What is Henoch Schonlein purpura
Henoch–Schönlein purpura (HSP) is a form of leukocytoclastic or small-vessel vasculitis with deposition of immune IgA complexes 1, most often observed in children. It is sometimes called anaphylactoid purpura. Henoch Schonlein purpura results from inflammation of the small blood vessels in the skin and various other tissues within the body.
Henoch Schonlein purpura generally affects children, but it may also occur in adults. Henoch Schonlein purpura is the most common form of vasculitis in children, with an annual incidence on the order of 15 cases/100,000 children (under 17 years old) per year 2. 75% of cases occur in children with the mean age of patients with Henoch Schonlein purpura of 5.9 years. It is thought by most researchers to be more common in girls, although some have found a male predominance or both sexes to be equally affected. Henoch Schonlein purpura may occur in adults and when it does, it is often more severe and kidney damage is more common than is the case in children. There does not appear to be any racial predilection. 15 to 40% of children have at least one recurrence.
The most common symptoms of Henoch Schonlein purpura include a vasculitic rash, joint pain, and abdominal pain. It may affect the kidneys and in some instances this leads to irreversible kidney damage. However, most cases resolve without treatment or long-term consequences.
Henoch Schonlein purpura can’t spread to others, so your child can return to school or nursery when they feel well enough or you can go back to work as soon as you feel up to it.
Doctors don’t know how to prevent Henoch Schonlein purpura.
Hallmarks of Henoch Schonlein purpura:
- Arthritis: pain and swelling in the joints (such as the knees and ankles) which can come and go and can move around from joint to joint. Joint pain sometimes precedes the classical rash by one or two weeks. These symptoms subside when the disease clears and leave no lasting damage.
- Gastrointestinal involvement: abdominal pain, nausea, vomiting or blood in the feces (stools) is caused by the blood vessels in the bowel becoming inflamed (irritated and swollen) and can indicate more serious problems (such as an abnormal folding of the bowel called intussusception). These symptoms sometimes occur before the rash appears.
- Kidney inflammation: blood in the urine is caused by the blood vessels in the kidney becoming inflamed (irritated and swollen). Serious kidney problems don’t happen very often, but they can occur
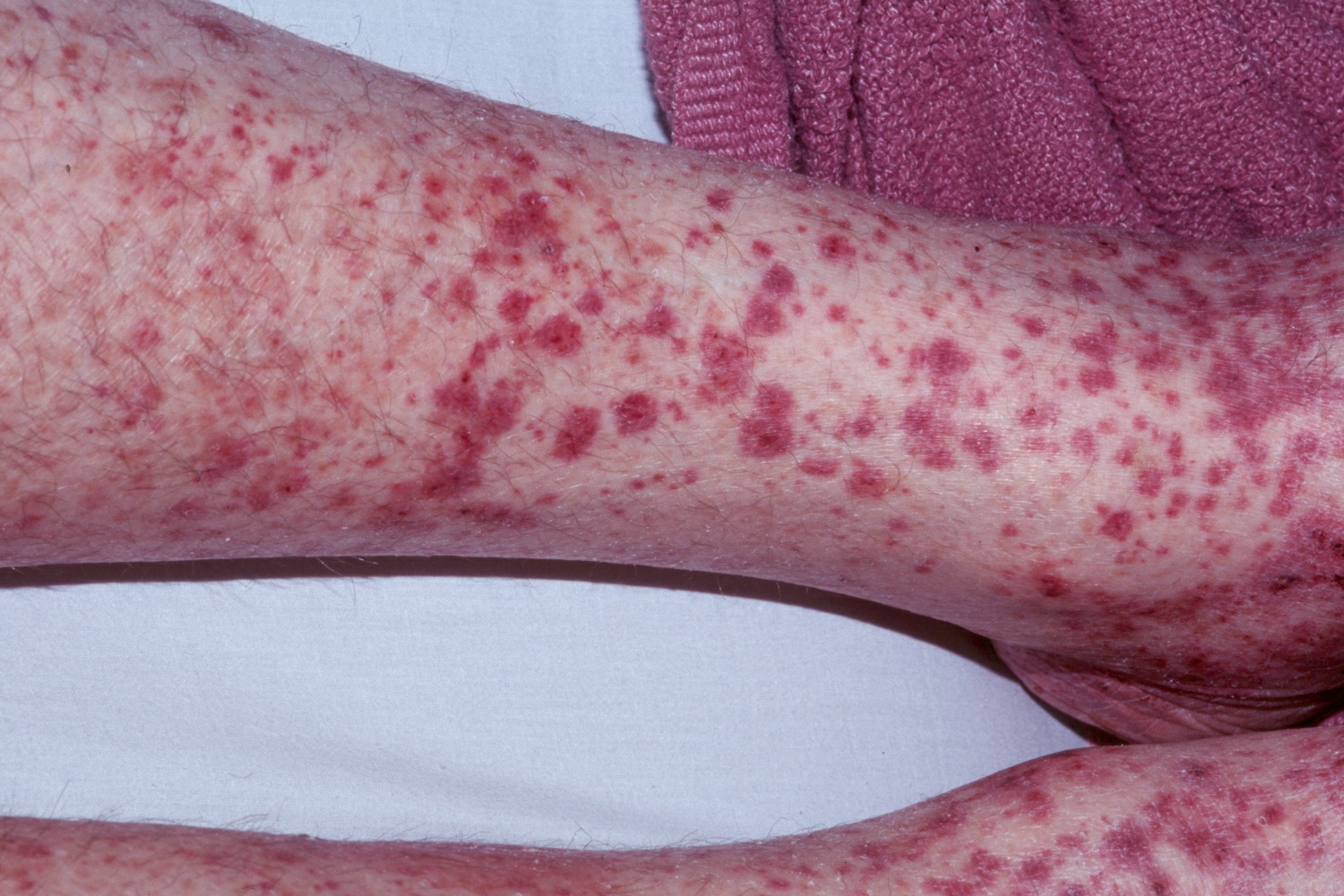
- Purpura (skin rash): this may start out looking like red spots, bumps or raised red skin welts which can be itchy. This quickly changes to small bruises or reddish-purple spots that are often raised; it usually appears on the buttocks, on the legs and around the elbows. Blisters and/or ulcers may develop in the affected areas.
Dr. William Heberden, a London physician, described the first cases of Henoch-Schönlein purpura (HSP) in 1801. Johann Schönlein (1837) and Edouard Henoch (1874) reported additional cases decades after Heberden. They recognized that the Henoch Schonlein purpura disorder often followed upper respiratory tract infections and was not always self-limited, sometimes progressing to serious kidney involvement.
Usually, Henoch Schonlein purpura affects a child shortly after an upper respiratory infection has resolved.
Fortunately, most people with Henoch Schonlein purpura make a full recovery without any treatment. But there’s also a small chance the kidneys could be permanently damaged (chronic kidney disease). Henoch Schonlein purpura develops into a chronic condition in up to 5% of individuals, which means they continue to have symptoms into adulthood 3. This is why it’s important to have regular check-ups.
Pain relief (such as paracetamol) can help the joint pain. You must follow the dosage instructions on the bottle. It is dangerous to give more than the recommended dose. Your doctor may recommend a drug called prednisolone. This can help people with severe stomach pains or very painful joints.
The illness lasts 4 to 6 weeks in most patients. The rash (purpura) changes from red to purple, becomes rust-colored and then fades completely.
About one-third of those with Henoch Schonlein purpura can get it again, usually within 4 months of the initial illness. Repeat episodes of Henoch Schonlein purpura are usually milder and shorter and more common in patients with kidney involvement.
Henoch Schonlein purpura in adults
Compared with children, Henoch Schonlein purpura in adults is more severe, adults are more prone to permanent kidney damage and frequently associated with cancer 4. Compared with children, clinical features and prognosis are different in adults: firstly the renal damage seems more frequent and serious, and then the frequency of associated cancers is higher 5. Cancers involved are bronchopulmonary, digestive, renal, and prostate. Henoch Schonlein purpura prognosis is usually good, except in gastrointestinal and nephritis involvements. However, patients can take some comfort in knowing that fewer than 5% of patients with Henoch Schonlein purpura develop progressive renal insufficiency.
Figure 1. Henoch Schonlein purpura rash
Figure 2. Henoch schonlein purpura (with vesicle [blister] formation)
Henoch Schonlein purpura long term effects
Most people with Henoch Schonlein purpura get better over time without treatment and have no long-term problems. Any kidney problems usually get better without treatment. But sometimes Henoch Schonlein purpura can be severe and last several months, particularly in adults. About 5 percent of those with Henoch Schonlein purpura develop long-term kidney disease (called glomerulonephritis). This may occur in the first week or so of the illness, but there may be a delay of weeks or months before it appears. Your doctor will want to check urine samples and blood pressure several times after the Henoch Schonlein purpura goes away to check for kidney problems. These checks should go on for at least 6 months and some doctors recommend a blood pressure and urine check every year for life.
Relapse occurs in one-third of cases, usually within 4 months of the initial episode. Some patients with Henoch Schonlein purpura can go on to develop hypertension (high blood pressure) or significant renal impairment later in life. Pulmonary hemorrhage is rare, but when does occur, is often fatal 6. Presenting symptoms include dyspnea, tachypnea, coughing and hemoptysis.
Henoch Schonlein purpura complications
For most people, symptoms improve within a month, leaving no lasting problems. But recurrences are fairly common.
Complications associated with Henoch-Schonlein purpura include:
- Kidney damage. The most serious complication of Henoch-Schonlein purpura is kidney damage. This risk is greater in adults with the condition than in children. Occasionally the damage is severe enough that dialysis or a kidney transplant may be needed.
- Bowel obstruction. In rare cases, Henoch-Schonlein purpura can cause intussusception — a condition in which a section of the bowel folds into itself like a telescope, which prevents matter from moving through the bowel. This is rare in adults.
Henoch Schonlein purpura causes
Although the precise cause is unknown, clinical evidence points to an an abnormal response of the immune system. The result is inflammation in the microscopic blood vessels in the skin is called vasculitis. The vasculitis affects the small blood vessels in the skin, causing a rash (purple spots called purpura). Blood vessels in the joints, kidneys, or the intestines may also be affected. It is unclear why this occurs. It might be triggered by bacterial or viral infections, medicines, insect bites or exposure to chemicals or cold weather. Infectious triggers may include chickenpox, strep throat, measles and hepatitis.
In two-thirds of the cases, Henoch Schonlein purpura follows an upper respiratory tract infection, with onset an average of ten days after the start of respiratory symptoms. Despite this association, no single microorganism or environmental exposure has been confirmed as an important cause of Henoch Schonlein purpura.
The peak incidence of pediatric Henoch Schonlein purpura is during the autumn and winter months. It often preceded by an upper respiratory tract infection, and is found to cluster within families. Beta-haemolytic streptococci are often found on throat swab or there is positive streptococcal serology on blood testing.
A multitude of other associations have been reported, including medications. These include: ACE inhibitors, angiotensin II receptor antagonists, clarithromycin and nonsteroidal anti-inflammatories.
The underlying mechanism of small blood vessel inflammation is the deposition of IgA immunoglobulin within the blood vessel walls. This leads to leucocytoclastic vasculitis. A subtle defect of IgA may predispose people to developing Henoch Schonlein purpura.
Some evidence suggests that genetic predisposition may contribute to the development of this disease in some cases. Only a few families with multiple relatives affected by Henoch Schonlein purpura have been reported in the medical literature. The association between particular genes and a slight increase in the chance of developing Henoch Schonlein purpura has not been proven 7.
Risk factors for Henoch Schonlein purpura
Factors that may increase the risk of developing Henoch-Schonlein purpura include:
- Age. The disease affects primarily children and young adults, with the majority of cases occurring in children between 2 and 6 years of age.
- Sex. Henoch-Schonlein purpura is slightly more common in boys than girls.
- Race. White and Asian children are more likely to develop Henoch-Schonlein purpura than are black children.
- Time of year. Henoch-Schonlein purpura strikes mainly in autumn, winter and spring but rarely in summer.
Henoch Schonlein purpura symptoms
The classic presentation is with a tetrad of symptoms and signs:
- Rash (purpura)
- Arthritis
- Abdominal pain, which can come and go and in some cases can be severe
- Kidney impairment
The symptoms are usually preceded by 2-3 weeks of fever, headache, muscle/joint aches, or abdominal pain.
A rash is present in virtually all cases. It usually starts as red spots or bumps (which may have a ‘hive-like’ appearance) which rapidly change to small dark purple bumps (palpable purpura) within the first 24 hours. The most common sites of involvement are the lower legs, buttocks, elbows and knees. The rash is symmetrical and may even become generalized. Blisters and/or ulcers may develop in the affected areas.
Arthritis (joint inflammation) is present in 75% of cases and usually involves one to four joints, especially the ankles and knees. It may be transient and move between different joints.
Abdominal pain is present in half to three-quarters of patients and precedes the rash in up to one third. There may be associated diarrhea and bleeding from the bowel. Orchitis and interssusception are possible complications.
Kidney involvement is seen in up to 50% of cases. It is usually mild and self-limiting, however it is important that it is diagnosed and followed up as persistent impairment may occur. It normally occurs within a few days to one month after the onset of the other symptoms. Approximately 10% have serious kidney problems at presentation, 15% are left with subtle abnormalities in their urine tests, and 1-5% progress to end-stage kidney failure long term.
Many children with Henoch Schonlein purpura also have swelling over the backs of their feet and hands, and the scrotum in boys. Rarely involvement of other organs such as the lungs, brain, and heart occurs.
Henoch Schonlein purpura diagnosis
Purpura not due to a low platelet count, caused by inflammation in blood vessels of the skin, is the hallmark of Henoch Schonlein purpura. The tetrad of purpura, arthritis, kidney inflammation, and abdominal pain is often observed. However, all four elements of this tetrad are not required for diagnosis. The microscopic hallmark of Henoch Schonlein purpura is the deposition of IgA (an antibody found in blood, saliva, tears, etc.) in the walls of involved blood vessels.
More than 90% of cases occur in children. The disease usually resolves within a few weeks. However, adult cases are sometimes more difficult. Skin manifestations are more variable in adults, and sometimes symptoms in adults endure longer.
The diagnosis is often obvious if the classic symptoms are present:
- A blood and urine test should be performed to look for any signs of kidney involvement. These tests should be repeated at regular intervals initially to ensure kidney impairment is not developing or worsening.
- Blood pressure should be measured at the same time.
- A skin biopsy is often not necessary especially in children, but may be performed to confirm the diagnosis.
Henoch Schonlein purpura can be mimicked by other forms of systemic vasculitis that are more often life-threatening. Granulomatosis with polyangiitis and microscopic polyangiitis can also present with purpura, arthritis, and renal inflammation. These disorders both have the potential for serious involvement of other organs (for example, the lungs, eyes, and peripheral nerves) and carry more dire renal prognoses. Therefore, it is very important to distinguish the difference by performing a careful evaluation including bloodwork, urinalysis, chest imaging, and possibly biopsies. Henoch Schonlein purpura may be misdiagnosed as another form of vasculitis – most commonly hypersensitivity vasculitis – because of the frequent failure to perform direct immunofluorescence (DIF) testing on skin biopsy and the consequent failure to detect IgA.
Henoch Schonlein purpura treatment
Unfortunately, there is no cure for Henoch-Schonlein purpura (HSP). In the majority of cases, no specific treatment is required and the rash fades over one week. Recurrent crops of lesions occur over the next 6–16 weeks in up to one-third of cases. Five to ten per cent may even have persistent disease.
Treatments aim to relieve the symptoms of this condition.
- Non-steroidal-anti-inflammatory-drugs (e.g., ibuprofen, naprosyn) are effective at relieving joint and abdominal pain.
- In more severe cases, oral steroid medication is often used.
- Other options include dapsone or colchicine.
- If significant kidney involvement is present, steroids are usually combined with more potential immunosuppressives or intravenous immunoglobulin.
Non-steroidal-anti-inflammatory-drugs (NSAIDs) may alleviate arthralgias but can aggravate gastrointestinal symptoms, and should be avoided in any patient with renal disease. Dapsone (100 mg/day) may be effective in cases of Henoch Schonlein purpura, perhaps through disrupting the abnormal immune response. Although steroids have not been evaluated rigorously in Henoch Schonlein purpura, they appear to ease joint and gastrointestinal symptoms, in many (but not all) patients. Steroids, however, do not appear to improve the rash; although usually, over weeks to months, the recurrent bouts of purpura usually resolve on their own.
Surgery
If a section of the bowel has folded in upon itself or ruptured, surgical repair will be necessary.
Living With Henoch Schonlein purpura
Supportive care may involve a short course of prednisone or an non-steroidal-anti-inflammatory-drug (NSAID), such as naprosyn or ibuprofen, if the kidneys are not involved. Keeping the legs elevated may help prevent purpura during flares of active disease. Additionally, many patients’ purpura will recur after they start to feel better and become more active, inherently increasing their exposures to very minor trauma (e.g. jogging, leg shaving, increasing gravity exposures). Often, the recurring purpura is less prevalent and additional Henoch Schonlein purpura symptoms are often absent. In many fewer cases, primarily in adults, Henoch Schonlein purpura can progress from hematuria (blood in the urine) to renal insufficiency (decreased kidney function). Henoch Schonlein purpura patients who experience this symptom should be followed more closely, with regular testing of their urine for blood and protein. Recurrences, found in 33% of patients, usually develop within the first four months after resolution of the first bout.
Regular check-ups for kidney problems
You’ll have regular check-ups for 6 to 12 months to check how well your kidneys are working.
You’ll usually be asked to provide a sample of urine and have your blood pressure checked at each appointment. This may be done at home, at your doctor’s clinic or in hospital.
References- IgA immune complexes in Henoch-Schönlein purpura. Levinsky RJ, Barratt TM. Lancet. 1979 Nov 24; 2(8152):1100-3. https://www.ncbi.nlm.nih.gov/pubmed/91839/
- Clinical update: Henoch-Schönlein purpura. Saulsbury FT. Lancet. 2007 Mar 24; 369(9566):976-8. https://www.ncbi.nlm.nih.gov/pubmed/17382810/
- Bossart P. Henoch-Schonlein Purpura in Emergency Medicine. http://emedicine.medscape.com/article/780452-overview#a0199
- Pindi Sala T, Michot J-M, Snanoudj R, et al. Successful Outcome of a Corticodependent Henoch-Schönlein Purpura Adult with Rituximab. Case Reports in Medicine. 2014;2014:619218. doi:10.1155/2014/619218. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3988713/
- Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D. Henoch-Schönlein Purpura in adults: outcome and prognostic factors. Journal of the American Society of Nephrology. 2002;13(5):1271–1278. http://jasn.asnjournals.org/content/13/5/1271.long
- PD 1997;299
- He X, Yu C, Zhao P, Ding Y, Liang X, Zhao Y, Yue X, Wu Y, Yin W. The genetics of Henoch-Schönlein purpura: a systematic review and meta-analysis. Rheumatology International. 2013; Jan 17:Epub ahead of print. http://www.ncbi.nlm.nih.gov/pubmed/23325094