Flea bites on humans
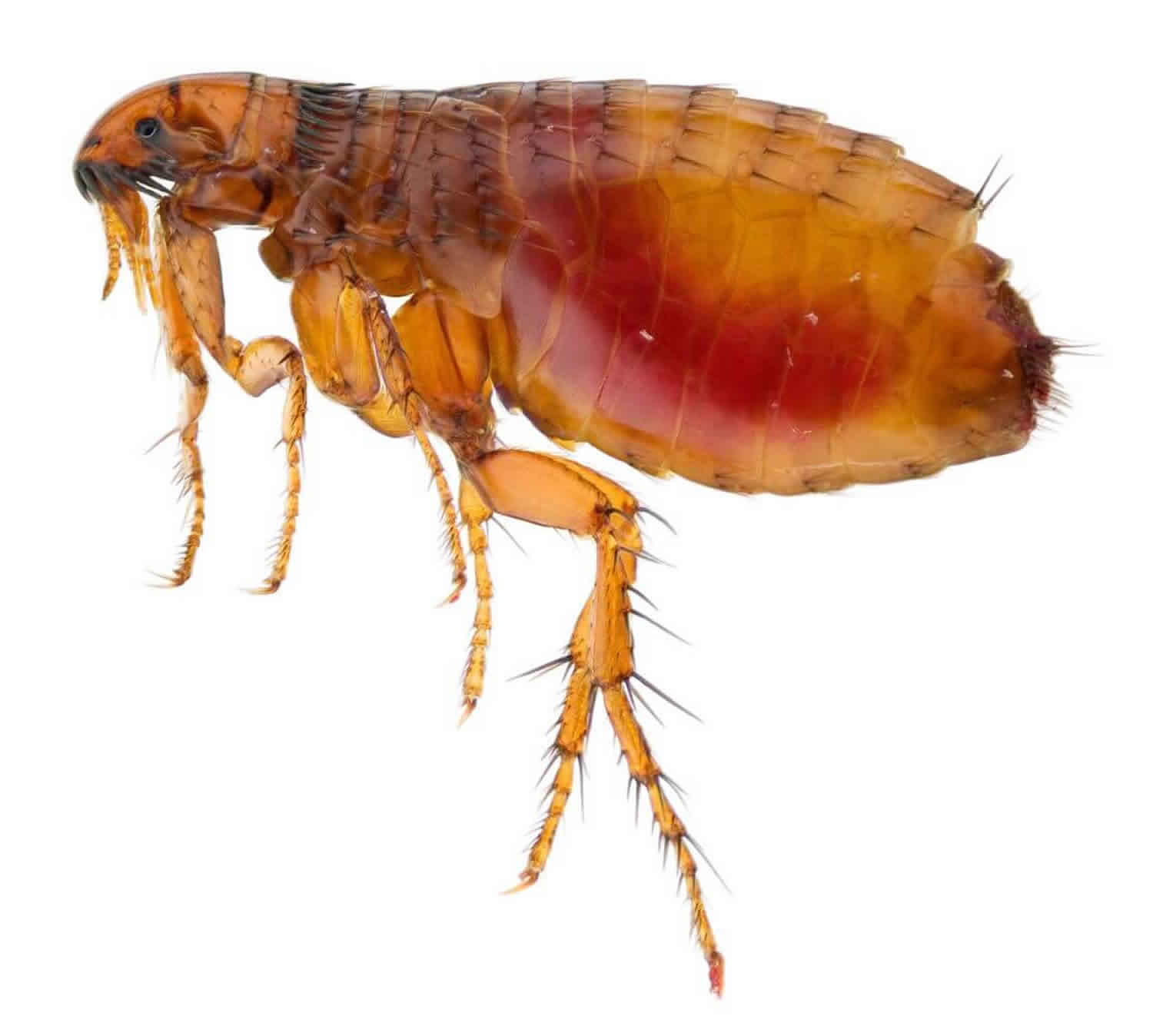
Fleas are insects from the order Siphonaptera, which are bloodsucking wingless insects with more than 2000 species that feed on the blood of humans, dogs, cats, and other warm-blooded animals. Fleas prefer to live on dogs and cats. They may also be found on humans and other warm-blooded animals. Fleas are small, 1–4 mm (1/16 to 1/8 in.) in length, have long hind legs adapted for jumping and blackish-brown 1. Although wingless, fleas are capable of taking giant leaps, jumping to a height of several meters. Adult fleas feed only on blood and are capable of going long periods without feeding. Pet owners may not be bothered by fleas until their pet has been gone for a long period of time. Fleas look for other sources of food and begin to bite humans.
Adult fleas can survive for some months without feeding. The flea uses its saw-like mandibles (jaws) to cut through skin, usually on accessible parts of the body such as the legs or feet. Flea saliva contains anticoagulants to encourage the blood to keep flowing. Female fleas are prompted to lay their eggs after feeding. The eggs are light coloured and oval shaped. The larvae cocoon themselves within weeks of hatching. Vibration, such as footsteps, prompts adult fleas to emerge from their cocoons. This is why you may be bitten after entering a house that has been unoccupied for some time.
The three main species of flea that infest humans are:
- Cat flea (Ctenocephalides felis)
- Dog flea (Ctenocephalides canis)
- Human flea (Pulex irritans).
Fleas that live on humans (Pulex irritans) are relatively uncommon. The species that humans are most likely to encounter is the cat flea (Ctenocephalides felis), which also infests dogs. Humans may also encounter the dog flea (Ctenocephalides canis) or the rat flea (Xenopsylla cheopis). Cat, dog, and rat fleas do not live on people, but they will bite a human if they encounter one and are looking for a blood meal.
Fleas most often bite people around the legs, the ankles and in places where clothes fit close to the body, such as the waist, buttocks, thighs, and lower abdomen. The resulting red bump is an allergic reaction to flea saliva. Flea bites, which are usually but not always felt immediately, become increasingly irritated and may remain sore and/or itchy for as long as a week. Itching may be just at the site of the flea bites or more generalized in nature.
Symptoms of flea bites include:
- Small red bumps, often three bumps together, that are very itchy
- Blisters if the person has an allergy to flea bites
Fleas are predominantly a nuisance to their host causing pruritic local reactions. However, fleas can also act as vectors for disease including typhus, rickettsial disease, bubonic plague, protozoan, and helminth infestations. Understanding these features can help to direct history taking, the physical exam, and treatment options. Additionally, exploring eradication techniques within the human environment can help to reduce the spread of disease from fleas to humans.
Seek medical care if:
- Itch is not alleviated using over-the-counter products
- The bites become infected due to scratching
- Blisters form in reaction to flea bites
- Bites do not resolve in a few weeks
If you develop large, painful lymph nodes and swelling in the groin, armpit or neck, seek medical help, as fleas can transmit the Yersinia pestis bacterium, which causes plague. Endemic plague is seen in the southwestern US (approximately 10-20 cases reported each year in the US) and other parts of the world.
Can a flea bite transmit diseases?
A flea can act as a transporter (called a vector) for other diseases caused by bacteria and viruses. For example:
- Rat fleas (Xenopsylla cheopis and Xenopsylla braziliensis) are known to transmit the bubonic plague and rickettsial typhus.
- Cat fleas may transmit Bartonella henselae, the cause of catscratch fever and bacillary angiomatosis
Tungiasis
The tropical species of sand fleas (Tunga penetrans) burrow into human skin and cause an inflammatory reaction known as tungiasis. Tungiasis typically appears as inflamed papules on the feet, especially in the webspaces between the toes, causing pain, itch and secondary staphylococcal skin infection 2.
Flea bites complications
Fleas are a critical factor in the epidemiologic cycles of several diseases including plague and typhus. As carriers of these diseases, they can spread them to humans through their bites.
Yersinia pestis, also known as the plague, is transmitted by fleas. Humans, after becoming infected with Y. pestis, are considered to be hosts but do not play an instrumental role in the natural disease cycle. In the United States, Yersinia pestis is most common in the south-western and Pacific coast states; however, the incidence of plague is low in the United States given that many of the regions affected are uninhabited 3. While there are numerous routes of transmission of the plague to humans, flea bites remain the most common. Various mammalian species are carriers of the plague including cats, dogs, squirrels, mice, and rats 4. Yersinia pestis, a gram-negative coccobacillus, manifests initially as regional lymphadenopathy secondary to an invasion of the lymphatic system. These inflamed lymph nodes are called buboes. Subsequent disease progression presents itself as pneumonia, hemorrhagic lesions, purpuric skin lesions, and sepsis secondary to bacteremia 5. Treatment includes gentamycin and fluoroquinolones as first-line agents.
Murine typhus is transmitted by fleas, primarily the rat flea, Xenopsylla cheopis. It also spreads by the mouse flea, Leptopsyllia segnis, and the cat flea, Ctenocephalides. Inoculation of humans occurs through the contamination of bite wounds with the feces of infected fleas. In the United States, Rickettsia typhi highly correlates with areas with large rat populations. Rickettsia typhi and Rickettsia felis are also found to be maintained by domestic cats and opossums in suburban settings 6. While Rickettsia felis does not cause murine typhus, the presentation of its infection is clinically indistinguishable from those of murine typhus. Manifestations include fever, headache, chills, myalgias, and other non-specific symptoms. A faint, maculopapular rash may also occur, spreading centrifugally but sparring the palms and soles 7. Complications may occur in those with severe comorbidities including hepatic, cardiac, pulmonary, renal, and neurologic dysfunction 7. Patient with uncomplicated typhus may receive treatment with doxycycline, which is more effective than azithromycin 8. Chloramphenicol may be an option as a third-line agent 9.
Risk factors for flea bites
Risk factors for flea bites include:
- close contact with infested household pets, livestock, and rodent infestation;
- visiting an unoccupied building that has previously housed infested pets – fleas can be found in the floorboards and carpets.
Species that primarily infest cats and dogs may bite humans if they have been starved since their last blood meal. Vibrations, e.g. from footsteps when entering a house, can also stimulate adult fleas to emerge from cocoons (pupal stage) and result in human bites.
Fleas typically bite when they come in contact with a host, commonly a cat or dog as well as other wildlife species including foxes and rats 10. Fleas feed off of the host’s blood and lay eggs in their fur. Ultimately, the flea’s eggs fall off of the animal allowing them to hatch in the host’s surrounding environment and perpetuating their lifecycle.
Some people are more sensitive to flea bites than others, and it can sometimes appear that the fleas are “picking on” one individual in a household but not others. Children aged younger than 10 are generally more sensitive than older people, as people tend to become desensitized by repeated exposure over time. Flea bites in children produce an allergic reaction in which recurrent or chronic small red bumps occur on the exposed skin areas. Individuals who are hypersensitive to fleas may also develop blister reactions.
Fleas are prevalent among mammals worldwide. In the developed world, the most influential vectors are household pets, specifically cats and dogs 11. In the developing world, fleas are a significant cause of papular urticaria, especially in tropical regions; this is seen most commonly in pediatric patients with a frequency of 2.4 to 16.3%. While other insects can also cause a similar rash, fleas are one of the most frequent causes. In most patients, the rash improves by age 7, though in some cases it can last into adulthood 12.
Tunga penetrans, also known as the chigoe or jigger flea, is a parasitic flea infestation found in tropical and subtropical climates including Africa, South America, and Central America 1. It is most common in underdeveloped and impoverished regions. Though rare in the United States and Europe despite global travel, it should be considered in patients returning from endemic regions. Peak incidence occurs during the dry season between August and September. Typically only adults are affected. Domestic and wild animals act as reservoirs of disease 13.
Flea life cycle
The life cycle of the flea consists of four main stages: egg, larva, pupa, and adult.
The adult flea survives exclusively through blood meals from its host. During feeding, the flea has a specialized mouthpiece that punctures intact skin and syphons blood. It simultaneously secretes saliva, which can be very antigenic (allergy-inducing). The saliva helps to prevent the host’s blood from clotting, which facilitates their feeding.
A flea has three pairs of legs, with long hind legs ideal for jumping. They are wingless. They can jump up to 18 cm in height. Adult fleas of domestic animals tend to live on the animal for easy access to blood meals.
The female fleas lay white, round eggs that tend to fall off the animal onto bedding, floor and soil. The emerging larva feeds on organic material in a moist environment including the faeces of adult fleas. After sufficient growth and development, the larva spins itself a cocoon and pupates. Cocoons are found in soil, carpets, under furniture and on animal bedding. With the right stimuli, such as warm temperatures, high humidity or vibrations from movement, the pupa emerges from its cocoon as an adult flea 14.
The life cycle of the flea can range from 2 weeks to up to 2 years in duration, and is usually within 8 weeks. Survival depends on adequate temperature and high humidity.
Adult fleas move toward a light source, then jump when the light is shadowed e.g. by a suitable warm-blooded host. The flea starts feeding immediately and is estimated to consume 13.6µL of blood per day. They soon die if removed from the host, and rarely colonize another animal.
Fleas can be hard to see. They are dark and wingless. They are more obvious if they are jumping onto a person wearing white socks. Flea feces (‘flea dirt’) appear as black pepper grains, and, when seen on a damp towel, are red, as a result of blood in the feces.
Household pets and fleas
Dogs and cats are common ‘reservoirs’ for fleas. Your pet may be irritated by flea bites and scratch often. Check for fleas by parting the fur, particularly around the ears and rump. Look for the fleas themselves or for flea feces (poop). Flea feces look like miniscule dark specks. For a positive identification, place a few of the specks on a piece of lightly moistened white tissue. Flea feces will leech a ring of blood into the tissue.
Flea bites prevention
Flea species that primarily infest cats and dogs may bite humans if they have been starved since their last blood meal. Vibrations, e.g. from footsteps when entering a house, can also stimulate adult fleas to emerge from cocoons (pupal stage) and result in human bites.
Prevention of human flea bites is best achieved by:
- Restricting your pet’s indoor (or outdoor) access
- Vacuuming carpets and cleaning bedding
- Regularly combing infested pets
- Keep fleas off of your pets. Use veterinarian-approved flea control products for cats and dogs such as flea collars, oral medication or spot-ons. Permethrin should not be used on cats. Animals that are allowed outside are more likely to come in contact with fleas and could bring them inside.
- Keep rodents and animals (e.g. opossums) away from your home, workplace, and recreational areas:
- Store food, including pet food, in tight sealing containers.
- Remove brush, rock piles, junk, and cluttered firewood outside of your home.
- Seal up holes in your home where rodents can enter.
- Keep tight lids on compost and trash cans.
- Protect yourself from flea bites:
- Do not feed or pet stray or wild animals.
- Always wear gloves if you are handling sick or dead animals.
- Use EPA-registered insect repellents (https://www.epa.gov/insect-repellents/find-repellent-right-you) on your skin and clothing when spending time outside. Always follow instructions listed on the product label.
Flea eggs can survive for several weeks and pets are readily reinfestated, so maintain these strategies long term to prevent perpetuating infestation. Difficult infestations may require the help of a professional exterminator.
If flea bites have occurred indoors, all sources must be treated for effective flea control. Carpets, pet bedding, and all rooms should be thoroughly vacuumed, and pets should be treated separately.
Flea control at home may be regulated by the following measures:
- Bedding should be clean and laundered regularly.
- Bedrooms should be vacuumed regularly, especially in the corners underneath the beds.
- The indoor environment can be sprayed with a chemical used for flea infestation such as methoprene.
- A professional exterminator may be needed.
- Pets should be kept clean and regularly checked by a veterinarian.
Flea control for pets includes the following:
- Oral flea medication (available for dogs but not for cats)
- Monthly topical spot-on products
- Flea collars.
What is used to treat and prevent pet infestations?
Pets carry about 5% of the total flea population and are the main reservoir of adult fleas. To minimise the use of potentially toxic insecticides:
- Inspect your pet for fleas regularly. Examine the base of the pet’s tail, around the neck, in the groin, on the back of the legs and the middle of the back.
- Clean the pet regularly with soapy water.
- Brush frequently using a flea comb; drown the fleas in soapy water.
Ask your veterinarian’s advice about which insecticides should be used for your pet. Prescription chemicals will be different in dogs and cats. Some methods of eliminating fleas from cats and dogs are listed below. Many of these agents are only available from a registered veterinarian.
- Safe topical spot-on anti-adult flea formulations include imidacloprid, fipronil, dinotefuran, metalfumizone and selamectin.
- Oral insecticides targeting the adult flea include nitenpyram or spinosad.
- Monthly insect growth regulators (IGRs) containing methoprene, pyriproxyfen, alsystin, cyromazine, and diflubenzuron and lefenuron do not kill adult fleas but prevent the growth of eggs and larvae. IGRs are available as flea collars, creams, sprays, injections and pills. They are considered safe 15.
Combination products are the most effective insecticides but are more expensive.
The following traditional flea-control agents are toxic to humans and pets and are best avoided (with the exception of permethrin, which may be used in dogs). In addition, insect resistance is increasing to these chemicals.
- Organophosphates (chlorpyrifos, dichlorvos, phosmet, naled, tetrachlorvinphos, diazinon and malathion), carbamates (carbaryl, propoxur)
- Organochlorines
- Pyrethrins and pyrethroids (permethrin, allethrin, tetramethrin, resmethrin, fenvalerate and cypermethrin).
How are fleas eliminated from the environment?
Several measures have been suggested to reduce fleas in the home environment.
- Wash pet bedding once weekly taking care not to spread flea eggs and larvae in the process.
- Vacuum carpet, floor and furniture thoroughly to remove adult fleas, eggs, larvae, and flea faeces. Seal and dispose of or burn vacuum bags to avoid re-infestation.
- Carpet cleaning with steam should be undertaken in case of severe infestation.
- Mow grass frequently in areas where pets spend most time outdoors.
- Discourage visitations by wildlife that might carry fleas.
- Plant a flea bomb, an aerosol fumigator for controlling fleas (follow the directions carefully).
- Consult a pest control specialist to set flea traps and insecticides inside and outside the house.
Flea bites on humans symptoms
Flea bites are most often found around the ankles and lower legs, where the fleas can have access to the skin from jumping height. Other common locations for flea bites include the area around the waist (where there is a gap between shirt and trousers or skirt, armpits), creases of the elbows, and behind the knees.or at the waistband.
Flea bites have certain features, including:
- It is extremely itchy (or pruritus). Flea bites can be extremely itchy and may show signs of bleeding. Scratching can lead to secondary infection.
- A red, swollen weal develops within half an hour of the bite. The redness disappears when pressure is applied.
- After a day or so, the weal (lump) may develop into a blister or small wound.
- The legs and feet are often targeted.
- Secondary infections caused by scratching are common.
- Some people may become hypersensitive (very sensitive) to bites.
Flea bites produce a variety of effects, ranging from a small, temporary itchy red bumps to long-term symptoms that may last for years depending on the sensitivity of the person bitten. The area of skin affected may increase over time, or the rash may spread to a different area. It most commonly affects exposed skin, generally, the feet and ankles and appears in clusters and linear patterns known as a “breakfast, lunch and dinner” pattern 16.
Some individuals mount an excessive immune response (allergy) to flea saliva resulting in a more pronounced or persistent bite reaction called papular urticaria, a form of prurigo. The site of the bite may become red and swell, sometimes with a central blister, which may break becoming oozy and crusted. Old bite marks may reactivate. Anaphylaxis has not been reported.
Flea bites can take a very long time to heal up and can sometimes evolve into “persistent bite reactions.” Itching and swelling may occur at the sites of older bites when the person is bitten again.
Tungiasis is an inflammatory skin condition caused by Tunga penetrans or Chigoe flea which is the smallest known flea. Skin irritation occurs when a female flea embeds itself into the epithelium of the skin. Fleas typically embed themselves in soft areas of skin such as the medial foot, under nails and between toes. In cases of severe disease, the thigh, hands, perianal and groin may be involved. During the first 1 to 2 days of infestation, the host may notice itching or discomfort. The abdomen of the flea then swell with eggs forming a white pearly lesion. This increased pressure can cause a painful foreign body sensation and irritate surrounding neurovascular structures. Following this, the lesion becomes dark and crusted. It may create a honeycomb pattern in more extensive infection which is prone to secondary infection and increases the risk of gangrene and tetanus. After healing, scarring can occur 17.
Tungarisis is usually benign and self-limited, especially in returning travelers. However, patients with extensive infestations may have complications including loss of nails, toe deformities and difficulty ambulating. Due to the high risk of secondary infection, patients with extensive infections should receive treatment with prophylactic antibiotics. In unvaccinated patients, tetanus risk is increased, and the practitioner should query all patients regarding their tetanus status. Conventional therapy is surgical extraction of the parasite under sterile conditions. No oral or topical therapy is entirely effective; however, in mild infections even without treatment the flea will die within 5 weeks and will be sloughed off with the skin. Basic hygiene as well as paving roads and floors can prevent infestation 12.
Allergic reaction to flea bites
Allergy is an abnormal response of the body to a foreign body, known as an antigen. It involves the immune system recognizing this antigen and mounting one of four types of response (type 1 to 4 hypersensitivity reaction or hypersensitivity response.
Allergy is also known as a ‘hypersensitivity reaction’ or a ‘hypersensitivity response’.
An allergy refers to the clinical syndrome while hypersensitivity is a descriptive term for the immunological process.
Most flea bites result in papular urticaria, which is a dual Type 1 and Type 4 hypersensitivity reaction.
Type 1 hypersensitivity reaction
Type 1 hypersensitivity reaction is the most widely known type of allergic reaction and includes anaphylaxis; this is where the body reacts to a stimulus, or allergen, leading to swelling of the airways, and cardiovascular and other organ system effects. True anaphylaxis is uncommon.
Anaphylaxis occurs when a specific type of antibody, immunoglobulin E (IgE), recognizes a foreign antigen and attaches itself to it. By attaching to the antigen, the IgE activates a chain of reactions that result in the widespread release of chemicals, including histamine.
The symptoms of a type 1 hypersensitivity reaction include:
- Urticaria (also known as hives; note that most cases of urticaria are not due to a hypersensitivity reaction)
- Hay fever
- Asthma
- Angioedema — swelling of the face; typically around the eyes and mouth
- Anaphylaxis — this is at the end of the reaction and includes:
- Airway swelling (laryngeal edema)
- Hypotension and resultant shock
- Diarrhea and other organ dysfunction.
Diagnosis of type 1 hypersensitivity reactions
The diagnosis of type I hypersensitivity reactions is largely based on the patient’s clinical history of typical symptoms and signs following exposure to a particular allergen. Tests can aid in confirming the diagnosis.
- A complete blood count may show eosinophilia.
- The serum tryptase level is elevated in most cases of anaphylactic reaction when measured within the first 1–2 hours after the event.
- A radioallergosorbent test (RAST) can be used to identify the causative allergen. This assay detects specific IgE antibodies against a range of common allergens.
RAST has now largely been replaced by fluoroenzyme assays (eg, the ImmunoCAP assay), which are more sensitive at detecting allergen-specific IgE. - Skin prick testing is widely used to test for type 1 hypersensitivity reaction. A small number of common allergens or patient-specific allergens are inoculated directly under the skin. The skin reaction is then compared against a control area to see if a positive (ie, allergic) reaction occurs. Prick testing should not be used to test for an allergen that has caused anaphylaxis or when severe pre-existing skin disease would obscure the result.
- Atopy patch tests are used to determine whether type 1 allergens might be contributing to atopic dermatitis (which is ordinarily not considered due to a specific allergy).
Treatment of type 1 hypersensitivity reactions
Anaphylaxis is a medical emergency requiring prompt recognition and treatment. Treatment of type 1 hypersensitivity reactions include:
- Adrenaline intramuscularly to reverse the airway swelling and cardiovascular effects
- Systemic glucocorticoids to lessen the inflammatory reaction while the body clears the allergen
- Antihistamines to prevent the action of widespread histamine release
- Avoidance of the allergen in future.
People with known anaphylaxis to common environmental triggers (e.g., bee venom or peanuts) may carry a pre-loaded adrenaline syringe or an adrenaline pen (eg, an EpiPen) that allows the rapid and easy injection of adrenaline into the thigh muscle in an emergency.
- Antihistamines are often enough to control mild symptoms (eg, urticaria).
- Topical steroid nasal sprays can be used to control hay fever.
Desensitization
Desensitization can be performed by an allergy specialist (an immunologist with interest in allergy) within the hospital environment. It involves gradually exposing the patient to increasing doses of the allergen (eg, an antibiotic) in an attempt to desensitize the patient’s immune response.
Type 4 hypersensitivity reaction
Type 4 hypersensitivity or delayed hypersensitivity reaction occurs 48–72 hours after exposure to the allergen. Type 4 hypersensitivity reaction does not involve antibodies. Instead, eosinophils, monocytes, or lymphocytes called T cells are activated by the antigen. The helper CD4+ T cells initially recognize the antigen, releasing cytokines that activate the immune system with killer CD8+ T cells to destroy the target cells on contact, and macrophages to wall off the antigen and prevent further damage.
Common examples of cutaneous type 4 hypersensitivity reactions include:
- Allergic contact dermatitis — commonly to hair dye, nickel in jewellery, Toxicodendron spp.(eg, poison ivy, Rhus)
- The Mantoux test (used to detect active tuberculosis)
- Delayed drug reactions, including:
- Morbilliform drug reactions
- Drug hypersensitivity syndrome (formerly known as drug reaction with eosinophilia and systemic symptoms [DRESS])
- Erythema multiforme
- Lichenoid drug eruptions
- Steven–Johnson syndrome (SJS) / toxic epidermal necrolysis (TEN).
Diagnosis of type 4 hypersensitivity reactions
A thorough history and examination are required to identify the likely causative agent when considering a possible allergic contact dermatitis. Diagnosis is confirmed through patch testing (also known as a contact delayed hypersensitivity allergy test).
- Small quantities of the potential allergens are applied to the skin.
- They are left in situ for two days.
- A patch of eczema at the site of an allergen is a positive reaction.
- Atopy patch tests using type 1 allergens are sometimes used in patients with atopic dermatitis.
Treatment of type 4 hypersensitivity reactions
The mainstay of treatment for type 4 hypersensitivity reactions is the avoidance of contact with the causative agent. For example, people with nickel allergy should select jewellery and clothing items that do not contain the metal.
Symptomatic relief of contact dermatitis is achieved through emollients and topical steroids.
Systemic corticosteroids are prescribed for severe reactions and tapered over 2–3 weeks to prevent a recurrence of the rash.
Flea bites diagnosis
Flea bites diagnosis is typically from the history and physical exam. There are no laboratory tests that can confirm fleas as the causal agent of the rash. Confirmation of the diagnosis can instead be via examination of debris from vacuuming and bedding 18. Flea bites typically result in papular urticaria, a rash that manifests as small, raised skin lesions. This reaction typically occurs within minutes of the bite and is characterized by local pruritus, swelling, and erythema. The ankles are the most common areas affected through any exposed skin such as the arms, legs, upper back, and scalp can show the rash. The buttocks, groin, genital, and axillary areas are typically spared. These bites may present in linear clusters referred to as a “breakfast, lunch and dinner” pattern 19.
Flea bites on humans treatment
Skin subjected to flea bites, as with all insect bites, should be washed with soap and water. Local swelling, redness, and itch are symptoms of a hypersensitivity reaction caused by flea bites and are treatable with cold packs and topical creams.
The primary goal of treatment is to relieve the itching, which can be achieved by the following:
- Wash the bites with antiseptic soap to reduce the risk of infection.
- Burow’s solution compresses applied to the bites.
- Apply an icepack frequently to help relieve swelling.
- Calamine lotion or pramoxine-containing lotions to which 0.25% menthol may be added by the pharmacist.
- Anaesthetic creams or similar to treat the itching.
- 1% hydrocortisone cream may take the edge off the itch.
Note that the application of topical antihistamines over large areas of skin should be avoided when oral histamine-1 antihistamines are in use; such a combination can result in systemic anticholinergic toxicity.
Prescription-strength mid- or high-potency topical corticosteroids can alleviate the severe itch.
Antihistamines may be prescribed by your doctor for the relief of the itching. Be aware that some antihistamines cause drowsiness.
- Diphenhydramine hydrochloride (Benadryl®) – 25, 50 mg tablets or capsules, 25–50 mg nightly or every 6 hours as needed
- Cetirizine hydrochloride (Zyrtec®) – 10 mg tablets, 10 mg per day
Pain, redness, oozing, crusting and pustules at the site of a bite indicates secondary bacterial infection, often requiring topical or oral antibiotics.
The rash can take several weeks to resolve.
Seek treatment for possible tapeworm infection, since fleas can transmit this parasite through their bite.
See your doctor if the symptoms worsen or if a secondary infection develops (indicated by discharge of pus from wounds).
Treating your pet for fleas
Infested animals should be treated fortnightly for several weeks. Suggestions on treating your pet include:
- See your veterinarian for a range of appropriate flea-killing products.
- Treatment options include tablets to be swallowed by the animal, and solutions or powders to be applied to their fur.
- Treat your pet for tapeworm, since fleas can transmit this parasite through their bite.
Treating your house for fleas
Your local pest control professionals can offer information and advice on dealing with a flea infestation. Some general suggestions on eliminating fleas yourself include:
- Clean animal bedding and the general surrounds thoroughly.
- Vacuum the carpets. Throw away the vacuum cleaner bag, since it will contain fleas and eggs, or use a surface spray into the bag.
- Use an appropriate spray or ‘flea bomb’ in your house, taking care to follow the label directions carefully.
- Treat outdoor areas commonly used by your pet, such as kennels, with appropriate insecticides, wearing gloves and long-sleeved protective clothing as instructed on the label.
- Repeat the procedure once or twice, since flea eggs can survive for some weeks.
- Maintain hygiene practices (regular vacuuming, keeping pets free of fleas and so on) to prevent another infestation.
- A persistent infestation may need to be treated by a qualified pest control operator.
Flea bites prognosis
Flea bites typically have a benign clinical course. Most patients only experience a mild local reaction called papular urticaria. This rash resolves spontaneously and is manageable with anti-histamines and anti-inflammatory medications. Secondary infections such as cellulitis and abscess are possible and should have treatment per current clinical guidelines. Fleas can be vectors for secondary infections such as Yersinia pestis and murine typhus as well as parasitic infections. The prognosis for these patients is related to the secondary infection and not the flea bite.
References- Anderson J, Paterek E. Flea Bites. [Updated 2019 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541118
- Arthropods in dermatology. J Am Acad Dermatol. 2004 Jun;50(6):819-42, quiz 842-4. https://doi.org/10.1016/j.jaad.2003.12.019
- Kwit N, Nelson C, Kugeler K, Petersen J, Plante L, Yaglom H, Kramer V, Schwartz B, House J, Colton L, Feldpausch A, Drenzek C, Baumbach J, DiMenna M, Fisher E, Debess E, Buttke D, Weinburke M, Percy C, Schriefer M, Gage K, Mead P. Human Plague – United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 2015 Aug 28;64(33):918-9.
- Perry RD, Fetherston JD. Yersinia pestis–etiologic agent of plague. Clin. Microbiol. Rev. 1997 Jan;10(1):35-66.
- Prentice MB, Rahalison L. Plague. Lancet. 2007 Apr 07;369(9568):1196-207.
- Civen R, Ngo V. Murine typhus: an unrecognized suburban vectorborne disease. Clin. Infect. Dis. 2008 Mar 15;46(6):913-8.
- Tsioutis C, Zafeiri M, Avramopoulos A, Prousali E, Miligkos M, Karageorgos SA. Clinical and laboratory characteristics, epidemiology, and outcomes of murine typhus: A systematic review. Acta Trop. 2017 Feb;166:16-24.
- Newton PN, Keolouangkhot V, Lee SJ, Choumlivong K, Sisouphone S, Choumlivong K, Vongsouvath M, Mayxay M, Chansamouth V, Davong V, Phommasone K, Sirisouk J, Blacksell SD, Nawtaisong P, Moore CE, Castonguay-Vanier J, Dittrich S, Rattanavong S, Chang K, Darasavath C, Rattanavong O, Paris DH, Phetsouvanh R. A Prospective, Open-label, Randomized Trial of Doxycycline Versus Azithromycin for the Treatment of Uncomplicated Murine Typhus. Clin. Infect. Dis. 2019 Feb 15;68(5):738-747.
- Shaked Y, Samra Y, Maier MK, Rubinstein E. Relapse of rickettsial Mediterranean spotted fever and murine typhus after treatment with chloramphenicol. J. Infect. 1989 Jan;18(1):35-7.
- Clark NJ, Seddon JM, Šlapeta J, Wells K. Parasite spread at the domestic animal – wildlife interface: anthropogenic habitat use, phylogeny and body mass drive risk of cat and dog flea (Ctenocephalides spp.) infestation in wild mammals. Parasit Vectors. 2018 Jan 08;11(1):8.
- Iannino F, Sulli N, Maitino A, Pascucci I, Pampiglione G, Salucci S. Fleas of dog and cat: species, biology and flea-borne diseases. Vet. Ital. 2017 Dec 29;53(4):277-288.
- Halpert E, Borrero E, Ibañez-Pinilla M, Chaparro P, Molina J, Torres M, García E. Prevalence of papular urticaria caused by flea bites and associated factors in children 1-6 years of age in Bogotá, D.C. World Allergy Organ J. 2017;10(1):36.
- Sanusi ID, Brown EB, Shepard TG, Grafton WD. Tungiasis: report of one case and review of the 14 reported cases in the United States. J. Am. Acad. Dermatol. 1989 May;20(5 Pt 2):941-4.
- Flea bite. https://dermnetnz.org/topics/flea-bite/
- Biology, treatment, and control of flea and tick infestations. Vet Clin North Am Small Anim Pract. 2009 Nov;39(6):1173-200, viii. doi: 10.1016/j.cvsm.2009.07.001 https://doi.org/10.1016/j.cvsm.2009.07.001
- Youssefi MR, Ebrahimpour S, Rezaei M, Ahmadpour E, Rakhshanpour A, Rahimi MT. Dermatitis caused by Ctenocephalides felis (cat flea) in human. Caspian J Intern Med. 2014 Fall;5(4):248-50.
- Cestari TF, Pessato S, Ramos-e-Silva M. Tungiasis and myiasis. Clin. Dermatol. 2007 Mar-Apr;25(2):158-64.
- Singh S, Mann BK. Insect bite reactions. Indian J Dermatol Venereol Leprol. 2013 Mar-Apr;79(2):151-64.
- Peres G, Yugar LBT, Haddad Junior V. Breakfast, lunch, and dinner sign: a hallmark of flea and bedbug bites. An Bras Dermatol. 2018 Sep-Oct;93(5):759-760.