score for patients greater than 12 years of age with a MELD score greater than 11. 90-day mortality based on MELD score is 1.9% for MELD <10, 6% for 10-19, 19.6% for 20-29, 52.6% for 30-39, and 71.3% for 40.
Discriminant function (DF) is calculated as 4.6 x (patient’s prothrombin time – control prothrombin time) + total bilirubin of the patient.
Discriminant function (DF) is also a useful predictive tool, and patients with alcoholic hepatitis and a DF greater than 32 have a >50% 30-day mortality.
- Nonalcoholic fatty liver disease. Angulo P. N Engl J Med. 2002 Apr 18; 346(16):1221-31. https://www.ncbi.nlm.nih.gov/pubmed/11961152/[↩]
- Francque, S. M., Marchesini, G., Kautz, A., Walmsley, M., Dorner, R., Lazarus, J. V., Zelber-Sagi, S., Hallsworth, K., Busetto, L., Frühbeck, G., Dicker, D., Woodward, E., Korenjak, M., Willemse, J., Koek, G. H., Vinker, S., Ungan, M., Mendive, J. M., & Lionis, C. (2021). Non-alcoholic fatty liver disease: A patient guideline. JHEP reports : innovation in hepatology, 3(5), 100322. https://doi.org/10.1016/j.jhepr.2021.100322[↩]
- Nonalcoholic Fatty Liver Disease: Common Questions and Answers on Diagnosis and Management. Am Fam Physician. 2020 Nov 15;102(9):603-612. https://www.aafp.org/afp/2020/1115/p603.html[↩][↩][↩]
- De Minicis S, Day C, Svegliati-Baroni G. From NAFLD to NASH and HCC: pathogenetic mechanisms and therapeutic insights. Curr Pharm Des. 2013;19(29):5239-49. DOI: 10.2174/1381612811319290006[↩]
- The National Institute of Diabetes and Digestive and Kidney Diseases Health Information Center. Definition & Facts of NAFLD & NASH. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts[↩][↩]
- Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Bugianesi E, Leone N, Vanni E, Marchesini G, Brunello F, Carucci P, Musso A, De Paolis P, Capussotti L, Salizzoni M, Rizzetto M. Gastroenterology. 2002 Jul; 123(1):134-40. https://www.ncbi.nlm.nih.gov/pubmed/12105842/[↩]
- American Liver Foundation. Alcohol-Related Liver Disease. http://www.liverfoundation.org/abouttheliver/info/alcohol/[↩][↩]
- Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018 Jan;67(1):328-357. doi: 10.1002/hep.29367[↩][↩][↩][↩][↩]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012 Feb 1;307(5):491-7. doi: 10.1001/jama.2012.39[↩]
- Kim, S. Y., England, L., Wilson, H. G., Bish, C., Satten, G. A., & Dietz, P. (2010). Percentage of gestational diabetes mellitus attributable to overweight and obesity. American journal of public health, 100(6), 1047–1052. https://doi.org/10.2105/AJPH.2009.172890[↩]
- Sarkar, M., Grab, J., Dodge, J. L., Gunderson, E. P., Rubin, J., Irani, R. A., Cedars, M., & Terrault, N. (2020). Non-alcoholic fatty liver disease in pregnancy is associated with adverse maternal and perinatal outcomes. Journal of hepatology, 73(3), 516–522. https://doi.org/10.1016/j.jhep.2020.03.049[↩][↩][↩]
- Cleveland, E., Bandy, A., & VanWagner, L. B. (2018). Diagnostic challenges of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Clinical liver disease, 11(4), 98–104. https://doi.org/10.1002/cld.716[↩]
- Antunes C, Azadfard M, Hoilat GJ, et al. Fatty Liver. [Updated 2021 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441992[↩][↩]
- Fatty Liver. https://www.msdmanuals.com/en-au/home/liver-and-gallbladder-disorders/manifestations-of-liver-disease/fatty-liver[↩]
- Leoni, S., Tovoli, F., Napoli, L., Serio, I., Ferri, S., & Bolondi, L. (2018). Current guidelines for the management of non-alcoholic fatty liver disease: A systematic review with comparative analysis. World journal of gastroenterology, 24(30), 3361–3373. https://doi.org/10.3748/wjg.v24.i30.3361[↩][↩]
- Loman BR, Hernández-Saavedra D, An R, Rector RS. Prebiotic and probiotic treatment of nonalcoholic fatty liver disease: a systematic review and meta-analysis. Nutr Rev. 2018 Nov 1;76(11):822-839. doi: 10.1093/nutrit/nuy031[↩]
- von Schönfels W, Beckmann JH, Ahrens M, Hendricks A, Röcken C, Szymczak S, Hampe J, Schafmayer C. Histologic improvement of NAFLD in patients with obesity after bariatric surgery based on standardized NAS (NAFLD activity score). Surg Obes Relat Dis. 2018 Oct;14(10):1607-1616. doi: 10.1016/j.soard.2018.07.012[↩]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016 Jun;64(6):1388-402. doi: 10.1016/j.jhep.2015.11.004[↩][↩]
- Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol. 2005 Jan;42(1):132-8. doi: 10.1016/j.jhep.2004.09.012[↩]
- Sanyal, A. J., Friedman, S. L., McCullough, A. J., Dimick-Santos, L., American Association for the Study of Liver Diseases, & United States Food and Drug Administration (2015). Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration Joint Workshop. Hepatology (Baltimore, Md.), 61(4), 1392–1405. https://doi.org/10.1002/hep.27678[↩]
- Non-alcoholic fatty liver disease (NAFLD): assessment and management. https://www.nice.org.uk/guidance/ng49/resources/nonalcoholic-fatty-liver-disease-nafld-assessment-and-management-pdf-1837461227461[↩][↩][↩][↩]
- Italian Association for the Study of the Liver (AISF). AISF position paper on nonalcoholic fatty liver disease (NAFLD): Updates and future directions. Dig Liver Dis. 2017 May;49(5):471-483. doi: 10.1016/j.dld.2017.01.147[↩][↩]
- Shields, W. W., Thompson, K. E., Grice, G. A., Harrison, S. A., & Coyle, W. J. (2009). The Effect of Metformin and Standard Therapy versus Standard Therapy alone in Nondiabetic Patients with Insulin Resistance and Nonalcoholic Steatohepatitis (NASH): A Pilot Trial. Therapeutic advances in gastroenterology, 2(3), 157–163. https://doi.org/10.1177/1756283X09105462[↩]
- Belfort R, Harrison SA, Brown K, Darland C, Finch J, Hardies J, Balas B, Gastaldelli A, Tio F, Pulcini J, Berria R, Ma JZ, Dwivedi S, Havranek R, Fincke C, DeFronzo R, Bannayan GA, Schenker S, Cusi K. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med. 2006 Nov 30;355(22):2297-307. doi: 10.1056/NEJMoa060326[↩]
- Sanyal, A. J., Chalasani, N., Kowdley, K. V., McCullough, A., Diehl, A. M., Bass, N. M., Neuschwander-Tetri, B. A., Lavine, J. E., Tonascia, J., Unalp, A., Van Natta, M., Clark, J., Brunt, E. M., Kleiner, D. E., Hoofnagle, J. H., Robuck, P. R., & NASH CRN (2010). Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. The New England journal of medicine, 362(18), 1675–1685. https://doi.org/10.1056/NEJMoa0907929[↩][↩][↩]
- Cusi K, Orsak B, Bril F, Lomonaco R, Hecht J, Ortiz-Lopez C, Tio F, Hardies J, Darland C, Musi N, Webb A, Portillo-Sanchez P. Long-Term Pioglitazone Treatment for Patients With Nonalcoholic Steatohepatitis and Prediabetes or Type 2 Diabetes Mellitus: A Randomized Trial. Ann Intern Med. 2016 Sep 6;165(5):305-15. doi: 10.7326/M15-1774[↩]
- Abner, E. L., Schmitt, F. A., Mendiondo, M. S., Marcum, J. L., & Kryscio, R. J. (2011). Vitamin E and all-cause mortality: a meta-analysis. Current aging science, 4(2), 158–170. https://doi.org/10.2174/1874609811104020158[↩][↩]
- Chitturi S, Wong VW, Chan WK, Wong GL, Wong SK, Sollano J, Ni YH, Liu CJ, Lin YC, Lesmana LA, Kim SU, Hashimoto E, Hamaguchi M, Goh KL, Fan J, Duseja A, Dan YY, Chawla Y, Farrell G, Chan HL. The Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease guidelines 2017-Part 2: Management and special groups. J Gastroenterol Hepatol. 2018 Jan;33(1):86-98. doi: 10.1111/jgh.13856[↩][↩][↩]
- Miller ER 3rd, Pastor-Barriuso R, Dalal D, Riemersma RA, Appel LJ, Guallar E. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med. 2005 Jan 4;142(1):37-46. doi: 10.7326/0003-4819-142-1-200501040-00110[↩]
- Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, Lau DC, le Roux CW, Violante Ortiz R, Jensen CB, Wilding JP; SCALE Obesity and Prediabetes NN8022-1839 Study Group. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N Engl J Med. 2015 Jul 2;373(1):11-22. doi: 10.1056/NEJMoa1411892[↩]
- Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, Hazlehurst JM, Guo K; LEAN trial team, Abouda G, Aldersley MA, Stocken D, Gough SC, Tomlinson JW, Brown RM, Hübscher SG, Newsome PN. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016 Feb 13;387(10019):679-690. doi: 10.1016/S0140-6736(15)00803-X[↩]
- Newsome, P., Francque, S., Harrison, S., Ratziu, V., Van Gaal, L., Calanna, S., Hansen, M., Linder, M., & Sanyal, A. (2019). Effect of semaglutide on liver enzymes and markers of inflammation in subjects with type 2 diabetes and/or obesity. Alimentary pharmacology & therapeutics, 50(2), 193–203. https://doi.org/10.1111/apt.15316[↩]
- Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, Sanyal AJ, Sejling AS, Harrison SA; NN9931-4296 Investigators. A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis. N Engl J Med. 2021 Mar 25;384(12):1113-1124. doi: 10.1056/NEJMoa2028395[↩]
- Kim YG, Hahn S, Oh TJ, Park KS, Cho YM. Differences in the HbA1c-lowering efficacy of glucagon-like peptide-1 analogues between Asians and non-Asians: a systematic review and meta-analysis. Diabetes Obes Metab. 2014 Oct;16(10):900-9. doi: 10.1111/dom.12293[↩]
- Ingwersen SH, Petri KC, Tandon N, Yoon KH, Chen L, Vora J, Yang W. Liraglutide pharmacokinetics and dose-exposure response in Asian subjects with Type 2 diabetes from China, India and South Korea. Diabetes Res Clin Pract. 2015 Apr;108(1):113-9. doi: 10.1016/j.diabres.2015.01.001[↩]
- Cohen DE, Anania FA, Chalasani N; National Lipid Association Statin Safety Task Force Liver Expert Panel. An assessment of statin safety by hepatologists. Am J Cardiol. 2006 Apr 17;97(8A):77C-81C. doi: 10.1016/j.amjcard.2005.12.014[↩]
- Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 24;129(25 Suppl 2):S1-45. doi: 10.1161/01.cir.0000437738.63853.7a. Epub 2013 Nov 12. Erratum in: Circulation. 2014 Jun 24;129(25 Suppl 2):S46-8. Erratum in: Circulation. 2015 Dec 22;132(25):e396[↩]
- Flora K, Hahn M, Rosen H, Benner K. Milk thistle (Silybum marianum) for the therapy of liver disease. Am J Gastroenterol. 1998 Feb;93(2):139-43. doi: 10.1111/j.1572-0241.1998.00139.x[↩]
- Wah Kheong C, Nik Mustapha NR, Mahadeva S. A Randomized Trial of Silymarin for the Treatment of Nonalcoholic Steatohepatitis. Clin Gastroenterol Hepatol. 2017 Dec;15(12):1940-1949.e8. doi: 10.1016/j.cgh.2017.04.016[↩][↩]
- Francque SM, Marchesini G, Kautz A, Walmsley M, Dorner R, Lazarus JV, Zelber-Sagi S, Hallsworth K, Busetto L, Frühbeck G, Dicker D, Woodward E, Korenjak M, Willemse J, Koek GH, Vinker S, Ungan M, Mendive JM, Lionis C. Non-alcoholic fatty liver disease: A patient guideline. JHEP Rep. 2021 Sep 17;3(5):100322. doi: 10.1016/j.jhepr.2021.100322[↩]
- Sayiner M, Koenig A, Henry L, Younossi ZM. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis in the United States and the Rest of the World. Clin Liver Dis. 2016 May;20(2):205-14. doi: 10.1016/j.cld.2015.10.001[↩][↩]
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016 Jul;64(1):73-84. doi: 10.1002/hep.28431[↩]
- Ge X, Zheng L, Wang M, Du Y, Jiang J. Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990-2017: a population-based observational study. BMJ Open. 2020 Aug 3;10(8):e036663. doi: 10.1136/bmjopen-2019-036663[↩][↩]
- Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E, Wai-Sun Wong V, Yilmaz Y, George J, Fan J, Vos MB. Global Perspectives on Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Hepatology. 2019 Jun;69(6):2672-2682. doi: 10.1002/hep.30251[↩]
- Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, George J, Bugianesi E. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018 Jan;15(1):11-20. doi: 10.1038/nrgastro.2017.109[↩]
- Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018 Jan;67(1):123-133. doi: 10.1002/hep.29466[↩]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016 Apr 9;387(10027):1513-1530. doi: 10.1016/S0140-6736(16)00618-8. Epub 2016 Apr 6. Erratum in: Lancet. 2017 Feb 4;389(10068):e2. doi: 10.1016/S0140-6736(16)32060-8[↩]
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014 Aug 30;384(9945):766-81. doi: 10.1016/S0140-6736(14)60460-8. Epub 2014 May 29. Erratum in: Lancet. 2014 Aug 30;384(9945):746.[↩]
- Le MH, Yeo YH, Li X, Li J, et al. 2019 Global NAFLD Prevalence: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2022 Dec;20(12):2809-2817.e28. doi: 10.1016/j.cgh.2021.12.002[↩][↩]
- Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021 Apr;18(4):223-238. doi: 10.1038/s41575-020-00381-6[↩]
- Alexander M, Loomis AK, Fairburn-Beech J, van der Lei J, Duarte-Salles T, Prieto-Alhambra D, Ansell D, Pasqua A, Lapi F, Rijnbeek P, Mosseveld M, Avillach P, Egger P, Kendrick S, Waterworth DM, Sattar N, Alazawi W. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018 Aug 13;16(1):130. doi: 10.1186/s12916-018-1103-x[↩]
- Teng ML, Ng CH, Huang DQ, Chan KE, Tan DJ, Lim WH, Yang JD, Tan E, Muthiah MD. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2023 Feb;29(Suppl):S32-S42. doi: 10.3350/cmh.2022.0365[↩]
- Mitra S, De A, Chowdhury A. Epidemiology of non-alcoholic and alcoholic fatty liver diseases. Transl Gastroenterol Hepatol. 2020 Apr 5;5:16. doi: 10.21037/tgh.2019.09.08[↩]
- Lu FB, Hu ED, Xu LM, Chen L, Wu JL, Li H, Chen DZ, Chen YP. The relationship between obesity and the severity of non-alcoholic fatty liver disease: systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2018 May;12(5):491-502. doi: 10.1080/17474124.2018.1460202[↩]
- Ayonrinde OT, Oddy WH, Adams LA, Mori TA, Beilin LJ, de Klerk N, Olynyk JK. Infant nutrition and maternal obesity influence the risk of non-alcoholic fatty liver disease in adolescents. J Hepatol. 2017 Sep;67(3):568-576. doi: 10.1016/j.jhep.2017.03.029[↩]
- Cusi K, Sanyal AJ, Zhang S, Hartman ML, Bue-Valleskey JM, Hoogwerf BJ, Haupt A. Non-alcoholic fatty liver disease (NAFLD) prevalence and its metabolic associations in patients with type 1 diabetes and type 2 diabetes. Diabetes Obes Metab. 2017 Nov;19(11):1630-1634. doi: 10.1111/dom.12973[↩]
- Zelber-Sagi S, Ivancovsky-Wajcman D, Fliss Isakov N, Webb M, Orenstein D, Shibolet O, Kariv R. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J Hepatol. 2018 Jun;68(6):1239-1246. doi: 10.1016/j.jhep.2018.01.015[↩]
- Mitchell T, McKinnon E, Ayonrinde O, Adams LA, Trinder D, Chua ACG, Newton RU, Straker L, Olynyk JK. Decreased Physical Working Capacity in Adolescents With Nonalcoholic Fatty Liver Disease Associates With Reduced Iron Availability. Clin Gastroenterol Hepatol. 2020 Jun;18(7):1584-1591. doi: 10.1016/j.cgh.2019.10.017[↩]
- Stefan N, Häring HU, Cusi K. Non-alcoholic fatty liver disease: causes, diagnosis, cardiometabolic consequences, and treatment strategies. Lancet Diabetes Endocrinol. 2019 Apr;7(4):313-324. doi: 10.1016/S2213-8587(18)30154-2[↩]
- Stefan N, Kantartzis K, Häring HU. Causes and metabolic consequences of Fatty liver. Endocr Rev. 2008 Dec;29(7):939-60. doi: 10.1210/er.2008-0009[↩][↩]
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi:10.1002/hep.28431[↩][↩][↩][↩]
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi:10.1002/hep.29367[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Nonalcoholic Fatty Liver Disease (NAFLD) & NASH. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash[↩][↩][↩]
- Nonalcoholic fatty liver disease. https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567[↩][↩]
- Cotter TG, Rinella M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology. 2020;158(7):1851–1864. doi:10.1053/j.gastro.2020.01.052[↩]
- Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. Journal of Hepatology. 2006;45(4):600–606. doi: 10.1016/j.jhep.2006.06.013[↩]
- Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388–1393. doi: 10.1542/peds.2006-1212[↩]
- Golabi P, Paik J, Hwang JP, Wang S, Lee HM, Younossi ZM. Prevalence and outcomes of non-alcoholic fatty liver disease (NAFLD) among Asian American adults in the United States. Liver International. 2019;39(4):748–757. doi:10.1111/liv.14038[↩][↩]
- Khoonsari M, Mohammad Hosseini Azar M, Ghavam R, Hatami K, Asobar M, Gholami A, Rajabi A, Safarnezhad Tameshkel F, Amirkalali B, Sohrabi M. Clinical Manifestations and Diagnosis of Nonalcoholic Fatty Liver Disease. Iran J Pathol. 2017 Spring;12(2):99-105. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5831064[↩]
- Petagine L, Zariwala MG, Patel VB. Non-alcoholic fatty liver disease: Immunological mechanisms and current treatments. World J Gastroenterol. 2023 Aug 28;29(32):4831-4850. doi: 10.3748/wjg.v29.i32.4831[↩][↩][↩][↩][↩][↩][↩]
- Mantovani A, Dalbeni A. Treatments for NAFLD: State of Art. Int J Mol Sci. 2021 Feb 26;22(5):2350. doi: 10.3390/ijms22052350[↩][↩]
- Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, Friedman SL, Diago M, Romero-Gomez M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015 Aug;149(2):367-78.e5; quiz e14-5. doi: 10.1053/j.gastro.2015.04.005[↩][↩][↩][↩]
- Moore MP, Cunningham RP, Dashek RJ, Mucinski JM, Rector RS. A Fad too Far? Dietary Strategies for the Prevention and Treatment of NAFLD. Obesity (Silver Spring). 2020 Oct;28(10):1843-1852. doi: 10.1002/oby.22964[↩][↩][↩][↩]
- Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ; American Gastroenterological Association; American Association for the Study of Liver Diseases; American College of Gastroenterologyh. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012 Jun;142(7):1592-609. doi: 10.1053/j.gastro.2012.04.001 Erratum in: Gastroenterology. 2012 Aug;143(2):503.[↩][↩]
- Pouwels S, Sakran N, Graham Y, Leal A, Pintar T, Yang W, Kassir R, Singhal R, Mahawar K, Ramnarain D. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC Endocr Disord. 2022 Mar 14;22(1):63. doi: 10.1186/s12902-022-00980-1[↩][↩][↩][↩]
- Wong VW, Chan RS, Wong GL, Cheung BH, Chu WC, Yeung DK, Chim AM, Lai JW, Li LS, Sea MM, Chan FK, Sung JJ, Woo J, Chan HL. Community-based lifestyle modification programme for non-alcoholic fatty liver disease: a randomized controlled trial. J Hepatol. 2013 Sep;59(3):536-42. doi: 10.1016/j.jhep.2013.04.013[↩][↩]
- Kudaravalli P, John S. Nonalcoholic Fatty Liver. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541033[↩][↩][↩][↩][↩][↩]
- Kim CH, Younossi ZM. Nonalcoholic fatty liver disease: a manifestation of the metabolic syndrome. Cleve Clin J Med. 2008 Oct;75(10):721-8. doi: 10.3949/ccjm.75.10.721[↩][↩]
- Rector RS, Thyfault JP, Wei Y, Ibdah JA. Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol. 2008 Jan 14;14(2):185-92. doi: 10.3748/wjg.14.185[↩][↩]
- Brennan PN, Elsharkawy AM, Kendall TJ, Loomba R, Mann DA, Fallowfield JA. Antifibrotic therapy in nonalcoholic steatohepatitis: time for a human-centric approach. Nat Rev Gastroenterol Hepatol. 2023 Oct;20(10):679-688. doi: 10.1038/s41575-023-00796-x[↩][↩]
- Kim K, Kim KH. Targeting of Secretory Proteins as a Therapeutic Strategy for Treatment of Nonalcoholic Steatohepatitis (NASH). Int J Mol Sci. 2020 Mar 26;21(7):2296. doi: 10.3390/ijms21072296[↩][↩]
- PNPLA3 gene. https://medlineplus.gov/genetics/gene/pnpla3[↩][↩]
- Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999 Sep;94(9):2467-74. doi: 10.1111/j.1572-0241.1999.01377.x[↩][↩]
- Brown GT, Kleiner DE. Histopathology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Metabolism. 2016 Aug;65(8):1080-6. doi: 10.1016/j.metabol.2015.11.008[↩][↩]
- Takahashi Y, Fukusato T. Histopathology of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014 Nov 14;20(42):15539-48. doi: 10.3748/wjg.v20.i42.15539[↩][↩]
- Nassir F, Rector RS, Hammoud GM, Ibdah JA. Pathogenesis and Prevention of Hepatic Steatosis. Gastroenterol Hepatol (N Y). 2015 Mar;11(3):167-75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836586[↩][↩]
- Qayyum A, Nystrom M, Noworolski SM, Chu P, Mohanty A, Merriman R. MRI steatosis grading: development and initial validation of a color mapping system. AJR Am J Roentgenol. 2012 Mar;198(3):582-8. doi: 10.2214/AJR.11.6729[↩][↩]
- Hardy T, Oakley F, Anstee QM, Day CP. Nonalcoholic Fatty Liver Disease: Pathogenesis and Disease Spectrum. Annu Rev Pathol. 2016 May 23;11:451-96. doi: 10.1146/annurev-pathol-012615-044224[↩]
- Heyens LJM, Busschots D, Koek GH, Robaeys G, Francque S. Liver Fibrosis in Non-alcoholic Fatty Liver Disease: From Liver Biopsy to Non-invasive Biomarkers in Diagnosis and Treatment. Front Med (Lausanne). 2021 Apr 14;8:615978. doi: 10.3389/fmed.2021.615978[↩][↩]
- El-Kamary SS, Mohamed MM, El-Raziky M, Shardell MD, Shaker OG, ElAkel WA, Esmat G. Liver fibrosis staging through a stepwise analysis of non-invasive markers (FibroSteps) in patients with chronic hepatitis C infection. Liver Int. 2013 Aug;33(7):982-90. doi: 10.1111/liv.12139[↩]
- Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005 Feb;115(2):209-18. doi: 10.1172/JCI24282. Erratum in: J Clin Invest. 2005 Apr;115(4):1100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC546435[↩]
- Shetty A, Jun Yum J, Saab S. The Gastroenterologist’s Guide to Preventive Management of Compensated Cirrhosis. Gastroenterol Hepatol (N Y). 2019 Aug;15(8):423-430. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6771034[↩][↩]
- Piazzolla VA, Mangia A. Noninvasive Diagnosis of NAFLD and NASH. Cells. 2020 Apr 17;9(4):1005. doi: 10.3390/cells9041005[↩][↩]
- Kumar R, Teo EK, How CH, Wong TY, Ang TL. A practical clinical approach to liver fibrosis. Singapore Med J. 2018 Dec;59(12):628-633. doi: 10.11622/smedj.2018145[↩][↩][↩][↩]
- Watanabe M, Tozzi R, Risi R, Tuccinardi D, Mariani S, Basciani S, Spera G, Lubrano C, Gnessi L. Beneficial effects of the ketogenic diet on nonalcoholic fatty liver disease: A comprehensive review of the literature. Obes Rev. 2020 Aug;21(8):e13024. doi: 10.1111/obr.13024[↩][↩]
- Schugar RC, Crawford PA. Low-carbohydrate ketogenic diets, glucose homeostasis, and nonalcoholic fatty liver disease. Curr Opin Clin Nutr Metab Care. 2012 Jul;15(4):374-80. doi: 10.1097/MCO.0b013e3283547157[↩]
- Cooper ID, Brookler KH, Kyriakidou Y, Elliott BT, Crofts CAP. Metabolic Phenotypes and Step by Step Evolution of Type 2 Diabetes: A New Paradigm. Biomedicines. 2021 Jul 9;9(7):800. doi: 10.3390/biomedicines9070800[↩]
- Luukkonen PK, Dufour S, Lyu K, Zhang XM, Hakkarainen A, Lehtimäki TE, Cline GW, Petersen KF, Shulman GI, Yki-Järvinen H. Effect of a ketogenic diet on hepatic steatosis and hepatic mitochondrial metabolism in nonalcoholic fatty liver disease. Proc Natl Acad Sci U S A. 2020 Mar 31;117(13):7347-7354. doi: 10.1073/pnas.1922344117[↩][↩]
- Achanta LB, Rae CD. β-Hydroxybutyrate in the Brain: One Molecule, Multiple Mechanisms. Neurochem Res. 2017 Jan;42(1):35-49. doi: 10.1007/s11064-016-2099-2[↩]
- Wu Y, Teng Y, Zhang C, Pan Y, Zhang Q, Zhu X, Liu N, Su X, Lin J. The ketone body β-hydroxybutyrate alleviates CoCrMo alloy particles induced osteolysis by regulating NLRP3 inflammasome and osteoclast differentiation. J Nanobiotechnology. 2022 Mar 9;20(1):120. doi: 10.1186/s12951-022-01320-0[↩]
- Miller VJ, Villamena FA, Volek JS. Nutritional Ketosis and Mitohormesis: Potential Implications for Mitochondrial Function and Human Health. J Nutr Metab. 2018 Feb 11;2018:5157645. doi: 10.1155/2018/5157645[↩]
- National Guideline Centre (UK). Non-Alcoholic Fatty Liver Disease: Assessment and Management. London: National Institute for Health and Care Excellence (NICE); 2016 Jul. (NICE Guideline, No. 49.) 17, Pharmacological interventions. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384725[↩]
- O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, Crosthwaite G, Brown W. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg. 2019 Jan;29(1):3-14. doi: 10.1007/s11695-018-3525-0[↩]
- Głuszyńska P, Lemancewicz D, Dzięcioł JB, Razak Hady H. Non-Alcoholic Fatty Liver Disease (NAFLD) and Bariatric/Metabolic Surgery as Its Treatment Option: A Review. J Clin Med. 2021 Dec 7;10(24):5721. doi: 10.3390/jcm10245721[↩][↩][↩]
- Lee KC, Wu PS, Lin HC. Pathogenesis and treatment of non-alcoholic steatohepatitis and its fibrosis. Clin Mol Hepatol. 2023 Jan;29(1):77-98. doi: 10.3350/cmh.2022.0237[↩][↩]
- Lee Y, Doumouras AG, Yu J, Brar K, Banfield L, Gmora S, Anvari M, Hong D. Complete Resolution of Nonalcoholic Fatty Liver Disease After Bariatric Surgery: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2019 May;17(6):1040-1060.e11. doi: 10.1016/j.cgh.2018.10.017[↩]
- Fakhry TK, Mhaskar R, Schwitalla T, Muradova E, Gonzalvo JP, Murr MM. Bariatric surgery improves nonalcoholic fatty liver disease: a contemporary systematic review and meta-analysis. Surg Obes Relat Dis. 2019 Mar;15(3):502-511. doi: 10.1016/j.soard.2018.12.002[↩]
- Baldwin D, Chennakesavalu M, Gangemi A. Systematic review and meta-analysis of Roux-en-Y gastric bypass against laparoscopic sleeve gastrectomy for amelioration of NAFLD using four criteria. Surg Obes Relat Dis. 2019 Dec;15(12):2123-2130. doi: 10.1016/j.soard.2019.09.060[↩]
- Pedersen JS, Rygg MO, Serizawa RR, Kristiansen VB, Albrechtsen NJW, Gluud LL, Madsbad S, Bendtsen F. Effects of Roux-en-Y Gastric Bypass and Sleeve Gastrectomy on Non-Alcoholic Fatty Liver Disease: A 12-Month Follow-Up Study with Paired Liver Biopsies. J Clin Med. 2021 Aug 24;10(17):3783. doi: 10.3390/jcm10173783[↩]
- Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005 Jul;129(1):113-21. doi: 10.1053/j.gastro.2005.04.014[↩][↩]
- Rafiq N, Bai C, Fang Y, Srishord M, McCullough A, Gramlich T, Younossi ZM. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009 Feb;7(2):234-8. doi: 10.1016/j.cgh.2008.11.005[↩][↩]
- Söderberg C, Stål P, Askling J, Glaumann H, Lindberg G, Marmur J, Hultcrantz R. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010 Feb;51(2):595-602. doi: 10.1002/hep.23314[↩]
- Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008 Oct;49(4):608-12. doi: 10.1016/j.jhep.2008.06.018[↩][↩]
- Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014 Sep 28;20(36):12956-80. doi: 10.3748/wjg.v20.i36.12956[↩][↩]
- Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011 Dec;43(8):617-49. doi: 10.3109/07853890.2010.518623[↩][↩]
- Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999 Jun;116(6):1413-9. doi: 10.1016/s0016-5085(99)70506-8[↩]
- Ekstedt M, Franzén LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006 Oct;44(4):865-73. doi: 10.1002/hep.21327[↩][↩][↩][↩][↩]
- Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999 Dec;30(6):1356-62. doi: 10.1002/hep.510300604[↩]
- Noureddin M, Yates KP, Vaughn IA, Neuschwander-Tetri BA, Sanyal AJ, McCullough A, Merriman R, Hameed B, Doo E, Kleiner DE, Behling C, Loomba R; NASH CRN. Clinical and histological determinants of nonalcoholic steatohepatitis and advanced fibrosis in elderly patients. Hepatology. 2013 Nov;58(5):1644-54. doi: 10.1002/hep.26465[↩]
- Wong VW, Wong GL, Choi PC, Chan AW, Li MK, Chan HY, Chim AM, Yu J, Sung JJ, Chan HL. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010 Jul;59(7):969-74. doi: 10.1136/gut.2009.205088[↩]
- Nakahara T, Hyogo H, Yoneda M, Sumida Y, Eguchi Y, Fujii H, Ono M, Kawaguchi T, Imajo K, Aikata H, Tanaka S, Kanemasa K, Fujimoto K, Anzai K, Saibara T, Sata M, Nakajima A, Itoh Y, Chayama K, Okanoue T; Japan Study Group of Nonalcoholic Fatty Liver Disease. Type 2 diabetes mellitus is associated with the fibrosis severity in patients with nonalcoholic fatty liver disease in a large retrospective cohort of Japanese patients. J Gastroenterol. 2014 Nov;49(11):1477-84. doi: 10.1007/s00535-013-0911-1[↩]
- Dixon JB, Bhathal PS, O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001 Jul;121(1):91-100. doi: 10.1053/gast.2001.25540[↩]
- White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012 Dec;10(12):1342-1359.e2. doi: 10.1016/j.cgh.2012.10.001[↩][↩]
- Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013 Nov;10(11):656-65. doi: 10.1038/nrgastro.2013.183[↩]
- Yasui K, Hashimoto E, Tokushige K, Koike K, Shima T, Kanbara Y, Saibara T, Uto H, Takami S, Kawanaka M, Komorizono Y, Okanoue T; Japan NASH Study Group. Clinical and pathological progression of non-alcoholic steatohepatitis to hepatocellular carcinoma. Hepatol Res. 2012 Aug;42(8):767-73. doi: 10.1111/j.1872-034X.2012.00986.x[↩]
- Guzman G, Brunt EM, Petrovic LM, Chejfec G, Layden TJ, Cotler SJ. Does nonalcoholic fatty liver disease predispose patients to hepatocellular carcinoma in the absence of cirrhosis? Arch Pathol Lab Med. 2008 Nov;132(11):1761-6. doi: 10.5858/132.11.1761[↩]
- Paradis V, Zalinski S, Chelbi E, Guedj N, Degos F, Vilgrain V, Bedossa P, Belghiti J. Hepatocellular carcinomas in patients with metabolic syndrome often develop without significant liver fibrosis: a pathological analysis. Hepatology. 2009 Mar;49(3):851-9. doi: 10.1002/hep.22734[↩]
- Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980 Jul;55(7):434-8.[↩][↩][↩][↩][↩]
- Anderson, M.L. (2006), Treating NASH. Journal of Gastroenterology and Hepatology, 21: 14-14. https://doi.org/10.1111/j.1440-1746.2005.04216.x[↩]
- CINAR, K., COBAN, S., IDILMAN, R., TUZUN, A., SARIOGLU, M., BEKTAS, M., ERDEN, E., BOZKAYA, H. and OZDEN, A. (2006), Long-term prognosis of nonalcoholic fatty liver disease: Is pharmacological therapy actually necessary?. Journal of Gastroenterology and Hepatology, 21: 169-173. https://doi.org/10.1111/j.1440-1746.2005.04221.x[↩]
- Neuschwander-Tetri BA. Fatty liver and nonalcoholic steatohepatitis. Clin Cornerstone. 2001;3(6):47-57. doi: 10.1016/s1098-3597(01)90078-x[↩]
- Neuschwander-Tetri BA. Evolving pathophysiologic concepts in nonalcoholic steatohepatitis. Curr Gastroenterol Rep. 2002 Feb;4(1):31-6. doi: 10.1007/s11894-002-0035-x[↩][↩]
- Drew L. Fatty liver disease: turning the tide. Nature. 2017 Oct 11;550(7675):S101. https://doi.org/10.1038/550S101a[↩]
- Nonalcoholic Fatty Liver Disease (NAFLD). https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-fatty-liver-disease-nafld[↩]
- Nonalcoholic Steatohepatitis (NASH). https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-steatohepatitis-nash[↩]
- Harrison SA, Bedossa P, Guy CD, et al. MAESTRO-NASH Investigators. A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis. N Engl J Med. 2024 Feb 8;390(6):497-509. doi: 10.1056/NEJMoa2309000[↩]
- Rabelo ACS, Andrade AKL, Costa DC. The Role of Oxidative Stress in Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis of Preclinical Studies. Nutrients. 2024 Apr 15;16(8):1174. doi: 10.3390/nu16081174[↩][↩][↩]
- Salete-Granado D., Carbonell C., Puertas-Miranda D., Vega-Rodríguez V.J., García-Macia M., Herrero A.B., Marcos M. Autophagy, Oxidative Stress, and Alcoholic Liver Disease: A Systematic Review and Potential Clinical Applications. Antioxidants. 2023;12:1425. doi: 10.3390/antiox12071425[↩][↩][↩][↩][↩]
- Zima T., Fialová L., Mestek O., Janebová M., Crkovská J., Malbohan I., Stípek S., Mikulíková L., Popov P. Oxidative stress, metabolism of ethanol and alcohol-related diseases. J. Biomed. Sci. 2001;8:59–70. doi: 10.1007/BF02255972[↩][↩]
- You M., Fischer M., Deeg M.A., Crabb D.W. Ethanol Induces Fatty Acid Synthesis Pathways by Activation of Sterol Regulatory Element-Binding Protein (SREBP) J. Biol. Chem. 2002;277:29342–29347. doi: 10.1074/jbc.M202411200[↩][↩][↩][↩]
- Tan H.K., Yates E., Lilly K., Dhanda A.D. Oxidative Stress in Alcohol-Related Liver Disease. World J. Hepatol. 2020;12:332–349. doi: 10.4254/wjh.v12.i7.332[↩][↩]
- Diesinger T., Buko V., Lautwein A., Dvorsky R., Belonovskaya E., Lukivskaya O., Naruta E., Kirko S., Andreev V., Buckert D. Drug Targeting CYP2E1 for the Treatment of Early-Stage Alcoholic Steatohepatitis. PLoS ONE. 2020;15:e0235990. doi: 10.1371/journal.pone.0235990[↩][↩]
- Lívero F.A.R., Acco A. Molecular Basis of Alcoholic Fatty Liver Disease: From Incidence to Treatment. Hepatol. Res. 2016;46:111–123. doi: 10.1111/hepr.12594[↩][↩]
- Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Bouvard V, Altieri A, Cogliano V; WHO International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of alcoholic beverages. Lancet Oncol. 2007 Apr;8(4):292-3. doi: 10.1016/s1470-2045(07)70099-2[↩][↩]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Alcohol Drinking. Lyon (FR): International Agency for Research on Cancer; 1988. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 44.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK531657[↩]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Personal Habits and Indoor Combustions. Lyon (FR): International Agency for Research on Cancer; 2012. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 100E.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK304391[↩]
- No level of alcohol consumption is safe for our health. https://www.who.int/europe/news/item/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health[↩][↩]
- Gapstur SM, Bouvard V, Nethan ST, Freudenheim JL, Abnet CC, English DR, Rehm J, Balbo S, Buykx P, Crabb D, Conway DI, Islami F, Lachenmeier DW, McGlynn KA, Salaspuro M, Sawada N, Terry MB, Toporcov T, Lauby-Secretan B. The IARC Perspective on Alcohol Reduction or Cessation and Cancer Risk. N Engl J Med. 2023 Dec 28;389(26):2486-2494. doi: 10.1056/NEJMsr2306723[↩]
- Yoo JE, Han K, Shin DW, Kim D, Kim BS, Chun S, Jeon KH, Jung W, Park J, Park JH, Choi KS, Kim JS. Association Between Changes in Alcohol Consumption and Cancer Risk. JAMA Netw Open. 2022 Aug 1;5(8):e2228544. doi: 10.1001/jamanetworkopen.2022.28544[↩]
- Islami F, Goding Sauer A, Miller KD, et al.. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31-54. doi: 10.3322/caac.21440[↩]
- Connor J. Alcohol consumption as a cause of cancer. Addiction. 2017;112(2):222-228. doi: 10.1111/add.13477[↩]
- Ahmad Kiadaliri A, Jarl J, Gavriilidis G, Gerdtham UG. Alcohol drinking cessation and the risk of laryngeal and pharyngeal cancers: a systematic review and meta-analysis. PLoS One. 2013;8(3):e58158. doi: 10.1371/journal.pone.0058158[↩]
- Jarl J, Gerdtham UG. Time pattern of reduction in risk of oesophageal cancer following alcohol cessation: a meta-analysis. Addiction. 2012;107(7):1234-1243. doi: 10.1111/j.1360-0443.2011.03772.x[↩]
- Heckley GA, Jarl J, Asamoah BO, G-Gerdtham U. How the risk of liver cancer changes after alcohol cessation: a review and meta-analysis of the current literature. BMC Cancer. 2011;11:446. doi: 10.1186/1471-2407-11-446[↩]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct 17;396(10258):1223-1249. doi: 10.1016/S0140-6736(20)30752-2[↩]
- Hussen N, Zhu L, Tetangco E, Ellison S. Hepatoptosis in a Patient with Alcoholic Hepatitis. Am J Gastroenterol. 2018 Nov;113(11):1581. doi: 10.1038/s41395-018-0182-9[↩]
- Weiskirchen R, Weiskirchen S, Tacke F. Recent advances in understanding liver fibrosis: bridging basic science and individualized treatment concepts. F1000Res. 2018 Jun 27;7:F1000 Faculty Rev-921. doi: 10.12688/f1000research.14841.1[↩][↩]
- American Liver Foundation. Alcohol-Related Liver Disease. http://www.liverfoundation.org/abouttheliver/info/alcohol[↩][↩][↩][↩][↩]
- Patel R, Mueller M. Alcoholic Liver Disease. [Updated 2023 Jul 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546632[↩][↩][↩][↩]
- U.S. National Library of Medicine. Medline Plus. Alcoholic liver disease. https://medlineplus.gov/ency/article/000281.htm[↩][↩][↩][↩]
- Edula RG, Muthukuru S, Moroianu S, Wang Y, Lingiah V, Fung P, Pyrsopoulos NT. CA-125 Significance in Cirrhosis and Correlation with Disease Severity and Portal Hypertension: A Retrospective Study. J Clin Transl Hepatol. 2018 Sep 28;6(3):241-246. doi: 10.14218/JCTH.2017.00070[↩]
- Haflidadottir S, Jonasson JG, Norland H, Einarsdottir SO, Kleiner DE, Lund SH, Björnsson ES. Long-term follow-up and liver-related death rate in patients with non-alcoholic and alcoholic related fatty liver disease. BMC Gastroenterol. 2014 Sep 27;14:166. doi: 10.1186/1471-230X-14-166[↩]
- Martin AP, Bartels M, Hauss J, Fangmann J. Overview of the MELD score and the UNOS adult liver allocation system. Transplant Proc. 2007 Dec;39(10):3169-74. doi: 10.1016/j.transproceed.2007.04.025[↩]
- Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM, Wolfe RA, Krom R; United Network for Organ Sharing Liver Disease Severity Score Committee. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003 Jan;124(1):91-6. doi: 10.1053/gast.2003.50016[↩]