What is liver failure ?
Liver failure means that your liver is losing or has lost all of its function. Acute liver failure is a life-threatening condition that demands urgent medical care because it can cause serious complications, including excessive bleeding and increasing pressure in the brain 1.
The first symptoms of liver failure are often:
- Nausea,
- Loss of appetite,
- Fatigue, and
- Diarrhea.
Because these symptoms can have any number of causes, it may be hard to tell that the liver is failing.
But as liver failure progresses, the symptoms become more serious. The patient may become confused and disoriented, and extremely sleepy. There is a risk of coma and death. Immediate treatment is needed. The medical team will try to save whatever part of the liver that still works. If this is not possible, the only option may be a liver transplant.
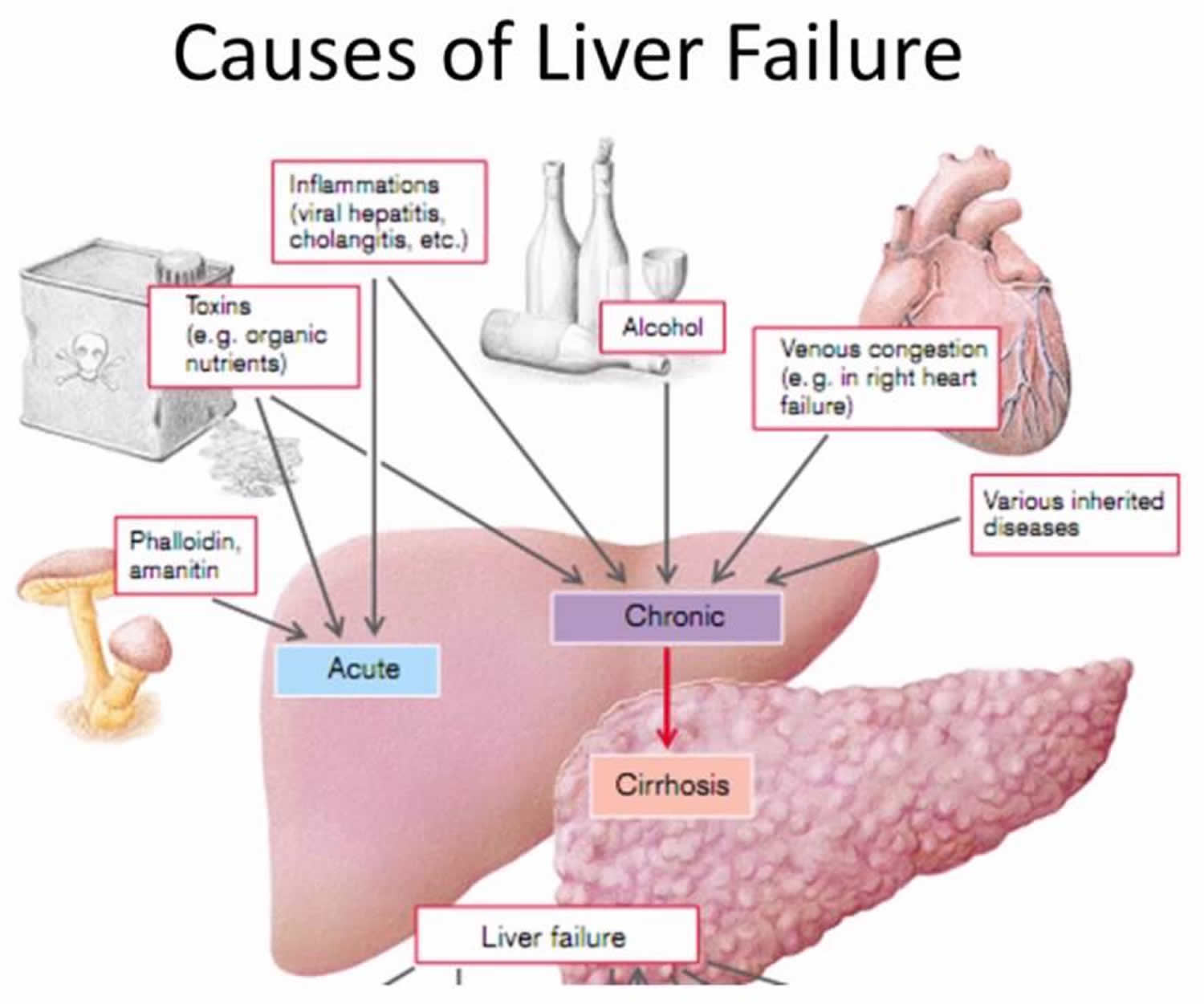
When liver failure occurs as a result of cirrhosis, it usually means that the liver has been failing gradually for some time, possibly for years. This is called chronic liver failure.
Chronic liver failure can also be caused by malnutrition. More rarely, liver failure can occur suddenly, in as little as 48 hours. This is called acute liver failure and is usually a reaction to poisoning or a medication overdose.
Acute liver failure
Acute liver failure typically presents in the absence of any previously known or no pre-existing liver disease with clinical and laboratory evidence of significant liver injury that leads to impaired hepatic function 2. Acute liver failure has also been called fulminant hepatic failure or acute hepatic failure, with the basic definition of the onset of hepatic encephalopathy within 8 weeks of the patient becoming jaundiced.
Certain researchers propose further subdivision of acute liver failure into:
- Hyperacute (0–7 days),
- Acute (8–28 days), and
- Subacute (29 days to <26 weeks), though these classifications have not been widely embraced 3.
Depending on the cause, acute liver failure can sometimes be reversed with treatment. In many situations, though, a liver transplant may be the only cure.
Regardless of the etiology, acute liver failure is considered an uncommon condition, with 2,000–2,300 cases per year in the United States 4. In 2009, diagnoses of acute hepatic necrosis accounted for 4.2% (243/5,748) of all adult liver transplants performed in the United States 5. Although the high mortality rate seen with acute liver failure has improved with advances in liver transplantation and intensive care unit (ICU) management, it still reaches 60–80%, far worse than most 1-year survival rates (80–90%) for liver transplant due to chronic liver disease 6. Early recognition and treatment, as well as consideration of liver transplant, are the major factors for improving survival rates.
Complications of Acute liver failure
Acute liver failure often causes complications, including:
- Excessive fluid in the brain (cerebral edema). Too much fluid causes pressure to build up in your brain.
- Bleeding and bleeding disorders. A failing liver cannot make enough clotting factors, which help blood to clot. Bleeding in the gastrointestinal tract is common with this condition. It may be difficult to control.
- Infections. People with acute liver failure are more likely to develop infections, particularly in the blood and in the respiratory and urinary tracts.
- Kidney failure. Kidney failure often occurs after following liver failure, especially if you had an acetaminophen overdose, which damages both your liver and your kidneys.
What causes acute liver failure ?
Acute liver failure occurs when liver cells are damaged significantly and are no longer able to function. Potential causes include:
- Acetaminophen overdose. Taking too much acetaminophen (Tylenol, others) is the most common cause of acute liver failure in the United States. Acute liver failure can occur after one very large dose of acetaminophen, or after higher than recommended doses every day for several days.
If you or someone you know has taken an overdose of acetaminophen, seek medical attention as quickly as possible. Don’t wait for the signs of liver failure.
- Prescription medications. Some prescription medications, including antibiotics, nonsteroidal anti-inflammatory drugs and anticonvulsants, can cause acute liver failure.
- Herbal supplements. Herbal drugs and supplements, including kava, ephedra, skullcap and pennyroyal, have been linked to acute liver failure.
- Hepatitis and other viruses. Hepatitis A, hepatitis B and hepatitis E can cause acute liver failure. Other viruses that can cause acute liver failure include Epstein-Barr virus, cytomegalovirus and herpes simplex virus.
- Toxins. Toxins that can cause acute liver failure include the poisonous wild mushroom Amanita phalloides, which is sometimes mistaken for one that is safe to eat. Carbon tetrachloride is another toxin that can cause acute liver failure. It is an industrial chemical found in refrigerants and solvents for waxes, varnishes and other materials.
- Autoimmune disease. Liver failure can be caused by autoimmune hepatitis — a disease in which your immune system attacks liver cells, causing inflammation and injury.
- Diseases of the veins in the liver. Vascular diseases, such as Budd-Chiari syndrome, can cause blockages in the veins of the liver and lead to acute liver failure.
- Metabolic disease. Rare metabolic diseases, such as Wilson’s disease and acute fatty liver of pregnancy, infrequently cause acute liver failure.
- Cancer. Cancer that either begins in or spreads to your liver can cause your liver to fail.
- Shock. Overwhelming infection (sepsis) and shock can severely impair blood flow to the liver, causing liver failure.
Many cases of acute liver failure have no apparent cause.
According to the United States Acute Liver Failure Group Registry statistics from 1998 to 2008, the most common etiologies of acute liver failure were acetaminophen (46%), followed by indeterminate causes (14%), other drugs (12%), hepatitis B (7.7%), and autoimmune causes (5.9%) 7. Less common causes included ischemia, Wilson disease, Budd-Chiari syndrome, and pregnancy.
Although European countries have similar statistics, viral hepatitis (mainly hepatitis B and A) is the predominant cause of acute liver failure worldwide 2. Drug-induced hepatitis is much less common in developing nations, though antituberculosis therapy warrants special mention as the most common cause of drug-induced acute liver failure in South Asia 8. Acute liver failure secondary to hepatitis B is also on the rise in Europe and the United States due to immigration, with some researchers attributing 5–10% of new acute liver failure cases to hepatitis B infection 9. Although only 1% of patients who develop acute hepatitis B progress to acute liver failure, the rate approaches 20% in cases of hepatitis D virus co-infection 10. Older patients and those with hepatitis C virus infection also have higher rates of acute liver failure in acute hepatitis B infection 11.
The majority of acute hepatitis A infections do not result in acute liver failure, and many young patients with acute hepatitis A are anicteric and asymptomatic. Older patients with acute hepatitis A develop acute liver failure approximately 0.2–0.4% of the time and accounted for 2.6% of cases within the acute liver failure registry in the United States.
Diagnosis of acute liver failure
The initial clinical presentation of acute liver failure is often non-specific and easily misdiagnosed, as it often occurs in otherwise healthy individuals without a history of chronic liver disease. Malaise, fatigue, and nausea usually appear first, followed by jaundice. Mental status changes usually appear after the onset of jaundice, with early onset changes associated with a higher risk of cerebral edema and intracranial hypertension 12. The subset of acute liver failure patients with a delayed presentation of jaundice and more gradual onset of hepatic insufficiency has lower rates of cerebral edema. These subfulminant hepatic failure patients were traditionally thought to have a worse overall prognosis, though recent guidelines emphasize that the etiology of acute liver failure is more important than the length of the illness 13.
History-taking is essential to narrow diagnostic possibilities, with exposures to medications and viral infections topping the list of questions to ask patients and their families.
- The use of herbal or over-the-counter supplements should be specifically investigated, as patients often do not consider these substances to be medications.
- Supplements such as hydroxycut, used for bodybuilding, have been well established as potential hepatotoxins, whereas many others such as green tea have been implicated in case reports 14, 15.
- Mushroom ingestion should also be specifically addressed, as ingestion of Amanita phalloides may produce acute liver failure 16.
- Sexual contacts, tattoos, travel, alcohol use, and recreational drug use should also be examined.
Laboratory confirmation of acute liver failure is fairly straightforward. A prolonged prothrombin time of approximately 4–6 seconds or more (international normalized ratio [INR] of greater than 1.5) with any degree of encephalopathy substantiates the diagnosis of acute liver failure and necessitates hospital admission. Other early laboratory tests that should be obtained include a complete blood count, complete metabolic panel with serum chemistries and liver-associated enzymes, arterial blood gases, and lactate. A serum acetaminophen level is important to obtain, though early therapy with n-acetylcysteine (NAC) may be beneficial even in nonacetaminophen acute liver failure 17. The complete list of laboratory tests for the initial evaluation of acute liver failure is shown in Table 1.
Table 1. Laboratory Tests to Perform in the Initial Evaluation of Acute Liver Failure
| Type of Tests | Specific Laboratory Tests |
|---|---|
| Serum chemistries |
|
| Hepatic panel |
|
| Hematology |
|
| Arterial blood |
|
| Toxicology |
|
| Viral hepatitis serologies |
|
| Autoimmune markers |
|
| Urine |
|
| Other |
|
- Ab=antibody; Ag=antigen; ALT=alanine aminotransaminase; AST=aspartate aminotransferase; HAV=hepatitis A virus; HCV=hepatitis C virus; HEV=hepatitis E virus; HSV=herpes simplex virus; Ig=immunoglobulin; INR=international normalized ratio; PCR=polymerase chain reaction; PT=prothrombin time; PTT=partial thromboplastin time; VZV=varicella zoster virus.
Numerous criteria and scoring systems based upon laboratory values and clinical findings have been developed to risk-stratify patients with acute liver failure. A system that is currently widely used comes from King’s College in London and divides patients into acetaminophen versus nonacetaminophen acute liver failure. This scoring system (Table 2) is generally quite accurate in predicting poor prognosis and, along with clinical judgment, is useful for ensuring timely transfer to a liver transplant center.
Table 2. King’s College Criteria for Poor Prognosis in Acute Liver Failure
| Acetaminophen-induced Acute Liver Failure | Nonacetaminophen-induced Acute Liver Failure |
|---|---|
| Arterial pH <7.30 after fluid resuscitation | Prothrombin time >100 sec (INR >6.5) |
Or all of the following:
| Or any 3 of the following:
|
- INR=international normalized ratio.
Acute liver failure treatment
Treatment of acute liver failure should begin even before its etiology is confirmed, particularly in cases of toxicity. Although the number of liver-directed therapies in acute liver failure is relatively limited, it is of paramount importance to recognize and administer the correct therapy. The well-established nomogram for acetaminophen level and time from exposure is useful to predict the chance of injury in a single acute ingestion, but it is important to note that this nomogram is not helpful in subacute acetaminophen toxicity or when acetaminophen is ingested in combination with alcohol. As n-acetylcysteine may also be helpful in nonacetaminophen-associated acute liver failure, it is reasonable to administer it as initial therapy, either orally or via 72-hour infusion 18. Side effects, which are usually mild, include nausea, vomiting, and, on rare occasions, bronchospasm or urticaria that responds to discontinuation, antihistamines, or epinephrine (for bronchospasm).
Mushroom poisoning also warrants special mention, as specific antidotes should be administered at an early stage, if possible. Penicillin G and milk thistle (silibinin) are thought to be helpful. Milk thistle dosing is somewhat problematic in the United States, as it is not available as a licensed drug, but rather as a supplement. The usual recommended dose is 30–40 mg/kg/day intravenously or orally, for an average of 3–4 days 19. The standard dose of penicillin G for this indication is 300,000–1,000,000 units/kg/day 20.
Treatment of viral hepatitis–induced acute liver failure has also benefited from the development of specific antiretrovirals. In hepatitis B–induced acute liver failure, antiviral treatment with new-generation nucleoside or nucleotide analog therapy should be considered, based upon early studies that showed that lamivudine was beneficial and potentially prevented the need for liver transplant when introduced at an early phase 21. It is important to emphasize that the overwhelming majority of acute hepatitis B cases do not require antiviral therapy, as most patients recover on their own, but in the setting of acute liver failure, antiviral therapy is indicated, as evidenced by encephalopathy or coagulopathy.
Hepatitis D co-infection may occur in conjunction with acute hepatitis B and is a risk factor for the development of acute liver failure. Although there is no specific therapy for hepatitis D infection, diagnosis is important, as the disease follows a characteristic biphasic pattern in which initial recovery is followed by clinical deterioration. Hepatitis E also has no specific antiviral therapy but can cause acute liver failure on rare occasions, particularly in pregnant women. Herpes simplex virus–related acute liver failure requires early recognition and immediate medical treatment with intravenous acyclovir 22. This relatively rare cause of acute liver failure can occur in pregnant women and immunosuppressed patients but has also been described in healthy individuals.
Another relatively uncommon but important cause of acute liver failure is Wilson disease, which accounts for 1–3% of acute liver failure cases in the United States annually. The typical fulminant Wilson disease patient is young, with an abrupt onset of hemolytic anemia, hyperbilirubinemia (direct and indirect), renal failure, and low serum alkaline phosphatase and uric acid levels 13. Although serum ceruloplasmin is usually low, it may be normal in up to 15% of cases; thus, 24-hour urinary copper as well as hepatic copper (via liver biopsy) are more sensitive diagnostic markers. Treatment with penicillamine is not recommended in the setting of significant hepatic dysfunction; rather, hemofiltration via albumin dialysis or plasma exchange is recommended. Some researchers suggest that early treatment with penicillamine prior to onset of encephalopathy may obviate the need for liver transplant 23. However, most cases of fulminant Wilson disease are thought to require transplant for patient survival, though this may be a function of the patient presenting late in their disease secondary to difficulty in diagnosis.
Autoimmune hepatitis is another cause of acute liver failure that is important to recognize. Autoantibodies may be absent, and liver biopsy is often required to obtain a definitive diagnosis. A small but significant subset of these patients will respond to treatment with steroids, whereas others will require liver transplantation.
Pregnancy-related acute liver failure is usually related to acute fatty liver of pregnancy or Hemolysis, Elevated Liver Enzymes, Low Platelets syndrome. Jaundice, coagulopathy, low platelets, and hypoglycemia are notable findings 13. These alterations resolve with delivery in the majority of patients, with a relative minority eventually requiring liver transplantation. As certain viral infections are more common among pregnant women, it is important not to overlook alternative or coexisting diagnoses in a jaundiced pregnant patient.
Acute Budd-Chiari syndrome is defined by acute hepatic vein thrombosis and can present with acute liver failure. Although the first-line treatment of Budd-Chiari syndrome is venous decompression via transjugular intrahepatic portosystemic shunts or a similar procedure, some patients present with hepatic dysfunction severe enough to warrant liver transplantation. One important caveat is to evaluate for the underlying cause of the thrombotic event and determine whether it is compatible with liver transplantation. For example, hypercoagulable states associated with malignancy would preclude liver transplantation, whereas other hypercoagulable states might be effectively managed with postoperative anticoagulation.
Liver Transplant for Acute Liver Failure
Despite aggressive medical management, many patients with acute liver failure deteriorate to a point where transplantation remains their only option for survival. The decision to list a patient with acute liver failure for transplant is difficult, though most physicians agree that there is a window of opportunity where the patient clearly requires transplantation and is well enough to survive the operation. Usually, this window comes after initial stabilization and before sepsis and multisystem organ failure. Relative contraindications for liver transplantation include sustained cerebral hypo-perfusion with cerebral perfusion pressures of less than 40 mmHg for more than 2 hours, the need for high-dose vasopressors, and the presence of acute respiratory distress syndrome with the need for inhaled oxygen at more than 60% FiO2 and peak end expiratory pressure of more than 12 cm H20.
Long-term outcomes following liver transplantation for acute liver failure are worse than those in chronic liver diseases, with 1-year survival rates of 58–92% and 5-year survival rates of 61–76% 24. Good-quality whole donor organs obtained after a short waiting period are considered the key to a successful outcome. The previously mentioned King’s College Criteria (Table 2) are relatively accurate in predicting poor outcome, whereas other scoring systems such as the Acute Physiology and Chronic Health Evaluation System, levels of factor v, and the Model for End-Stage Liver Disease (MELD) score have variable sensitivity and specificity 13. The etiology of liver failure also appears to be associated with prognosis, with acetaminophen, hepatitis A, shock liver, or pregnancy-related disease being associated with significantly higher transplant-free survival rates 25. Psychosocial issues are also important to consider, particularly relative to long-term outcomes, as patients with poor social support or overdose as the cause of their acute liver failure are difficult to manage after their initial recovery.
- The Progression of Liver Disease. American Liver Foundation. http://www.liverfoundation.org/abouttheliver/info/progression/[↩]
- McDowell Torres D, Stevens RD, Gurakar A. Acute Liver Failure: A Management Challenge for the Practicing Gastroenterologist. Gastroenterology & Hepatology. 2010;6(7):444-450. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2933761/[↩][↩][↩][↩]
- AASLD position paper: the management of acute liver failure. Polson J, Lee WM, American Association for the Study of Liver Disease. Hepatology. 2005 May; 41(5):1179-97. https://www.ncbi.nlm.nih.gov/pubmed/15841455[↩]
- Ichai P, Samuel D. Etiology and prognosis of fulminant hepatitis in adults. Liver Transpl. 2008;14(suppl 2):S67–79. https://www.ncbi.nlm.nih.gov/pubmed/18825677[↩]
- U.S. Department of Health & Human Services. OPTN: Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/[↩]
- Farmer DG, Anselmo DM, Ghobrial RM, et al. Liver Transplantation for Fulminant Hepatic Failure: Experience With More Than 200 Patients Over a 17-Year Period. Annals of Surgery. 2003;237(5):666-676. doi:10.1097/01.SLA.0000064365.54197.9E. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1514517/[↩]
- Management of acute liver failure. Stravitz RT, Kramer DJ. Nat Rev Gastroenterol Hepatol. 2009 Sep; 6(9):542-53. https://www.ncbi.nlm.nih.gov/pubmed/19652652/[↩]
- Kumar R, Shalimar, Bhatia v, et al. Antituberculosis therapy-induced acute liver failure: magnitude, profile, prognosis, and predictors of outcome. Hepatology. 2010;51:1665–1674. https://www.ncbi.nlm.nih.gov/pubmed/20196116[↩]
- Shiffman ML. Management of acute hepatitis B. Clin Liver Dis. 2010;14:75–91. https://www.ncbi.nlm.nih.gov/pubmed/20123442[↩]
- Shukla NB, Poles MA. Hepatitis B infection: co-infection with hepatitis C virus, hepatitis D virus and human immunodeficiency virus. Clin Liver Dis. 2004;8:445–460. https://www.ncbi.nlm.nih.gov/pubmed/15481349[↩]
- Sagnelli E, Coppola N, Pisaturo M, et al. HBv superinfection in HCv chronic carriers: a disease that is frequently severe but associated with the eradication of HCv. Hepatology. 2009;49:1090–1097. https://www.ncbi.nlm.nih.gov/pubmed/19263473[↩]
- Lee WM. Acute liver failure. N Engl J Med. 1993;329:1862–1872. https://www.ncbi.nlm.nih.gov/pubmed/8305063[↩]
- Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology. 2005;41:1179–1197. https://www.ncbi.nlm.nih.gov/pubmed/15841455[↩][↩][↩][↩]
- Fong TL, Klontz KC, Canas-Coto A, et al. Hepatotoxicity due to hydroxycut: a case series. Am J Gastroenterol. 2010 Jan 26.[↩]
- Gloro R, Hourman-Olivier I, Mosquet B, et al. Fulminant hepatitis during self medication with hydroalcoholic extract of green tea. Eur J Gastroenterol Hepatol. 2005;17:1135–1137. https://www.ncbi.nlm.nih.gov/pubmed/16148563[↩]
- Ganzert M, Felgenhauer N, Zilker T. Reassessment of predictors of fatal outcome in amatoxin poisoning: some critical comments. J Hepatol. 2007;47:424–425. https://www.ncbi.nlm.nih.gov/pubmed/17631978[↩]
- Lee W, Hynan L, Rossaro L, et al. INTRAVENOUS N-ACETYLCYSTEINE IMPROVES TRANSPLANT-FREE SURVIVAL IN EARLY STAGE NON-ACETAMINOPHEN ACUTE LIVER FAILURE. Gastroenterology. 2009;137(3):856-864.e1. doi:10.1053/j.gastro.2009.06.006. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3189485/[↩]
- Sotelo N, de los Angeles Durazo M, Gonzalez A, Dhanakotti N. Early treatment with N-acetylcysteine in children with acute liver failure secondary to hepatitis A. Ann Hepatol. 2009;8:353–358. https://www.ncbi.nlm.nih.gov/pubmed/20009135[↩]
- Hruby K, Csomos G, Fuhrmann M, Thaler H. Chemotherapy of Amanita phalloides poisoning with intravenous silibinin. Hum Toxicol. 1983;2:138–185. https://www.ncbi.nlm.nih.gov/pubmed/6862461[↩]
- Broussard CN, Aggarwal A, Lacey SR, et al. Mushroom poisoning–from diarrhea to liver transplantation. Am J Gastroenterol. 2001;96:3195–3198. https://www.ncbi.nlm.nih.gov/pubmed/11721773[↩]
- Tillmann HL, Hadem J, Leifeld L, et al. Safety and efficacy of lamivudine in patients with severe acute or fulminant hepatitis B, a multicenter experience. J viral Hepatol. 2006;13:256–263. https://www.ncbi.nlm.nih.gov/pubmed/16611192[↩]
- Ichai P, Roque Afonso AM, Sebagh M, et al. Herpes simplex virus-associated acute liver failure: a difficult diagnosis with a poor prognosis. Liver Transpl. 2005;11:1550–1555. https://www.ncbi.nlm.nih.gov/pubmed/16315311[↩]
- Durand F, Bernuau J, Giostra E, et al. Wilson’s disease with severe hepatic insufficiency: beneficial effects of early administration of D-penicillamine. Gut. 2001;48(6):849-852. doi:10.1136/gut.48.6.849. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1728316/pdf/v048p00849.pdf[↩]
- Chan G, Taqi A, Marotta P, et al. Long-term outcomes of emergency liver transplantation for acute liver failure. Liver Transpl. 2009;15:1696–1702. https://www.ncbi.nlm.nih.gov/pubmed/19938124[↩]
- Ostapowicz G, Fontana RJ, SchiØdt Fv, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–954. https://www.ncbi.nlm.nih.gov/pubmed/12484709[↩]