What is vaginitis
Vaginitis is an inflammation of the vagina that is characterized by vaginal symptoms, including vaginal discharge, bad odor, itching, irritation, pain or burning 1. Vaginal symptoms are a common reason women seek medical care. There are many types of vaginitis, each with its own cause, symptoms, and treatment. The cause of vaginitis is usually a change in the normal balance of vaginal bacteria or an infection. Reduced estrogen levels after menopause and some skin disorders can also cause vaginitis. Pregnant women with some types of vaginitis may be at higher risk of preterm birth.
Most women have at least one episode of vaginitis during their lives, making it the most common gynecologic diagnosis in primary care. Studies have shown a negative effect on quality of life in women with vaginitis, with some women expressing anxiety, shame, and concerns about hygiene, particularly in those with recurrent symptoms.
Physicians traditionally diagnose vaginitis using the combination of symptoms, physical examination, pH of vaginal fluid, microscopy, and the whiff test.
Symptoms of vaginitis
Symptoms of vaginitis include:
- an abnormal vaginal discharge
- vaginal irritation or itching
- pain when peeing or having sex
- light bleeding or spotting
A strong, unpleasant smell, particularly after sex, can be a sign of bacterial vaginosis or trichomoniasis, which can sometimes cause vaginitis.
The most common types of vaginitis are:
Bacterial vaginosis, trichomoniasis, and vulvovaginal candidiasis are the most common infectious causes of vaginitis 2.
- Bacterial vaginosis, which results from a change of the normal bacteria found in your vagina to overgrowth of other organisms
- Yeast infections, which are usually caused by a naturally occurring fungus called Candida albicans
- Trichomoniasis, which is caused by a parasite and is commonly transmitted by sexual intercourse
Women with trichomoniasis or bacterial vaginosis are at a greater risk of acquiring sexually transmitted infections because of the inflammation caused by these disorders. In pregnant women, symptomatic bacterial vaginosis and trichomoniasis have been associated with premature deliveries and low birth weight babies.
Treatment depends on the type of vaginitis you have.
How to treat vaginitis
Treatment for vaginitis depends on what’s causing it.
Yeast infections, such as vaginal thrush, are usually treated with antifungal medicines, and bacterial infections are usually treated with antibiotics.
- Bacterial vaginosis—Your doctor may offer you oral pills or a vaginal cream. Your sex partner usually will not need to be treated.
- Vulvovaginal candidiasis—Your doctor may recommend vaginal cream, vaginal pills, or oral pills. Your sex partner does not need to be treated.
- Trichomoniasis—Oral pills can treat this infection. Your sex partner should also be treated. Your doctor may test you again in three months to see if you have been infected again.
See your doctor or go to a sexual health clinic if you have any unusual vaginal symptoms, particularly if:
- You have vaginal itching or an unpleasant smelling vaginal discharge
- You’ve never had a vaginal infection. Seeing your doctor can establish the cause and help you learn to identify the signs and symptoms.
- You have had vaginal infections in the past, but this time your symptoms are different
- You have had multiple sex partners or you have a new sexual partner – you could have a sexually transmitted infection (STI) also known as sexually transmitted diseases (STDs). Some sexually transmitted infections have signs and symptoms similar to those of a yeast infection or bacterial vaginosis.
- You have finished a course of medication (over-the-counter anti-yeast medication) for vaginal thrush, but your symptoms are persisting
- You have a fever, chills or pelvic pain.
There’s no need to see your doctor if you’ve been diagnosed with thrush in the past and your symptoms are the same.
If you’re sure you have thrush and you’ve treated it successfully in the past with over-the-counter medication, you can treat it yourself again.
Vaginitis symptoms
Vaginitis signs and symptoms can include:
- Change in color, odor or amount of discharge from your vagina
- Vaginal itching or irritation
- Pain during intercourse
- Painful urination
- Light vaginal bleeding or spotting
If you have vaginal discharge, which many women don’t, the characteristics of the discharge might indicate the type of vaginitis you have. Examples include:
- Bacterial vaginosis. You might develop a grayish-white, foul-smelling discharge. The odor, often described as a fishy odor, might be more obvious after sexual intercourse.
- Yeast infection. The main symptom is itching, but you might have a white, thick discharge that resembles cottage cheese.
- Trichomoniasis. An infection called trichomoniasis can cause a greenish-yellow, sometimes frothy discharge.
What causes vaginitis
Vaginitis can be caused by any of the following infections or irritants:
- Bacterial vaginosis – a bacterial infection where the balance of bacteria inside the vagina is disrupted. This most common cause of vaginitis results from a change of the normal bacteria found in your vagina, to overgrowth of one of several other organisms. Usually, bacteria normally found in the vagina (lactobacilli) are outnumbered by other bacteria (anaerobes) in your vagina. If anaerobic bacteria become too numerous, they upset the balance, causing bacterial vaginosis. This type of vaginitis seems to be linked to sexual intercourse — especially if you have multiple sex partners or a new sex partner — but it also occurs in women who aren’t sexually active.
- Candidal vaginitis or yeast infections – a common yeast infection that affects most women at some point. These occur when there’s an overgrowth of a fungal organism — usually C. albicans — in your vagina. C. albicans also causes infections in other moist areas of your body, such as in your mouth (thrush), skin folds and nail beds. The fungus can also cause diaper rash.
- Trichomoniasis – an sexually transmitted infection (STI) caused by a tiny parasite (Trichomonas vaginalis). This common sexually transmitted infection is caused by a microscopic, one-celled parasite called Trichomonas vaginalis. This organism spreads during sexual intercourse with someone who has the infection. In men, the organism usually infects the urinary tract, but often it causes no symptoms. In women, trichomoniasis typically infects the vagina, and might cause symptoms. It also increases a women’s risk of getting other sexually transmitted infections.
- Chemical irritation – for example, from perfumed soap, bubble bath, or fabric conditioner, or from spermicide (a chemical that kills sperm, sometimes used on condoms) and some sanitary products. Foreign objects, such as tissue paper or forgotten tampons, in the vagina can also irritate vaginal tissues.
- Washing inside your vagina
- Chlamydia – an sexually transmitted infection caused by bacteria
- Gonorrhoea – an sexually transmitted infection caused by bacteria
- Genital herpes – an sexually transmitted infection caused by the herpes simplex virus
- Atrophic vaginitis (genitourinary syndrome of menopause). Vaginal dryness, itching or discomfort (particularly during sex) can also sometimes be caused by a decrease in estrogen levels after the menopause. This is known as vaginal atrophy or atrophic vaginitis, and is due to the thinning of the vagina’s lining.
Table 1 describes common causes, symptoms, and signs of vaginitis and Table 2 lists risk factors that contribute to the development of the condition.
In a review of studies published between 1966 and 2003, bacterial vaginosis was diagnosed in 22 to 50 percent of symptomatic women, vulvovaginal candidiasis in 17 to 39 percent, and trichomoniasis in 4 to 35 percent 2. Approximately 30 percent of symptomatic women remained undiagnosed after clinical evaluation 3. Among multiple individual symptoms and signs, only the following were found to be helpful for the diagnosis of vaginitis in symptomatic women:
- A lack of itching makes diagnosis of vulvovaginal candidiasis unlikely.
- A lack of perceived odor makes bacterial vaginosis unlikely.
- Presence of inflammatory signs is more commonly associated with vulvovaginal candidiasis.
- Presence of a fishy odor on examination is predictive of bacterial vaginosis.
- Lack of odor is associated with vulvovaginal candidiasis.
Individual symptoms and signs, pH level, and microscopy results often do not lead to an accurate diagnosis of vaginitis. Laboratory tests perform better than standard office-based evaluation for diagnosing causes of vaginitis 3, but they do not add substantially to the treatment threshold and are justified only in patients with recurrent or difficult-to-diagnose symptoms.
Table 1. Causes, Symptoms, and Signs of Vaginitis
| Type | Etiology | Clinical symptoms | Clinical signs | |||
|---|---|---|---|---|---|---|
| Discharge | Pain | Pruritus | Vagina | Vulva | ||
Bacterial vaginosis | Gardnerella vaginalis, Mycoplasma hominis | Malodorous; homogenous; clear, white, or gray; fishy odor | Not primary symptom | Not primary symptom | No signs of inflammation | Unaffected |
Anaerobic bacteria: Prevotella species, Mobiluncus species | ||||||
Trichomoniasis | Trichomonas vaginalis | Green-yellow, frothy | Pain with sexual intercourse, vaginal soreness, dysuria | Not primary symptom | Signs of inflammation, “strawberry cervix” | Vestibular erythema may be present |
Vulvovaginal candidiasis | Candida albicans, Candida krusei, Candida glabrata | White, thick, lack of odor | Burning, dysuria, dyspareunia | Frequent | Signs of inflammation, edema | Excoriations |
Atrophic vaginitis | Estrogen deficiency | Yellow, greenish, lack of odor | Vaginal dryness, pain with sexual intercourse | Rare | Vagina mildly erythematous, easily traumatized | Vestibule thin and dry; labia majora lose their subcutaneous fat; labia minora irritated and friable |
Erosive lichen planus | Etiology is unknown | Yellow or gray | Intense pain, dyspareunia, postcoital bleeding | Intense | Erythema with friable epithelium | Erosions, white plaques |
Irritant or allergic contact dermatitis | Contact irritation or allergic reaction with episodic flares | Minimal | Burning on acute contact, soreness | More likely in allergic reactions | Vulvar erythema possible | Erythema with or without edema; vesicles or bullae rare |
[Source 2]
Risk factors for vaginitis
Factors that increase your risk of developing vaginitis include:
- Hormonal changes, such as those associated with pregnancy, birth control pills or menopause
- Sexual activity
- Having a sexually transmitted infection
- Medications, such as antibiotics and steroids
- Use of spermicides for birth control
- Uncontrolled diabetes
- Use of hygiene products such as bubble bath, vaginal spray or vaginal deodorant
- Douching
- Wearing damp or tightfitting clothing
- Using an intrauterine device (IUD) for birth control
Table 2. Risk Factors Contributing to Vaginitis
| Type of vaginitis | Risk factors |
|---|---|
Bacterial vaginosis | Low socioeconomic status, vaginal douching, smoking, use of an intrauterine contraceptive device, new/multiple sex partners, unprotected sexual intercourse, homosexual relationships, frequent use of higher doses of spermicide nonoxynol-9 |
Trichomoniasis | Low socioeconomic status, multiple sex partners, lifetime frequency of sexual activity, other sexually transmitted infections, lack of barrier contraceptive use, illicit drug use, smoking |
Vulvovaginal candidiasis | Vaginal or systemic antibiotic use, diet high in refined sugars, uncontrolled diabetes mellitus |
Atrophic vaginitis | Menopause, other conditions associated with estrogen deficiency, oophorectomy, radiation therapy, chemotherapy, immunologic disorders, premature ovarian failure, endocrine disorders, antiestrogen medication |
Irritant contact dermatitis | Soaps, tampons, contraceptive devices, sex toys, pessary, topical products, douching, fastidious cleansing, medications, clothing |
Allergic contact dermatitis | Sperm, douching, latex condoms or diaphragms, tampons, topical products, medications, clothing, atopic history |
Bacterial Vaginosis
Bacterial vaginosis is the most prevalent cause of vaginal discharge or malodor, occurring in up to 30 percent of women 4. It occurs when the normal Lactobacillus species in the vagina are replaced with anaerobic bacteria, resulting in reduced levels of hydrogen peroxide and organic acids usually present in the vagina.
The underlying cause of bacterial vaginosis is not fully understood. More than 50 percent of women with bacterial vaginosis are asymptomatic. The fishy odor caused by production of amines from anaerobic bacteria found in many of these patients is predictive of bacterial vaginosis 3. When vaginal alkalinity increases after sexual intercourse (with the presence of semen) and during menses (with the presence of blood), the odor becomes more prevalent 5. Vaginal discharge is a more common but less specific symptom. Bacterial vaginosis is not associated with vaginal mucosal inflammation and rarely causes vulvar itch 5.
Bacterial vaginosis, even when asymptomatic, is associated with a high incidence of endometritis and pelvic inflammatory disease following abortion and gynecologic procedures in the general population. Among women with bacterial vaginosis, no overall increased risk of developing pelvic inflammatory disease has been found 6. Bacterial vaginosis is associated with late miscarriages, premature rupture of membranes, and preterm birth 7. Both symptomatic and asymptomatic bacterial vaginosis have been strongly linked with an increased risk of human immunodeficiency virus (HIV)-1 transmission 8.
Bacterial vaginosis in pregnancy
Bacterial vaginosis is present in up to 20 percent of women during pregnancy. The effect of treating bacterial vaginosis in symptomatic or asymptomatic pregnant women on subsequent preterm delivery has produced conflicting results in clinical trials 9. The U.S. Preventive Services Task Force (USPSTF) recommends against routine bacterial vaginosis screening of asymptomatic pregnant women at low risk of preterm delivery (USPSTF grade D recommendation) 10.
Recurrent bacterial vaginosis
Most relapses of bacterial vaginosis occur within the first year and strongly correlate with new sex partners. Reported recurrence rates are 15 to 30 percent within three months.37,38 One RCT on persistent bacterial vaginosis indicated that metronidazole gel 0.75% (Metrogel), used twice weekly for six months after initial treatment, effectively maintained a clinical cure for six months.39
Bacterial vaginosis diagnosis
In clinical practice, bacterial vaginosis is diagnosed by the presence of three out of four Amsel criteria 11:
- Thin, homogenous vaginal discharge
- Vaginal pH greater than 4.5
- Positive whiff test (fishy amine odor when 10 percent potassium hydroxide solution is added)
- At least 20 percent clue cells (vaginal epithelial cells with borders obscured by adherent coccobacilli on wet-mount preparation or Gram stain).
In a prospective observational study of 269 women, a vaginal pH of more than 4.5 was found to be the most sensitive (89 percent) and a positive whiff test was the most specific (93 percent) method of detecting bacterial vaginosis 12. The positive presence of these two tests is as sensitive as three or more Amsel criteria. 12. Culture of Gardnerella vaginalis is not recommended because of low specificity. Cervical cytology has no clinical value for diagnosing bacterial vaginosis, especially in asymptomatic women, because it has low sensitivity 13.
Trichomoniasis
Symptoms and signs of trichomoniasis are not specific, and diagnosis by microscopy is more reliable. Features suggestive of trichomoniasis are trichomonads seen with saline, leukocytes more numerous than epithelial cells, positive whiff test, and vaginal pH greater than 5.4 3. The wet-mount preparation is an inexpensive and quick test with variable sensitivity of 58 to 82 percent 14 and is influenced by the experience of the examiner and the number of parasites in the vaginal fluid sample. Adding examination of the spun urine specimen can increase the detection rate of Trichomonas vaginalis from 73 to 85 percent 15.
Trichomoniasis in pregnancy
A Cochrane review found that metronidazole is effective against trichomoniasis when taken by women and their partners during pregnancy. A trial of women treated before 23 weeks of gestation was stopped early because women taking metronidazole were more likely to give birth preterm and have low-birth-weight infants 16. The Centers for Disease Control and Prevention (CDC) (Table 4. Centers for Disease Control and Prevention Recommended Treatment of Vaginitis) recommends giving 2 g of metronidazole as a single dose, preferably after 37 weeks of gestation, and counseling patients about the potential risks and benefits of treatment.
Trichomoniasis Treatment
Almost any nitroimidazole drug given orally in a single dose or over a longer period results in parasitologic cure in 90 percent of cases 17. A single 2-g dose of metronidazole is adequate but can cause dyspepsia and metallic taste; compliant patients may prefer a longer regimen at a lower daily dosage with fewer adverse effects. Metronidazole in a dosage of 500 mg twice daily for seven days will treat bacterial vaginosis and trichomoniasis. Metronidazole in a dosage of 2 to 4 g daily for seven to 14 days is recommended for metronidazole-resistant strains.
The parasitologic cure rate of intravaginal nitroimidazole creams is an unacceptably low 50 percent. In randomized controlled trials, combined oral and intravaginal treatments have been more effective than oral treatment alone. Sex partners should be treated simultaneously 17. To reduce recurrence, partners should avoid resuming sexual intercourse until both have completed treatment and are asymptomatic. Your doctor may test you again in three months to see if you have been infected again.
Candidal vaginitis
An estimated 75 percent of women will have at least one episode of vulvovaginal candidiasis, and 40 to 45 percent will have two or more 18. Changes in the host vaginal environment precipitate and induce pathologic effects of the organism 19. Several risk factors for vulvovaginal candidiasis are listed in Table 2.
Candidal vaginitis diagnosis
Although symptoms of vulvovaginal candidiasis such as pruritus, vaginal soreness, dyspareunia, and vaginal discharge are common, none of them are specific 3. Most patients can be diagnosed by microscopic examination of vaginal secretions with a 10% potassium hydroxide solution (sensitivity, 65 to 85 percent). Vaginal pH is usually normal (4.0 to 4.5). Vaginal culture should be considered in recurrently symptomatic women with negative microscopy and a normal pH. The Pap smear, although specific, is insensitive, with positive results in only about 25 percent of patients with culture-positive symptomatic vulvovaginal candidiasis 19. A rapid yeast detection test (Savyon Diagnostics) can be performed by the patient and costs less than $10, compared with a mean of $65 for the yeast culture 20. Polymerase chain reaction testing is considered the most sensitive method, but is very expensive.
Candidal vaginitis treatment
On the basis of clinical presentation, microbiology, host factors, and response to therapy, vulvovaginal candidiasis can be classified as uncomplicated or complicated. Patients with uncomplicated vulvovaginal candidiasis are not pregnant, are otherwise healthy, and have all of the following:
- Mild to moderate disease
- Fewer than four episodes of candidiasis per year
- Pseudohyphae or hyphae visible on microscopy.
Treatment of uncomplicated vulvovaginal candidiasis involves a short course of antifungals (Table 5) 21; oral and topical preparations are similarly effective.
Patients with complicated vulvovaginal candidiasis have one or more of the following:
- Moderate to severe disease
- Four or more episodes of candidiasis per year
- Only budding yeast visible on microscopy
- Adverse host factors (e.g., pregnancy, diabetes mellitus, immunocompromise).
Treatment of complicated vulvovaginal candidiasis involves an intensive, longer course of antifungals (Table 5).
Vaginitis prevention
Good hygiene may prevent some types of vaginitis from recurring and may relieve some symptoms:
- Avoid baths, hot tubs and whirlpool spas.
- Avoid irritants. These include scented tampons, pads, douches and scented soaps. Rinse soap from your outer genital area after a shower, and dry the area well to prevent irritation. Don’t use harsh soaps, such as those with deodorant or antibacterial action, or bubble bath.
- Wipe from front to back after using the toilet. Doing so avoids spreading fecal bacteria to your vagina.
Other things you can do that may help prevent vaginitis include:
- Don’t douche. Your vagina doesn’t require cleansing other than normal bathing. Repetitive douching disrupts the normal organisms that reside in the vagina and can actually increase your risk of vaginal infection. Douching won’t clear up a vaginal infection.
- Use a latex condom. Both male and female latex condoms may help you avoid infections spread by sexual contact.
- Wear cotton underwear. Also wear pantyhose with a cotton crotch. If you feel comfortable without it, skip wearing underwear to bed. Yeast thrives in moist environments.
Vaginitis diagnosis
To diagnose vaginitis, your doctor is likely to:
- Review your medical history. This includes your history of vaginal or sexually transmitted infections.
- Perform a pelvic exam. During the pelvic exam, your doctor may use an instrument (speculum) to look inside your vagina for inflammation and abnormal discharge.
- Collect a sample for lab testing. Your doctor might collect a sample of cervical or vaginal discharge for lab testing to confirm what kind of vaginitis you have.
- Perform pH testing. Your doctor might test your vaginal pH by applying a pH test stick or pH paper to the wall of your vagina. An elevated pH can indicate either bacteria vaginosis or trichomoniasis. However, pH testing alone is not a reliable diagnostic test.
Table 3 describes laboratory tests used to diagnose infectious causes of vaginitis.
Table 3. Laboratory Testing for Infectious Causes of Vaginitis
| Test | Bacterial vaginosis | Trichomoniasis | Vulvovaginal candidiasis | Cost* |
|---|---|---|---|---|
Point-of-care tests* | ||||
Amsel criteria | Sensitivity, 69%; specificity, 93% | NA | NA | $$ |
pH | pH > 5: sensitivity, 77%; specificity, 35% | pH > 5.4: sensitivity, 92%; specificity, 51% | pH < 4.9: sensitivity, 71%; specificity, 90% | $ |
Whiff test (the amine odor produced by mixing 10% potassium hydroxide solution with a sample of vaginal discharge) | Positive test: sensitivity, 67%; specificity, 93% | Positive test: sensitivity, 67%; specificity, 65% | Negative test | $ |
Fem Exam card (Cooper Surgical, Shelton, Conn.) Two colorimetric strips: card 1 measures pH and amine levels; card 2 measures proline aminopeptidase activity | Cards 1 and 2 combined: sensitivity, 91%; specificity, 61% | NA | NA | $$ |
Rapid (two minutes), less subjective than whiff test, easily performed | ||||
Microscopy (with 10% potassium hydroxide solution, saline) | Clue cells, bacilli with corkscrew motility, scant or absent lactobacilli | Motile protozoa with flagella; more leukocytes than epithelial cells | Budding filaments, mycelia with 10% potassium hydroxide solution | $ |
Sensitivity, 53 to 90%; specificity, 40 to 100% | Sensitivity, 50 to 70% (may be increased by vaginal lavage to 74%); specificity, 100% | Sensitivity, 61%; specificity, 77% | ||
pH, trimethylamine card (QuickVue Advance Quidel, San Diego, Calif.) | Sensitivity, 53%; specificity, 97% | NA | NA | $ |
Rapid, simple, comparable with pH and whiff test | ||||
Proline aminopeptidase card (Pip Activity TestCard, Litmus Concepts, Inc., Santa Clara, Calif.) Indirect test for a chemical produced by the organisms associated with bacterial vaginosis | Sensitivity, 70%; specificity, 81% | NA | NA | $ |
Rapid, simple, comparable with Fem Exam card 2 | ||||
OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Mass.), uses color immunochromatographic “dipstick” technology with murine monoclonal antibodies | NA | Sensitivity, 90 to 100% 10 minutes to complete test | NA | $$$ |
BD Affirm VPIII Microbial Identification Test (BD Diagnostic Systems, Sparks, Md.) | Sensitivity, 95 to 100% 45 minutes to complete test | Sensitivity, 90 to 100% | Sensitivity, 90 to 100% | $$$ |
False-positive results may occur, especially in low-prevalence groups | ||||
Polymerase chain reaction: based on DNA amplification (Quest Diagnostics, Madison N.J.), Instagene Matrix (Bio-Rad Laboratories, Hercules, Calif.) | Effective at identifying bacteria responsible for bacterial vaginosis | Sensitivity, 80%; specificity, 97% | Polymerase chain reaction more sensitive than culture in detecting Candida; not yet commercially available as a diagnostic test | $$$ |
Reference laboratory testing* | ||||
Culture | Predictive value of a positive Gardnerella vaginalis culture is less than 50%; generally not recommended, but may have value in recalcitrant cases | InPouch Culture System (Biomed, White City, Ore.) | Positive culture alone does not necessarily indicate that the yeast identified are responsible for vaginal symptoms | $$$ |
Combined wet-mount preparation and culture kit; can be kept at room temperature for up to 18 hours; samples taken during menses were not adversely affected | ||||
Sensitivity, 81 to 100% | ||||
Patient-performed tests | ||||
Over-the-counter test for vaginal infections (Fem-V; Synova Healthcare, Inc., New York, NY) | Positive test suggests possibility of bacterial vaginosis and need for physician visit (20% false-positive rate) | Positive test suggests possibility of trichomoniasis and need for physician visit (20% false-positive rate) | Negative test suggests possibility of yeast infection | $ |
Over-the-counter antifungal treatment recommended (10% false-negative rate) | ||||
Over-the-counter rapid yeast detection test (Savyon Diagnostics, Ashdod, Israel): uses the concept of lateral flow immunoassay systems | NA | NA | Positive test: sensitivity, 73%; specificity, 84% | $ |
Patient-performed tests have results similar to physician-performed tests | ||||
Negative test: not sensitive enough to rule out yeast infection and avoid a culture | ||||
NA = not applicable.
*—Relative cost of testing does not include physician office charges.
Vaginitis treatment
Treatment for vaginitis depends on what’s causing it.
A variety of organisms and conditions can cause vaginitis, so treatment targets the specific cause:
- Bacterial vaginosis. For this type of vaginitis, your doctor may prescribe metronidazole (Flagyl) tablets that you take by mouth or metronidazole (MetroGel) gel or clindamycin (Cleocin) cream that you apply to your vagina. You’ll need to get tested and be given a prescription for these medications.
- Candidal vaginitis or yeast infections. Yeast infections usually are treated with an over-the-counter antifungal cream or suppository, such as miconazole (Monistat 1), clotrimazole (Gyne-Lotrimin), butoconazole (Femstat 3) or tioconazole (Vagistat-1). Yeast infections may also be treated with a prescription oral antifungal medication, such as fluconazole (Diflucan). The advantages of over-the-counter treatment are convenience, cost and not waiting to see your doctor. However, you might have something other than a yeast infection. Using the wrong medicine may delay an accurate diagnosis and proper treatment.
- Trichomoniasis. Your doctor may prescribe metronidazole (Flagyl) or tinidazole (Tindamax) tablets.
- Atrophic vaginitis (genitourinary syndrome of menopause). Estrogen in the form of vaginal creams, tablets or rings — can effectively treat this condition. This treatment is available by prescription from your doctor, after other risk factors and possible complications are reviewed.
- Noninfectious vaginitis. To treat this type of vaginitis, you need to pinpoint the source of the irritation and avoid it. Possible sources include new soap, laundry detergent, sanitary napkins or tampons.
You’ll need prescription medication to treat trichomoniasis, bacterial vaginosis and vaginal atrophy.
If you know you have a candidal vaginitis (yeast infection), you can take these steps:
- Use an over-the-counter medication specifically for yeast infections. Options include one-day, three-day or seven-day courses of cream or vaginal suppositories. The active ingredient varies, depending on the product: clotrimazole (Gyne-Lotrimin), miconazole (Monistat 1) or tioconazole (Vagistat-1). Some products also come with an external cream to apply to the labia and opening of the vagina. Follow package directions and complete the entire course of treatment, even if you’re feeling better right away.
- Apply a cold compress, such as a washcloth, to the labial area to ease discomfort until the antifungal medication takes full effect.
Treatment of Noninfectious Causes of Vaginitis
Irritant contact dermatitis and allergic contact dermatitis are two noninfectious causes of vaginitis. They may be associated with use of feminine hygiene products or contraceptive materials, among many other causes. Atrophic vaginitis can manifest clinically with symptoms of vaginal dryness, itching, discharge, irritation, and dyspareunia. It affects 10 to 40 percent of women who have conditions associated with estrogen deficiency 22. Diagnosis is based on history and physical findings, supplemented by vaginal pH levels, vaginal wet-mount preparation (to exclude superimposed infection), and, rarely, culture or cytology. Both systemic and topical estrogen treatments are effective in relieving symptoms. Topical vaginal estrogen is preferred because of the low systemic absorption and reduced risk of adverse effects compared with oral therapy. Estrogen-containing creams, pessaries, intravaginal tablets, and the estradiol vaginal ring appear equally effective for the symptoms of atrophic vaginitis 23.
Self care
To help improve your vaginitis you should:
- keep your genital area clean and dry – take a warm bath rather than a hot one and use unperfumed soap to clean your genital area (the vagina cleans itself with natural secretions); dry yourself thoroughly
- avoid douching (spraying water inside your vagina) – it may make your vaginitis symptoms worse by removing the healthy bacteria that line the vagina and help keep it free from infection
- not use feminine hygiene products – such as sprays, deodorants or powders
- use pads rather than tampons if you’re using intravaginal creams or pessaries to treat an infection – tampons may ‘soak up’ the treatment meaning there’s less available in the vagina
- wear loose-fitting cotton underwear – this may be beneficial if you have external soreness, but it won’t prevent getting vaginitis in the future
Having sex
You should also practice safe sex by using condoms to avoid getting or spreading sexually transmitted infections (STIs).
If you have mild to moderate vaginitis, using a lubricant can help relieve pain and discomfort while having sex. Lubricants provide short-term symptom relief and can improve vaginal dryness during sex, but there’s no evidence to show they’re an effective long-term treatment.
Several types of lubricant are available – some are water-based and some are silicone-based. You may need to try a few before finding one that’s suitable. Ask your doctor or pharmacist if you need further advice.
Vaginal atrophy
Hormone replacement therapy (HRT) may be recommended if you have vaginitis that’s caused by vaginal atrophy (thinning of the lining of the vagina after the menopause). Hormone replacement therapy (HRT) replaces the female hormones, estrogen and progesterone.
Creams, pessaries or vaginal tablets that contain estrogen are also available. Unlike HRT, they only restore estrogen to your vagina rather than to your whole body, reducing the risk of side effects.
Antibiotics for vaginitis
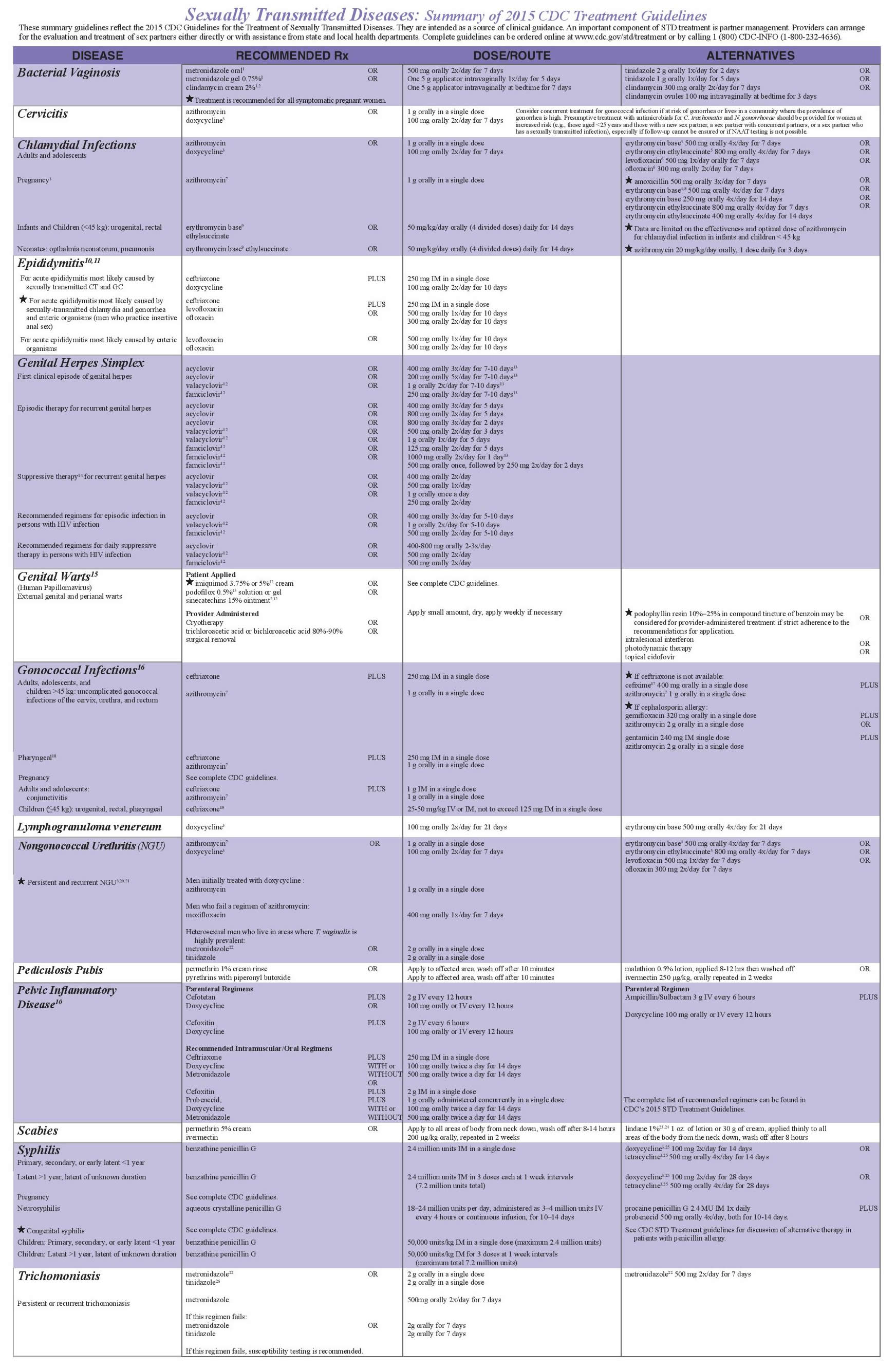
Current treatment recommendations from the Centers for Disease Control and Prevention (CDC) are listed in Table 4. Nonpregnant and pregnant women with symptomatic disease require antibacterial therapy to relieve vaginal symptoms. Other benefits of treatment include decreasing the risk of HIV and other sexually transmitted infections and reducing infectious complications following abortion or hysterectomy 24.
Table 4. Centers for Disease Control and Prevention Recommended Treatment of Vaginitis
[Source 24]A Cochrane review of 24 randomized controlled trials showed that clindamycin and metronidazole (Flagyl) are equally effective, achieving clinical cure in 91 and 92 percent of cases, respectively, after two to three weeks of treatment 25. Six randomized controlled trials showed topical and oral antibiotic preparations to be equally effective. One disadvantage of oral regimens is a longer duration of treatment 25. Intravaginal clindamycin cream is preferred in case of allergy or intolerance to metronidazole. Metronidazole in a single 2-g dose has the lowest effectiveness for treating bacterial vaginosis and is no longer recommended. Metronidazole, 500 mg twice daily for one week, is effective for treating bacterial vaginosis and trichomoniasis.
Although lactobacillus probiotics are safe, there is no conclusive evidence that they are superior to or enhance the effectiveness of antibiotics in the treatment of bacterial vaginosis or prevent its recurrence 26. Treatment of sex partners and follow-up visits if symptoms are resolved are not recommended.
Table 5. Treatment of Candidal Vaginitis
| Vulvovaginal candidiasis, uncomplicated | ||||
| Butoconazole 2% cream (Gynazole-1)† | $$ | |||
| 5 g intravaginally once daily for three days | ||||
| Butoconazole 2% cream, sustained release | $ | |||
| 5 g intravaginally in a single dose | ||||
| Clotrimazole 1% cream† | $ | |||
| 5 g intravaginally once daily for seven to 14 days | ||||
| Clotrimazole 2% cream† | $ | |||
| 5 g intravaginally once daily for three days | ||||
| Miconazole 2% cream† | $ | |||
| 5 g intravaginally once daily for seven days | ||||
| Miconazole 4% cream† | $ | |||
| 5 g intravaginally once daily for three days | ||||
| Miconazole vaginal suppository† | ||||
| 100-mg vaginal suppository once daily for seven days | $ | |||
| 200-mg vaginal suppository once daily for three days | $$ | |||
| 1,200-mg vaginal suppository in a single dose | $$ | |||
| Nystatin vaginal tablet | $ | |||
| 100,000-unit vaginal tablet once daily for 14 days | ||||
| Tioconazole 6.5% ointment† | $$ | |||
| 5 g intravaginally in a single dose | ||||
| Terconazole 0.4% cream | $$ | |||
| 5 g intravaginally once daily for seven days | ||||
| Terconazole 0.8% cream | $$ | |||
| 5 g intravaginally once daily for three days | ||||
| Terconazole vaginal suppository | $$ | |||
| 80-mg vaginal suppository once daily for three days | ||||
| Fluconazole (Diflucan) | $$ | |||
| 150 mg orally in a single dose | ||||
| Vulvovaginal candidiasis, complicated | ||||
| Recurrent | ||||
| Initial regimen | ||||
| Any topical agent | ||||
| Seven to 14 days | ||||
| Fluconazole | $$$ | |||
| 100, 150, or 200 mg orally once daily every third day for three doses | ||||
| Maintenance regimen | ||||
| Fluconazole | $$$ | |||
| 100, 150, or 200 mg orally once weekly for six months | ||||
| Severe | ||||
| Any topical azole | $$ | |||
| Intravaginally once daily for seven to 14 days | ||||
| Fluconazole | $$$ | |||
| 150 mg orally once daily in two doses 72 hours apart | ||||
| Vulvovaginal candidiasis, nonalbicans | ||||
| Nonfluconazole azole (oral or topical) | $ | |||
| Seven to 14 days | ||||
| Boric acid gelatin capsule | $$ | |||
| Intravaginally once daily for 14 days | ||||
| Pregnancy* | ||||
| Any topical azole | $$ | |||
| Intravaginally once daily for seven days | ||||
- Vaginitis: Diagnosis and Treatment. Am Fam Physician. 2018 Mar 1;97(5):321-329. https://www.aafp.org/afp/2018/0301/p321.html
- Vaginitis: Diagnosis and Treatment. Am Fam Physician. 2011 Apr 1;83(7):807-815. https://www.aafp.org/afp/2011/0401/p807.html
- Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291(11):1368–1379.
- Allsworth JE, Peipert JF. Prevalance of bacterial vagniosis: 2001–2004 National Health and Nutrition Examination Survey data. Obstet Gynecol. 2007;109(1):114–120.
- Livengood CH III, Thomason JL, Hill GB. Bacterial vaginosis: diagnostic and pathogenetic findings during topical clindamycin therapy. Am J Obstet Gynecol. 1990;163(2):515–520.
- Ness RB, Hillier SL, Kip KE, et al. Bacterial vaginosis and risk of pelvic inflammatory disease. Obstet Gynecol. 2004;104(4):761–769.
- Leitich H, Bodner-Adler B, Brunbauer M, Kaider A, Egarter C, Husslein P. Bacterial vaginosis as a risk factor for preterm delivery: a meta-analysis. Am J Obstet Gynecol. 2003;189(1):139–147.
- Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis. 1999;180(6):1863–1868.
- McDonald HM, Brocklehurst P, Gordon A. Antibiotics for treating bacterial vaginosis in pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000262.
- U.S. Preventive Services Task Force. Screening for bacterial vaginosis in pregnancy to prevent preterm delivery: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;148(3):214–219. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/bacterial-vaginosis-in-pregnancy-to-prevent-preterm-delivery-screening
- Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983;74(1):14–22.
- Gutman RE, Peipert JF, Weitzen S, Blume J. Evaluation of clinical methods for diagnosing bacterial vaginosis. Obstet Gynecol. 2005;105(3):551–556.
- Sexually Transmitted Diseases (STDs). https://www.cdc.gov/std/
- Wiese W, Patel SR, Patel SC, Ohl CA, Estrada CA. A meta-analysis of the Papanicolaou smear and wet mount for the diagnosis of vaginal trichomoniasis. Am J Med. 2000;108(4):301–308.
- Blake DR, Duggan A, Joffe A. Use of spun urine to enhance detection of Trichomonas vaginalis in adolescent women. Arch Pediatr Adolesc Med. 1999;153(12):1222–1225.
- Gülmezoglu AM. Interventions for trichomoniasis in pregnancy. Cochrane Database Syst Rev. 2002;(3):CD000220.
- Forna F, Gülmezoglu AM. Interventions for treating trichomoniasis in women. Cochrane Database Syst Rev. 2003;(2):CD000218.
- Corsello S, Spinillo A, Osnengo G, et al. An epidemiological survey of vulvovaginal candidiasis in Italy. Eur J Obstet Gynecol Reprod Biol. 2003;110(1):66–72.
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369(9577):1961–1971.
- Chatwani AJ, Mehta R, Hassan S, Rahimi S, Jeronis S, Dandolu V. Rapid testing for vaginal yeast detection: a prospective study. Am J Obstet Gynecol. 2007;196(4):309.e1–4.
- Nurbhai M, Grimshaw J, Watson M, Bond C, Mollison J, Ludbrook A. Oral versus intra-vaginal imidazole and triazole anti-fungal treatment of uncomplicated vulvovaginal candidiasis (thrush). Cochrane Database Syst Rev. 2007;(4):CD002845.
- Greendale GA, Judd HL. The menopause: health implications and clinical management. J Am Geriatr Soc. 1993;41(4):426–436.
- Suckling JA, Lethaby A, Kennedy R. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2006; (4):CD001500.
- 2015 Sexually Transmitted Diseases Treatment Guidelines. https://www.cdc.gov/std/tg2015/default.htm
- Oduyebo OO, Anorlu RI, Ogunsola FT. The effects of antimicrobial therapy on bacterial vaginosis in non-pregnant women. Cochrane Database Syst Rev. 2009;(3):CD006055.
- Senok AC, Verstraelen H, Temmerman M, Botta GA. Probiotics for the treatment of bacterial vaginosis. Cochrane Database Syst Rev. 2009; (4):CD006289.