What is a laryngectomy
Laryngectomy is a major surgery to remove part or all of the larynx (voice box), usually done for advanced laryngeal cancer. Laryngectomy is done in the hospital under general anesthesia. You will be asleep and pain-free. During a laryngectomy, the surgeon will first create a new passage for breathing: a tracheostomy tube from your windpipe that opens out at the neck, the breathing opening is called a stoma. The surgeon will then remove the larynx (or part of the larynx), and close the passage to ensure that food does not go down the windpipe. A small opening will be made to allow air to travel from the esophagus, or gullet, to the windpipe. With practice, many people who have had a laryngectomy can learn to speak using their esophagus.
You might or might not require a tracheotomy and/or feeding tube, depending on the extent of the laryngectomy and reconstruction.
Most often, laryngectomy is done to treat cancer of the larynx. Laryngectomy is also done to treat:
- Severe trauma, such as a gunshot wound or other injury.
- Severe damage to the larynx from radiation treatment. This is called radiation necrosis.
Partial laryngectomy. Smaller cancers of the larynx often can be treated by removing only part of the voice box. There are different types of partial laryngectomies, but they all have the same goal: to take out all of the cancer while leaving behind as much of the larynx as possible.
In a supraglottic laryngectomy, only the part of your larynx above the vocal cords is removed. Supraglottic laryngectomy procedure can be used to treat some supraglottic cancers, and will allow you to speak normally afterward.
For small cancers of the vocal cords, the surgeon may be able to remove the cancer by taking out only one side of the larynx (one vocal cord) and leaving the other behind. This is called a hemilaryngectomy. Some speech remains after this surgery.
Total laryngectomy removes the whole larynx. Part of your pharynx may be taken out as well (pharyngectomy). Your pharynx is the mucous membrane-lined passage between your nasal passages and esophagus. In total laryngectomy procedure, your entire larynx is removed. The trachea (windpipe) is then brought up through the skin of the front of your neck as a stoma (or hole) that you breathe through (see the picture below). This is called a tracheostomy. When the entire larynx is removed, you can no longer speak normally, but you can learn other ways of speaking. The connection between the throat and the esophagus (swallowing tube) is usually not affected, so you can swallow food and liquids just as you did before the operation.
- The surgeon will make a cut in your neck to open up the area. Care is taken to preserve major blood vessels and other important structures.
- The larynx and tissue around it will be removed. The lymph nodes may also be removed.
- The surgeon will then make an opening in your trachea and a hole in front of your neck. Your trachea will be attached to this hole. The hole is called a stoma. After surgery you will breathe through your stoma. It will never be removed.
- Your esophagus, muscles, and skin will be closed with stitches or clips. You may have tubes coming from your wound for a while after surgery.
The surgeon may also do a tracheoesophaheal puncture (TEP).
- A TEP laryngectomy is a small hole in your windpipe (trachea) and the tube that moves food from your throat to your stomach (esophagus).
- Your surgeon will place a small man-made part (prosthesis) into this opening. The prosthesis will allow you to speak after your voice box has been removed.
There are many less invasive surgeries to remove part of the larynx.
- The names of some of these procedures are endoscopic (or transoral resection), vertical partial laryngectomy, horizontal or supraglottic partial laryngectomy, and supracricoid partial laryngectomy.
- These procedures may work for some people. The surgery you have depends on how much your cancer has spread and what type of cancer you have.
The surgery can take 5 to 9 hours.
Figure 1. Partial laryngectomy
Figure 2. Total laryngectomy
Figure 3. Laryngectomy stoma
Figure 4. Laryngectomy tube
Before the laryngectomy procedure
You will have medical visits and tests before you have surgery. Some of these are:
- A complete physical exam and blood tests. Imaging studies may be performed.
- A visit with a speech therapist and a swallowing therapist to prepare for changes after surgery.
- Nutritional counseling.
- Stop-smoking – counseling. If you are a smoker and have not quit.
Always tell your health care provider:
- If you are or could be pregnant
- What medicines you are taking, even drugs, supplements, or herbs you bought without a prescription
- If you have been drinking a lot of alcohol, more than 1 or 2 drinks a day
During the days before your surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), clopidogrel (Plavix), warfarin (Coumadin), and any other drugs that make it hard for your blood to clot.
- Ask which drugs you should still take on the day of your surgery.
On the day of your surgery:
- You will be asked not to drink or eat anything after midnight the night before your surgery.
- Take the drugs your provider told you to take with a small sip of water.
- You will be told when to arrive at the hospital.
Laryngectomy vs Tracheostomy
A tracheostomy also known as a tracheotomy, is a surgical procedure to create an opening through the neck into the trachea (windpipe). A tracheostomy tube or trach tube is most often placed through this opening to provide an airway and to remove secretions from the lungs. General anesthesia is used, unless the situation is critical. If that happens, a numbing medicine is placed into the area to help you feel less pain during the procedure. Other medicines are also given to relax and calm you (if there is time).
The neck is cleaned and draped. Surgical cuts are made to reveal the tough cartilage rings that form the outer wall of the trachea. The surgeon creates an opening into the trachea and inserts a tracheostomy tube.
A tracheostomy may be done if you have:
- A large object blocking the airway
- An inability to breathe on your own
- An inherited abnormality of the larynx or trachea
- Breathed in harmful material such as smoke, steam, or other toxic gases that swell and block the airway
- Cancer of the neck, which can affect breathing by pressing on the airway
- Paralysis of the muscles that affect swallowing
- Severe neck or mouth injuries
- Surgery around the voice box (larynx) that prevents normal breathing and swallowing
A person may have a sense of panic and feel unable to breathe and speak when first waking up after the tracheostomy and placement of the tracheostomy tube. This feeling will lessen over time. Medicines may be given to help reduce the patient’s stress.
If the tracheostomy is temporary, the tube will eventually be removed. Healing will occur quickly, leaving a minimal scar. Sometimes, a surgical procedure may be needed to close the site (stoma).
Occasionally a stricture, or tightening of the trachea may develop, which may affect breathing.
If the tracheostomy tube is permanent, the hole remains open.
Most people need 1 to 3 days to adapt to breathing through a tracheostomy tube. It will take some time to learn how to communicate with others. At first, it may be impossible for the person to talk or make sounds.
After training and practice, most people can learn to talk with a tracheostomy tube. People or family members learn how to take care of the tracheostomy during the hospital stay. Home-care service may also be available.
You should be able to go back to your normal lifestyle. When you are outside, you can wear a loose covering (a scarf or other protection) over the tracheostomy stoma (hole). Use safety precautions when you are exposed to water, aerosols, powder, or food particles.
Laryngectomy procedure
The larynx, also called the voice box, has a number of functions. Its main function is a conduit for air to enter your lungs. Also, the larynx works to prevent food, liquids and saliva from falling into your lungs and causing pneumonia. Finally, the larynx is responsible for creating voice.
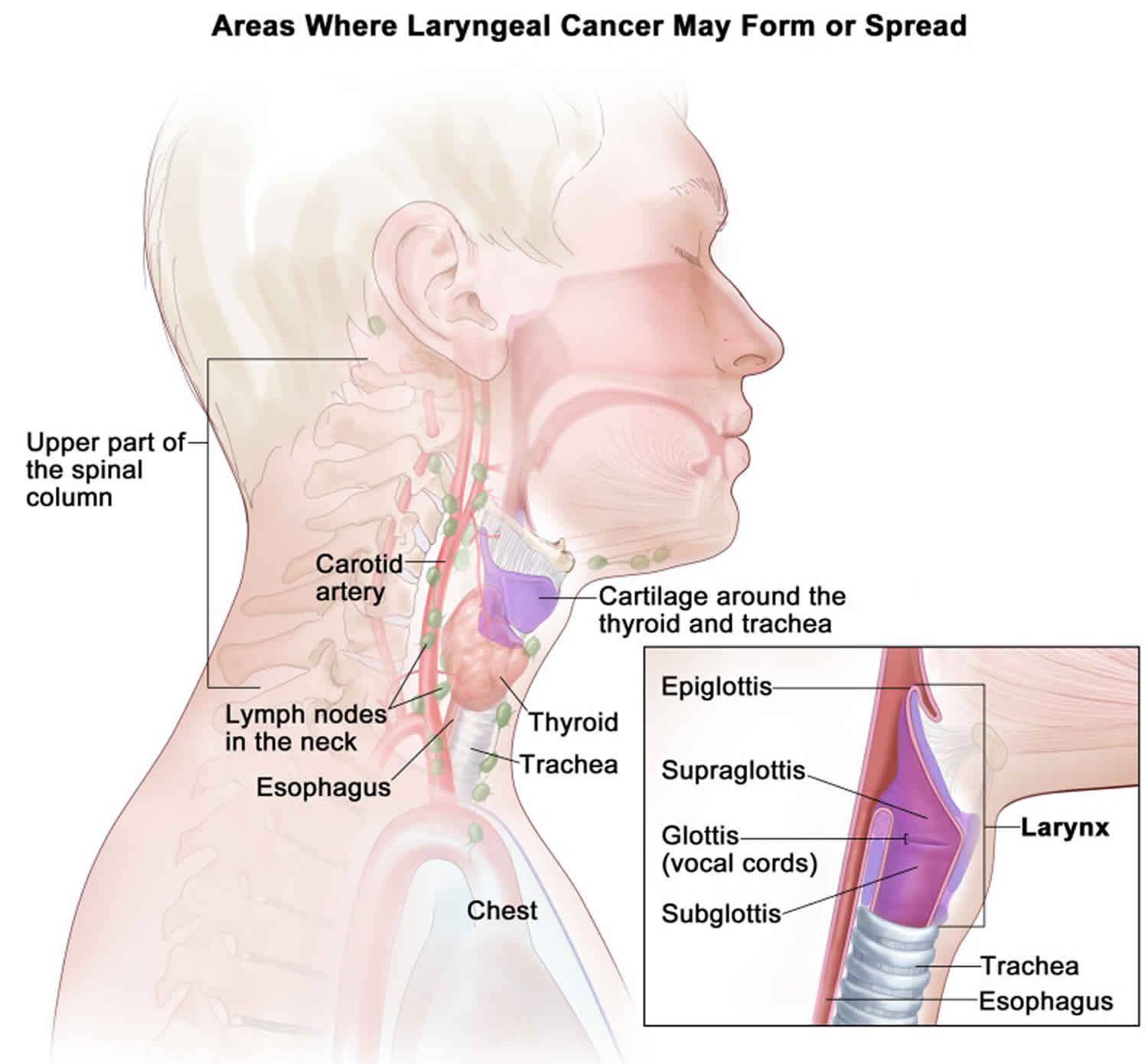
The larynx is part of the throat. It is located below the oropharynx and in front of the hypopharynx.
The anatomy of the voice box can get complicated for people (including doctors) who don’t deal with this area all the time. It is located in the middle of the neck, partly protected by the thyroid cartilage (which you can feel in your neck as the Adam’s Apple).
From a cancer perspective, the larynx is divided into three subsites: the supraglottis, glottis and subglottis. Cancer of the larynx starts in one of these subsites, but it can grow into another subsite.
- Supraglottis: This part of the voice box is above the vocal cords. Subsites of the supraglottis include the epiglottis above the hyoid bone, the epiglottis below the hyoid bone, the aryepiglottic folds, the arytenoids and the false vocal cords (also called the ventricular folds).
- Glottis: This part of the voice box is hidden behind the thyroid cartilage. It is responsible for producing your voice. It is made up of the true vocal cords. The anterior commisure refers to the location in the front of the larynx where the vocal cords meet.
- Subglottis: This part of the voice box extends from the bottom of the vocal cords to one centimeter below where it joins with the trachea (or windpipe).
A laryngectomy is the removal of some or all of the voice box—partial versus total laryngectomy. There are a number of types of laryngectomies.
Total laryngectomy
Total laryngectomy involves removal of the entire voice box. This is done for four main reasons:
- A large larynx cancer that has not been previously treated and has eroded through cartilage and other structures.
- A recurrent cancer that came back after some sort of prior treatment, such as radiation with or without chemotherapy.
- Cancer resection of another site—such as the entire tongue base, or the hypopharynx—would lead to major aspiration pneumonia complications if the primary tumor was removed but the larynx was left in place.
- In cases in which there is no cancer, but the larynx is not performing its main function as a result of prior treatment for cancer. A laryngectomy might be performed for patients who cannot safely eat or drink. For example, if food and liquids fall into the lungs because of a non-functional larynx, patients might have their larynx removed in order to eat. Also, if the pharynx or esophagus is closed off as a result of prior treatment and the patient is unable to eat or drink, a laryngectomy (with pharyngectomy and subsequent reconstruction) might allow a patient to eat again.
For a total laryngectomy, the incision is placed in the central neck, extending quite far to the side in order to perform neck dissections on both sides. This will allow exposure to remove the voice box along with the lymph nodes in the neck, if required. As part of this surgery, one or both lobes of your thyroid gland will be removed. Your surgeon might send frozen section margins after the voice box is removed to confirm no cancer cells are left behind. The closure will then be performed and will include creation of a laryngostome. A laryngostome involves sewing the top part of the trachea directly to the skin. This makes you a “neck breather” because there is no longer a connection from your mouth/nose down into your lungs. However, your mouth does remain connected to your throat and esophagus down into your stomach to allow you to eat.
Associated procedures might include bilateral (both sides) neck dissections, hemi- or total thyroidectomy or partial or total pharyngectomy (see total laryngopharyngectomy). Reconstruction and rehabilitation procedures might include repair of the pharynx with primary closure, a pectoralis major muscle flap or a free flap.
In some cases, a tracheoesophageal puncture might be done at the same time as the total laryngectomy to assist with speech in the post-operative time period.
If you don’t already have a gastric feeding tube, you will have a feeding tube placed either through the nose, directly in the stomach or inserted through the tracheoesophageal puncture. You will start eating anywhere from a few days to one or two weeks after the procedure, depending on your surgeon’s preference and prior treatment you might have received.
At the end of the procedure, your surgeon will likely place a small drain coming out of your skin. This is to drain any blood and/or fluid that might accumulate in the space that is created by removing the larynx as well as any fat and lymph nodes from the neck dissection. When the time is right—one day to a few days—the drain will be removed by your surgical team. This takes only a few seconds, and you can think of it as removing a bandage. There will be a little discomfort, but it will go by quickly.
It is important to immediately check your calcium level post-operatively, because the blood supply to the parathyroid glands could become compromised after this surgery. By saving one half of the thyroid gland, it should protect two of the parathyroid glands.
After the larynx is removed, there are a number of ways to speak. Some possible techniques include a tracheoesophageal puncture, shown Figure 2 above, and esophageal speech or an electrolarynx, shown below.
Figure 5. Total laryngectomy electrolarynx
Figure 6. Total laryngectomy electrolarynx
Partial laryngectomy
In open partial laryngectomy your entire voice box is not removed. The main goals of partial laryngectomy procedure are to get rid of the cancer while avoiding a permanent breathing tube in the neck, preserving a suitable voice and maintaining your ability to swallow.
Today, open partial laryngectomies have less of an application than they did many years ago. Currently, an open partial laryngectomy is limited to small cancers that have recurred after prior non-surgical therapy. Transoral microsurgery is another option in these situations. You should speak with your doctor about the possibility of this being an option to treat your cancer. Your surgeon will probably speak to you about the possibility of converting to a total laryngectomy, depending on what is seen during the surgery or of the frozen section.
There are several types of open partial laryngectomies:
Laryngofissure with cordectomy
In laryngofissure with cordectomy procedure, an incision is made in the midline of your neck, over the area of the Adam’s apple. The thyroid cartilage is split vertically, and the inside of the voice box is revealed. This gives excellent exposure to a tumor on a vocal cord, which can be removed. The thyroid cartilage is then sealed and the incision is closed. In some cases, you might have a temporary stent placed in your voice box for a few weeks to prevent a scar band from forming. You might receive a temporary tracheotomy tube.
Figure 7. Partial laryngectomy with cordectomy
Horizontal laryngectomy
A horizontal partial laryngectomy can be either a supraglottic hemi-laryngectomy (removal of half the larynx above the vocal cords) or a supracricoid hemilaryngectomy (removal of half the larynx above the cricoid cartilage). This can be performed with or without resection of the hyoid bone. After resection, the cricoid cartilage is sewn back up to the hyoid bone or to the hyoid bone and epiglottis, depending on what remains after resection of the tumor.
Figure 8. Horizontal laryngectomy
Vertical hemi-laryngectomy or frontolateral vertical partial laryngectomy
In vertical hemi-laryngectomy, or frontolateral vertical partial laryngectomy procedure, an incision is made in the middle of your neck, exposing the thyroid cartilage. Then a vertical incision is made in the thyroid cartilage, and one entire vocal cord and arytenoid is removed. Up to 75% of the thyroid cartilage can be removed, and the resection can include a small part of the vocal cord on the other side as well. Reconstruction can be performed in various ways, including local flaps, staged procedures and/or free flaps.
Figure 9. Vertical partial laryngectomy
Transoral laser microsurgery with partial laryngectomy
This is a partial laryngectomy performed through the mouth using special laryngoscopes, instruments and lasers. While this is most commonly used for small cancers on the vocal cords themselves, some surgeons are comfortable performing this for larger tumors of the voice box. This remains an option for small recurrent cancers after non-surgical therapy.In this procedure, you are put completely to sleep with general anesthesia. In many cases you will require a tracheotomy, but not all the time. The voice box is exposed using special instruments. A laser is used to cut out the tumor, with the aim of getting a margin of normal tissue around it. Once it is removed, your surgeon will orient the tumor and have a pathologist examine the margins under a microscope as a frozen section. If the margins are all clear, the surgery can be considered complete, as now major reconstruction is required.Associated procedures might include a tracheotomy, feeding tube placement or a neck dissection—sometimes performed a few weeks later as a staged neck dissection.
Transoral robotic-assisted partial laryngectomy
Transoral robotic-assisted partial laryngectomy procedure simply uses a robot to get exposure and to remove a tumor of the larynx through the mouth. The principles are the same as transoral laser microsurgery with the exception that the instruments are different. This procedure remains experimental in most areas, but experience is building. The purpose is to limit incisions and limit dissection of neck contents. Associated procedures might include a tracheotomy, feeding tube placement or a neck dissection—sometimes performed a few weeks later as a staged neck dissection.
Laryngectomy recovery and aftercare
The recovery course will depend on the extent of the surgery and reconstruction. With some surgeries, you could go home after a few hours of observation in the recovery room. Others might require a stay in the hospital for one to two weeks. A stay longer than two weeks is usually due to some sort of post-operative complication that your doctors are working to improve.
If you do stay in the hospital for recovery, the recovery course can happen in a few different parts of the hospital. Your pathway might include trips to the recovery room, intensive care unit, step-down unit and a shared or private “floor” bed. As soon as possible and when the time is right for each step, you will progress from having your tubes and drains removed to being disconnected from the lines, and eventually getting up and out of bed. Asking for assistance to get out of bed to move around will help your recovery.
Once your doctors determine that you no longer need in-patient level care, you will be ready for discharge. The discharge planning process begins well before you are ready to leave the hospital. While some patients can go home from the hospital with or without visiting nurses or receiving home care, others might go to a rehabilitation or skilled nursing facility for a short while before going home. Your discharge planning team, which includes your doctors, social workers, nurses and physical therapists, along with you and your family, will determine the best place for you to go once you’re ready to leave the hospital.
Any additional reconstruction, cosmetic procedures or treatments are planned after discharge. This gives you time to recover from the initial surgery, get the pathology results of the surgery and make appropriate arrangements for the next steps.
After the laryngectomy procedure
You will need to stay in the hospital for several days after surgery.
After the laryngectomy procedure, you will be groggy and will not be able to speak. An oxygen mask will be on your laryngectomy stoma. It’s important to keep your head raised, rest a lot, and move your legs from time to time to improve blood flow. Keeping blood moving reduces your risk of getting a blood clot.
You can use warm compresses to reduce pain around your incisions. You will get pain medicine.
You will receive nutrition through an IV (a tube that goes into a vein) and tube feedings. Tube feedings are given through a tube that goes through your nose and into your esophagus (feeding tube).
You may be allowed to swallow food as soon as 2 to 3 days after surgery. However, it is more common to wait 5 to 7 days after your surgery to start eating through your mouth.
Your drain may be removed in 2 to 3 days. You will be taught how to care for your laryngectomy tube and laryngectomy stoma. You will learn how to safely shower. You must be careful not to let water enter through your laryngectomy stoma.
Speech rehabilitation with a speech therapist will help you relearn how to speak.
You will need to avoid heavy lifting or strenuous activity for about 6 weeks. You may slowly resume your normal, light activities.
Follow up with your doctor as you are told.
Laryngectomy rehabilitation
Depending on the treatment and treatment-related side effects, the ability to speak or eat may be compromised post-treatment. Working with a speech pathologist may improve a patient’s ability to speak.
Swallowing function can be impaired even several years after the completion of surgery, radiation therapy or chemoradiation therapy. Rehabilitation can include any of the following type of exercises: swallowing maneuvers, such as effortful swallow or Mendelsohn maneuver (prolonged swallow); range of motion exercises (e.g., jaw, tongue); tongue strengthening exercises; and tactile stimulation.
Depending on the changes that occurred to your anatomy post-treatment (e.g., decrease in size of muscles, surgical removal of structures), you may require voice rehabilitation. Between 34 to 70 percent of head and neck cancer survivors will develop a speech impairment. A wide variety of tools can be used as a part of voice rehabilitation. These range from the use of prosthetic devices to help with vocalization to surgical reconstruction.
In addition, pyschosocial rehabilitation should be considered; approximately 20 percent of patients had depression after the completion of therapy for head and neck cancer, and 28 percent had depression approximately 10 years after diagnosis and treatment. If the patient is experiencing anxiety, he or she may want to obtain group therapy or individualized counseling or psychotherapy.
Laryngectomy risks and complications
Risks for any surgery are:
- Allergic reactions to medicines
- Breathing problems
- Heart problems
- Excess swelling or bleeding
- Infection
- Infection
- Wound opens
- Wound heals poorly
- Damage to nearby structures
- Blood clots
- Reaction to anesthesia
Risks for laryngectomy surgery are:
- Hematoma (a buildup of blood outside the blood vessels). If there is severe bleeding after the procedure, your surgeon might need to quickly take you back to the operating room to stop the bleeding.
- Wound infection. Total laryngectomy is often done with both sided neck dissections, therefore, in theory, joining saliva and mucous with the sterile neck contents. Interestingly, infections of the neck are quite rare. Still, as with any surgical procedure, there is always risk of an infection after the surgery. This might require antibiotics and/or drainage of the infection.
- Salivary Fistula (tissue connections that form between the pharynx and the skin that are not normally there). This term is used to describe when saliva is leaking from the pharynx into the neck. The chances of this increase if you have had previous treatment including radiation and/or chemotherapy. This is because wound healing might be impaired in these cases. Typical treatment for this is to place a drain to divert the saliva away from critical structures in the neck and later to place packing into that diverted tract and let the body heal on its own. In some cases, an additional surgical procedure might be required to close the leak (such as a pectoralis major muscle flap).
- The stoma opening may become too small or tight. This is called stomal stenosis.
- Saliva leaking around the tracheoesophageal puncture (TEP) and prosthesis
- Damage to other areas of the esophagus or trachea
- Problems swallowing and eating
- Unable to speak—aphonia
- Hypocalcemia: Low calcium levels can occur post-operatively if all four parathyroid glands are either removed and not re-implanted (permanent hypocalcemia) or put into a state of shock by affecting their blood supply (temporary hypocalcemia). This is why calcium levels need to be closely monitored after a total laryngectomy (or total laryngopharyngectomy) and calcium replacement needs to be given as needed.
- Hypothyroidism: This can happen if both lobes of the thyroid gland are removed, if only one lobe is removed but the other lobe cannot make enough thyroid hormone to keep up with the body’s needs or regardless of how much thyroid is removed, but radiation treatment has affected the function of the thyroid gland. In any case, thyroid function can be measured with blood tests, and a once-daily pill can replace the function of the thyroid hormone.
- Blood clots: Patients who undergo major surgeries, especially patients who have cancer, are at an increased risk of developing blood clots in their legs (deep venous thrombosis). Sometimes these blood clots can travel through the veins and into the lungs, causing a pulmonary embolus. This can be a serious complication, causing problems with oxygenation of your blood. If such a problem occurs, you will likely require anticoagulation (blood-thinning) medication to prevent more clots from forming and ending up in your lungs. This blood-thinning medicine, though necessary to prevent more clots, might cause another complication, such as bleeding, especially immediately after surgery. This is why it is important for you to get out of bed early and move your legs. If you are not up and moving about, dynamic compression stockings should be used (these are like massage boots for your calves to keep the blood flowing). Also, you will probably be given a low dose of blood-thinning medication immediately after surgery to help prevent clots.
- Aspiration: This is impossible after a total laryngectomy because the trachea is sewn to the skin of the neck, so there is no connection between the mouth and the lungs to allow for aspiration. However, after any sort of partial laryngectomy, this is a major consideration. Having saliva and/or food and drink falling into your lungs can lead to pneumonia.
- Cancer comes back
Laryngectomy prognosis
Your wounds will take about 2 to 3 weeks to heal. You can expect full recovery in about a month. Many times, removal of the larynx will take out all the cancer or injured material. People learn how to change their lifestyle and live without their voice box. You may need other treatments, such as radiotherapy or chemotherapy.