Food sensitivity test
Food sensitivity also known as food intolerance is a broad term that is used to describe a wide range of unwanted reactions (usually digestive system reactions) to certain foods, that cause symptoms after eating some foods 1. Food sensitivity (food intolerance) occurs when something in food irritates a person’s digestive system or when a person is unable to properly digest, or break down, the food. The types of foods that trigger food sensitivity or food intolerance vary from individual to individual. Common foods that may cause food sensitivity include dairy products (e.g., cheddar cheese, cottage cheese, cow’s milk, mozzarella cheese, yogurt); egg white and egg yolk; grains (e.g., barley, bran, brown rice, gluten); fruits (e.g., apple, avocado, banana); meat (e.g., beef, chicken, lamb); and more. Consuming certain foods can cause various symptoms including stomach pain, bloating, gas/flatulence, diarrhea, irritable bowel syndrome (IBS), rashes, hives (urticaria), recurrent mouth ulcers or headaches. Intolerance to lactose, which is found in milk and other dairy products, is the most common food sensitivity or food intolerance affecting about 10 percent of Americans. If food sensitivity (food intolerances) are not properly managed, these symptoms can adversely affect general health and wellbeing. Unfortunately, tests cannot easily identify most food sensitivities. While there are tests are available that look for dozens of types of antibodies called immunoglobulin-G (IgG) in the blood. Experts advise against this type of screening because it has not been shown to be accurate in identifying true food intolerance and sensitivities.
Causes of food sensitivity include:
- Absence of an enzyme needed to fully digest a food. Lactose intolerance is a common example.
- Irritable bowel syndrome (IBS). This chronic condition can cause cramping, constipation and diarrhea.
- Sensitivity to food additives. For example, sulfites used to preserve dried fruit, canned goods and wine can trigger asthma attacks in people who are sensitive to food additives.
Finding the cause of a food sensitivity is not easy. Unfortunately, tests cannot easily identify most food sensitivity. While there are tests are available that look for dozens of types of antibodies called immunoglobulin-G (IgG) in the blood. Experts advise against this type of screening because it has not been shown to be accurate in identifying true food intolerance and sensitivities 2, 3, 4, 5.
Food sensitivities and food intolerances are not the same as food allergies and are sometimes confused with or mislabeled as food allergies. The key difference is that food allergy is an immune system reaction (antibody mediated food allergy). A food allergy is caused by an overreaction of the immune system due to your body mistaking an ingredient in food — usually a protein — as harmful (the allergen) and creates a defense system (antibodies) to attack the allergen. An allergic reaction occurs when the antibodies are battling an “invading” food protein. The most common food allergies are shellfish, nuts, fish, eggs, peanuts, and milk. It should be noted that reactions that do not involve the immune system are not food allergies (e.g., milk intolerance). Anaphylaxis is a very serious and potentially life-threatening allergic reaction that involves a sudden drop in blood pressure, swelling of the airways to the lungs, wheezing, shortness of breath, loss of consciousness and body system failure. If you’ve had allergic reactions to food or insect bites, your doctor will prescribe an epinephrine (adrenaline) injection (Adrenaclick, Auvi-Q, EpiPen) for emergency self-treatment.
With food sensitivities or food intolerances, digestive system reactions are normally predictable and increase based on how much of the food is consumed. Furthermore, food sensitivities or food intolerances (except for sulphite and benzoate reactions) do not cause anaphylaxis (severe allergic reactions), that can be life threatening. In contrast, food allergic reactions (immunoglobulin E [IgE] antibody mediated food allergy) can have unpredictable severity and often occur with minuscule levels of exposure or even just contact with the skin.
Examples of food sensitivities or food intolerances include 6:
- Lactose intolerance
- Non-celiac gluten sensitivity
- Caffeine intolerance
- Alcohol sensitivity
- Intolerance to food additives like sulfites
- Intolerance to short-chain fermentable carbohydrates (FODMAPs – fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) – excess fructose, lactose, sorbitol, mannitol, fructans and galacto-oligosaccharides
- Wheat and/or components of wheat (in the absence of coeliac disease) such as amylase/trypsin inhibitors and wheat lectin agglutinin
- Food chemicals such as salicylates, vasoactive amines (for example, histamine), glutamates (monosodium glutamate) and caffeine
- Food containing excess histamine such as spoilt fish, leading to scombroid food poisoning
- Sucrose and starch (in the case of sucrase-isomaltase deficiency)
- Fatty foods and spicy foods.
Symptoms of food sensitivity (food intolerance) include:
- Nausea
- Stomach pain
- Gas, cramps or bloating
- Vomiting
- Heartburn
- Diarrhea
- Headaches
- Irritability or nervousness
Food sensitivity is often tricky to diagnose because you may be able to eat small amounts of a problem food without having any reaction. Instead, symptoms may only appear after you eat a large portion of the food, or eat it frequently. Some substances within foods, and the quantity (dose) of foods eaten, can increase the frequency and severity of your symptoms. The best way to identify problem foods is with a food diary. Write down what you eat for every meal, including individual foods and portions. Then list any symptoms that occur afterwards and rate their level of intensity on a scale of one to 10, with one being no reaction to 10 being the most severe. Maintain your diary for two weeks to a month, and then review. Once you’ve pinpointed one, or several, potential problem foods, eliminate them from your diet. After a few days, add only one food back into your diet and monitor your reaction. If your symptoms return, you’ve found the offending food. However, if the problem food is a source of vital nutrients, make sure you find an adequate replacement. For example, cutting out gluten foods like wheat can rob your diet of fiber and B vitamins. Switch to gluten-free bread, or increase your intake of gluten-free grains like quinoa, sorghum, teff, millet, and buckwheat. For lactose intolerance, drink lactose free milk or there are supplements containing enzymes produced by lactose-digesting bacteria (Lactaid, Lactrase, others) that can be taken as tablets or added to foods. Some milk products (Lactaid) to which lactase has been added may contain little or no lactose, and they may taste sweeter than untreated products, because the milk sugar has already been broken down.
An allergist or immunologist is a doctor specially trained to diagnose and treat people with food sensitivities and food allergies. They can help you figure out your triggers, discuss treatment options and help you avoid allergens.
Food sensitivity test or food intolerance test is only done after a person has had symptoms of an adverse food reaction. In this way, food sensitivity testing is a tool for diagnosis, helping to identify foods that provoke an abnormal reaction. It is uncommon to do broad screening for food sensitivities, especially if you haven’t already had signs or symptoms of a food reaction.
It is generally recommended to only test for food sensitivity or food intolerance after you have experienced symptoms. If you haven’t had symptoms, food sensitivity testing is likely to have more downsides than benefits. No test exists that can accurately detect all food sensitivities. Testing for a wide range of possible reactions can return a false positive, which means the test shows an intolerance or sensitivity for a food that doesn’t actually cause you problems. False positives can cause unnecessary changes to your diet that may affect your nutrition.
Many tests have been promoted for detecting food sensitivities and food intolerances without any credible evidence and have not been proven to be accurate or effective and experts recommend against using them 7, 8. Examples of unvalidated tests include 9:
- Immunoglobulin-G (IgG) and IgG subclass 4 (IgG4) antibody tests
- Cytotoxic food testing
- Gastric juice analysis
- Alcat testing
- Hair analysis
- Basophil histamine release/activation
- Lymphocyte stimulation
- Blood cell analysis, including flow cytometry and mediator release tests
- Provocation or neutralization testing
- Rinkel’s intradermal skin testing
- Electrodermal testing (Vega testing)
- Facial thermography
- Muscle reaction or strength tests
- Endoscopic allergen provocation
- Applied kinesiology
- Mediator release assay (LEAP diet)
Not only do these tests lack any scientific rationale, but have been shown to be inaccurate and unreliable in published studies. Treatment based on inaccurate results is not only misleading, but can result in ineffective and sometimes harmful treatments, and delay the proper management of food allergies and intolerances.
If you’ve had signs of a food reaction, see your doctor to determine whether you have a food intolerance or a food allergy. By reviewing your experience and symptoms, your doctor can describe the pros and cons of testing for specific allergens, intolerances, and/or sensitivities. Food sensitivity testing is normally conducted in a doctor’s office, clinic, or medical laboratory. The procedure depends on the specific test being used.
However, most food intolerances are found through trial and error to determine which food or foods cause symptoms. You may be asked to keep a food diary to record what you eat and when you get symptoms, and then look for common factors. For example, after charting what he eats every day for a month, a man finds that he had symptoms only on the days he ate cheese. This points the finger at cheese as a possible cause of his discomfort.
Another way to identify problem foods is an elimination diet. You begin by completely eliminating any suspect foods from your diet until you are symptom-free. You then begin to reintroduce the foods, one at a time. This can help you pinpoint which foods cause symptoms. Seek the advice of your doctor or a registered dietitian before beginning an elimination diet to be sure your diet provides adequate nutrition.
Food Sensitivity Versus Food Allergy
Food sensitivity is NOT a food allergy. A food allergy always involves an immune system reaction to a certain food, while a food sensitivity does not have an immune component. Food sensitivity typically produces gastrointestinal disturbance marked by bloating, nausea and indigestion, some of which can also occur with certain food allergies. A true allergy, on the other hand, causes an immune reaction, involving the production of antibodies toward the allergenic food, with symptoms like hives, itching of the mouth and throat, swelling of the face, lips, tongue and throat and difficulty breathing.
Food sensitivity also known as food intolerance is a broad term that is used to describe a wide range of unwanted reactions (usually digestive system reactions) to certain foods, that cause symptoms after eating some foods 10. Food intolerance or food sensitivity occurs when something in food irritates a person’s digestive system or when a person is unable to properly digest, or break down, the food. One of the tricky aspects of diagnosing food intolerance is that some people are sensitive not to the food itself but to a substance or ingredient used in the preparation of the food. The types of foods that trigger food sensitivity or food intolerance vary from individual to individual. Common foods that may cause food sensitivity include dairy products (e.g., cheddar cheese, cottage cheese, cow’s milk, mozzarella cheese, yogurt); egg white and egg yolk; grains (e.g., barley, bran, brown rice, gluten); fruits (e.g., apple, avocado, banana); meat (e.g., beef, chicken, lamb); and more. Consuming certain foods can cause various symptoms including stomach pain, cramps, nausea, diarrhea, bloating, gas/flatulence, diarrhea, vomiting, irritable bowel syndrome (IBS), rashes, hives (urticaria), recurrent mouth ulcers, heartburn, headaches and irritability or nervousness. Depending on the type of food intolerance you have, you may be able to eat small amounts of problem foods without a reaction. By contrast, if you have a true food allergy, even a tiny amount of the food may trigger an allergic reaction. Intolerance to lactose, which is found in milk and other dairy products, is the most common food sensitivity or food intolerance affecting about 10 percent of Americans. If food intolerances (food sensitivity) are not properly managed, these symptoms can adversely affect general health and wellbeing. Unfortunately, tests cannot easily identify most food sensitivities. While there are tests are available that look for dozens of types of antibodies called immunoglobulin-G (IgG) in the blood. Experts advise against this type of screening because it has not been shown to be accurate in identifying true food intolerance and sensitivities.
Food allergy is an immune system reaction (antibody mediated food allergy) and can be immunoglobulin E (IgE)-mediated or non-IgE-mediated 11, 12, 13, 3, 14, 15. A food allergy is caused by an overreaction of the immune system due to your body mistaking an ingredient in food — usually a protein (the allergen) — as harmful and creates a defense system (antibodies) to attack the allergen 16. An allergic reaction occurs when the antibodies are battling an “invading” food protein. Any food can cause allergy but overall only a few foods account for the vast majority of food allergies 17. The most common food allergies that trigger 90% of food allergic reactions are shellfish, peanuts, tree nuts, fish, eggs, wheat, soy, and milk 3. It should be noted that reactions that do not involve the immune system are not food allergies (e.g., milk intolerance). About 6% of children experience food allergic reactions in the first three years of life, including approximately 2.5% with cow’s milk allergy, 1.5% with egg allergy, and 1% with peanut allergy 11. Anaphylaxis is a very serious and potentially life-threatening allergic reaction that involves a sudden drop in blood pressure, swelling of the airways to the lungs, wheezing, shortness of breath, loss of consciousness and body system failure. If you’ve had allergic reactions to food or insect bites, your doctor will prescribe an epinephrine (adrenaline) injection (Adrenaclick, Auvi-Q, EpiPen) for emergency self-treatment.
Being allergic to a food may also result in being allergic to a similar protein found in something else. For example, if you are allergic to ragweed, you may also develop reactions to bananas or melons. This is known as cross-reactivity. Cross-reactivity happens when the immune system thinks one protein is closely related to another. When foods are involved it is called oral allergy syndrome (OAS). Symptoms are typically triggered by eating these foods when they’re fresh and uncooked. However, when these foods are cooked, symptoms may be less severe.
Different foods can cause different kinds of food allergy symptoms. For example, fruits and vegetables tend to cause milder symptoms such as rashes, whereas nuts and shellfish often trigger severe allergic reactions. In food allergies, even small amounts of the food can be enough to trigger an allergic reaction. The symptoms can vary greatly and affect a number of different organs:
- Reactions in the mouth and throat and on the skin: These are the most common symptoms. They involve swelling and itching of lips and mouth, itching and swelling or rashes with reddened skin and hives (urticaria), eczema (atopic dermatitis) and scaly itchy dry patches of skin.
- Gastrointestinal (stomach and bowel) problems: The typical symptoms are abdominal pain, nausea, vomiting and diarrhea. They usually appear within half an hour of eating the food, or a few hours afterwards at the latest.
- Breathing problems: Signs include coughing, a hoarse voice, difficulty breathing or wheezing.
The symptoms of a food allergy may look like other health conditions or problems. Always talk with your doctor for a diagnosis.
Foods can also trigger more severe life-threatening allergic reaction known as anaphylaxis, which is always a medical emergency. Anaphylaxis is a very serious and potentially life-threatening allergic reaction that involves a sudden drop in blood pressure, swelling of the airways to the lungs, wheezing, shortness of breath, loss of consciousness and body system failure.
The symptoms of anaphylaxis are:
- Trouble breathing or wheezing
- Confusion
- Rapid heart beat (fast pulse)
- Low blood pressure
- Swelling of the lips, tongue and throat
- Wheezing
- Confusion
- Bluish skin (cyanosis)
- Light-headedness, dizziness or feeling faint
- Loss of consciousness
- Hives and generalized itching
- Anxiety
- Heart palpitations
- Nausea and vomiting
- Diarrhea
- Abdominal pain or cramping
- Cough
Peanut allergy, the most common food allergy, is the leading cause of life-threatening anaphylaxis. If you’ve had allergic reactions to food or insect bites, your doctor will prescribe an epinephrine (adrenaline) injection (Adrenaclick, Auvi-Q, EpiPen) for emergency self-treatment.
Food Protein-Induced Enterocolitis Syndrome (FPIES), sometimes referred to as a delayed food allergy, is a severe condition causing vomiting and diarrhea. In some cases, symptoms can progress to dehydration and shock brought on by low blood pressure and poor blood circulation. Food Protein-Induced Enterocolitis Syndrome (FPIES) allergic reactions are triggered by ingesting a food allergen. Although any food can be a trigger, the most common culprits include milk, soy and grains. Food Protein-Induced Enterocolitis Syndrome (FPIES) often develops in infancy, usually when a baby is introduced to solid food or formula.
Most children tend to outgrow milk and egg allergies by school-age. In contrast, children with peanut, nut, or seafood allergy retain their allergy for life 18, 19. Children with asthma, allergic rhinitis, atopic dermatitis, or an allergy to insect venom, medications, or latex are at an increased risk of developing food allergies 12.
Diagnosis of food allergy starts with a detailed, allergy-focused history addressing specific risk factors such as atopic dermatitis and a family history of atopic disease 20. Tests for food allergies include avoidance of the food, allergy skin prick testing, serum immunoglobulin E (IgE) testing, and an oral food challenge. In patients with suspected food allergy, the first step should be elimination of the suspected food to see if symptoms resolve. Immunoglobulin E (IgE) specific antibody and skin testing are helpful to confirm or exclude allergens. In patients with a history suggestive of anaphylaxis to a particular food, the response to specific IgE antibody levels and a skin test can confirm and predict the results of an oral food challenge 21, 22. An oral food challenge is used to confirm a negative or questionable test result. The only definitive diagnostic method for food allergy is the oral food challenge, in which increasing doses of a potential food allergen are ingested over fixed time intervals, until either an allergic reaction is observed or a maximum dose is reached 23. Oral food challenges are typically performed in an allergist’s office where the proper equipment and expertise are available in the event of severe anaphylactic reaction. To avoid this possibility, the oral food challenges test is reserved for patients with a low risk of severe reaction, and the tested food is administered using progressive dosing until a customary meal dose is met. A negative food allergy test results together with negative oral food challenge can help reassure the patient and family that no allergy is present and no further testing is necessary 22.
The best way to prevent an allergic reaction is to avoid food(s) and eliminate the offending food(s) that have caused reactions in the past from your diet. People who have had severe reactions in the past, should carry an EpiPen® (injectable epinephrine) for treatment of anaphylaxis. An identification bracelets/necklace stating the allergy should also be worn. There is no medicine to prevent food allergies, although research is ongoing.
Figure 1. Food allergy diagnostic algorithm
Footnotes: The only definitive diagnostic method for food allergy is the oral food challenge, in which increasing doses of a potential food allergen are ingested over fixed time intervals, until either an allergic reaction is observed or a maximum dose is reached 23. However, the oral food challenge method is infrequently used outside properly equipped and staffed specialist centers because it is resource-intensive and carries the risk of inducing a severe anaphylactic reaction.
[Source 24 ]What causes food sensitivity or food intolerance?
Natural substances in foods can cause food intolerances or food sensitivities. Foods are composed of proteins, carbohydrates, fats, various nutrients and several natural chemicals. These following naturally occurring compounds often add flavor and smell to food, but they can trigger symptoms in some people.
- Lactose intolerance is an example of an enzyme deficiency, which occurs when people are born with, or develop, insufficient lactase enzymes to digest lactose in cow’s milk and other dairy products. This can result in bloating, gas/flatulence, stomach upset and diarrhea after having dairy products. Lactose intolerance is uncomfortable but not dangerous and does not cause rashes or anaphylaxis. Lactose intolerance diagnosis is by temporary elimination of lactose and reintroduction.
- Monosodium glutamate (MSG, additive numbers 621 and 625) was originally isolated from seaweed in 1908 by a Japanese chemist. Glutamates also occur naturally in such foods as camembert cheese, Parmesan cheese, tomatoes, soy sauce and mushrooms. MSG (monosodium glutamate) stimulates nerve endings, which may be why it is used as a flavor enhancer when it is added to food.
- Vasoactive amines such as tyramine, serotonin and histamine are well known triggers of migraines in some people. They are present naturally in pineapples, bananas, baked meat, vegetables, red wine, wood-matured white wine, avocados, chocolate, citrus fruits and mature cheese. Amines can act directly on small blood vessels to expand their capacity. This may be why they can trigger flushing, migraines and nasal congestion in some people.
- Sulfites may occur naturally — as in red wines — or may be added to prevent the growth of mold, also are a source of intolerance for some people. The Food and Drug Administration (FDA) has banned the use of spray-on sulfates to preserve fruits and vegetables, but sulfates are still found naturally in some foods.
- Salicylates are natural aspirin like compounds that are present in a wide variety of herbs, spices as well as fruit and vegetables. Reactions to salicylates may be even more common than reactions to artificial colors and preservatives. Aspirin can trigger hives by acting directly on skin mast cells, and therefore salicylates can also worsen hives in some people.
- Toxins can cause severe symptoms. Contamination of food with micro-organisms (such as bacteria) or their products (due to spoilage) can cause food poisoning due to toxins. For example, if some types of fish are stored poorly, their gut bacteria can convert histidine to histamine, resulting in allergy like symptoms.
- Histamine toxicity. Certain fish, such as tuna or mackerel, that are not refrigerated properly and that contain high amounts of bacteria may also contain high levels of histamine that trigger symptoms similar to those of food allergy. Rather than an allergic reaction, this is known as histamine toxicity or scombroid poisoning.
- Irritants. Caffeine, capsaicin (an active component of chili peppers) and curry are gut irritants that can trigger indigestion in some people. It is important to realize that reactions to these substances are not due to allergy.
- Celiac disease. While celiac disease is sometimes referred to as a gluten allergy, it does not result in anaphylaxis. Like a food allergy, celiac disease does involve an immune system response, but it’s a unique reaction that’s more complex than a simple food allergy. When people with celiac disease eat a gluten product, their body usually produces certain autoantibodies. Examples of these autoantibodies that may be detected in at-home testing include:
- Anti-tissue transglutaminase antibodies immunoglobulin A (tTG-IgA)
- Anti-tissue transglutaminase antibodies immunoglobulin G (tTG-IgG)
- Anti-endomysial antibody (EMA-IgA)
- Tests can also look for antibodies that target a part of the gluten protein called gliadin. Examples of these antibodies include:
- Anti-deamidated gliadin peptide antibodies immunoglobulin A (DGP-IgA)
- Anti-deamidated gliadin peptide antibodies immunoglobulin G (DGP-IgG)
- In general, testing for anti-tissue transglutaminase antibodies immunoglobulin A (tTG-IgA) is the preferred blood test for detecting celiac disease. The anti-endomysial antibody (EMA-IgA) antibody test is also considered to be a dependable way to check for celiac disease in most people. Tests for anti-tissue transglutaminase antibodies immunoglobulin G (tTG-IgG) and the anti-deamidated gliadin peptide (DGP) antibodies are not considered as reliable and are generally used in certain circumstances.
- Recurring stress or psychological factors. Sometimes the mere thought of a food may make you sick. The reason is not fully understood.
How can you tell the difference between food allergy and food intolerance?
Food allergies are the result of a reaction that starts in the immune system. For instance, if you have an allergy to eggs, your immune system identifies a protein found in eggs as an allergen. Your immune system reacts by producing antibodies called immunoglobulin E (IgE) to neutralize the allergy-causing food or food substance (the allergen). These antibodies attach to cells in your skin, lungs and gastrointestinal tract. If you come in contact with the allergen again, the cells release chemicals including histamine into your bloodstream, which cause food allergy symptoms such as itching, hives, swelling, diarrhea, wheezing and a potentially life-threatening reaction called anaphylaxis. Symptoms of anaphylaxis may include difficulty breathing, dizziness or loss of consciousness. Without immediate treatment—an injection of epinephrine and expert care in a hospital—anaphylaxis can be fatal.
Food allergies can be triggered by even a microscopic amount of the food (includes touching or inhaling the food) and occur every time the food is consumed. People with food allergies are generally advised to avoid the offending foods completely. Symptoms of allergic reactions to foods are generally seen on the skin (hives, itchiness, swelling of the skin). Gastrointestinal symptoms may include vomiting and diarrhea. Respiratory symptoms may accompany skin and gastrointestinal symptoms, but don’t usually occur alone.
Food allergy can strike children and adults alike. Many food allergies are first diagnosed in young children, though they may also appear in older children and adults. While many children outgrow a food allergy, it is also possible for adults to develop allergies to particular foods. Eight foods are responsible for the majority of allergic reactions:
- Cow’s milk
- Chicken eggs
- Fish
- Peanuts
- Shellfish such as shrimp, lobster and crab
- Soy
- Tree nuts such as walnuts and pecans
- Wheat
Being allergic to a food may also result in being allergic to a similar protein found in something else. For example, if you are allergic to ragweed, you may also develop reactions to bananas or melons. This is known as cross-reactivity. Cross-reactivity happens when the immune system thinks one protein is closely related to another. When foods are involved it is called oral allergy syndrome (OAS). In oral allergy syndrome (OAS), certain fresh fruits and vegetables or nuts and spices can trigger an allergic reaction that causes the mouth to tingle or itch. In serious cases, the reaction results in swelling of the throat or even anaphylaxis. Proteins in certain fruits, vegetables, nuts and spices cause the reaction because they’re similar to allergy-causing proteins found in certain pollens. This is an example of pollen-food allergy syndrome. Symptoms are typically triggered by eating these foods when they’re fresh and uncooked. However, when these foods are cooked, symptoms may be less severe. The following table shows the specific fruits, vegetables, nuts and spices that can cause oral allergy syndrome (OAS) or pollen-food allergy syndrome in people who are allergic to different pollens.
Table 1. Oral allergy syndrome (OAS) or pollen-food allergy syndrome
| If you are allergic to >> | Birch pollen | Ragweed pollen | Grasses | Mugwort pollen |
|---|---|---|---|---|
| You may also have a reaction to >> | Almond Apple Apricot Carrot Celery Cherry Hazelnut Peach Peanut Pear Plum Raw potatoes Soybean Some herbs and spices (anise, caraway seed, coriander, fennel, parsley) | Bananas Cucumber Melons (cantaloupe, honeydew and watermelon) Zucchini | Kiwi Melons (cantaloupe, honeydew and watermelon) Orange Peanut Tomatoes White potato Zucchini | Apples Bell pepper Broccoli Cabbage Carrots Cauliflower Celery Garlic Onion Peach Some herbs and spices (anise, black pepper, caraway seed, coriander, fennel, mustard, parsley) |
Exercise-induced food allergy also known as Food Dependent Exercise Induced Anaphylaxis (FDEIAn): Exercise-induced food allergy is a disorder in which allergic symptoms (feeling itchy and lightheaded) occur if exercise takes place within several hours after consumption of the causative food allergen, as identified by clinical history and allergy testing 25. Serious cases may even involve hives or anaphylaxis. Omega-5 gliadin, a protein component of gluten, is a major protein involved in wheat allergy causing exercise-induced food allergy, although other foods have also been implicated, including egg, nuts, crustaceans, meats, fruits, and vegetables 26. The diagnosis of exercise-induced food allergy can be made when a patient has signs and symptoms consistent with recurrent allergic symptoms upon or soon after physical exertion, and if the food allergen was consumed within two to four hours prior to the allergic event. There should also be an absence of symptoms during vigorous physical activities or food allergen ingestion alone 27. Not eating for a couple of hours before exercising and avoiding certain foods may help prevent this problem.
Food Protein-Induced Enterocolitis Syndrome (FPIES), sometimes referred to as a delayed food allergy, is a severe condition causing vomiting and diarrhea. In some cases, symptoms can progress to dehydration and shock brought on by low blood pressure and poor blood circulation. Much like other food allergies, food protein-induced enterocolitis Syndrome (FPIES) allergic reactions are triggered by ingesting a food allergen. Although any food can be a trigger, the most common culprits include milk, soy and grains. Food Protein-Induced Enterocolitis Syndrome (FPIES) often develops in infancy, usually when a baby is introduced to solid food or formula.
Food Protein-Induced Allergic Proctitis (FPIAP). Food protein-induced allergic proctitis (FPIAP) is the least severe, non-IgE-mediated disease and is a common cause of isolated rectal bleeding in otherwise healthy infants 28. Pathogenic inflammation is primarily limited to the rectum, but rarely, it can extend further up the sigmoid colon 29. Although food protein-induced allergic proctitis (FPIAP) has been rarely described in older children, it is more commonly found in breastfed infants and typically starts within the first few months of life 30. Infants classically present with a history of stools streaked with bright red blood and mucous. Although stools may be more frequent, frank diarrhea is uncommon, and infants otherwise appear healthy. The diagnosis of food protein-induced allergic proctitis (FPIAP) is made based on clinical history and resolution of symptoms following food elimination; skin testing and other in vitro tests assessing for food-specific IgE are not recommended 31. The most common causes in breastfeeding infants are milk, soy, and egg from the maternal diet, and most patients will have symptom resolution within 72 hours of strict food elimination 30. Typically, cow’s milk should be strictly eliminated first, followed by soy and then egg if symptoms do not completely resolve within two weeks 32. Formula-fed infants and breastfed infants that do not respond to elimination diets should be placed on an extensively hydrolyzed or amino acid-based formula due to a high rate of sensitization to both cow’s milk and soy proteins 33. It may be necessary to perform a more extensive evaluation in children who continue to have symptoms despite food elimination. Colonoscopy in food protein-induced allergic proctitis (FPIAP) generally demonstrates features of mild colitis, patchy erythema, and a loss of vascularity, and biopsies are notable for high numbers of eosinophilia in the lamina propria and muscularis mucosa 34. After symptom resolution, home diet reintroduction is generally recommended after six to nine months of age since most children have been shown to tolerate the implicated food after this time. Some studies have even demonstrated that up to 20% of breastfed infants had spontaneous resolution of symptoms without changes in the maternal diet 35.
Food protein-induced enteropathy (FPE). In contrast to food protein-induced allergic proctitis (FPIAP), food protein-induced enteropathy (FPE) involves the small bowel and typically presents in the first nine months of life with protracted diarrhea that can lead to failure to thrive in over 50% of infants 36. In many infants, symptoms usually have a gradual onset within a few weeks of introduction of the implicated food. Although the most common causal food of food protein-induced enteropathy (FPE) is cow’s milk, other foods such as soy, egg, rice, poultry, fish, and shellfish have been described 37. Food protein-induced enteropathy (FPE) can also occur after acute episodes of infectious gastroenteritis 38. The diagnosis of food protein-induced enteropathy (FPE) is made upon the presence of clinical symptoms often with confirmation by endoscopy and biopsies. Histological findings include mucosal changes in the proximal and distal small bowel with villous atrophy and cellular infiltration 36. As in other non-IgE-mediated diseases, skin testing and in vitro assessments for food-specific IgE are not recommended. Once a diagnosis is established, elimination of the implicated food generally leads to resolution of symptoms within one to three weeks, with severe cases sometimes requiring partial parenteral nutrition during the initial recovery period 39. After one to two years, most children with food protein-induced enteropathy (FPE) have been shown to tolerate reintroduction of the eliminated food without any clinical symptoms or long-term complications.
Eosinophilic Esophagitis (EoE) is a chronic, rare, and food antigen-driven immune-mediated inflammatory condition of the esophagus that is estimated to affect 1 in every 2000 people 40. There is a large body of evidence that eosinophilic esophagitis (EoE) subjects have aeroallergen sensitization and concurrent allergic disorders, including asthma, allergic rhinitis, eczema and food allergy 41. The esophagus is the tube that sends food from the throat to the stomach. Most research suggests that the leading cause of eosinophilic esophagitis (EoE) is an allergy or a sensitivity to particular proteins found in foods. The most common management approaches for eosinophilic esophagitis (EoE) are topical glucocorticosteroids, dietary elimination, and esophageal dilation 41.
Many people who think they are allergic to a food may actually be intolerant to it. Some of the symptoms of food intolerance and food allergy are similar, but the differences between the two are very important.
Food intolerance (food sensitivity) typically involves the gastrointestinal tract, causing uncomfortable symptoms like abdominal pain, nausea, vomiting and diarrhea, but there is no risk of anaphylaxis. Furthermore, food intolerances (food sensitivities) often are dose related; people with food intolerance (food sensitivity) may not have symptoms unless they eat a large portion of the food or eat the food frequently. For example, a person with lactose intolerance may be able to drink milk in coffee or a single glass of milk, but becomes sick if he or she drinks several glasses of milk.
Food allergies and food intolerances also are different from food poisoning, which generally results from spoiled or tainted food and affects more than one person eating the food. Your doctor can help determine if you have food allergy or food intolerance, and establish a plan to help control your symptoms.
Food sensitivity prevention
Taking a few simple steps can help you prevent the symptoms associated with a food sensitivity.
- Learn which foods in which amounts cause you to have symptoms, and limit your intake to amounts you can handle.
- When you dine out, ask your server about how your meal will be prepared. Some meals may contain foods you cannot tolerate, and that may not be evident from the description on the menu.
- Learn to read food labels and check the ingredients for problem foods. Don’t forget to check condiments and seasonings. They may contain MSG or another additive that can lead to symptoms.
- Early exposure. Early introduction of peanut products has been associated with a lower risk of peanut allergy. In a recent study, high-risk infants — such as those with atopic dermatitis or egg allergy or both — were selected to either ingest or avoid peanut products from 4 to 6 months of age until 5 years of age. Researchers found that high-risk children who regularly consumed peanut protein, such as peanut butter or peanut-flavored snacks, were around 80% less likely to develop a peanut allergy. Before introducing allergenic foods, talk with your child’s doctor about the best time to offer them.
Food sensitivity signs and symptoms
Symptoms of food sensitivity include:
- Nausea
- Stomach pain
- Gas, cramps or bloating
- Vomiting
- Heartburn
- Diarrhea
- Headaches
- Irritability or nervousness
There are many other adverse reactions to foods, including:
- Feeling unwell after eating from other causes such as heartburn after a fatty or spicy meal or a hangover after too much red wine.
- Celiac disease is not an allergy, but does involve an immune system response to foods containing gluten. When gluten-containing cereals (like wheat) are eaten, inflammation of the gut occurs, resulting in poor absorption of nutrients. Major symptoms are gut upset, fatigue, anemia or weight loss.
- Non-celiac gluten intolerance is a recently recognized condition which can cause symptoms such as abdominal disturbance (usually bloating but sometimes other symptoms as well) and occasionally malaise and tiredness. It appears to be genuine as proven by blinded challenge studies but the mechanism is not known.
- Food aversion is a condition where a person not only dislikes a food, but also experiences unpleasant physical symptoms when they see or smell the food. Symptoms are triggered by emotions associated with food rather than the food itself. This does not usually occur if the food is disguised.
- Underlying anxiety can result in unconscious over-breathing or hyperventilation. The symptoms that result (dizziness, tight chest, blurred vision or numbness) can be very distressing, and can sometimes resemble food allergy.
Food sensitivity test
It is generally recommended to only test for food sensitivities or intolerances after you have experienced symptoms of a potential problem. If you haven’t had symptoms, food sensitivity testing is likely to have more downsides than benefits. Food sensitivity can often be difficult to diagnose, with the exception of tests for lactose and sucrose intolerance. The best approach is to first see your doctor to make a diagnosis and check for other conditions that may be causing symptoms. Diagnosis of unwanted reactions to foods should be based on your clinical history, your response to treatment and testing. There is no single comprehensive test available to check for all or even most types of food sensitivities. As a result, tests are typically tailored to match your symptoms and health history. Because there can be symptom overlap between food sensitivity and food allergies, your doctor may recommend a skin prick test or blood allergy test to be sure that you don’t have a food allergy. If you are concerned about a possible food intolerance, it’s important to discuss your symptoms with your doctor to determine the most appropriate tests in your case.
At-home testing is available for certain types of food sensitivities or specific intolerances. Many tests that are marketed for detecting food sensitivities and intolerances have not been proven to be accurate or effective, and experts recommend against using them. Examples of Unvalidated and Unreliable food sensitivity tests include:
- Immunoglobulin-G (IgG and IgG4) antibody tests. Experts advise against this type of screening because it has not been shown to be accurate in identifying true food intolerance and sensitivities.
- Hair tests. Hair analysis either measures the “electromagnetic energy” of the hair sample when it’s in contact with the suspected allergen, or measures mineral content of the hair sample.
- Blood cell analysis, including flow cytometry and mediator release tests
- Bicom (bioresonance) testing. Bicom (bioresonance) test claims to detect abnormalities in electromagnetic emissions by body tissues using electrodes.
- Provocation or neutralization testing
- Electrodermal testing or Vega testing. Electrodermal (Vega testing) technique detects allergies by measuring changes in electrical currents within the body using a “vega machine”. The patient holds a negative electrode in one hand, while the positive electrode is applied to acupuncture points on fingers or toes. The allergen is introduced to the electrical circuit, and if an alteration in the current is detected, this indicates sensitivity.
- Muscle reaction or strength tests
- Cytotoxic food testing or Alcat testing. In cytotoxicity testing or Alcat tests white blood cells are collected from a sample of blood. These cells are mixed with the suspected food allergen and viewed under a microscope. Changes in the appearance of cells indicate an allergy.
- Kinesiology. Muscle strength is measured after exposure to a suspected allergen, with a reduction in muscle strength indicating exposure to an allergen or “toxic” substance.
- Allergy elimination techniques
- Iridology
- Pulse testing. Pulse testing measures the pulse after a suspected allergen is consumed. A sensitivity is diagnosed if the pulse increases after consumption.
- Rinkel’s intradermal skin testing
- Reflexology
- VoiceBio. This technique analyses the person’s voice, and draws conclusions regarding soundwave frequencies, organ dysfunction, and the presence of food allergies/intolerances.
These tests are characterized by a lack of supportive scientific evidence, poor correlation with evidence-based tests, and inconsistent findings when repeated in the same person.
Some tests for lactose intolerance and celiac disease can be done with at-home kits to obtain a blood sample that is then sent by mail to a laboratory. A positive result on at-home testing usually requires follow-up tests prescribed by a doctor.
- Lactose intolerance, which is the inability to properly digest a type of sugar found in milk products, can be detected with lactose tolerance tests. These include blood or breath tests that demonstrate disrupted lactose digestion.
- Celiac disease is a disorder in which a person’s immune system attacks their intestinal lining when they consume gluten, a protein found in wheat and other grains. Blood tests can help diagnose celiac disease by analyzing levels of specific antibodies, which are proteins produced by the immune system.
Some people are intolerant of gluten without having celiac disease, and this is often referred to as non-celiac gluten sensitivity (NCGS). There is no test that has been validated to accurately detect non-celiac gluten sensitivity (NCGS).
If you are concerned about a possible food sensitivity, it’s important to discuss your symptoms with your doctor to determine the most appropriate tests in your case.
For most other food intolerances and sensitivities, there is no reliable test to detect them. As a result, a doctor may suggest other types of tests:
- Oral food challenge: This involves eating increasing quantities of a food over a period of hours while being closely monitored for adverse reactions. Oral food challenges follow a specific protocol and should only be done in a controlled medical setting.
- Food elimination diet: This requires following a strict diet that excludes specific foods or additives for a period of weeks. Over time, the dietary restrictions may be modified to try to identify specific intolerances or sensitivities.
People with symptoms of food reactions may have testing for other conditions such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS) or malabsorption of nutrients. Examples of tests related to these conditions are listed in the table below.
| Test name | Test sample | What it measures |
|---|---|---|
| Xylose Absorption | Blood and urine | How well the body absorbs a simple sugar |
| Fecal fat | Stool | Amount of fat in a stool sample |
| Erythrocyte Sedimentation Rate (ESR) | Blood | Rate at which certain red blood cells fall when blood is placed in a test tube |
At home food sensitivity test
No test exists that can accurately detect all food sensitivities. Testing for a wide range of possible reactions can return a false positive, which means the test shows an intolerance or sensitivity for a food that doesn’t actually cause you problems. False positives can cause unnecessary changes to your diet that may affect your nutrition. If you’ve had signs of a food reaction, talk with your doctor. By reviewing your history and symptoms, your doctor can describe the pros and cons of testing for specific allergens, intolerances, and/or sensitivities.
At-home testing is available for certain types of food sensitivity. Some tests for lactose intolerance and celiac disease can be done with at-home kits to obtain a blood sample that is then sent by mail to a laboratory. A positive result on at-home testing usually requires follow-up tests prescribed by a doctor.
Some tests are available that look for dozens of types of antibodies called immunoglobulin-G (IgG) in the blood. However, experts advise against this type of screening because it has not been shown to be accurate in identifying true food intolerance and sensitivities.
If you are concerned about a possible food intolerance, it’s important to discuss your symptoms with your doctor to determine the most appropriate tests in your case.
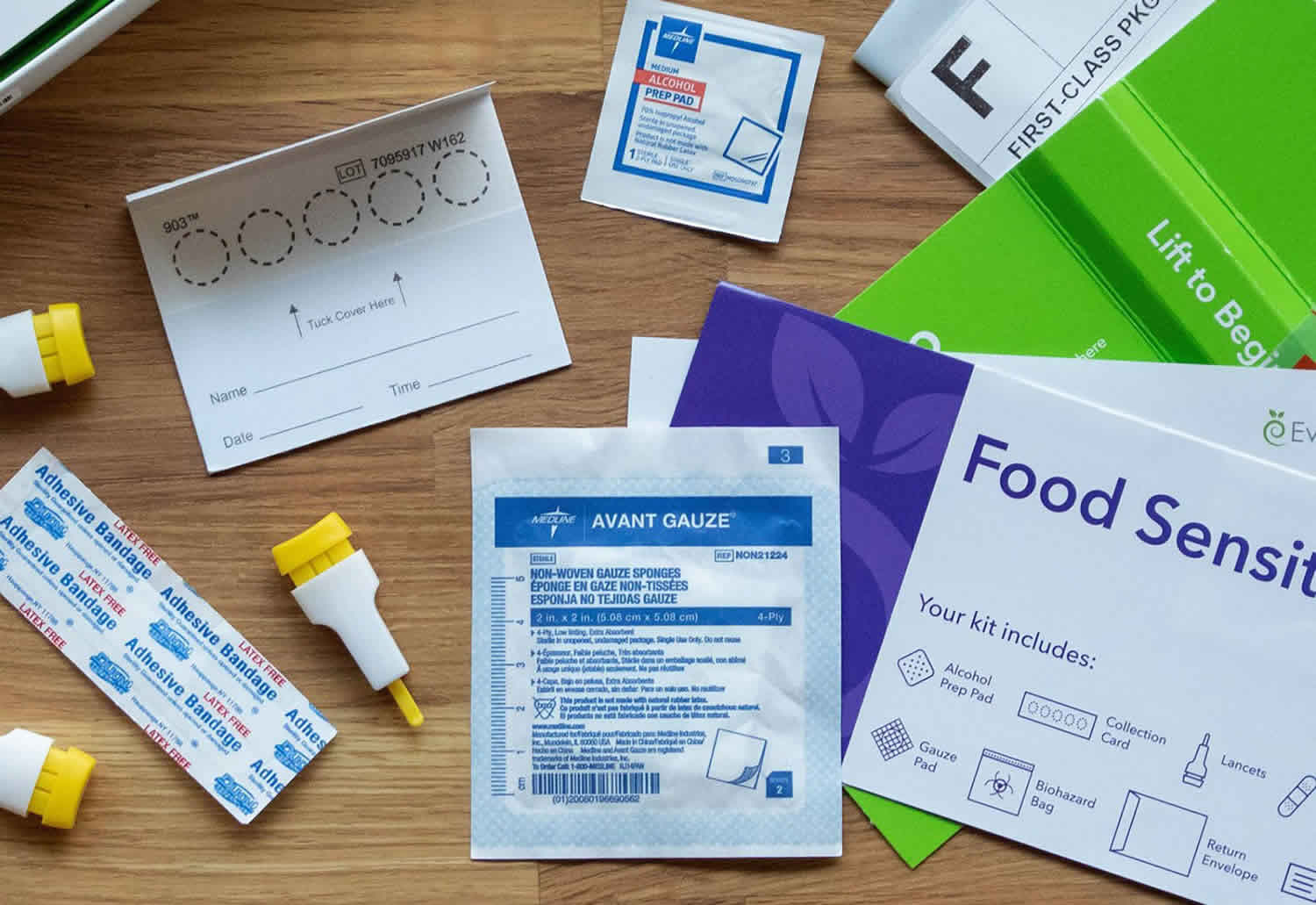
Everlywell Food Sensitivity Comprehensive Test
- Price: $299
- Type: Self-collection
- Sample: Blood
- Tests for: 204 foods
- Results timeline: 2-3 weeks
The Everlywell Food Sensitivity Comprehensive Test is an at-home test that helps diagnose food sensitivities by measuring IgG antibody response to 204 foods, including a wide range of dairy products, fruits, seafood, and vegetables. Each food is rated on a scale of 0 to 3, with 0 being normal and 3 showing high reactivity. Everlywell recommends using the results in conjunction with an elimination diet to help determine if you are sensitive to certain foods. Common symptoms of food sensitivity are indigestion, abdominal pain, and bloating.
You can administer the test at home with a user-friendly skin prick kit. Using a prepaid label, ship the sample to Everywell for analysis at a CLIA-certified lab.
Don’t allergists use a blood test to investigate food allergy?
Yes, but a different test is ordered: food-specific immunoglobulin E (IgE) levels, not immunoglobulin-G (IgG) or IgG subclass 4 (IgG4). Even with food-specific immunoglobulin E (IgE) measurements, large “screening” panels are not recommended. Making the diagnosis of a specific food allergy may include the following: a full medical history, physical examination, skin prick testing, carefully selected food-specific immunoglobulin E (IgE) levels and oral food challenges to suspected food allergens in some instances 42.
Is there a relation between food-specific IgG levels and food allergy?
Research from the early 1980s reported a potential mechanism for immunoglobulin-G subclass 4 (IgG4) to trigger basophil histamine release, suggesting a role in the allergic response 43. Subsequent research clarified that this relation was not limited to IgG4 and in fact involved immunoglobulin E (IgE)-receptor cross-linking through a receptor complex found on the basophil membrane 44. This supports clinical observations that neither total immunoglobulin-G (IgG) nor IgG4 levels correlate with food allergy as shown on double-blind placebo-controlled food challenges 44.
Are food-specific IgG levels a marker of disease?
The detection of food-specific immunoglobulin-G (IgG) shows a physiologic response of the immune system to exposure to food. For immunoglobulin-G subclass 4 (IgG4) in particular, this may be the normal human response 5. Immunoglobulin G (IgG) antibodies directed at specific foods can be found in healthy children as well as adults 45. Higher levels of IgG4 to foods in infancy may be associated with tolerance to those foods later in childhood 46.
The relation between IgG4 and food has been further explored through the recent developments in oral immunotherapy to foods. Efforts to induce permanent tolerance to allergens such as milk or peanuts have been accompanied by increases in patients’ IgG4 levels to those foods 47. Therefore, IgG4 is believed to be a marker of exposure to food and possibly of tolerance 5. Further research is required to clarify any role for specific IgG measurement in the assessment of a patient with potential food allergy.
Food allergy testing
There’s no perfect test used to confirm or rule out a food allergy. Food allergy involves your immune system overreacting to a particular protein found in that food and unlike an intolerance to food, a food allergy can cause a serious or even life-threatening reaction by eating a microscopic amount, touching or inhaling the food. For food allergies, the quantity of food consumed often doesn’t matter and even contact of the food with the skin may provoke a reaction. According to the National Institute of Allergy and Infectious Diseases, it doesn’t take much food to cause a severe allergic reaction—1/44,000 of a peanut can cause a severe reaction in a highly allergic person. On the other hand, food intolerances and sensitivities, increased consumption usually worsens symptoms. Experts recommend food allergy testing only after symptoms of an allergy have occurred. Many people who think they are allergic to a food may actually be intolerant to it. Some of the symptoms of food intolerance and food allergy are similar. Individuals with suspected food allergies should see an allergist – specialist doctor trained to help people prevent, diagnose and manage their allergies and other immune system diseases.
Some facts about food allergies:
- Eggs, milk, and peanuts are the most common causes of food allergies in children.
- Peanuts, tree nuts, fish, and shellfish commonly cause the most severe reactions.
- Nearly 1 in 20 children under the age of 5 years have food allergies.
- From 1997 to 2007, food allergies increased by 18% among children under age 18 years.
- Most children “outgrow” their allergies. But allergies to peanuts, tree nuts, and shellfish may be lifelong.
There is no single test to look for all food allergies and tests can show signs of an allergy when no real allergic reaction occurs. This is known as a false positive result. Because a test that looks for all possible allergens can return many false positives, doctors normally order food allergy tests that look only for specific allergens based on your history of symptoms.
About 9 in 10 food allergies are caused by these foods:
- Cow’s milk
- Eggs
- Fish
- Peanuts
- Sesame
- Shellfish
- Soy
- Tree nuts
- Wheat
Food allergy diagnosis is made based on the following:
- History of symptoms, including frequency, severity and diet/nutrition
- Your family history of allergies. Also share information about members of your family who have allergies of any kind.
- A physical examination. A careful exam can often identify or exclude other medical problems.
- Skin prick test involves putting a drop of a possible allergen on your skin and then poking that area with a very small needle to let the substance get just beneath the top layer of skin. Even though you don’t eat the food, an allergic reaction is still detected in the skin. This test must be performed under careful medical supervision in case a severe reaction occurs.
- Allergy blood test measures levels of proteins called immunoglobulin-E (IgE) that can be elevated when you have an allergy to a specific food.
- Oral food challenge includes eating progressively larger amounts of a food at specified intervals over a period of a few hours. During the test, you are closely monitored by a doctor to see if there is an allergic reaction and to immediately treat a severe reaction if it occurs.
- Food elimination is not a strict testing method, but it may be employed to prepare for other tests and to see if avoiding a food reduces allergy symptoms. Food elimination generally requires carefully controlling your diet for a period of time to ensure that you have no exposure to one or more potential allergens.
While other types of tests may be marketed as food allergy tests, experts and professional organizations discourage their use because they are not proven to accurately determine when a person has a true allergy.
Skin prick test
Allergy skin prick test involves injecting a small amount of the suspected allergen under your skin. In this test, a small amount of the suspected food is placed on the skin of your forearm or back. A doctor then pricks your skin with a needle to allow a tiny amount of the substance beneath your skin surface. Even though you don’t eat the food, an allergic reaction is still detected in the skin. If you’re allergic to a particular substance being tested, you develop a raised bump or reaction. However, a positive reaction to this test alone isn’t enough to confirm a food allergy.
Blood test
Allergy blood test can measure your immune system’s response to particular foods by measuring the allergy-related antibody known as immunoglobulin E (IgE). For this test, a blood sample taken in your care professional’s office is sent to a medical laboratory. It will then be tested for different foods. However, a blood test is not always reliable as you can have a negative test result (no antibodies detected) and still be allergic. The opposite is also true: A test may detect antibodies to certain foods, but you may never have an allergic reaction.
Elimination diet
You may be asked to eliminate suspect foods for a week or two and then add the food items back into your diet one at a time. This process can help link symptoms to specific foods. However, elimination diets aren’t foolproof. An elimination diet can’t tell you whether your reaction to a food is a true allergy instead of a food sensitivity. Also, if you’ve had a severe reaction to a food in the past, an elimination diet may not be safe.
Oral food challenge
During food challenges, done in a allergist’s or immunologist’s office where the proper equipment and expertise are available in the event of severe anaphylactic reaction, you’ll be given small but increasing amounts of the food suspected of causing your symptoms. If you don’t have a reaction during this test, you may be able to include this food in your diet again.
At home food allergy test
at home food allergy test kits are available for food allergy blood testing. These tests involve pricking your finger and putting one or more drops of blood on a test strip. You then mail the test strip to a laboratory that analyzes your blood immunoglobulin for signs of a potential allergy.
A positive test result alone cannot diagnose a food allergy. Instead, a doctor must evaluate your symptoms and health history along with any test results. When you discuss your symptoms with your doctor prior to testing, the doctor can look for the most likely allergens. However, this is not possible with at home food allergy tests that look for a predetermined list of allergens.
Because allergy blood testing can return false-positive results, your doctor will likely want to do follow-up testing if your at home food allergy test indicates that you may have an allergy.
Follow-up exams by a doctor who specializes in allergies may be necessary if there are indications that you may have a food allergy.
Best at home food allergy tests
Most at-home food allergy tests are self-collection tests, which means that you take a sample at home and send it to a lab where it can be analyzed. There are many types of at home food allergy tests available, and only tests that measure immunoglobulin E (IgE) in the blood are known to potentially help identify food allergies. Other types of at home food allergy tests are considered to be unvalidated and unproven and are not recommended by most experts.
Blood tests for allergen-specific immunoglobulin E (IgE) levels are a useful tool in identifying possible allergies, but they are not perfect. Blood tests for allergen-specific immunoglobulin E (IgE) levels use a blood sample that is taken by pricking your finger with a small needle. A test may include levels for one or more allergens. Although broad tests may seem beneficial, doctors generally recommend against them because of the risk of misleading results because IgE levels do not perfectly correspond to actual allergies, so it is possible to test positive when you are not actually allergic or test negative when you really do have an allergy. Furthermore, due to cross-reactivity of various antigens, a false positive blood test may occur.
Some other factors that can affect the overall accuracy of food allergy testing include:
- Lack of established reference ranges: For some types of foods, there is no consensus about what levels of IgE are most likely to correctly indicate a food allergy. In addition, most studies to validate IgE levels have been done in children, so there may be more difficulty in interpreting test results in adults.
- Variation among laboratory methods: There are different methods and technologies for analyzing blood for allergen-specific IgE. Results are not always interchangeable between them, which may create variability in accuracy depending on how the laboratory analysis is conducted.
Biodivision Diagnostics – Victus88 Food Allergy Test
- Price: $495 (test only), $560 (test + consultation)
- Type: Self-collection or in-person
- Sample: Blood
- Tests for: 382 foods, 88 antigens, and four biomarkers
- Results timeline: 14 to 21 business days
One of the most comprehensive food allergy tests on the market, the Victus88 from Biovision Diagnostics consists of a simple blood test that checks for four key allergy biomarkers: immunoglobulin E (IgE), immunoglobulin G (IgG), immunoglobulin G4 (IgG4), and C3D complement response. These four biomarkers can be used to identify 88 antigens in 382 different foods.
A painless finger prick extracts your blood sample. Those who wish to self-collect can request a kit for at-home blood drawing when they order Victus88. You can also choose your own phlebotomist to draw the blood, in which case you’ll need to handle shipping the specimen to Biovision Diagnostics. Alternatively, you can schedule an appointment with Getlabs or Travalabs mobile blood labs — they’ll handle shipping for you. Most people receive their full results within three weeks.
By measuring all four biomarkers, Victus88 not only identifies which foods you’re allergic to but also the severity of your allergies. After completing the test, you’ll receive a “Green Light/Red Light” report to give you a full picture of your gut health. The report lays out everything you need to know in clear, concise language with a full breakdown of what each biomarker signifies and dietary tips based on your allergies.
Victus88 is fairly expensive, but may prove invaluable if you’re struggling with your day-to-day diet and suspect a food allergy may be at play. For an additional fee, you can schedule an online follow-up consultation with one of Biodivision Diagnostics’ dietary experts.
Everlywell Food Sensitivity Comprehensive Test
- Price: $299
- Type: At-home
- Sample: Blood
- Tests for: Immunoglobulin G sensitivity to 204 foods
- Results timeline: 2 to 3 weeks
Everlywell’s Food Sensitivity Comprehensive Test measures your immunoglobulin G (IgG) reactivity toward 204 different foods. These include the following:
- 15 dairy products
- Egg whites and yolks
- 35 fruits
- 37 vegetables
- 13 grains
- 13 legumes
- Seven types of meat
- 25 varieties of seafood
- 16 seeds and nuts
- 41 spices
The test can be administered at home using lancels to collect your blood sample. All equipment needed for collection is included with your order, and detailed instructions for using the lancets and storing the specimen can be found on the test’s product page. Most people receive results within a few weeks of mailing their sample, which is analyzed at one of Everlywell’s CLIA-certified labs.
Each food is rated on a 0-3 scale ranging from normal reactivity to high reactivity. The more reactive a certain food is, the likelier you are to be allergic to it. After your results are processed, you’ll receive a personalized report. Everlywell works with you to establish a two-step elimination diet that cuts out any potential allergens.
The test is available to adults 18 and older. Although most insurance companies won’t cover the cost of your Food Sensitivity Comprehensive Test, you may be able to pay for the test using an HSA or FSA card.
Interpreting At-Home Food Allergy Test Results
Results from at-home food allergy tests are normally provided through a website or smartphone app. The test report typically lists the levels of immunoglobulin E (IgE) for specific allergens and may indicate whether those levels are low, medium, or high.
It is important to remember that immunoglobulin E (IgE) levels alone are not able to diagnose a food allergy. People without an allergy can have an elevated immunoglobulin E (IgE), and people with an allergy do not always have higher immunoglobulin E (IgE) for that allergen.
For this reason, diagnosis of a food allergy must involve consultation with a doctor. By reviewing any allergy symptoms and their potential triggers, a doctor can most effectively interpret an allergy blood test.
A positive test may show a higher likelihood of a reaction to a particular allergen, but IgE levels do not definitely prove an allergy exists. Even when an allergy exists, IgE levels do not correspond to the severity of the allergy.
In many cases, a negative result on a food allergy blood test is an indication that you are tolerant of that food and can consume it without having an allergic reaction. However, this is not always the case, which is why test results must always be interpreted by a physician in the context of past allergy symptoms.
Even though a test report may offer a simple tool for seeing your IgE levels for specific allergens, reviewing your test results with your doctor or an allergist is essential to fully understanding whether you are likely to have a food allergy.
At-home food allergy test versus doctor food allergy testing
At-home food allergy tests can be purchased without a prescription, making it simple to have your blood tested for IgE levels associated with specific allergens. However, it’s important to be aware of how this testing compares with typical food allergy testing ordered by a doctor.
A major difference is that a doctor can prescribe tailored allergy testing based on your situation. This includes deciding between a skin or blood test as well as determining the allergens that have the highest potential to be causing your symptoms.
Once the results from doctor-prescribed tests are ready, the doctor carefully interprets those results in the context of your symptoms. With at-home tests, you may receive a detailed report, but in-depth medical consultation about your results is not always included.
Doctor-prescribed allergy blood tests normally involve a blood sample that is taken from a vein in your arm. At-home food allergy tests, on the other hand, use drops of blood that come from pricking your finger with a small needle.
Costs can also vary depending on how and where your test is conducted. Health insurance providers often pay for at least part of allergy testing if it is prescribed by a doctor. For at-home food allergy testing, you will normally have to pay the full cost yourself.
How are food sensitivity or food intolerance treated?
Food sensitivity or food intolerance treatment is based on avoiding or reducing your intake of problem foods and treating symptoms when you do eat a problem food; for example, taking an antacid medication for heartburn or stomachache.
Elimination diets
The only reliable way to determine if diet is playing a role is by people being placed on a temporary elimination diet, under the supervision of a dietitian and medical practitioner.
If removing the food from the diet helps, this is followed by challenges under controlled conditions to identify food triggers which may need to be avoided in the future.
It is important that elimination diets are temporary, so they should only be undertaken for a short term trial period, under strict medical supervision, as a diagnostic tool. Prolonged restricted diets can lead to problems with adequate nutrition, particularly in children.
It is important to note that low salicylate and low amine diets should not be used for investigation of food intolerance until other potential causes for reactions are explored.
What is food allergy?
Food allergy is an immune system reaction (antibody mediated) that occurs soon after eating a certain food. A food allergy is caused by an overreaction of the immune system due to your body mistaking an ingredient in food — usually a protein — as harmful and creates a defense system (immunoglobulin E [IgE]) to fight it. An allergic reaction occurs when the antibodies are battling an “invading” food protein. The most common food allergies are shellfish, nuts, fish, eggs, peanuts, and milk. Even a tiny amount of the allergy-causing food can trigger signs and symptoms such as digestive problems, hives or swollen airways. In some people, a food allergy can cause severe symptoms or even a life-threatening reaction known as anaphylaxis. If you’ve had allergic reactions to food or insect bites, your doctor will prescribe an epinephrine (adrenaline) injection (Adrenaclick, Auvi-Q, EpiPen) for emergency self-treatment.
Food allergy affects an estimated 8% of children under age 5 and up to 4% of adults. While there’s no cure, some children outgrow their food allergies as they get older.
It’s easy to confuse a food allergy with a much more common reaction known as food intolerance. While bothersome, food intolerance is a less serious condition that does not involve the immune system.
Table 2. Different types of food allergies
| IgE-mediated Reactions | Mixed Allergic Reactions | Non-IgE-mediated Reactions |
|---|---|---|
| Food ingestion reactions within 2 hours of ingestion | Atopic Dermatitis | Food Protein Induced Enteropathy (FPE) |
| “Alpha Gal” Allergy | Eosinophilic Esophagitis (EoE) | Food Protein Induced Enterocolitis (FPIES) |
| Oral Allergy Syndrome (OAS) | Eosinophilic Gastritis (EG) | Food Protein Induced Proctitis (FPIAP) |
| Food Dependent Exercise Induced Anaphylaxis (FDEIAn) | Celiac disease |
What are the symptoms of a food allergy?
Symptoms of a food allergy can range from mild to severe, and the amount of food necessary to trigger a reaction varies from person to person. For some people, an allergic reaction to a particular food may be uncomfortable but not severe. For other people, an allergic food reaction can be frightening and even life-threatening. Food allergy symptoms normally develop within a few minutes to 2 hours after eating the offending food. Rarely, symptoms may be delayed for several hours.
Symptoms of a food allergy may include:
- Tingling or itching in the mouth
- Rash or hives (red, itchy skin)
- Nausea
- Cramping stomach pain
- Vomiting
- Diarrhea
- Itchy skin
- Shortness of breath
- Stuffy or itchy nose, sneezing or itchy, teary eyes
- Angioedema or swelling of the lips, face, tongue and throat or other parts of the body
- Chest pain
- Swelling of the airways to the lungs
In some cases, food allergies can cause a severe reaction called anaphylaxis. Anaphylaxis is a very serious and potentially fatal allergic reaction that involves a sudden drop in blood pressure, loss of consciousness and body system failure. Signs of anaphylaxis include:
- Hoarseness, throat tightness or a lump in the throat
- Wheezing, chest tightness or trouble breathing
- Tingling in the hands, feet, lips or scalp
- Shock with a severe drop in blood pressure
- Rapid pulse
- Dizziness, lightheadedness or loss of consciousness
People with food allergy should always carry auto-injectable epinephrine to be used in the event of an anaphylactic reaction. If you experience any of these symptoms in the context of eating, use the epinephrine auto-injector and immediately call your local emergency number. Don’t wait to see if your symptoms go away or get better on their own.
Food allergy diagnosis
There’s no perfect test used to confirm or rule out a food allergy. Your doctor will consider a number of factors before making a diagnosis. These factors include:
- Your symptoms. Give your doctor a detailed history of your symptoms — which foods, and how much, seem to cause problems.
- Your family history of allergies. Also share information about members of your family who have allergies of any kind.
- A physical examination. A careful exam can often identify or exclude other medical problems.
- A skin test. A skin prick test can determine your reaction to a particular food. In this test, a small amount of the suspected food is placed on the skin of your forearm or back. A doctor or another health care provider then pricks your skin with a needle to allow a tiny amount of the substance beneath your skin surface. If you’re allergic to a particular substance being tested, you develop a raised bump or reaction. Keep in mind, a positive reaction to this test alone isn’t enough to confirm a food allergy.
- A blood test. A blood test can measure your immune system’s response to particular foods by measuring the allergy-related antibody known as immunoglobulin E (IgE). For this test, a blood sample taken in your doctor’s office is sent to a medical laboratory, where different foods can be tested.
- Elimination diet. You may be asked to eliminate suspect foods for a week or two and then add the food items back into your diet one at a time. This process can help link symptoms to specific foods. However, elimination diets aren’t foolproof. An elimination diet can’t tell you whether your reaction to a food is a true allergy instead of a food sensitivity. Also, if you’ve had a severe reaction to a food in the past, an elimination diet may not be safe.
- Oral food challenge. During this test, done in the doctor’s office, you’ll be given small but increasing amounts of the food suspected of causing your symptoms. If you don’t have a reaction during this test, you may be able to include this food in your diet again.
The gold standard for diagnosis of immunoglobulin E (IgE)-mediated food allergy remains the oral food challenge, with serum IgE testing and skin prick testing serving as acceptable alternatives 49.
How are food allergies treated?
There is currently no cure for food allergy, but there are many promising treatments under investigation and one treatment currently being studied as a treatment for food allergy is oral immunotherapy. In this treatment, small doses of the food you’re allergic to are swallowed or placed under your tongue (sublingual). The dose of the allergy-provoking food is gradually increased.
The U.S. Food and Drug Administration (FDA) has recently approved the first oral immunotherapy treatment, Peanut (Arachis hypogaea) Allergen Powder-dnfp (Palforzia), to help reduce the severity of allergic reactions to peanuts, including anaphylaxis, in children aged 4 through 17 with a confirmed peanut allergy. This medication isn’t recommended for people with uncontrolled asthma or certain conditions, including eosinophilic esophagitis.
For a minor allergic reaction, prescribed antihistamines or those available without a prescription may help reduce symptoms. These drugs can be taken after exposure to an allergy-causing food to help relieve itching or hives. However, antihistamines can’t treat a severe allergic reaction.
For a severe allergic reaction, you may need an emergency injection of epinephrine and a trip to the emergency room. Many people with allergies carry an epinephrine autoinjector (Adrenaclick, EpiPen). This device is a combined syringe and concealed needle that injects a single dose of medication when pressed against your thigh.
If your doctor has prescribed an epinephrine autoinjector:
- Be sure you know how to use the autoinjector. Also, make sure the people closest to you know how to administer the drug — if they’re with you in an anaphylactic emergency, they could save your life.
- Carry it with you at all times. It may be a good idea to keep an extra autoinjector in your car or in your desk at work.
- Always be sure to replace epinephrine before its expiration date or it may not work properly.
On the whole, however, avoidance, education and preparedness are the keys to managing food allergy.
- Always ask about ingredients when eating at restaurants or when you are eating foods prepared by family or friends. Also, make sure food isn’t prepared on surfaces or in pans that contained any of the food you’re allergic to.
- Carefully read food labels. The United States and many other countries require that major food allergens are to be listed in common language (milk, egg, fish, shellfish, tree nuts, wheat, peanuts and soybeans).
- If you have already had a severe reaction, wear a medical alert bracelet or necklace that lets others know that you have a food allergy in case you have a reaction and you’re unable to communicate.
- Carry and know how to use auto-injectable epinephrine (Adrenaclick, EpiPen) and antihistamines to treat emergency reactions. Teach family members and other people close to you how to use epinephrine. If a reaction occurs, have someone take you to the emergency room, even if symptoms subside. Afterwards, get follow-up care from your allergist.
If your child has a food allergy, take these precautions to ensure his or her safety:
- Notify key people that your child has a food allergy. Talk with child care providers, school personnel, parents of your child’s friends and other adults who regularly interact with your child. Emphasize that an allergic reaction can be life-threatening and requires immediate action. Make sure that your child also knows to ask for help right away if he or she reacts to food.
- Explain food allergy symptoms. Teach the adults who spend time with your child how to recognize signs and symptoms of an allergic reaction.
- Write an action plan. Your plan should describe how to care for your child when he or she has an allergic reaction to food. Provide a copy of the plan to your child’s school nurse and others who care for and supervise your child.
- Have your child wear a medical alert bracelet or necklace. This alert lists your child’s allergy symptoms and explains how others can provide first aid in an emergency.
While exposure to airborne food allergens (e.g., from cooking vapors) usually does not result in anaphylaxis, it can cause a runny nose and itchy eyes similar to a reaction from coming in contact with pollen. However, eating even a small amount of the food, such as that left on cooking utensils or from a food processing facility, can cause a life-threatening reaction. This is why reading the ingredients on food labels and asking questions about prepared foods are an essential part of avoidance plans.
People with food allergy should always carry auto-injectable epinephrine to be used in the event of an anaphylactic reaction. Symptoms of anaphylaxis may include difficulty breathing, dizziness or loss of consciousness. If you have any of these symptoms in the context of eating, use the epinephrine auto-injector and immediately call 911. Don’t wait to see if your symptoms go away or get better on their own.
Outgrowing food allergies
Most children outgrow their allergies to cow’s milk, egg, soy and wheat, even if they have a history of a severe reaction. However, peanut, tree nut fish and shellfish allergy tends to persist through adulthood. Repeat allergy testing with your allergist can help you learn when you or your child’s food allergies are resolving with time.
References- Food Intolerance. https://www.allergy.org.au/patients/food-other-adverse-reactions/food-intolerance
- Stapel SO, Asero R, Ballmer-Weber BK. et al. Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI Task Force Report. Allergy. 2008;63:793–796. doi: 10.1111/j.1398-9995.2008.01705.x
- Boyce JA, Assa’ad A, Burks AW, et al. NIAID-Sponsored Expert Panel. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report. J Allergy Clin Immunol. 2010 Dec;126(6):1105-18. doi: 10.1016/j.jaci.2010.10.008
- Lavine E. Blood testing for sensitivity, allergy or intolerance to food. CMAJ. 2012 Apr 3;184(6):666-8. doi: 10.1503/cmaj.110026
- Bock SA. AAAAI support of the EAACI Position Paper on IgG4. J Allergy Clin Immunol. 2010 Jun;125(6):1410. doi: 10.1016/j.jaci.2010.03.013
- What Is Food Sensitivity? https://www.testing.com/food-sensitivity-testing
- Carr S, Chan E, Lavine E, Moote W. CSACI Position statement on the testing of food-specific IgG. Allergy Asthma Clin Immunol. 2012 Jul 26;8(1):12. doi: 10.1186/1710-1492-8-12
- American Academy of Allergy, Asthma & Immunology Position Statement. https://www.aaaai.org/Aaaai/media/Media-Library-PDFs/Tools%20for%20the%20Public/Conditions%20Library/Library%20-%20Allergies/eacci-igg4-2010.pdf
- Boyce, Joshua A et al. “Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report.” The Journal of allergy and clinical immunology vol. 126,6 (2010): 1105-18. https://doi.org/10.1016/j.jaci.2010.10.008
- Food Intolerance. https://www.allergy.org.au/patients/food-other-adverse-reactions/food-intolerance
- Lopez CM, Yarrarapu SNS, Mendez MD. Food Allergies. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482187
- Bright DM, Stegall HL, Slawson DC. Food Allergies: Diagnosis, Treatment, and Prevention. Am Fam Physician. 2023 Aug;108(2):159-165. https://www.aafp.org/pubs/afp/issues/2023/0800/food-allergies.html
- Barni S, Liccioli G, Sarti L, Giovannini M, Novembre E, Mori F. Immunoglobulin E (IgE)-Mediated Food Allergy in Children: Epidemiology, Pathogenesis, Diagnosis, Prevention, and Management. Medicina (Kaunas). 2020 Mar 4;56(3):111. doi: 10.3390/medicina56030111
- Chang KL, Guarderas JC. Allergy Testing: Common Questions and Answers. Am Fam Physician. 2018 Jul 1;98(1):34-39. https://www.aafp.org/pubs/afp/issues/2018/0701/p34.html
- Budimir J, Mravak-Stipetić M, Bulat V, Ferček I, Japundžić I, Lugović-Mihić L. Allergic reactions in oral and perioral diseases-what do allergy skin test results show? Oral Surg Oral Med Oral Pathol Oral Radiol. 2019 Jan;127(1):40-48. doi: 10.1016/j.oooo.2018.08.001
- Sicherer SH, Sampson HA. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018 Jan;141(1):41-58. doi: 10.1016/j.jaci.2017.11.003
- Burks AW, Tang M, Sicherer S, Muraro A, Eigenmann PA, Ebisawa M, Fiocchi A, Chiang W, Beyer K, Wood R, Hourihane J, Jones SM, Lack G, Sampson HA. ICON: food allergy. J Allergy Clin Immunol. 2012 Apr;129(4):906-20. doi: 10.1016/j.jaci.2012.02.001
- Rial MJ, Sastre J. Food Allergies Caused by Allergenic Lipid Transfer Proteins: What Is behind the Geographic Restriction? Curr Allergy Asthma Rep. 2018 Sep 11;18(11):56. doi: 10.1007/s11882-018-0810-x
- Shroba J, Rath N, Barnes C. Possible Role of Environmental Factors in the Development of Food Allergies. Clin Rev Allergy Immunol. 2019 Dec;57(3):303-311. doi: 10.1007/s12016-018-8703-2
- NIAID-Sponsored Expert Panel; Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010 Dec;126(6 Suppl):S1-58. doi: 10.1016/j.jaci.2010.10.007
- Sampson HA, Aceves S, Bock SA, James J, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol. 2014 Nov;134(5):1016-25.e43. doi: 10.1016/j.jaci.2014.05.013
- Sampson HA. Utility of food-specific IgE concentrations in predicting symptomatic food allergy. J Allergy Clin Immunol. 2001 May;107(5):891-6. doi: 10.1067/mai.2001.114708
- Chinthrajah RS, Tupa D, Prince BT, Block WM, Rosa JS, Singh AM, Nadeau K. Diagnosis of Food Allergy. Pediatr Clin North Am. 2015 Dec;62(6):1393-408. doi: 10.1016/j.pcl.2015.07.009
- Muraro A., Werfel T., Hoffmann-Sommergruber K., Roberts G., Beyer K., Bindslev-Jensen C., Cardona V., Dubois A., duToit G., Eigenmann P., et al. EAACI Food Allergy and Anaphylaxis Guidelines Group. EAACI food allergy and anaphylaxis guidelines: Diagnosis and management of food allergy. Allergy. 2014;69:1008–1025. doi: 10.1111/all.12429
- Sampson HA, Aceves S, Bock SA, James J, Jones S, Lang D, Nadeau K, Nowak-Wegrzyn A, et al. Food allergy: a practice parameter update-2014. J Allergy Clin Immunol. 2014 Nov;134(5):1016-25.e43. doi: 10.1016/j.jaci.2014.05.013
- Brockow K, Kneissl D, Valentini L, Zelger O, Grosber M, Kugler C, Werich M, Darsow U, Matsuo H, Morita E, Ring J. Using a gluten oral food challenge protocol to improve diagnosis of wheat-dependent exercise-induced anaphylaxis. J Allergy Clin Immunol. 2015 Apr;135(4):977-984.e4. doi: 10.1016/j.jaci.2014.08.024
- Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, Bernstein JA, Burks AW, Feldweg AM, Fink JN, Greenberger PA, Golden DB, James JM, Kemp SF, Ledford DK, Lieberman P, Sheffer AL, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, Lang D, Nicklas RA, Oppenheimer J, Portnoy JM, Randolph C, Schuller DE, Spector SL, Tilles S, Wallace D. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol. 2010 Sep;126(3):477-80.e1-42. doi: 10.1016/j.jaci.2010.06.022. Epub 2010 Aug 7. Erratum in: J Allergy Clin Immunol. 2010 Dec;126(6):1104.
- Ravelli A, Villanacci V, Chiappa S, Bolognini S, Manenti S, Fuoti M. Dietary protein-induced proctocolitis in childhood. Am J Gastroenterol. 2008 Oct;103(10):2605-12. doi: 10.1111/j.1572-0241.2008.02035.x
- Jenkins, H. R., Pincott, J. R., Soothill, J. F., Milla, P. J., & Harries, J. T. (1984). Food allergy: the major cause of infantile colitis. Archives of disease in childhood, 59(4), 326–329. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1628682/pdf/archdisch00735-0040.pdf
- Lake AM. Food-induced eosinophilic proctocolitis. J Pediatr Gastroenterol Nutr. 2000;30 Suppl:S58-60. doi: 10.1097/00005176-200001001-00009
- Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, Plaut M, Cooper SF, Fenton MJ. Guidelines for the Diagnosis and Management of Food Allergy in the United States: summary of the NIAID-sponsored expert panel report. J Am Diet Assoc. 2011 Jan;111(1):17-27. doi: 10.1016/j.jada.2010.10.033
- Lake AM, Whitington PF, Hamilton SR. Dietary protein-induced colitis in breast-fed infants. J Pediatr. 1982 Dec;101(6):906-10. doi: 10.1016/s0022-3476(82)80008-5
- Lucarelli, S., Di Nardo, G., Lastrucci, G., D’Alfonso, Y., Marcheggiano, A., Federici, T., Frediani, S., Frediani, T., & Cucchiara, S. (2011). Allergic proctocolitis refractory to maternal hypoallergenic diet in exclusively breast-fed infants: a clinical observation. BMC gastroenterology, 11, 82. https://doi.org/10.1186/1471-230X-11-82
- Arvola T, Ruuska T, Keränen J, Hyöty H, Salminen S, Isolauri E. Rectal bleeding in infancy: clinical, allergological, and microbiological examination. Pediatrics. 2006 Apr;117(4):e760-8. doi: 10.1542/peds.2005-1069
- Xanthakos SA, Schwimmer JB, Melin-Aldana H, Rothenberg ME, Witte DP, Cohen MB. Prevalence and outcome of allergic colitis in healthy infants with rectal bleeding: a prospective cohort study. J Pediatr Gastroenterol Nutr. 2005 Jul;41(1):16-22. doi: 10.1097/01.mpg.0000161039.96200.f1
- Iyngkaran N, Yadav M, Boey CG, Lam KL. Severity and extent of upper small bowel mucosal damage in cow’s milk protein-sensitive enteropathy. J Pediatr Gastroenterol Nutr. 1988 Sep-Oct;7(5):667-74. doi: 10.1097/00005176-198809000-00008
- Walker-Smith JA. Cow milk-sensitive enteropathy: predisposing factors and treatment. J Pediatr. 1992 Nov;121(5 Pt 2):S111-5. doi: 10.1016/s0022-3476(05)81418-0
- Kleinman RE. Milk protein enteropathy after acute infectious gastroenteritis: experimental and clinical observations. J Pediatr. 1991 Apr;118(4 Pt 2):S111-5. doi: 10.1016/s0022-3476(05)81437-4
- Kuitunen, P., Visakorpi, J. K., Savilahti, E., & Pelkonen, P. (1975). Malabsorption syndrome with cow’s milk intolerance. Clinical findings and course in 54 cases. Archives of disease in childhood, 50(5), 351–356. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1544424/pdf/archdisch00841-0031.pdf
- Dellon, E. S., & Hirano, I. (2018). Epidemiology and Natural History of Eosinophilic Esophagitis. Gastroenterology, 154(2), 319–332.e3. https://doi.org/10.1053/j.gastro.2017.06.067
- Rank, Matthew A et al. “Technical review on the management of eosinophilic esophagitis: a report from the AGA institute and the joint task force on allergy-immunology practice parameters.” Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology vol. 124,5 (2020): 424-440.e17. doi:10.1016/j.anai.2020.03.021
- Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report. J Allergy Clin Immunol. 2010;126(6):1105-1118. Boyce, J. A., Assa’ad, A., Burks, A. W., Jones, S. M., Sampson, H. A., Wood, R. A., Plaut, M., Cooper, S. F., Fenton, M. J., Arshad, S. H., Bahna, S. L., Beck, L. A., Byrd-Bredbenner, C., Camargo, C. A., Jr, Eichenfield, L., Furuta, G. T., Hanifin, J. M., Jones, C., Kraft, M., Levy, B. D., … NIAID-Sponsored Expert Panel (2010). Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report. The Journal of allergy and clinical immunology, 126(6), 1105–1118. https://doi.org/10.1016/j.jaci.2010.10.008
- Lavine E. (2012). Blood testing for sensitivity, allergy or intolerance to food. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 184(6), 666–668. https://doi.org/10.1503/cmaj.110026
- Hamilton RG. Clinical laboratory assessment of immediate-type hypersensitivity. J Allergy Clin Immunol. 2010 Feb;125(2 Suppl 2):S284-96. doi: 10.1016/j.jaci.2009.09.055
- Husby S. Normal immune responses to ingested foods. J Pediatr Gastroenterol Nutr. 2000;30 Suppl:S13-9. doi: 10.1097/00005176-200001001-00003
- Tomicić S, Norrman G, Fälth-Magnusson K, Jenmalm MC, Devenney I, Böttcher MF. High levels of IgG4 antibodies to foods during infancy are associated with tolerance to corresponding foods later in life. Pediatr Allergy Immunol. 2009 Feb;20(1):35-41. doi: 10.1111/j.1399-3038.2008.00738.x
- Jones, S. M., Pons, L., Roberts, J. L., Scurlock, A. M., Perry, T. T., Kulis, M., Shreffler, W. G., Steele, P., Henry, K. A., Adair, M., Francis, J. M., Durham, S., Vickery, B. P., Zhong, X., & Burks, A. W. (2009). Clinical efficacy and immune regulation with peanut oral immunotherapy. The Journal of allergy and clinical immunology, 124(2), 292–300.e3097. https://doi.org/10.1016/j.jaci.2009.05.022
- Chinthrajah, R. S., Tupa, D., Prince, B. T., Block, W. M., Rosa, J. S., Singh, A. M., & Nadeau, K. (2015). Diagnosis of Food Allergy. Pediatric clinics of North America, 62(6), 1393–1408. https://doi.org/10.1016/j.pcl.2015.07.009
- Hammond C, Lieberman JA. Unproven Diagnostic Tests for Food Allergy. Immunol Allergy Clin North Am. 2018 Feb;38(1):153-163. doi: 10.1016/j.iac.2017.09.011