What is hemolytic anemia
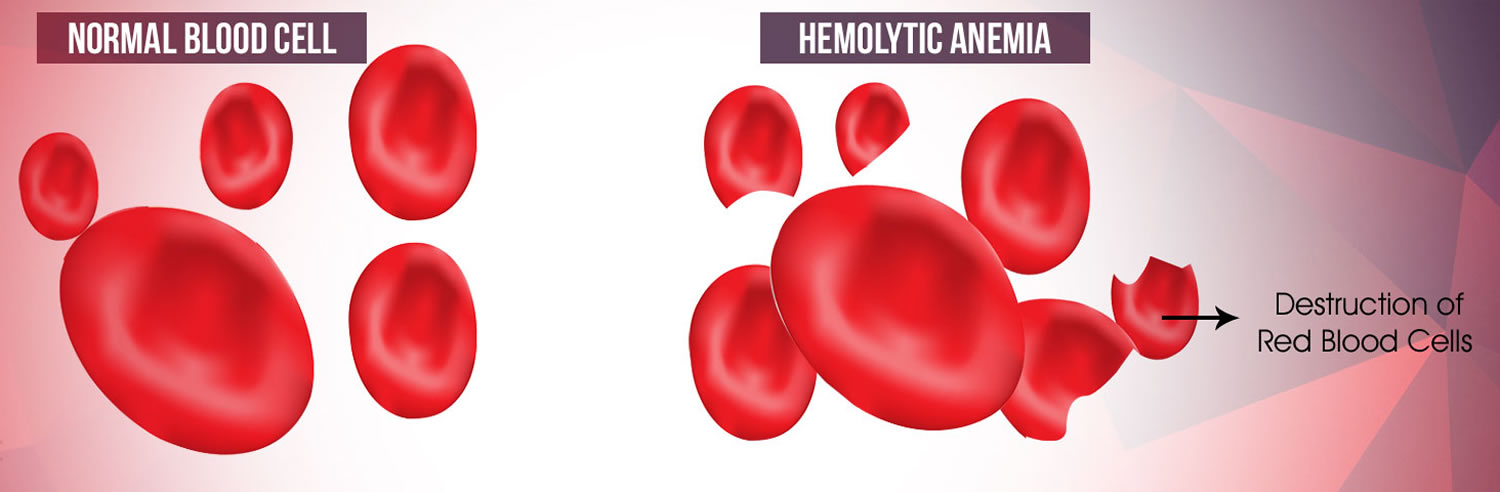
Hemolytic anemia is a condition in which red blood cells are destroyed and removed from the bloodstream before their normal lifespan is over.
The term “anemia” usually refers to a condition in which the blood has a lower than normal number of red blood cells.
Anemia also can occur if your red blood cells don’t contain enough hemoglobin. Hemoglobin is an iron-rich protein that carries oxygen from the lungs to the rest of the body.
Red blood cells are disc-shaped and look like doughnuts without holes in the center. These cells carry oxygen to your body. They also remove carbon dioxide (a waste product) from your body.
Red blood cells are made in the bone marrow—a sponge-like tissue inside the bones. They live for about 120 days in the bloodstream and then die.
White blood cells and platelets also are made in the bone marrow. White blood cells help fight infections. Platelets stick together to seal small cuts or breaks on blood vessel walls and stop bleeding.
When blood cells die, the body’s bone marrow makes more blood cells to replace them.
Hemolytic anemia is caused by high rates of red blood cell destruction. Many diseases, conditions, and factors can cause the body to destroy its red blood cells.
These causes can be inherited or acquired. “Inherited” means your parents passed the gene(s) for the condition on to you. “Acquired” means you aren’t born with the condition, but you develop it. Sometimes the cause of hemolytic anemia isn’t known.
There are many types of hemolytic anemia. Treatment and outlook depend on what type you have and how severe it is. The condition can develop suddenly or slowly. Symptoms can range from mild to severe.
Hemolytic anemia often can be successfully treated or controlled. Mild hemolytic anemia may need no treatment at all. Severe hemolytic anemia requires prompt and proper treatment, or it may be fatal.
Inherited forms of hemolytic anemia are lifelong conditions that may require ongoing treatment. Acquired forms of hemolytic anemia may go away if the cause of the condition is found and corrected.
Hemolytic anemia can lead to many health problems, such as fatigue (tiredness), pain, irregular heartbeats called arrhythmias, an enlarged heart, and heart failure.
Other names for hemolytic anemia
- Alloimmune hemolytic anemia
- Autoimmune hemolytic anemia (AIHA)
- Drug-induced hemolytic anemia
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency
- Hereditary elliptocytosis
- Hereditary ovalocytosis
- Hereditary spherocytosis
- Immune hemolytic anemia
- Microangiopathic hemolytic anemia
- Paroxysmal nocturnal hemoglobinuria (PNH)
- Pyruvate kinase deficiency
- Sickle cell anemia
- Thalassemias
Figure 1. Bone marrow anatomy
 Types of hemolytic anemia
Types of hemolytic anemia
There are many types of hemolytic anemia. The condition can be inherited or acquired. “Inherited” means your parents passed the gene for the condition on to you. “Acquired” means you aren’t born with the condition, but you develop it.
Inherited Hemolytic Anemias
With inherited hemolytic anemias, one or more of the genes that control red blood cell production are faulty. This can lead to problems with the hemoglobin, cell membrane, or enzymes that maintain healthy red blood cells.
The abnormal cells may be fragile and break down while moving through the bloodstream. If this happens, an organ called the spleen may remove the cell debris from the bloodstream.
Sickle Cell Anemia
Sickle cell anemia is a serious, inherited disease. In this disease, the body makes abnormal hemoglobin. This causes the red blood cells to have a sickle, or crescent, shape.
Sickle cells don’t last as long as healthy red blood cells. They usually die after only about 10 to 20 days. The bone marrow can’t make new red blood cells fast enough to replace the dying ones.
In the United States, sickle cell anemia mainly affects African Americans.
Thalassemias
Thalassemias are inherited blood disorders in which the body doesn’t make enough of certain types of hemoglobin. This causes the body to make fewer healthy red blood cells than normal.
Thalassemias most often affect people of Southeast Asian, Indian, Chinese, Filipino, Mediterranean, or African origin or descent.
Hereditary Spherocytosis
In this condition, a defect in the surface membrane (the outer covering) of red blood cells causes them to have a sphere, or ball-like, shape. These blood cells have a lifespan that’s shorter than normal.
Hereditary spherocytosis is the most common cause of hemolytic anemia among people of Northern European descent.
Hereditary Elliptocytosis (Ovalocytosis)
Like hereditary spherocytosis, this condition also involves a problem with the cell membrane. In this condition, the red blood cells are elliptic (oval) in shape. They aren’t as flexible as normal red blood cells, and they have a shorter lifespan.
Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency
In G6PD deficiency, the red blood cells are missing an important enzyme called G6PD. G6PD is part of the normal chemistry inside red blood cells.
In G6PD deficiency, if red blood cells come into contact with certain substances in the bloodstream, the missing enzyme causes the cells to rupture (burst) and die.
Many factors can trigger the breakdown of the red blood cells. Examples include taking sulfa or antimalarial medicines; being exposed to naphthalene, a substance found in some moth balls; eating fava beans; or having an infection.
G6PD deficiency mostly affects males of African or Mediterranean descent. In the United States, the condition is more common among African Americans than Caucasians.
Pyruvate Kinase Deficiency
In this condition, the body is missing an enzyme called pyruvate kinase. Not having enough of this enzyme causes red blood cells to break down easily.
This disorder is more common among the Amish than other groups.
Acquired Hemolytic Anemias
With acquired hemolytic anemias, your red blood cells may be normal. However, some other disease or factor causes the body to destroy red blood cells and remove them from the bloodstream.
The destruction of the red blood cells occurs in the bloodstream or, more commonly, in the spleen.
Immune Hemolytic Anemia
In immune hemolytic anemia, your immune system destroys your red blood cells. The three main types of immune hemolytic anemia are autoimmune, alloimmune, and drug-induced.
Autoimmune hemolytic anemia. In this condition, your immune system makes antibodies (proteins) that attack your red blood cells. Why this happens isn’t known.
Autoimmune hemolytic anemia accounts for half of all cases of hemolytic anemia. Autoimmune hemolytic anemia may come on very quickly and become serious.
Having certain diseases or infections can raise your risk for autoimmune hemolytic anemia. Examples include:
- Autoimmune diseases, such as lupus
- Chronic lymphocytic leukemia
- Non-Hodgkin’s lymphoma and other blood cancers
- Epstein-Barr virus
- Cytomegalovirus
- Mycoplasma pneumonia
- Hepatitis
- HIV
Autoimmune hemolytic anemia also can develop after you have a blood and marrow stem cell transplant.
In some types of autoimmune hemolytic anemia, the antibodies made by the body are called warm antibodies. This means they’re active (that is, they destroy red blood cells) at warm temperatures, such as body temperature.
In other types of autoimmune hemolytic anemia, the body makes cold-reactive antibodies. These antibodies are active at cold temperatures.
Cold-reactive antibodies can become active when parts of the body, such as the hands or feet, are exposed to temperatures lower than 32 to 50 degrees Fahrenheit (0 to 10 degrees Celsius).
Warm antibody autoimmune hemolytic anemia is more common than cold antibody autoimmune hemolytic anemia.
Alloimmune hemolytic anemia. This type of hemolytic anemia occurs if your body makes antibodies against red blood cells that you get from a blood transfusion. This can happen if the transfused blood is a different blood type than your blood.
This type of hemolytic anemia also can occur during pregnancy if a woman has Rh-negative blood and her baby has Rh-positive blood. “Rh-negative” and “Rh-positive” refer to whether your blood has Rh factor. Rh factor is a protein on red blood cells.
Drug-induced hemolytic anemia. Certain medicines can cause a reaction that develops into hemolytic anemia. Some medicines, such as penicillin, bind to red blood cell surfaces and can cause antibodies to develop.
Other medicines cause hemolytic anemia in other ways. Examples of these medicines include chemotherapy, acetaminophen, quinine and antimalarial medicines, anti-inflammatory medicines, and levodopa.
Mechanical Hemolytic Anemias
Physical damage to red blood cell membranes can cause them to break down faster than normal. Damage may be due to:
- Changes in the small blood vessels.
- An artificial heart valve or other device used in blood vessels.
- Hemodialysis. This treatment for kidney failure removes waste products from the blood.
- A heart-lung bypass machine, which may be used during open-heart surgery.
- Preeclampsia or eclampsia. Preeclampsia is high blood pressure during pregnancy. Eclampsia, which follows preeclampsia, is a serious condition that causes seizures in pregnant women.
- Malignant hypertension. This is a condition in which your blood pressure suddenly and rapidly rises.
- Thrombotic thrombocytopenic purpura. This rare blood disorder causes blood clots to form in small blood vessels throughout the body.
Blood cell damage also may occur in the limbs as a result of doing strenuous activities, such as taking part in marathons.
Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria is a disorder in which the red blood cells are faulty due to a lack of certain proteins. The body destroys these cells more quickly than normal.
People who have paroxysmal nocturnal hemoglobinuria are at increased risk for blood clots in the veins and low levels of white blood cells and platelets.
Other Causes of Damage to Red Blood Cells
Certain infections and substances also can damage red blood cells and lead to hemolytic anemia. Examples include malaria and blackwater fever, tick-borne diseases, snake venom, and toxic chemicals.
Hemolytic anemia causes
The immediate cause of hemolytic anemia is the early destruction of red blood cells. This means that red blood cells are destroyed and removed from the bloodstream before their normal lifespan is over.
Many diseases, conditions, and factors can cause the body to destroy its red blood cells. These causes can be inherited or acquired. “Inherited” means your parents passed the gene for the condition on to you. “Acquired” means you aren’t born with the condition, but you develop it.
Sometimes, the cause of hemolytic anemia isn’t known.
Inherited Hemolytic Anemias
In inherited hemolytic anemias, the genes that control how red blood cells are made are faulty. You can get a faulty red blood cell gene from one or both of your parents.
Different types of faulty genes cause different types of inherited hemolytic anemia. However, in each type, the body makes abnormal red blood cells. The problem with the red blood cells may involve the hemoglobin, cell membrane, or enzymes that maintain healthy red blood cells.
The abnormal cells may be fragile and break down while moving through the bloodstream. If this happens, an organ called the spleen may remove the cell debris from the bloodstream.
Acquired Hemolytic Anemias
In acquired hemolytic anemias, the body makes normal red blood cells. However, a disease, condition, or other factor destroys the cells. Examples of conditions that can destroy the red blood cells include:
- Immune disorders
- Infections
- Reactions to medicines or blood transfusions
- Hypersplenism (an enlarged spleen)
Risk Factors for hemolytic anemia
Hemolytic anemia can affect people of all ages and races and both sexes. Some types of hemolytic anemia are more likely to occur in certain populations than others.
For example, glucose-6-phosphate dehydrogenase (G6PD) deficiency mostly affects males of African or Mediterranean descent. In the United States, the condition is more common among African Americans than Caucasians.
In the United States, sickle cell anemia mainly affects African Americans.
Screening and Prevention of hemolytic anemia
You can’t prevent inherited types of hemolytic anemia. One exception is glucose-6-phosphate dehydrogenase (G6PD) deficiency.
If you’re born with G6PD deficiency, you can avoid substances that may trigger the condition. For example, avoid fava beans, naphthalene (a substance found in some moth balls), and certain medicines (as your doctor advises).
Some types of acquired hemolytic anemia can be prevented. For example, reactions to blood transfusions, which can cause hemolytic anemia, can be prevented. This requires careful matching of blood types between the blood donor and the recipient.
Prompt and proper prenatal care can help you avoid the problems of Rh incompatibility. This condition can occur during pregnancy if a woman has Rh-negative blood and her baby has Rh-positive blood. “Rh-negative” and “Rh-positive” refer to whether your blood has Rh factor. Rh factor is a protein on red blood cells.
Rh incompatibility can lead to hemolytic anemia in a fetus or newborn.
Hemolytic anemia signs and symptoms
The signs and symptoms of hemolytic anemia will depend on the type and severity of the disease.
People who have mild hemolytic anemia often have no signs or symptoms. More severe hemolytic anemia may cause many signs and symptoms, and they may be serious.
Many of the signs and symptoms of hemolytic anemia apply to all types of anemia.
Signs and Symptoms of Anemia
The most common symptom of all types of anemia is fatigue (tiredness). Fatigue occurs because your body doesn’t have enough red blood cells to carry oxygen to its various parts.
A low red blood cell count also can cause shortness of breath, dizziness, headache, coldness in your hands and feet, pale skin, and chest pain.
A lack of red blood cells also means that your heart has to work harder to move oxygen-rich blood through your body. This can lead to arrhythmias (irregular heartbeats), a heart murmur, an enlarged heart, or even heart failure.
Signs and Symptoms of Hemolytic Anemia
Jaundice
Jaundice refers to a yellowish color of the skin or whites of the eyes. When red blood cells die, they release hemoglobin into the bloodstream.
The hemoglobin is broken down into a compound called bilirubin, which gives the skin and eyes a yellowish color. Bilirubin also causes urine to be dark yellow or brown.
Pain in the Upper Abdomen
Gallstones or an enlarged spleen may cause pain in the upper abdomen. High levels of bilirubin and cholesterol (from the breakdown of red blood cells) can form into stones in the gallbladder. These stones can be painful.
The spleen is an organ in the abdomen that helps fight infection and filters out old or damaged blood cells. In hemolytic anemia, the spleen may be enlarged, which can be painful.
Leg Ulcers and Pain
In people who have sickle cell anemia, the sickle-shaped cells can clog small blood vessels and block blood flow. This can cause leg sores and pain throughout the body.
A Severe Reaction to a Blood Transfusion
You may develop hemolytic anemia due to a blood transfusion. This can happen if the transfused blood is a different blood type than your blood.
Signs and symptoms of a severe reaction to a transfusion include fever, chills, low blood pressure, and shock. Shock is a life-threatening condition that occurs if the body isn’t getting enough blood flow.
Hemolytic anemia diagnosis
Your doctor will diagnose hemolytic anemia based on your medical and family histories, a physical exam, and test results.
Specialists Involved
Primary care doctors, such as a family doctor or pediatrician, may help diagnose and treat hemolytic anemia. Your primary care doctor also may refer you to a hematologist. This is a doctor who specializes in diagnosing and treating blood diseases and disorders.
Doctors and clinics that specialize in treating inherited blood disorders, such as sickle cell anemia and thalassemias, also may be involved.
If your hemolytic anemia is inherited, you may want to consult a genetic counselor. A counselor can help you understand your risk of having a child who has the condition. He or she also can explain the choices that are available to you.
Medical and Family Histories
To find the cause and severity of hemolytic anemia, your doctor may ask detailed questions about your symptoms, personal medical history, and your family medical history.
He or she may ask whether:
- You or anyone in your family has had problems with anemia
- You’ve recently had any illnesses or medical conditions
- You take any medicines, and which ones
- You’ve been exposed to certain chemicals or substances
- You have an artificial heart valve or other medical device that could damage your red blood cells
Physical Exam
Your doctor will do a physical exam to check for signs of hemolytic anemia. He or she will try to find out how severe the condition is and what’s causing it.
The exam may include:
- Checking for jaundice (a yellowish color of the skin or whites of the eyes)
- Listening to your heart for rapid or irregular heartbeats
- Listening for rapid or uneven breathing
- Feeling your abdomen to check the size of your spleen
- Doing a pelvic and rectal exam to check for internal bleeding
Diagnostic Tests and Procedures
Many tests are used to diagnose hemolytic anemia. These tests can help confirm a diagnosis, look for a cause, and find out how severe the condition is.
Complete Blood Count
Often, the first test used to diagnose anemia is a complete blood count (CBC). The complete blood count measures many parts of your blood.
This test checks your hemoglobin and hematocrit levels. Hemoglobin is an iron-rich protein in red blood cells that carries oxygen to the body. Hematocrit is a measure of how much space red blood cells take up in your blood. A low level of hemoglobin or hematocrit is a sign of anemia.
The normal range of these levels may vary in certain racial and ethnic populations. Your doctor can explain your test results to you.
The complete blood count also checks the number of red blood cells, white blood cells, and platelets in your blood. Abnormal results may be a sign of hemolytic anemia, a different blood disorder, an infection, or another condition.
Finally, the complete blood count looks at mean corpuscular volume (MCV). Mean corpuscular volume (MCV) is a measure of the average size of your red blood cells. The results may be a clue as to the cause of your anemia.
Other Blood Tests
If the complete blood count results confirm that you have anemia, you may need other blood tests to find out what type of anemia you have and how severe it is.
Reticulocyte count. A reticulocyte count measures the number of young red blood cells in your blood. The test shows whether your bone marrow is making red blood cells at the correct rate.
People who have hemolytic anemia usually have high reticulocyte counts because their bone marrow is working hard to replace the destroyed red blood cells.
Peripheral smear. For this test, your doctor will look at your red blood cells through a microscope. Some types of hemolytic anemia change the normal shape of red blood cells.
Coombs’ test. This test can show whether your body is making antibodies (proteins) to destroy red blood cells.
Haptoglobin, bilirubin, and liver function tests. When red blood cells break down, they release hemoglobin into the bloodstream. The hemoglobin combines with a chemical called haptoglobin. A low level of haptoglobin in the bloodstream is a sign of hemolytic anemia.
Hemoglobin is broken down into a compound called bilirubin. High levels of bilirubin in the bloodstream may be a sign of hemolytic anemia. High levels of this compound also occur with some liver and gallbladder diseases. Thus, you may need liver function tests to find out what’s causing the high bilirubin levels.
Hemoglobin electrophoresis. This test looks at the different types of hemoglobin in your blood. It can help diagnose the type of anemia you have.
Testing for paroxysmal nocturnal hemoglobinuria (PNH). In paroxysmal nocturnal hemoglobinuria, the red blood cells are missing certain proteins. The test for paroxysmal nocturnal hemoglobinuria can detect red blood cells that are missing these proteins.
Osmotic fragility test. This test looks for red blood cells that are more fragile than normal. These cells may be a sign of hereditary spherocytosis (an inherited type of hemolytic anemia).
Testing for glucose-6-phosphate dehydrogenase (G6PD) deficiency. In G6PD deficiency, the red blood cells are missing an important enzyme called G6PD. The test for G6PD deficiency looks for this enzyme in a sample of blood.
Urine Test
A urine test will look for the presence of free hemoglobin (a protein that carries oxygen in the blood) and iron.
Bone Marrow Tests
Bone marrow tests show whether your bone marrow is healthy and making enough blood cells. The two bone marrow tests are aspiration (as-pi-RA-shun) and biopsy.
For a bone marrow aspiration, your doctor removes a small amount of fluid bone marrow through a needle. The sample is examined under a microscope to check for faulty cells.
A bone marrow biopsy may be done at the same time as an aspiration or afterward. For this test, your doctor removes a small amount of bone marrow tissue through a needle. The tissue is examined to check the number and type of cells in the bone marrow.
You may not need bone marrow tests if blood tests show what’s causing your hemolytic anemia.
Tests for Other Causes of Anemia
Because anemia has many causes, you may have tests for conditions such as:
- Kidney failure
- Lead poisoning
- Vitamin or iron deficiency
Newborn Testing for Sickle Cell Anemia and G6PD Deficiency
All States mandate screening for sickle cell anemia as part of their newborn screening programs. Some States also mandate screening for G6PD deficiency. These inherited types of hemolytic anemia can be detected with routine blood tests.
Diagnosing these conditions as early as possible is important so that children can get proper treatment.
Hemolytic anemia treatment
Treatments for hemolytic anemia include blood transfusions, medicines, plasmapheresis, surgery, blood and marrow stem cell transplants, and lifestyle changes.
People who have mild hemolytic anemia may not need treatment, as long as the condition doesn’t worsen. People who have severe hemolytic anemia usually need ongoing treatment. Severe hemolytic anemia can be fatal if it’s not properly treated.
Goals of Treatment
The goals of treating hemolytic anemia include:
- Reducing or stopping the destruction of red blood cells
- Increasing the red blood cell count to an acceptable level
- Treating the underlying cause of the condition
Treatment will depend on the type, cause, and severity of the hemolytic anemia you have. Your doctor also will consider your age, overall health, and medical history.
If you have an inherited form of hemolytic anemia, it’s a lifelong condition that may require ongoing treatment. If you have an acquired form of hemolytic anemia, it may go away if its cause can be found and corrected.
Blood Transfusions
Blood transfusions are used to treat severe or life-threatening hemolytic anemia.
A blood transfusion is a common procedure in which blood is given to you through an intravenous (IV) line in one of your blood vessels. Transfusions require careful matching of donated blood with the recipient’s blood.
Medicines
Medicines can improve some types of hemolytic anemia, especially autoimmune hemolytic anemia (AIHA). Corticosteroid medicines, such as prednisone, can stop your immune system from, or limit its ability to, make antibodies (proteins) against red blood cells.
If you don’t respond to corticosteroids, your doctor may prescribe other medicines to suppress your immune system. Examples include the medicines rituximab and cyclosporine.
If you have severe sickle cell anemia, your doctor may recommend a medicine called hydroxyurea. This medicine prompts your body to make fetal hemoglobin. Fetal hemoglobin is the type of hemoglobin that newborns have.
In people who have sickle cell anemia, fetal hemoglobin helps prevent red blood cells from sickling and improves anemia.
Plasmapheresis
Plasmapheresis is a procedure that removes antibodies from the blood. For this procedure, blood is taken from your body using a needle inserted into a vein.
The plasma, which contains the antibodies, is separated from the rest of the blood. Then, plasma from a donor and the rest of the blood is put back in your body.
This treatment may help if other treatments for immune hemolytic anemia don’t work.
Surgery
Some people who have hemolytic anemia may need surgery to remove their spleens. The spleen is an organ in the abdomen. A healthy spleen helps fight infection and filters out old or damaged blood cells.
An enlarged or diseased spleen may remove more red blood cells than normal, causing anemia. Removing the spleen can stop or reduce high rates of red blood cell destruction.
Blood and Marrow Stem Cell Transplant
In some types of hemolytic anemia, such as thalassemias, the bone marrow doesn’t make enough healthy red blood cells. The red blood cells it does make may be destroyed before their normal lifespan is over. Blood and marrow stem cell transplants may be used to treat these types of hemolytic anemia.
A blood and marrow stem cell transplant replaces damaged stem cells with healthy ones from another person (a donor).
During the transplant, which is like a blood transfusion, you get donated stem cells through a tube placed in a vein. Once the stem cells are in your body, they travel to your bone marrow and begin making new blood cells.
Lifestyle Changes
If you have autoimmune hemolytic anemia with cold-reactive antibodies, try to avoid cold temperatures. This can help prevent the breakdown of red blood cells. It’s very important to protect your fingers, toes, and ears from the cold.
To protect yourself, you can:
- Wear gloves or mittens when taking food out of the refrigerator or freezer.
- Wear a hat, scarf, and a coat with snug cuffs during cold weather.
- Turn down air conditioning or dress warmly while in air-conditioned spaces.
- Warm up the car before driving in cold weather.
People born with glucose-6-phosphate dehydrogenase (G6PD) deficiency can avoid substances that may trigger anemia. For example, avoid fava beans, naphthalene (a substance found in some moth balls), and certain medicines (as your doctor advises).
Living with hemolytic anemia
Hemolytic anemia can be mild or severe. Inherited forms of hemolytic anemia are lifelong conditions and may require ongoing treatment. Acquired forms of the condition may go away if the cause is found and corrected.
Ongoing Care
If you have hemolytic anemia, take good care of your health. See your doctor regularly and follow your treatment plan. Talk with your doctor about whether you should get a yearly flu shot and a pneumonia vaccine.
Ask your doctor about ways to reduce your chance of getting an infection, such as:
- Staying away from people who are sick and avoiding large crowds of people.
- Avoiding certain kinds of foods that can expose you to bacteria, such as uncooked foods.
- Washing your hands often.
- Brushing and flossing your teeth and getting regular dental care to reduce the risk of infection in your mouth and throat.
Lifestyle Changes
You can take steps to stay healthy. For example, try to get plenty of rest.
If you have cold-reactive autoimmune hemolytic anemia, stay away from cold temperatures. During cold weather, wear a hat, scarf, and a warm coat. When taking cold food out of the refrigerator or freezer, wear gloves. Turn down air conditioning or dress warmly while in air-conditioned spaces. Warm up the car before driving in cold weather.
If you have glucose-6-phosphate dehydrogenase (G6PD) deficiency, avoid substances that can trigger anemia. For example, avoid fava beans, naphthalene (a substance found in some moth balls), and certain medicines (as your doctor advises).
Ask your doctor what types and amounts of physical activity are safe for you. You may want to avoid certain sports or activities that could worsen your condition or lead to complications.
Hemolytic Anemia and Children
Parents of children who have hemolytic anemia usually want to learn as much as possible about the condition from their child’s health care team.
You can be an active partner in caring for your child. Talk with your child’s health care team about treatment, diet, and physical activity. Learn the signs of worsening anemia and possible complications so you can contact your child’s doctor.
You may want to educate family members, friends, and your child’s classmates about hemolytic anemia. You also may want to tell your child’s teachers or other caregivers about the condition. Let them know whether your child has any special limitations or restrictions.
Family members, friends, teachers, and caregivers can provide a network of support to help your child cope with his or her hemolytic anemia.
Allow teenagers to have input in decisions about their health. This encourages them to take an active role in their health care. Help them understand lifestyle restrictions and their medical needs so they can better cope with having hemolytic anemia.