What is hypereosinophilic syndrome
Hypereosinophilic syndrome refers to a group of rare blood disorders characterized by persistent peripheral blood eosinophilia of 1.5 ×109/L (1,500 eosinophils/μL) or higher with evidence of end organ involvement attributable to the eosinophilia and not otherwise explained in the clinical setting 1. In 1975, Chusid et al 2 defined the three features required for a diagnosis of hypereosinophilic syndrome:
- A sustained absolute eosinophil count greater than >1500/µL, which persists for longer than 6 months
- No evidence of parasites, allergy or other known causes of an elevated eosinophil count.
- Signs and symptoms of organ involvement.
Most people have less than 500 eosinophils/microliter (500 eosinophils/μL) in their blood. People with hypereosinophilic syndrome usually have more than 1,500 eosinophils/microliter (1.5 ×109/L) in their blood for 6 months or more and the cause cannot be identified. These eosinophils make their way into various tissues, causing inflammation and eventually organ dysfunction.
Hypereosinophilic syndrome signs and symptoms vary significantly based on which parts of the body are affected. Although any organ system can be involved in hypereosinophilic syndrome, the skin, lungs, digestive tract, heart, blood and central nervous system (brain and spinal cord) are the most commonly affected. Hypereosinophilic syndrome was originally thought to be “idiopathic” or of unknown cause. However, recent advances in diagnostic testing have allowed a cause to be identified in approximately a quarter of cases (e.g., allergic, rheumatologic, infectious, and neoplastic disorders). Moreover, the cause of the eosinophilia in hypereosinophilic syndromes can be primary (myeloid), secondary (lymphocyte-driven), or unknown. Some varieties of hypereosinophilic syndrome tend to run in families. Other types have been associated with certain types of cancers, infections or other health problems.
Hypereosinophilic syndrome can affect anyone. But it occurs more often in men (90%), usually between the ages of 20 and 50.
Hypereosinophilic syndrome usually presents with fever, weight loss, fatigue, and rash. A rash is present in over 50% of patients, but is non-specific in appearance. Most commonly, red swollen itchy nodules (lumps) have been described. It can also resemble urticaria (hives). An enlarged liver and spleen is often present indicating liver and spleen involvement. The lungs, kidneys, heart and nervous system can be affected.
Symptoms of hypereosinophilic syndrome are also common in many other medical problems, making an initial diagnosis more difficult. Some patients have an underlying blood disorder present, most commonly a form of leukemia. Leukemia may also be diagnosed up to 9-12 years after the initial diagnosis of hypereosinophilic syndrome.
Untreated, hypereosinophilic syndrome can become life-threatening. Hypereosinophilic syndrome treatment varies based on the severity of the condition and whether or not an underlying cause has been identified but generally includes imatinib or corticosteroids as an initial treatment 3. Approximately 70% of patients respond to high dose oral corticosteroid therapy with oral prednisone, with the eosinophilia returning to normal levels. Although corticosteroids remain the first-line therapy for most forms of hypereosinophilic syndromes, the availability of an increasing number of novel therapeutic agents, including tyrosine kinase inhibitors and monoclonal antibodies, has necessarily altered the approach to treatment of hypereosinophilic syndromes.
The overall 5-year survival for patients with hypereosinophilic syndrome is 80% and the cause of death is usually heart failure.
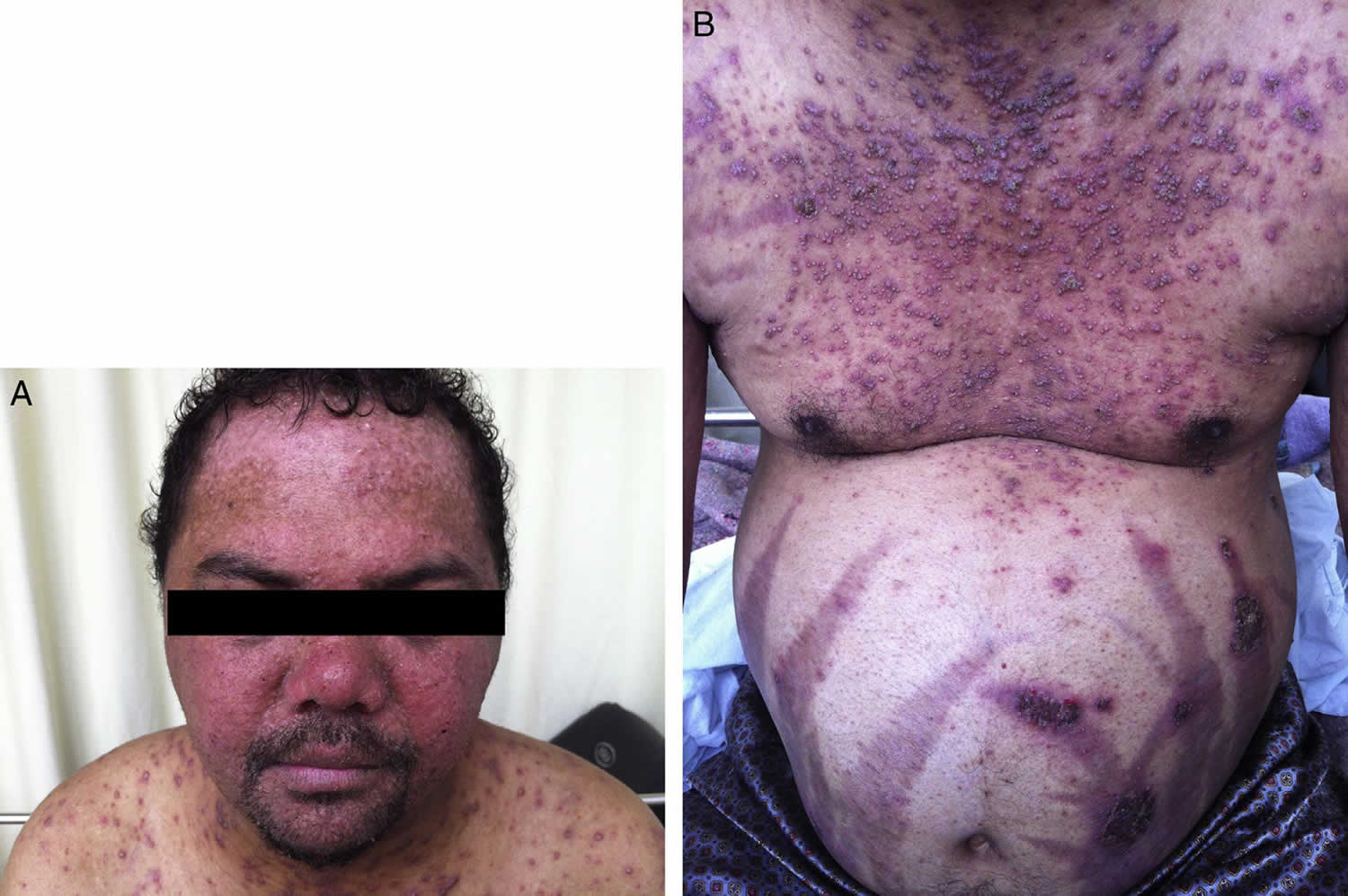
Figure 1. Hypereosinophilic syndrome skin
Footnote: A 30-year-old male patient presented to the emergency department with dyspnea, fever and productive cough for three days. He had been taking 20 mg of prednisone for 20 years. On this occasion, the patient was treated for streptococcal glomerulonephritis. After discharge, he did not return and was lost to follow-up. The patient also had pruritic skin lesions since ten years of age, which used to erupt, vanish and reappear spontaneously in two-week intervals. After prednisone was started, the frequency of the lesions was related to its intake, as the frequency of lesion reappearance was much higher without prednisone.
[Source 4 ]Hypereosinophilic syndrome causes
The cause of hypereosinophilic syndrome is not known. Hypereosinophilia is associated with a variety of conditions, including allergic, infectious, and neoplastic disorders. Causes of hypereosinophilia may be classified as familial or acquired 5. Familial hypereosinophilia is an autosomal dominant disorder with a stable eosinophil count and a benign clinical course. Acquired hypereosinophilia is further divided into secondary, clonal, and idiopathic eosinophilia 6.
Idiopathic eosinophilia
Idiopathic eosinophilia is a diagnosis of exclusion when secondary and clonal causes of eosinophilia are excluded. Hypereosinophilic syndrome is a subset of idiopathic eosinophilia characterized by persistent eosinophilia (absolute eosinophil count >1500/µL) of longer than 6 months duration associated with organ damage. However, long-term follow-up and X-linked clonality studies indicate that at least some patients with hypereosinophilic syndrome have an underlying clonal myeloid malignancy or a clonal or phenotypically abnormal T-cell population, suggesting a true secondary process.
The literature now favors the view that cases of idiopathic hypereosinophilic syndrome with FIP1L1 indeed represent chronic eosinophilic leukemia, because thypereosinophilic syndromee patients have a molecular genetic abnormality, specifically an FIP1L1–PDGFRA fusion gene 7. In addition, there are documented cases of acute transformation to either acute myeloid leukemia (AML) or granulocytic sarcoma in some cases of hypereosinophilic syndrome after an interval as long as 24 years. In such cases, a diagnosis of chronic eosinophilic leukemia is made in retrospect when acute transformation provides indirect evidence that the condition was likely to have been a clonal, neoplastic, myeloproliferative disorder from the beginning.
In addition, some patients with hypereosinophilic syndrome present with features typical of myeloproliferative disorders, such as hepatosplenomegaly, the presence of leukocyte precursors in the peripheral blood, increased alkaline phosphatase level, chromosomal abnormalities, and reticulin fibrosis. Cytogenetic studies in such cases may be normal, but molecular genetic studies may show aberrations.
The best-described aberration is the interstitial deletion on chromosome 4q12, resulting in fusion of the 5’ portion of the FIP1L1 gene to the 3’ portion of the PDGFRA gene. This fusion gene encodes for the FIP1L1–PDGFR alpha protein, the constitutively activated tyrosine kinase activity that induces eosinophilia. The prevalence of such a mutation is 0.4% in unselected cases of eosinophilia, but it can be as high as 12–88% in cohorts that meet the World Health Organization (WHO) criteria for idiopathic hypereosinophilic syndrome, particularly those with features of myeloproliferative disorder (increased levels of tryptase and mast cells in the bone marrow).
Patients with hypereosinophilic syndrome with the PDGFRA mutation have a very high incidence of cardiac involvement and carry a poor prognosis without therapy. Fortunately, the results of imatinib therapy in such cases of hypereosinophilic syndrome are very encouraging.
The other subset of idiopathic eosinophilia, hypereosinophilic syndrome with clonal or immunophenotypically aberrant T-cells, is associated with increased secretion of IL-5 and cutaneous manifestations. Simon et al reported immunophenotypic abnormality in 16 of 60 patients with hypereosinophilic syndrome 8. Moreover, nine patients had CD3+CD4+CD8- T cells, three had CD3+CD4-CD8+ cells, three had CD3+CD4-CD8- cells, and two had CD3-CD4+ cells (one patient had two distinct populations). Progression to T-cell lymphoma was observed in this subset of patients with hypereosinophilic syndrome, particularly those with the CD3-CD4+ phenotypes 8.
Secondary eosinophilia
Secondary eosinophilia is a cytokine-derived (interleukin-5 [IL-5]) reactive phenomenon. Worldwide, parasitic diseases are the most common cause, whereas in developed countries, allergic diseases are the most common cause 9. Other causes include the following:
- Malignancies – Metastatic cancer, T-cell lymphoma 10, colon cancer
- Pulmonary eosinophilia – Loffler syndrome 11, Churg-Strauss syndrome, allergic bronchopulmonary aspergillosis
- Connective tissue disorders – Scleroderma, polyarteritis nodosa
- Skin diseases – Dermatitis herpetiformis
- Inflammatory bowel disease
- Sarcoidosis
- Addison disease
Clonal eosinophilia
Clonal eosinophilia is diagnosed by bone marrow histology, cytogenetics, and molecular genetics. Causes include the following:
- Acute leukemia – Pre-B acute lymphoblastic leukemia (ALL), acute myeloid leukemia M4 with bone marrow eosinophilia (AML-M4Eo)
- Chronic myeloid disorders
Molecularly defined disorders include the following:
- BCR-ABL chronic myeloid leukemia
- PDGFRA (platelet-derived growth factor receptor, alpha polypeptide)–rearranged eosinophilia – Systemic mastocytosis–chronic eosinophilic leukemia (SM-CEL)
- PDGFRβ-rearranged eosinophilia
- KIT-mutated systemic mastocytosis
Clinicopathologically assigned disorders include the following:
- Myelodysplastic syndrome
- Myeloproliferative disorders – classic myeloproliferative disorder (polycythemia) and atypical myeloproliferative disorder (chronic eosinophilic leukemia, systemic mastocytosis, chronic myelomonocytic leukemia)
Chronic eosinophilic leukemia
Chronic eosinophilic leukemia is caused by autonomous proliferation of clonal eosinophilic precursors. Simplified criteria for the diagnosis of chronic eosinophilic leukemia include the following:
- Eosinophil count of at least 1500/µL
- Peripheral blood blast count of >2% and a bone marrow blast cell count that is >5% but < 19% of all nucleated cells
- Criteria for atypical chronic myelogenous leukemia (CML), chronic myelomonocytic leukemia, and chronic granulocytic leukemia (BCR-ABL–positive CML) are not met
- Myeloid cells are demonstrated to be clonal (eg, by detection of clonal cytogenetic abnormality or by demonstration of a very skewed expression of X chromosome genes)
Some of the cytogenetic abnormalities that have been described in chronic eosinophilic leukemia include t(5:12) and t(8:13), and molecular genetic abnormalities include the FIP1L1-PDGFRA fusion gene and ETV6-PDGFRβ.
Hypereosinophilic syndrome symptoms
The symptoms of hypereosinophilic syndrome may vary widely, depending on the part of the body that is affected. Symptoms may include cough, fever, fatigue, shortness of breath and wheezing. The symptoms of hypereosinophilic syndrome are also common in many other medical problems, including autoimmune diseases, allergic disease, cancer, and drug reactions, making hypereosinophilic syndrome more difficult to diagnose.
Hypereosinophilic syndrome symptoms include:
- Skin rashes such as urticaria or angioedema
- Dizziness
- Memory loss or confusion
- Cough
- Shortness of breath
- Fatigue
- Fever
- Mouth sores
Hypereosinophilic syndrome diagnosis
Since many different problems can cause high numbers of eosinophils in the blood, higher than normal blood eosinophil number alone does not mean an individual has, or will develop, hypereosinophilic syndrome. When trying to determine whether you have hypereosinophilic syndrome, your doctor is likely to ask about your travel history and any medications you’re taking, to help rule out these other causes.
Criteria has been developed that must be fulfilled for an individual to be diagnosed with hypereosinophilic syndrome.
- Peripheral blood eosinophilia (high numbers of eosinophils in the blood) more than 1500 eosinophils, for at least six months duration.
- End-organ (heart, lungs, gastrointestinal tract, brain, skin, etc) involvement with eosinophil tissue infiltration (invasion) and injury.
- Exclusion of known other causes for the eosinophilia such as parasitic infections and certain bone marrow/blood diseases.
Tests are needed to diagnose hypereosinophilic syndrome and include a complete blood cell count, including eosinophil count, blood samples for liver and kidney function, and blood tests for vitamin B12 and tryptase.
Depending on symptoms and test results, other studies may be performed. For instance, ultrasound (echocardiography) is used to look at the function of the heart. A chest x-ray may be done to examine the lungs. A bone marrow biopsy is recommended in patients suspected of having hypereosinophilic syndrome. It commonly reveals high number of eosinophils and some other abnormalities, suggestive of an innate bone marrow/blood disease of eosinophils. Therefore, hypereosinophilic syndrome is classified as hematologic neoplasm (disease of the blood and bone marrow) and is part of the larger group of Myeloproliferative Neoplasms.
Closely related disease to hypereosinophilic syndrome is chronic eosinophilic leukemia (CEL). Major difference, in simple terms, is that in chronic eosinophilic leukemia all eosinophils found in the bone marrow and blood are proven to be identical (also called “clonal”, meaning that all originate from the same, one, abnormal eosinophil).
Hypereosinophilic syndrome may be diagnosed and monitored by a team of specialists, such as allergist/immunologist, hematologist, and/or cardiologist.
Laboratory tests
Your doctor may also need information from some of the following lab tests:
- Blood tests, to detect autoimmune conditions, parasitic infections, or problems with your liver or kidneys
- Allergy tests, to detect environmental or food allergies
- Stool tests, to detect parasitic infections such as hookworm
- Genetic test, to check for a gene mutation that can cause hypereosinophilic syndrome
Imaging tests
Imaging tests may include:
- X-rays, to check the condition of your lungs
- CT scan, to detect problems in the chest, abdomen and pelvis
- Echocardiogram or MRI, to assess heart function
Hypereosinophilic syndrome treatment
Treatment goals include decreasing blood eosinophil numbers, preventing organ damage, and slowing disease progression. Treatments vary based on organs involved and disease verity, as well as on the presence of other medical problems a patient may have. Therapy for hypereosinophilic syndrome requires careful discussion with your health care providers regarding the risks and benefits of the treatment for your specific hypereosinophilic syndrome- related organ involvement.
Hypereosinophilic syndrome treatment may include glucocorticosteroids (i.e., prednisone) and chemotherapy medicines such as chlorambucil, hydroxyurea, and vincristine. Frequent injections of interferon-alpha may also be prescribed.
Improved treatment options for hypereosinophilic syndrome are an area of ongoing research, including the use of tyrosine kinase inhibitors (i.e., Gleevec, Dasatinib, and Nilotinib) and anti-interleukin-5 (IL-5) monoclonal antibodies (mepolizumab and reslizumab).
Systemic steroids are often needed to treat hypereosinophilic syndrome with organ involvement or with systemic symptoms, like a severe rash, fluid retention, and similar. Steroids are medications that fight (suppress) many types of inflammation. They are not specific for suppressing eosinophils, although eosinophils are particularly sensitive to them. Systemic steroids, those that are absorbed into the bloodstream (oral or IV), are very effective for treating a number of eosinophilic disorders. Steroids are very effective for controlling eosinophil numbers in blood and most hypereosinophilic syndrome patients can be maintained on oral steroid medication (called prednisone) for a long period of time with good control of the disease. However, the blood eosinophils and disease symptoms generally return once steroids have been stopped. Long-term steroid use (especially when used in high doses) has, unfortunately, been associated with certain side-effects. Serious side effects can include osteoporosis (brittle bones from bone loss), infections, adrenal insufficiency (body becomes unable to properly respond to illness or stress), avascular necrosis (collapse of the bones in a joint, usually the hip), and stunted growth. Common side effects may include fluid retention (swelling), increased appetite, “moon-face”, and irritability.
Interferon alpha (IFNa) is used for a variety of diseases including infections (like hepatitis) and malignancies (like certain types of leukemia). Interferon alpha (IFNa) has been shown to be effective in hypereosinophilic syndrome by suppressing the symptoms related to the disease. Toxicity, however, is a major obstacle to the use of this therapy. Interferon alpha (IFNa) is commonly injected into the fatty tissue under the skin 3-5 times a week. Upon the initiation of therapy most patients experience influenza-like symptoms such as fever, chills, muscle aches, headaches, and joint pain. Other side effects of interferon alpha (IFNa) are low blood counts and elevated liver enzymes that require careful monitoring. These side effects usually lessen over time, but other toxicities can manifest themselves in various forms after long-term therapy. Overall experience with interferon alpha (IFNa) in myeloproliferative neoplasms is that about 25-30% of patients require discontinuation of therapy due to side effects. New long-acting forms of IFNa (pegylated interferons) have been developed over the last few years and are now approved as a therapy for hepatitis. These medications are administered only once a week and may, therefore, be better tolerated.
Cyclosporine is a potent medication that suppresses the immune system and it is used primarily to prevent organ rejection in people who have had organ transplants. In some patients with hypereosinophilic syndrome there might be evidence that the immune cells have a role in supporting the diseases existence (so-called T cells) and cyclosporine may have a role as therapy in such cases.
Anti-neoplastic agents (chemotherapy) provide an alternative approach to therapy of advanced cases of hypereosinophilic syndrome. These are chemotherapeutic agents that may control the disease. They are used to treat many malignancies and are not specific for eosinophilic disorders. They are potent medications that kill cells that grow the fastest (eosinophils in hypereosinophilic syndrome) but may potentially have harmful side effects and are reserved only for more severe cases. Careful monitoring while taking these medications is essential. Chemotherapeutic agents that have been used in hypereosinophilic syndrome include: Hydroxyurea, Methotrexate, Etoposide, Cyclophosphamide, Vincristine, and Cladribine.
Gleevec (Imatinib Mesylate) is a tyrosine kinase inhibitor. As a result of cell growth research, scientists have been able to develop a group of therapeutic agents known as tyrosine kinase inhibitors (TKI). Tyrosine kinases are enzymes in the cells with a variety of functions. By blocking the ability of tyrosine kinases to function, tyrosine kinase inhibitor provides a valuable tool for controlling malignant cell growth. Several years ago a discovery was made in some patients with hypereosinophilic syndrome of a genetic abnormality involving tyrosine kinase called PDGFRα (platelet-derived growth factor receptor, alpha polypeptide). In these cases, it seems that PDGFRα abnormality is responsible for disease existence. Gleevec is a tyrosine kinase inhibitor that inhibits PDGFRα (platelet-derived growth factor receptor, alpha polypeptide) and may eliminate the disease in hypereosinophilic syndrome patients with PDGFRα abnormality. Genetic testing for PDGFRα abnormality is usually part of the bone marrow evaluation and can help determine if Gleevec is best first therapy. Not all patients with hypereosinophilic syndrome will respond to Gleevec as about 10-20% of patients may have PDGFRα. In hypereosinophilic syndrome patients without PDGFRα abnormality, Gleevec can be tried as therapy but it is unlikely to eliminate the disease; it may help control the disease signs and symptoms for a period of time.
New therapies for hypereosinophilic syndrome
For patients who are refractory to conventional therapies, use of monoclonal antibody therapy (medications that selectively bind to specific proteins) should be considered. Two drugs are currently available: mepolizumab that targets interleukin-5, a cytokine in blood that is recognized as a very important protein that governs eosinophil growth, and alemtuzumab that targets the CD52 protein expressed on the surface of eosinophils (its function not yet known). Mepolizumab, therefore, by blocking interleukin-5 eliminates a cytokine from blood that provides signal for eosinophil growth. Alemtuzumab, on the other hand, by binding to CD52 kills the eosinophil. Mepolizumab is not approved therapy yet and is currently available in a compassionate-use program (https://clinicaltrials.gov/) sponsored by GlaxoSmithKline, for patients with life-threatening hypereosinophilic syndrome that is not responding to usual therapy. Alemtuzumab is currently approved by the Food and Drug Administration (FDA) for use in B-cell chronic lymphocytic leukemia.
Hypereosinophilic syndrome prognosis
The prognosis in hypereosinophilic syndrome depends on the organ systems involved, disease severity and response to therapy. Outcomes can vary greatly from one person to the next. There is no cure. If hypereosinophilic syndrome is left untreated, the disease may be fatal. Your doctor can best answers questions about your specific prognosis in hypereosinophilic syndrome.
Bone marrow biopsy in hypereosinophilic syndrome, exhibiting a markedly increased number of eosinophils. This may happen with a number of disorders, including parasitic infection.
Although initial studies of hypereosinophilic syndrome showed a very poor prognosis (a 3 year survival rate of 12%) 2, management of cardiovascular disease by early echocardiographic monitoring and advances in medical and surgical therapies have improved the overall survival. A study of 40 cases by Lefebcve et al 12 showed a 5-year survival of 80% and a 15-year survival of 42%.
The availability of tyrosine kinase inhibitors such as imatinib, which prevent progression of cardiac disease and other organ damage—particularly in FIP1L1/PGDFRA–positive cases—will likely further improve the prognosis of hypereosinophilic syndrome. However, FIP1L1/PGDFRA– negative cases of hypereosinophilic syndrome that are resistant to corticosteroids have not been shown to have a durable response to imatinib.
Lastly, additional insight into the molecular pathogenesis of such cases of hypereosinophilic syndrome is required to develop effective targeted therapies.
Features that indicate a favorable prognosis in hypereosinophilic syndrome include the following:
- Angioedema
- Urticaria
- Elevated serum IgE level
- Sustained response to corticosteroids
- Early diagnosis and intensive management
The presence of features that are suggestive of myeloproliferative disorder and leukocytosis greater than 90,000/μ L carry a worse prognosis in hypereosinophilic syndrome.
Hypereosinophilic syndrome life expectancy
Hypereosinophilic syndrome is a chronic and progressive disorder that is potentially fatal. Blast transformation could occur after many years. True idiopathic hypereosinophilic syndrome is generally indolent, but patients with characteristics suggestive of a myeloproliferative/neoplastic disorder and those who develop chronic heart failure have a worse prognosis.
An older review of 57 patients with advanced hypereosinophilic syndrome reported a mean survival of 9 months and a 3-year survival rate of 12% 2. A later analysis from France noted an 80% survival at 5 years and a 42% survival at 15 years among 40 patients with hypereosinophilic syndrome 12.
References- Amy D. Klion; How I treat hypereosinophilic syndromes. Blood 2015; 126 (9): 1069–1077. doi: https://doi.org/10.1182/blood-2014-11-551614
- Chusid MJ, Dale DC, West BC, Wolff SM. The hypereosinophilic syndrome: analysis of fourteen cases with review of the literature. Medicine (Baltimore). 1975 Jan. 54(1):1-27.
- Noh HR, Magpantay GG. Hypereosinophilic syndrome. Allergy Asthma Proc. January 2017; 38(1):78-81.
- Queiroz Neto, Miguel Pedro de, & Gondim Filho, Fernando Antônio Galvão. (2017). Idiopathic hypereosinophilic syndrome with 20 years of diagnostic delay. Revista Brasileira de Hematologia e Hemoterapia, 39(2), 170-174. https://doi.org/10.1016/j.bjhh.2016.11.008
- Wardlaw AJ. Eosinophils and Related Disorders. Kaushansky K, Lichtman MA, Prchal JT, Levi MM, Press OW, Burns LJ, Caligiuri MA, eds. Williams Hematology. 9th ed. New York, NY: McGraw-Hill Education; 2016. 947-64.
- Gleich GJ, Leiferman KM. The hypereosinophilic syndromes: current concepts and treatments. Br J Haematol. 2009 May. 145(3):271-85.
- Yamada Y, Sanchez-Aguilera A, Brandt EB, et al. FIP1L1/PDGFRalpha synergizes with SCF to induce systemic mastocytosis in a murine model of chronic eosinophilic leukemia/hypereosinophilic syndrome. Blood. 2008 Sep 15. 112(6):2500-7.
- Simon HU, Plötz SG, Dummer R, Blaser K. Abnormal clones of T cells producing interleukin-5 in idiopathic eosinophilia. N Engl J Med. 1999 Oct 7. 341(15):1112-20.
- Curtis C, Ogbogu P. Hypereosinophilic Syndrome. Clin Rev Allergy Immunol. 2016 Apr. 50 (2):240-51.
- Yamada Y, Sanchez-Aguilera A, Brandt EB, et al. FIP1L1/PDGFRalpha synergizes with SCF to induce systemic mastocytosis in a murine model of chronic eosinophilic leukemia/hypereosinophilic syndrome. Blood. 2008 Sep 15. 112(6):2500-7
- Cincin AA, Ozben B, Tanrikulu MA, Baskan O, Agirbasli M. Large apical thrombus in a patient with persistent heart failure and hypereosinophilia: Löffler endocarditis. J Gen Intern Med. 2008 Oct. 23(10):1713-8.
- Lefebvre C, Bletry O, Degoulet P, et al. [Prognostic factors of hypereosinophilic syndrome. Study of 40 cases] [French]. Ann Med Interne (Paris). 1989. 140(4):253-7.