What is graft versus host disease
Graft-versus-host disease is a life-threatening complication that can occur after certain stem cell or bone marrow transplants. Graft-versus-host disease happens when the cells from your donor (the graft) see your body’s cells (the host) as different and attack them. Graft versus host disease means the graft (cells from your donor) reacts against the host (your body’s cells). The graft is the donated marrow or stem cells. The host is the person receiving the transplant. Graft versus host disease can cause diarrhea, skin rashes and liver damage.
Graft versus host disease may occur after a bone marrow, or stem cell, transplant in which someone receives bone marrow tissue or cells from a donor. This type of transplant is called allogeneic. The new, transplanted cells regard the recipient’s body as foreign. When this happens, the cells attack the recipient’s body.
Graft versus host disease does not occur when people receive their own cells. This type of transplant is called autologous.
Graft versus host disease happens when particular types of white blood cell (T cells) in the donated bone marrow or stem cells attack your own body cells. This happens because the donated cells (the graft) see your body cells (the host) as foreign and attack them.
Some people have a very mild form which doesn’t last long. For others, graft versus host disease can be severe. It may even be life threatening in a few cases. Some people may have graft versus host disease over many months, or even years.
There are medicines to help lower your risk of getting graft versus host disease. But even with medicine, some people still get graft versus host disease.
Before a transplant, tissue and cells from possible donors are checked to see how closely they match the recipient. graft versus host disease is less likely to occur, or symptoms will be milder, when the match is close. The chance of graft versus host disease is:
- Around 35% to 45% when the donor and recipient are related.
- Around 60% to 80% when the donor and recipient are not related.
Graft-versus-host disease can range from mild to severe. Many patients will have some symptoms of graft versus host disease after transplant.
Having some graft versus host disease is not always bad. If your transplant was for a blood cancer, your doctor may see mild graft versus host disease as a good thing. It’s a sign that the new cells are working to destroy any cancer cells that are still in your body. Patients who have some graft versus host disease may have a lower risk of the cancer returning after transplant.
The type of graft versus host disease you have depends on when it starts after your transplant. Doctors also look at:
- what parts of the body are affected
- how badly your body has been affected
- the biopsy results
Types of graft versus host disease:
- Acute graft versus host disease: Typically develops in the early weeks and months after transplant. It’s called Late Acute graft versus host disease when it develops 3 or more months after transplant.
- Chronic graft versus host disease: Typically develops within 1 year of transplant. It’s called Overlap Chronic graft versus host disease when signs and symptoms of chronic and acute graft versus host disease appear together.
Acute graft versus host disease
Acute graft versus host disease generally starts within 100 days of your transplant but it can sometimes happen after this time. It usually happens about 2 to 3 weeks after your transplant when your new bone marrow begins to make blood cells. This is called engraftment.
It can be mild or severe, and often starts with a rash on:
- the palms of your hands
- the soles of your feet
- your ears
- your face
The rash may be itchy or painful. It may also affect your mouth, gut (digestive system) and liver. This can cause:
- diarrhea
- sickness
- loss of appetite
- yellowing of the skin (jaundice)
Your doctor assesses your graft versus host disease to decide what treatment you need. The treatment aims to manage your symptoms and treat the graft versus host disease.
Assessing graft versus host disease
Your doctor assesses your graft versus host disease and gives it a grade. There are 4 grades which range from grade 1 to grade 4. The grade depends on:
- the number of organs affected (skin, bowel, or liver) – graft versus host disease can affect any or all of these 3 organs
- how bad the graft versus host disease is
Your treatment depends on the grade of your graft versus host disease. You may not need any treatment if you have grade 1 graft versus host disease, but you will need some type of treatment for grade 2 or above.
- Grade 1 is mild graft versus host disease. It means up to a quarter (25%) of your skin is affected.
- Grade 2 is moderate graft versus host disease. It means up to half your skin (25 to 50%) is affected. There are mild changes in your liver or you may have some mild diarrhea or feel sick.
- Grade 3 is severe graft versus host disease. It means more than half your skin (over 50%) is affected. You may look as though you have severe sunburn. Your liver is affected and you have stomach cramps and diarrhea.
- Grade 4 is very severe graft versus host disease. Your skin has blistered and may have broken down in places. Your skin may be yellow (jaundiced) because your liver is not working properly. You have severe diarrhea.
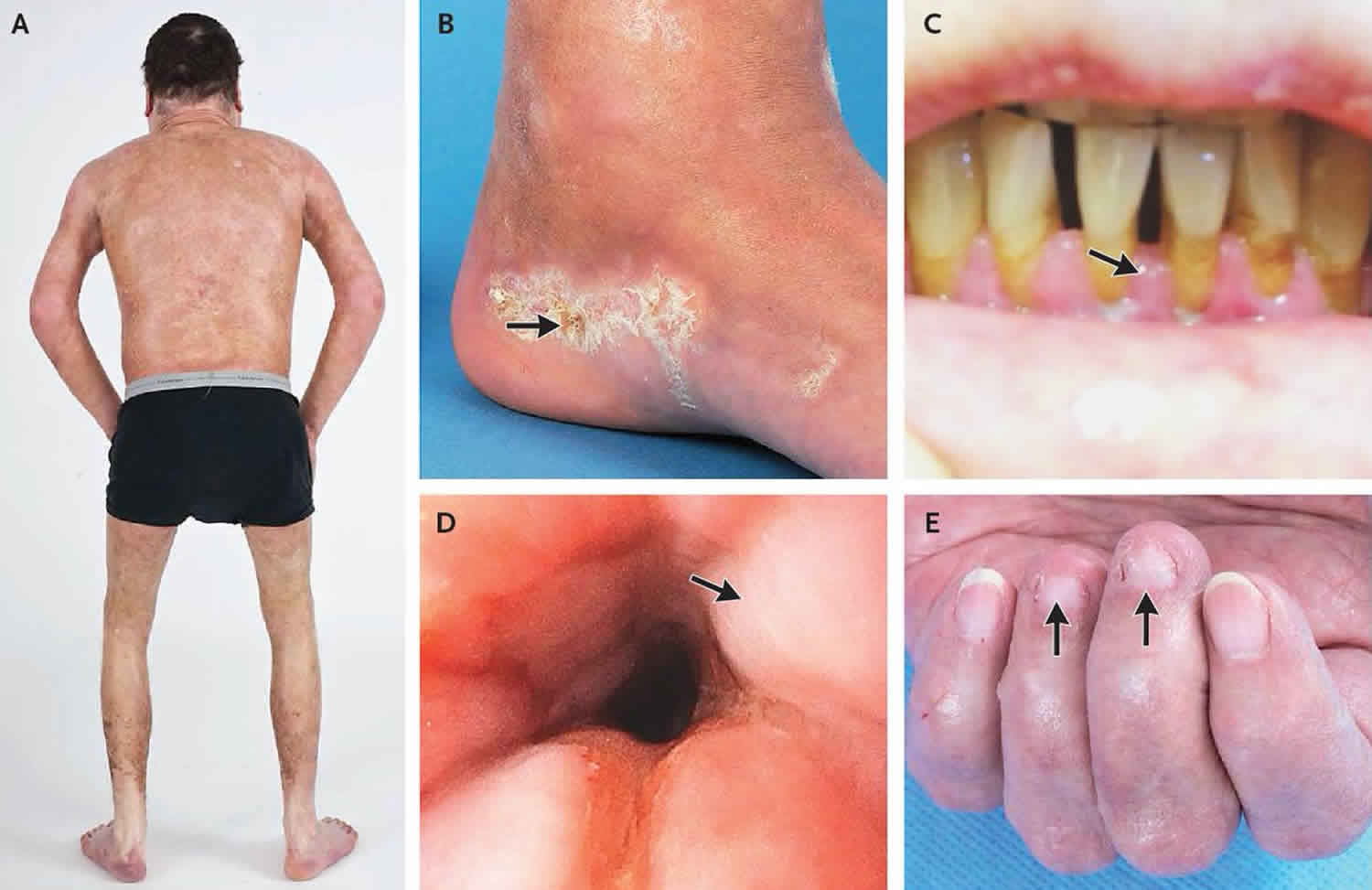
Chronic graft versus host disease
Chronic graft versus host disease starts more than 100 days after your transplant. You are more likely to get it if you have had acute graft versus host disease but it can happen even if you haven’t. It can be mild or severe, and for some people can go on for several months or even years.
It may affect your:
- skin
- gut
- liver
- mouth
- eyes
- lungs
- vagina
- joints
Late acute graft versus host disease and overlap syndrome
There are two other types of graft versus host disease known as:
- late acute graft versus host disease which starts after day 100
- overlap syndrome with features of both acute and chronic graft versus host disease
They are both more likely to happen after mini transplants (reduced intensity conditioning). Nowadays, doctors use mini transplants more often.
Graft versus host disease causes
An acute graft versus host disease starts between 7 to 30 days after either transfusion or transplantation with one of the followings 1:
- Blood product infusion with viable lymphocytes
- Maternal-fetal blood transfusion
- Intrauterine transfusion
- Transfusion of packed red blood cells
- Transfusion of frozen cells
- Transfusion of platelet and frozen plasma
- Transfusion of leukocyte-poor erythrocytes
- Therapeutic whole blood transfusion
- Transplantation of fetal thymus
- Transplantation of fetal liver and bone marrow
Graft-versus-host disease occurs secondary to an organ or tissue transplantation and must fulfill these criteria:
- Histocompatibility differences between the graft (donor) and the host (recipient)
- Presence of immunocompetent T lymphocytes in the graft
- An immunodeficient recipient, whose immune system is not competent enough to mount an effective immune response against the foreign T cells
- Occurring before an arbitrary 100-day period and clinical manifestations may occur after 100-day post-graft
- Signs of tissue damage occur due to high cytokine release (including interleukin-1, tumor-necrosis factor alpha, and gamma interferon) and direct cellular toxicity
Graft versus host disease occurs in stem cell transplantations as bone marrow graft and also in solid organ transplants. Recognition of major histocompatibility antigens (MHC) on immune cells of the recipient is the stimulus that graft competent T cells have for attacking the recipient. Indeed if there is an MHC-mismatch or disparity between donor and receptor instead of an acute transplantation rejection a graft versus host disease occurs.
Graft versus host disease may develop despite good genetic compatibility by molecular techniques due to polymorphisms of cytokines including interleukins and growth factors, the presence of differences between the minor histocompatibility antigens and non-MHC encoded gene diversity. Severe graft versus host disease is now rare due to improving histocompatibility techniques, a better T-cell depletion process, in combination with stem cell enrichment.
How graft versus host disease develops
Graft versus host disease happens because the transplant affects your immune system.
The donor’s bone marrow or stem cells will contain some T cells. T cells are a type of white blood cell that help us fight infections. T cells attack and destroy cells they see as foreign, and potentially harmful such as viruses.
Normally T cells don’t attack our own body cells, because they recognise proteins on the cells called HLA (human leukocyte antigens). We inherit our HLA from our parents. Apart from identical twins, HLA is unique to each person.
Before a bone marrow or stem cell transplant, you and your donor have blood tests to check how closely your HLA matches. This test is called tissue typing. If you and your donor have very similar HLA this lowers the chance of graft versus host disease. The more differences there are between your HLA and your donor’s, the more likely you are to get graft versus host disease.
After a transplant your bone marrow starts making new blood cells from the donor stem cells. These new blood cells have the donor’s HLA pattern. They recognise the HLA pattern on your body cells as different (foreign) and may begin to attack some of them.
The graft versus host disease may affect different areas of your body. Most commonly it affects the skin, digestive system (including the bowel and stomach) or the liver.
About T cells
Before and after your transplant, your doctors will use treatments to reduce the chance of graft versus host disease. These treatments destroy T cells.
T cells are white blood cells that are part of the immune system. They attack cells that are foreign to the body. Graft versus host disease happens when T cells in the donated bone marrow or stem cells (the graft) attack your own body cells (the host).
So reducing the number of T cells in the donor marrow or stem cells (the graft) reduces graft versus host disease.
Sometimes graft versus host disease is a good thing. The T cells in the graft will also attack any remaining cancer cells. This reduces the risk of your disease coming back. This is called the graft versus disease effect. Doctors try to strike a balance between preventing severe graft versus host disease and getting some possible benefits from mild graft versus host disease.
To lower your risk of graft versus host disease you might have treatment:
- before your transplant
- to remove T cells from the bone marrow or stem cells
- after your transplant
Graft versus host disease prevention
Many people who had a transplant will have some graft versus host disease. But, there are some steps you can take to help lower your risk.
1. Take your medicines
Your doctor will give you medicine to help prevent graft versus host disease. Keep taking that medicine as directed, even if you’re feeling healthy. Call your doctor right away if you are unable to take the medicine for any reason.
2. Watch for early warning signs
Tell your doctor if you notice early signs of graft versus host disease. Early treatment of graft versus host disease, infections and other side effects from treatment can make a big difference in your long-term recovery.
3. Protect yourself from the sun
Exposing yourself to the sun’s ultraviolet (UV) rays increases your risk of developing graft versus host disease. To limit your exposure to the sun:
- Avoid the sun as much as possible.
- Wear a hat, sunglasses, long sleeves and pants when you go out.
- Apply SPF 50 or higher sunscreen on any skin that is not covered. You can also wear clothes with SPF. Don’t forget, even on a cool, overcast day the sun is just as harmful as on a hot, bright day.
Even if you’re feeling well, your checkups are important to staying healthy because late complications can happen. Late complications are health problems that can start 100 or more days after transplant. During your checkups, your doctor will:
- Look for signs and symptoms of problems from your treatment, like graft-versus-host disease (graft versus host disease) if you had an allogeneic transplant
- Talk with you about what cancer screenings you may need
- Watch for signs of the disease coming back (relapse)
- Ask about your quality of life, including your emotional and sexual health.
Getting the best donor match
graft versus host disease can develop when the donor and the person receiving donor cells have a different tissue type. So your transplant specialist will make sure your donor is as closely matched to you as possible. This is called tissue typing and helps reduce your risk of graft versus host disease.
Tissue typing
The HLA (human leukocyte antigen) system describes the proteins found on your blood cells. Your doctors aim to find a donor with the closest HLA match possible.
Doctors usually test for 5 pairs of major HLA antigens. This gives a total of 10 antigens. We inherit one half of the pair from each of our parents. When choosing a donor, doctors aim to match 10 out of 10 HLA proteins. But it may be possible to do a transplant if they don’t all match.
Finding a donor
We inherit the proteins from our parents so your best chance of a match is with a relative. You have a 1 in 4 (25%) chance of an exact match if you have a brother or sister. Other members of family can be tested if you don’t have siblings or if they don’t match your tissue type. Parents may be a close enough match.
Your doctor will search for a bone marrow match on a register of the general population if no one in your family is a match. Another possibility is to look at cord blood registries. These contain blood taken from umbilical cords at births, which can be used as a source of stem cells.
Treatment before your transplant
Before your transplant you have a drug to reduce the number of T cells in your donated marrow or stem cells. You usually have a drug called ciclosporin which is also called Deximune, Neoral or Sandimmum.
- You start having it by drip (intravenously) a couple of days before your transplant. Before you go home you start taking it daily as a capsule.
- You should never take it with grapefruit or grapefruit juice because this can change the way the drug works
You usually keep taking ciclosporin for about 6 months after the transplant. As an alternative to ciclosporin, you might take a combination of mycophenolate mofetil (MMF) and tacrolimus.
You might have treatment with other drugs before your transplant, such as:
- alemtuzumab (Campath)
- antithymocytic globulin (ATG)
- newer drugs, including sirolimus (Rapamide)
Removing T cells from the bone marrow or stem cells
Your doctors can remove T cells from your donor’s bone marrow after it has been donated, or during the donation of stem cells. This is called T cell depletion. It isn’t commonly used.
Treatment after transplant
You have treatment with drugs after your transplant to reduce the risk of graft versus host disease.
Methotrexate
Low doses of the chemotherapy drug methotrexate suppresses your immune system. This helps to keep the T cells down and so stops them attacking your body cells.
Cyclophosphamide
You may have a chemotherapy drug called cyclophosphamide after a stem cell transplant. This is more likely after a half matched transplant from a family member, usually a parent or child. This is called a haploidentical transplant. The donor is a 50% match with the person having the transplant.
Before the transplant, you have chemotherapy to lower your immune system. These are usually lower doses of chemotherapy than in a traditional stem cell transplant. This is called reduced intensity conditioning.
A few days after the transplant, you have a high dose of cyclophosphamide. The donor’s immune cells recognise your body cells as foreign, and start to multiply to attack them. The cyclophosphamide kills these rapidly growing immune cells, and so stops them attacking your body cells. This reduces side effects such as graft versus host disease. You may have this treatment as part of a clinical trial.
Graft versus host disease symptoms
There are two types of graft versus host disease: acute and chronic. Symptoms in both acute and chronic graft versus host disease range from mild to severe.
Acute graft versus host disease usually happens within days or as late as 6 months after a transplant. The immune system, skin, liver, and intestines are mainly affected. Common acute symptoms include:
- Abdominal pain or cramps, nausea, vomiting, and diarrhea
- Jaundice (yellow coloring of the skin or eyes) or other liver problems
- Skin rash, itching, redness on areas of the skin
- Increased risk for infections
Chronic graft versus host disease usually starts more than 3 months after a transplant, and can last a lifetime. Chronic symptoms may include:
- Dry eyes, burning sensation, or vision changes
- Dry mouth, white patches inside the mouth, and sensitivity to spicy foods
- Fatigue, muscle weakness, and chronic pain
- Joint pain or stiffness
- Skin rash with raised, discolored areas, as well as skin tightening or thickening
- Shortness of breath due to lung damage
- Vaginal dryness
- Weight loss
- Reduced bile flow from the liver
- Brittle hair and premature graying
- Damage to sweat glands
- Cytopenia (decrease in number of mature blood cells)
- Pericarditis (swelling in the membrane surrounding the heart; causes chest pain)
Not everyone experiences all the warning signs of graft versus host disease, but many transplant recipients experience some of them. Some symptoms might develop into long-term problems. Others are temporary and will go away with treatment. Many of the early warning signs for graft versus host disease could also be caused by infection or another side effect. That’s why it’s important to tell your doctor about any changes in your body that you see or feel.
If you have any signs or symptoms:
- Call your transplant team immediately.
- Give your health care team as many details as you can. Tell them when the symptoms started and what you’re feeling. This can help them figure out the cause and the best way to treat it.
Consider wearing a medical alert bracelet to tell others that you received a blood or marrow transplant. Keep a short treatment summary and your doctor’s phone number in your wallet. Then, in case of an emergency, anyone helping you will have this important medical information.
For parents
If your child had a transplant, look for early warning signs of graft versus host disease every day. If you’re child’s old enough, ask specific questions about how he or she feels. Remind your child to tell you about any changes he or she sees or feels right away.
Graft versus host disease complications
Graft versus host disease is a complication of allogeneic hematopoietic stem cell transplant that can usually have other complications including bronchiolitis obliterans syndrome, interstitial lung disease, obliterative bronchiolitis, organizing pneumonia, and pleuroparenchymal fibroelastosis 2.
Other complications reported include gastrointestinal involvement resulting in fibrosis, motility abnormalities, and malabsorption. Lung problems may cause bronchiectasis. Infection is usual and fatal.
Liver complications include endothelialitis, bile duct destruction, and pericholangitis, but liver biopsy is not done routinely due to associated thrombocytopenia 3.
Graft versus host disease diagnosis
Your symptoms might suggest that you have graft versus host disease but you will still need to have tests to confirm this. Your doctor might take a sample (a biopsy) of the affected area.
You might need to see different specialists for some of these tests. For example, if you have skin graft versus host disease your doctor may refer you to a skin specialist (dermatologist).
Several lab and imaging tests can be done to diagnose and monitor problems caused by graft versus host disease. These may include:
- X-ray abdomen
- CT scan abdomen and CT chest
- Liver function tests
- PET scan
- MRI
- Capsule endoscopy
- Liver biopsy
A biopsy of the skin, mucous membranes in the mouth, may also help to confirm the diagnosis.
Having a biopsy
The doctor removes a small amount of tissue from the affected part of your body. They send the sample to the lab so that a specialist doctor (pathologist) can examine it under a microscope. It may take a while to get the results of your biopsy.
The biopsy you have depends on which part of your body is involved. For example, you might need a skin biopsy or a liver biopsy.
Skin biopsy
The doctor gives you a local anesthetic injection to numb your skin. Then they remove a small amount of the affected skin and put a dressing over the biopsy site.
Liver biopsy
You usually have an ultrasound or CT scan at the same time as a liver biopsy. The doctor uses the images from the CT or ultrasound scan to guide the biopsy needle into the right place in the liver.
After giving you some local anaesthetic, the doctor puts a needle through your skin and into the affected part of the liver. The doctor takes tissue samples.
After a liver biopsy, you have to stay in hospital for a few hours or possibly overnight. The liver has a very rich blood supply and there is a risk of bleeding afterwards, so your nurse will monitor you closely.
Endoscopy
You might need an endoscopy if your doctor suspects you have graft versus host disease in your digestive system. The doctor can take a biopsy during the endoscopy.
For this test the doctor uses a tube to look at the inside of your food pipe (oesophagus) and stomach.
Or you might need a tube into your back passage to look at your bowel (sigmoidoscopy or colonoscopy).
X-rays and scans
You may need an x-ray or CT scan of your lungs. This is painless and you don’t need any preparation for it.
Or you might have an ultrasound scan of your liver to see if there are any signs of graft versus host disease.
Lung function tests
If you have symptoms of graft versus host disease in the lungs, you have tests to check how well your lungs are working.
These tests check how much air you can breathe in and out, and how quickly.
Graft versus host disease treatment
After a transplant, the recipient usually takes medicines, such as prednisone (a steroid), which suppress the immune system. Steroids are a kind of medicine called an immunosuppressant. These medicines weaken the new immune system so your new cells don’t attack your body. This helps reduce the chances (or severity) of graft versus host disease. Starting graft versus host disease treatment as early as possible can lead to better results.
You’ll continue taking the medicines until your health doctor thinks the risk for graft versus host disease is low. Many of these medicines have side effects, including kidney and liver damage. You’ll have regular tests to watch for these problems.
Because your new immune system is weaker, you may be limited in what you can do, even if your transplant was more than 1 year ago. For example, you may need to avoid yard work and large crowds. Ask your doctor what you may need to avoid.
Follow your doctor’s advice carefully. Don’t stop taking your graft versus host disease medicine without letting your doctor know. If you can’t take them for any reason, tell your doctor right away. If you can’t swallow your medicines, you may need to get them through an intravenous (IV) line (directly into your bloodstream) temporarily.
Graft versus host disease treatment works well for many patients. You may need to be treated for weeks or months because it can take time to find the best type and dose of medicine with the fewest side effects for you.
Acute graft versus host disease treatment
Treatment is based on drugs that reduce your body’s immune response and reduce the number of T cells. The most common treatment is corticosteroids (usually prednisolone).
Doctors sometimes use a drug called ciclosporin with the steroids. Ciclosporin is also called Deximune, Neoral or Sandimmum. You take it as a tablet.
Sometimes steroids and ciclosporin do not control graft versus host disease. In this case, your doctor will use other treatments, which may include:
- infliximab (Remicade)
- etanercept
- sirolimus
- mycophenolate mofetil (MMF)
- a type of light therapy called extracorporeal photopheresis (ECP)
Prochymal is a new drug approved for pediatric patients with acute graft versus host disease refractory to conventional treatment with steroids 4. In a trial, patients received eight biweekly IV Infusions of 2 × 10(6) of human mesenchymal stem cells (hMSCs)/kg for four weeks, with an additional four weekly injections after day twenty-eight for those patients who achieved either an undesired response. Seventy-five patients were treated in this study. Complete and partial response at day twenty-eight was 66.7% for agraft versus host disease grade B, 76.2% for grade C, and 53.3% for grade D. Overall response for individual organs at day twenty-eight was 75.6% for skin, and 44.4% for liver and 58.5% for the gastrointestinal system. The overall reaction at day twenty-eight for patients treated for severe agraft versus host disease was 61.3% and correlated with statistically significant survival at day +100 after Prochymal infusion. The drug infusions were often well tolerated 5. Despite the favorable risk/benefit profile and safety of this cell product that has been investigated in various phase I-II studies, several larger and prospective randomized trials are needed to confirm its efficacy in severe refractory acute graft versus host disease and to identify the optimal schedule of administration in terms of cell dose, infusion timing, and pharmacological synergism 6.
Acute graft versus host disease skin treatment
The most common treatment for skin graft versus host disease is steroids. Your treatment depends on the grade of graft versus host disease you have.
- Mild graft versus host disease (grade 1): This may get better without any treatment but you will have to keep your skin well moisturized. Or you might have treatment which involves applying a steroid cream to the affected areas.
- Moderate graft versus host disease (grade 2): You will probably have either a steroid cream or a course of steroid tablets.
- Severe graft versus host disease (grade 3 and 4): You will need to have steroids through a drip (intravenously). You might also need other drugs for graft versus host disease to reduce your immune reaction. Your doctor may refer you to a skin consultant (dermatologist) for specialist advice on how to treat and manage your skin. They may prescribe special moisturising creams and bath oils.
What you can do to help yourself
There are some things you can do to help keep your skin more comfortable. These include:
- wear cotton clothes
- try not to get too hot or too cold
- use unperfumed soaps
- use warm, not hot, water for washing
- let your skin dry in the air, or gently pat it dry – don’t rub it
- keep your skin well moisturized with unperfumed creams or lotions
- cover up your skin in the sun
Acute gut graft versus host disease treatment
Graft versus host disease of the gut might cause sickness or diarrhea. To control your symptoms you might need:
- fluids by drip into a vein, to prevent and treat dehydration
- painkillers if you have any abdominal cramps
- anti sickness drugs if you feel sick
- drugs to control your diarrhea
- feeding though a tube into your stomach or directly into your bloodstream, if you can’t eat and are losing weight
Once you are able to eat, you will start with a diet that is low in fiber, fat and lactose. You should also avoid spicy and acidic foods as they can irritate the gut.
Treatment of the graft versus host disease itself is based on drugs that reduce your body’s immune response and lower the number of T cells.
The main treatment is steroids, which generally work well. Your doctor might also treat you with other drugs to suppress your immune system and so reduce the graft versus host disease. Light therapy with extracorporeal photophoresis can also help.
What you can do to help yourself
There are some things you can do to help with sickness and diarrhea. These include:
- drinking plenty of fluids – tell your doctor or nurse if you feel sick and find it difficult to drink
- taking anti sickness drugs
- taking the painkillers your nurse gives you
- keeping the area around your back passage clean and dry if you have diarrhea – you may need a barrier cream to try to prevent the skin getting sore and breaking down.
Acute liver graft versus host disease treatment
You might not have symptoms of liver graft versus host disease. Your doctors might have picked it up from your regular liver function tests or LFTs (a type of blood test).
Graft versus host disease of the liver is graded according to the amount of bilirubin in your blood. Bilirubin is a waste product made when red blood cells break down. A raised bilirubin level in the blood can show that the liver isn’t working properly. The more bilirubin you have, the higher your grade of graft versus host disease will be.
Doctors treat liver graft versus host disease with steroids. They might also give you other drugs to reduce the number of T cells your new bone marrow is making.
If you have symptoms of liver graft versus host disease you might have:
- drugs to relieve itchy, jaundiced skin
- blood transfusions if you have a low red blood cell count (anemia), or a low platelet count
- painkillers
Your doctor will continue to do regular liver function tests to check how the treatment is working. You might need to cut down or stop taking any medicines that are known to affect the liver. Be sure to speak to your doctor about this first though.
Your doctor may also refer you to a consultant specializing in gut and liver problems (a gastroenterologist).
What you can do to help yourself
There are things you can do to help with liver graft versus host disease symptoms:
- don’t get too cold or too hot – this can make itching worse
- wear cotton instead of man made fabrics like nylon
- take the drugs your doctor or nurse gives you to help with any itching
- take painkillers regularly, as prescribed by your doctor – they will work better than if you take them now and again.
Chronic graft versus host disease treatment
Your treatment depends on how bad your chronic graft versus host disease is and which parts of your body are affected.
Your doctor may grade chronic graft versus host disease as either mild, moderate or severe.
General treatments for chronic graft versus host disease
Treatment for chronic graft versus host disease usually includes steroids. You might also have ciclosporin (which is known as Deximune, Neoral or Sandimmum) to reduce your immune response.
If these drugs do not control the graft versus host disease, your doctor may suggest other treatments to damp down your immune system. Some of these treatments depend on which part of your body is affected.
Treatments include:
- tacrolimus
- sirolimus
- pentostatin
- rituximab
- imatinib
- mycophenolate mofetil (MMF)
- a special type of light therapy called extracorporeal photophoreses (ECP)
The risk of infections
Your treatment for chronic graft versus host disease will make you more at risk of picking up infections. So you will have antibiotics to help protect you. The risk can be serious, particularly if your immune system is very weak.
Talk to your doctor or specialist nurse about what precautions you might need to take to avoid infection. In general you should avoid crowded places and people with infections.
You must never have live vaccinations although most vaccines these days aren’t live. But check with your doctor if you are unsure. A year after having a stem cell transplant your doctor may advise you to have the flu vaccine to help protect you.
Treating chronic skin graft versus host disease
The treatment for chronic graft versus host disease of the skin includes keeping your skin clean and moisturizing regularly. You should use unperfumed soaps and moisturizing creams.
Your doctor prescribes steroid creams or a cream called tacrolimus if the skin problems are just in small areas. Your doctor may refer you to another doctor who specializes in skin problems (a dermatologist).
Chronic graft versus host disease can last for many months, sometimes years, so you will need to carry on with the treatments for a long time. As with other chronic skin conditions this can take up a lot of time. You might need help from a partner or carer to manage your skin properly.
More severe skin graft versus host disease can be treated with a type of light therapy called ECP (extracorporeal photophoreses). Newer treatments being tried include halofuginone, etanercept and hydroxychloroquine.
To help yourself with symptoms:
- wear cotton clothes
- try not to get too hot or too cold
- when you are washing don’t have the water too hot
- let your skin dry in the air or gently pat it dry instead of rubbing it
- protect your skin from the sun by covering up, and using at least a factor 15 sunscreen
- use lots of moisturizing creams to relieve itchy, dry skin – try putting on lots of cream at night and wear old nightclothes and socks
Treating chronic gut graft versus host disease
Chronic graft versus host disease might affect your gut anywhere from your mouth to your bowel. Again it can last for a long time, so you might need to carry on with treatments long term.
You will need to clean your mouth regularly, especially if it is dry and sore. Your doctors and nurses will give you mouthwashes, and other medicines if your mouth gets infected. Artificial saliva may help with dryness.
Having diarrhea can make you dehydrated so you might need to have a drip with fluids. Your doctor might suggest feeding you through a tube if you can’t eat for whatever reason. The tube enters either through your nose into your stomach, or directly into your bloodstream through a central line, PICC line or portacath.
Diarrhea can make the skin get sore and break down around your anus. You will need to wash the area regularly to keep it clean. You may also need a barrier cream to stop the skin breaking down. Your doctor may give you medicines to help control the diarrhea.
Your nurse will give you anti sickness drugs if you feel sick. You might be referred to a specialist (a gastroenterologist) if your sickness doesn’t improve.
Treating chronic lung graft versus host disease
Chronic graft versus host disease can cause inflammation of the small air tubes in the lungs. This can cause shortness of breath, wheezing and a persistent cough. But it may only be a problem if you have a chest infection. You will probably need to take steroids long term, and antibiotics to stop you getting infections. You might need oxygen therapy if your symptoms are bad.
Your doctor may refer you to a specialist in lung diseases.
Your doctor may use combinations of treatments to damp down your immune system, such as mycophenolate mofetil (MMF), imatinib and perhaps extracorporeal photopheresis (ECP).
Treating chronic eye graft versus host disease
Chronic graft versus host disease of the eye can make your eyes sore and dry.
You can have artificial tears and steroid eyedrops to help keep your eyes moist. These will help to protect the front of your eye (the cornea) from getting scratched. Sometimes using cyclosporin A ointment in the eye can help. Other treatments include tacrolimus capsules or ointment.
You might need to see a specialist eye doctor (ophthalmologist). They might be able to arrange for you to have eyedrops made from the clear part of your own blood if artificial tears do not help. These are called autologous serum eyedrops and are produced by the National Blood and Transplant Service.
Treating chronic vaginal graft versus host disease
The lining of the vagina may become inflamed or narrowed. This can make it uncomfortable to have sex.
Treatment with steroid creams into the vagina can help to stop it getting worse and can clear it for some women.
Late complications treatment
If you have late complications after transplant, there are treatments available. When problems are found early, they can be treated better. Sometimes, you may need to try 2 or 3 different treatments before finding a medicine or combination of medicines that work best for you. Talk to your doctor to learn more about the best treatment for you.
Here are some tips to manage symptoms of common late complications:
Eyes
- Dryness, itching, irritation: Avoid eye strain and rest your eyes. Use preservative-free artificial tears, a humidifier or warm compresses. For more difficult symptoms, ask your doctor about medicines for your eyes or “punctal plugs,” which help your tears last longer.
- Severely dry eyes: Ask your doctor about specially made serum eye drops or bandage contact lenses if other treatments haven’t helped.
- Cataracts: For early or mild cataracts, try new glasses or better lighting. If your sight gets much worse, ask your doctor about cataract surgery.
Heart and blood vessels
- High cholesterol or high blood pressure: Eat a well-balanced diet with less fat and follow an exercise program. Take any medicines as prescribed by your doctor.
Mouth
- Pain and dryness: Avoid eating very spicy and acidic foods. Ask your doctor about special rinses and lubricants, which may relieve mouth sores.
Skin, bones and joints
- Rashes: When going out into the sun, wear hats and long sleeves to protect your skin. Check with your doctor before using any new skin creams or lotions.
- Scleroderma (hard, tight skin): Scleroderma affects the skin and joints, making them less flexible. Medicines, exercise and physical therapy may help increase blood flow, strength and flexibility.
- Avascular necrosis (also known as osteonecrosis): With avascular necrosis, a bone in a joint doesn’t have enough blood flow. This causes the bone to break down and you may feel joint pain. Your doctors may treat this with medicine, crutches or braces, and range of motion or stretching exercises. In more severe cases, surgery can repair or replace the joint.
- Osteopenia: Ask your doctor if you should be taking calcium and vitamin D supplements or have a test for weak bones. Weight bearing exercise, such as walking, can build bone strength.
Screening for cancer
A new cancer could be a result of your treatment. During your regular checkups, talk to your doctor about your risk for new cancers. Be an advocate for your health by:
- Following cancer prevention recommendations from the American Institute for Cancer Research
- Asking your doctor if you need cancer screenings (like a mammogram)
When a new cancer is caught early, there may be more treatment options available and those treatments can be more effective.
Graft versus host disease survival rate
Outlook depends on the severity of graft versus host disease. People who receive closely matched bone marrow tissue and cells usually do better.
Some cases of graft versus host disease can damage the liver, lungs, digestive tract, or other body organs. There is also a risk for severe infections.
Many cases of acute or chronic graft versus host disease can be treated successfully. But this doesn’t guarantee that the transplant itself will succeed in treating the original disease.
Graft versus host disease prognosis
The prognosis of acute graft versus host disease is poor. Once the disease starts, it leads to a fatal outcome. Very early suspicion of acute graft versus host disease and aggressive therapy with immunosuppressive along with specific monoclonal antibodies can potentially achieve a better result.
Chronic graft versus host disease may evolve:
- Directly from acute graft versus host disease, which is known as progressive (has a grim prognosis)
- After a period of resolution, which is known as interrupted (has an intermediate prognosis)
- De novo in a patient with no history of acute graft versus host disease (has a good prognosis).
- Sunul H, Erguven N. Transfusion-associated graft-versus-host disease. Transfus. Apher. Sci. 2013 Oct;49(2):331-3
- Bergeron A, Cheng GS. Bronchiolitis Obliterans Syndrome and Other Late Pulmonary Complications After Allogeneic Hematopoietic Stem Cell Transplantation. Clin. Chest Med. 2017 Dec;38(4):607-621
- Ferrara JL, Levine JE, Reddy P, Holler E. Graft-versus-host disease. Lancet. 2009 May 02;373(9674):1550-61
- Justiz Vaillant AA, Gossman WG. Graft Versus Host Disease. [Updated 2019 May 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538235
- Kurtzberg J, Prockop S, Teira P, Bittencourt H, Lewis V, Chan KW, Horn B, Yu L, Talano JA, Nemecek E, Mills CR, Chaudhury S. Allogeneic human mesenchymal stem cell therapy (remestemcel-L, Prochymal) as a rescue agent for severe refractory acute graft-versus-host disease in pediatric patients. Biol. Blood Marrow Transplant. 2014 Feb;20(2):229-35
- Locatelli F, Algeri M, Trevisan V, Bertaina A. Remestemcel-L for the treatment of graft versus host disease. Expert Rev Clin Immunol. 2017 Jan;13(1):43-56.