Loin pain hematuria syndrome
Loin pain hematuria syndrome (LPHS) is the combination of severe, unexplained loin pain and microscopic or macroscopic amounts of blood in the urine (hematuria) that is otherwise unexplained 1. The loin pain can be on one side of body or both sides. The frequency and length of pain episodes can vary. The blood may be easily seen in the urine or may only be seen under a microscope. Diagnosis of loin pain hematuria syndrome includes a variety of tests that rule out other possible causes of the loin pain and blood in the urine. Loin pain hematuria syndrome is considered primary when it occurs without finding any damage to the tiny blood cleaning filters of the kidneys (glomeruli), and secondary when it occurs with glomerular disease caused by another disease, such as IgA nephropathy. A kidney biopsy is needed to tell the difference between primary and secondary loin pain hematuria syndrome 2.
Few data exist regarding the epidemiology of loin pain hematuria syndrome, which is an extremely rare disease with a prevalence of about 0.012% 2. Loin pain hematuria syndrome is more common in women with as many as 70% of patients with loin pain hematuria syndrome being females 3.
The cause of primary loin pain hematuria syndrome is currently unknown. Unless the glomerular disease is treatable, treatment of both primary and secondary loin pain hematuria syndrome focuses on relieving the symptoms, mainly through pain management 4. Loin pain hematuria syndrome is not known to cause major kidney damage, end-stage kidney disease, or early death 5.
Loin pain hematuria syndrome causes
The cause of primary loin pain hematuria syndrome is not known. The blood in the urine associated with loin pain hematuria syndrome is believed to come from the glomeruli, which are the tiny blood filtering units of the kidneys. Normally the blood is filtered in a glomerulus and the waste and extra fluid is passed into a connected tubule to become urine. However, the majority of kidney biopsies from people with loin pain hematuria syndrome also find red blood cells in the tubules, suggesting at least some of the glomeruli are damaged or abnormal, causing them to be leaky. It is not clear however why sometimes the kidney biopsies do not find red blood cells in the tubules. The pain associated with loin pain hematuria syndrome is believed to come from the kidneys, but how the pain develops is not understood 5.
About half of the people with loin pain hematuria syndrome have had kidney stones in the past. Some scientists, therefore, suspect that the formation of crystals and/or stones in the kidney may also contribute to loin pain hematuria syndrome as the crystal or stones may block or injure the renal tubules (the long narrow tubes in the kidney that concentrate and transport urine) 2.
Sometimes loin pain hematuria syndrome is related to other conditions. When the cause of loin pain hematuria syndrome is known, some experts refer to this as loin pain hematuria syndrome, type 1 or secondary loin pain hematuria syndrome 6.
Loin pain hematuria syndrome pathophysiology
Since Little et al. first described the condition in 1967 7, several hypotheses have been proposed regarding the pathophysiology of loin pain hematuria syndrome. These include vascular disease of the kidney, complement activation on arterioles 8, coagulopathy 9, venocalyceal fistula 10, abnormal ureteral peristalsis 11, hypersensitivity 8, psychopathology 12, intratubular deposition of calcium 13 and nephritis 12. Of these, nephritis (usually IgA) is the only one documented 14.
When no acquired underlying glomerular disease is responsible for the loin pain hematuria syndrome, it is designated primary loin pain hematuria syndrome, as opposed to secondary loin pain hematuria syndrome when due to an underlying glomerular process, usually IgA nephropathy. The distinction can only be made by kidney biopsy 15.
Some studies have suggested that thin glomerular basement membrane (GBM) disease could be associated with or contribute to loin pain hematuria syndrome. In a study conducted by Herbert et al. seven patients were described with thin GBM, which was linked with loin pain hematuria syndrome 15. Renal biopsies on those patients showed red cells in the renal tubules, which indicated glomerular hematuria, the only glomerular abnormality present. These red cells were occluding the tubules, leading Herbert et al. 16 to suggest that occlusion of a fraction of renal tubules could be behind the cause of the loin pain if back-leak of glomerular filtrate occurred resulting in expansion of the renal parenchymal volume and stretching of the renal capsule. Thus, they concluded that thin glomerular basement membrane could be a cause of the flank pain and gross hematuria in some patients with loin pain hematuria syndrome 15.
Another possible mechanism for loin pain hematuria syndrome is microcrystal formation in the renal tubules. Praga et al. 17 conducted a study that noted high prevalence of hyperuricosuria, hypercalciuria and nephrolithiasis in patients with thin glomerular basement membrane neuropathy. They suggested that the concomitant occurrence of factors that promote urolithiasis and glomerular hematuria may result in the formation of intratubular microcrystals. Combined with intratubular red blood cells, microcrystal formation could lead to increased intratubular obstruction and amplified flank pain 17. It has since been found that most non-calcium oxalate stone formers make stones by tubular crystallization and do not have loin pain hematuria syndrome; although most stone formers do not have loin pain hematuria syndrome, many patients with loin pain hematuria syndrome have a history of kidney stones (up to 50%) 13.
No causal relationship has been established between complement activation on arterioles and loin pain hematuria syndrome but several case reports have described an association. Miller et al. 8 described a case where the kidney biopsy showed microaneurysmal and glomeruloid angiomatous changes. The depositions of properdin, C5b-9 complex and C3 in arterioles would suggest complement activation. Both Naish et al. 18 and Miller et al. 8 described an association between C3 deposition and loin pain hematuria syndrome.
With regard to coagulopathy, even though platelet counts, prothrombin times, thrombin times and fibrinogen levels are usually all normal, several studies have shown more occult abnormalities. Abnormalities included below-normal heparin-thrombin clotting times 19, low factor XII levels 20, elevated plasma b-thromboglobulin levels with increased platelet aggregation by serotonin and adenosine diphosphate and higher than normal plasma C-reactive protein and D-dimer levels 21. In another study, Siegler et al. 9 hypothesized that abnormal platelet activation and fibrin deposition played a role in the pathogenesis of loin pain hematuria syndrome.
Although renal vascular disease was thought to be one of the underlying pathophysiological processes in loin pain hematuria syndrome early on 22, more recent renal arteriography studies of patients with loin pain hematuria syndrome disagree with this hypothesis as the renal vasculature more commonly appears normal 21.
It is important to note that loin pain hematuria syndrome still remains a diagnosis of exclusion and can be the common presentation of a variety of pathologic processes as opposed to a single etiology.
Loin pain hematuria syndrome symptoms
As the name of the syndrome suggests, the main symptoms of loin pain hematuria syndrome are 5:
- Loin pain: the pain is often described as a burning or throbbing and for some can worsen with exercise or when lying down flat on their back (facing upward). The pain may be felt on one side of the body (unilateral) or both sides (bilateral).
- Blood in the urine (hematuria): the blood may be noticeable in the urine or may only be seen under a microscope. Although larger amounts of blood in the urine are usually associated with severe pain episodes, in some cases, the blood may clear up even during a pain episode.
Other symptoms of loin pain hematuria syndrome may include 2:
- Nausea and vomiting during episodes of pain
- Low-grade fever (up to 101°F or 38.3 °C)
- Painful urination
loin pain hematuria syndrome can affect people differently. The episodes of pain and blood in the urine can last hours, weeks, or may be constant. Episodes can range from happening several times a year to being chronic with little or no relief between episodes 5.
Loin pain hematuria syndrome diagnosis
Loin pain hematuria syndrome is diagnosed when all other nonglomerular causes of the symptoms have been ruled out (known as a diagnosis of exclusion). Glomeruli are the blood cleaning units of the kidneys and are believed to be the source of the bleeding in loin pain hematuria syndrome. In addition to ruling out other possible causes, the episodes loin pain and blood in the urine must persist or be recurrent for at least 6 months and not associated with blockages due to kidney stones 5.
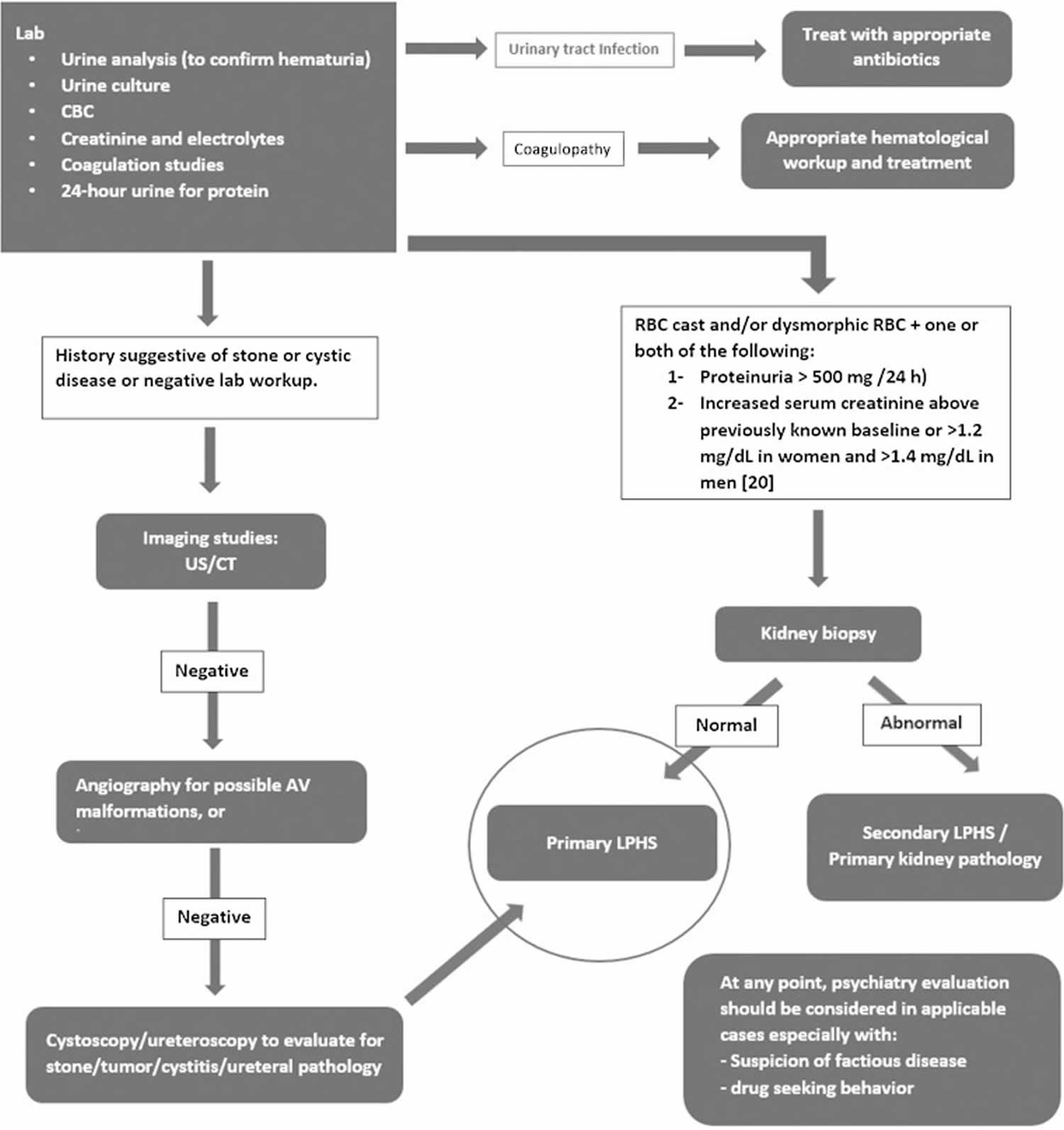
Tests to rule out other possible causes of loin pain and blood in the urine may include 23:
- Urine culture to rule out infection
- Urinalysis to check for damage to the filtering units of the kidney (glomerular disease)
- Endoscopy of the urethra and bladder (cystoscopy) and/or CT scan to rule out kidney stones, tumors, and cysts
- Special X-ray or CT scan with dye (angiography or CT angiography) to rule out problems with the kidney’s blood vessels, such as a tangle of veins and arteries (arteriovenous malformations or AVM)) or benign tumors made up of a build up of blood vessels (hemangiomas)
- Upper urinary tract endoscopy (flexible ureteroscopy) to rule out problems with the tubes that carry the urine from the kidneys to the bladder (ureters)
- Special blood tests to rule out bleeding disorders
A kidney biopsy may be performed to rule out secondary loin pain hematuria syndrome if there are any signs of glomerular disease, such as microscopic blood in the urine or abnormal shaped blood cells with the presence of protein in urine (proteinuria), and/or increased creatinine levels in the blood. In some cases, a kidney biopsy may also be recommended to evaluate the structure and function of the kidney 24.
Figure 1. Loin pain hematuria syndrome diagnosis
Footnote: Diagnostic work-up for loin pain hematuria syndrome.
Abbreviations: AV = arteriovenous; CBC = complete blood count; CT = computed tomography; LPHS = loin pain hematuria syndrome; RBC = red blood cell; US = ultrasound.
[Source 2 ]Exam findings
Physical exam and laboratory findings from loin pain hematuria syndrome vary. Many patients have unremarkable physical exam findings. Numerous patients report low-grade fevers and the majority have normal renal function, judged by creatinine clearance and serum creatinine. Studies have shown that there are no abnormal 24-hour urine concentrations of calcium, phosphorus, uric acid, oxalate and cystine. Coagulation studies in these patients are frequently normal, including partial thromboplastin time, prothrombin time, bleeding time, hematocrit and platelet count 15.
Hematuria in loin pain hematuria syndrome is typically glomerular in origin characterized by dysmorphic red cells with or without red blood cell casts. However, as described earlier, intratubular crystal depositions could play a role in the pathogenesis of loin pain hematuria syndrome and the absence of typical findings to suggest glomerular origin of hematuria does not exclude loin pain hematuria syndrome.
Hematuria can be either microscopic or macroscopic. Episodes of macroscopic hematuria are usually associated with worsening pain but in between episodes urine analysis may show microscopic hematuria or in some patients, the hematuria clears completely even though the pain persists 15.
Proteinuria is not a feature of loin pain hematuria syndrome. One series of 34 patients showed the protein excretion to be above the upper limit of the normal of 150 mg/day in 11 patients and above 500 mg/day in only two patients.
Loin pain hematuria syndrome treatment
At this time, there is no disease-specific treatment or cure for loin pain hematuria syndrome, since the cause of the disease is not understood. As some studies have shown that 25–50% of loin pain haematuria syndrome patients enter a period of spontaneous remission within 3–5 years 15, a gradual approach in treatment progressing from conservative management to more invasive measures would be reasonable. Unless the cause of glomerular disease is treatable, the treatment of primary and secondary loin pain hematuria syndrome focuses on pain management 5. Pain management with opiate and non-opiate analgesia is common.
People with loin pain hematuria syndrome may be told to avoid activities that increase or trigger their pain, such as exercise, riding in a car, or lying on their back. Pain management may include medications, such as non-opioid pain pills (analgesics), narcotics, or opioids depending on the severity of pain, and/or possibly a nerve block or transcutaneous electrical nerve stimulation (TENS). Medications may also be used to treat nausea and vomiting if needed. If there is a history of kidney stones or build of calcium deposits, recommended treatment may include management of the amount of liquid a person drinks or changes in diet 5.
Limited evidence suggests that drugs that inhibit angiotensin (angiotensin converting enzyme inhibitors or angiotensin II receptor blockers) may reduce the frequency and severity of episodes of loin pain and severe hematuria 5. Similarly, one study in 2009 found neuromodulation through implanted electrodes successfully reduced the pain in four women with loin pain hematuria syndrome, but it is unclear if neuromodulation has been tested further as a treatment for loin pain hematuria syndrome 23.
People with debilitating pain who do not respond to other therapies may be offered surgery, such as renal denervation, nephrectomy, or kidney auto-transplantation; however, surgical treatment of loin pain hematuria syndrome is controversial as some studies suggest that it has limited value for treating the recurrent pain and the possible complications of the procedures may outweigh the benefits 5.
Loin pain hematuria syndrome prognosis
While loin pain hematuria syndrome does not normally affect the function of the kidneys or cause other health problems, the pain associated with loin pain hematuria syndrome can be chronic and/or severe and may seriously decrease a person’s quality of life. Long term treatment with narcotics and opiates can lead to drug addiction, which can add further social and medical issues 23. Due to the disabling nature of chronic, severe pain, those caring for a person with loin pain hematuria syndrome should watch for signs of depression and/or anxiety 25.
Currently, there are few long term studies to have a clear understanding of the course of loin pain hematuria syndrome, but two small, older studies, as well as the experience of specialists, propose the symptoms of loin pain hematuria syndrome will eventually get better spontaneously, however this can be after many years. Published cases and studies suggest a range for the duration of symptoms of 2-35 years 23.
References- Loin pain hematuria syndrome: case series. W V Med J. 2003 Sep-Oct;99(5):192-3. https://www.ncbi.nlm.nih.gov/pubmed/14959511
- Zubair AS, Salameh H, Erickson SB, Prieto M. Loin pain hematuria syndrome. Clin Kidney J. 2016;9(1):128–134. doi:10.1093/ckj/sfv125 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4720203
- Taba Taba Vakili S, Alam T, Sollinger H. Loin pain hematuria syndrome. Am J Kidney Dis 2014; 64: 460.
- Loin pain hematuria syndrome. Am J Kidney Dis. 2014 Sep;64(3):460-72. doi: 10.1053/j.ajkd.2014.01.439. Epub 2014 Apr 13. https://www.ajkd.org/article/S0272-6386(14)00588-5/fulltext
- Loin pain-hematuria syndrome. https://www.uptodate.com/contents/loin-pain-hematuria-syndrome
- Bath NM, Williams DH, Sollinger HW, Redfield RR 3rd. Commentary: Loin Pain Hematuria Syndrome. Rare Dis Res Treat. 2018; 3(4):1-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6457464
- Little PJ, Sloper JS, de Wardener HE. A syndrome of loin pain and haematuria associated with disease of peripheral renal arteries. Q J Med 1967; 36: 253–259
- Miller F, Lane BP, Kirsch M, et al. Loin pain-hematuria syndrome with a distinctive vascular lesion and alternative pathway complement activation. Arch Pathol Lab Med 1994; 118: 1016–1019
- Siegler RL, Brewer ED, Hammond E. Platelet activation and prostacyclin supporting capacity in the loin pain hematuria syndrome. Am J Kidney Dis 1988; 12: 156–160
- Low AI, Matz LR. Haematuria and renal fornical lesions. Br J Urol 1972; 44: 681–691
- Woolfson RG, Lewis CA, Hill PD, et al. Ureteric peristalsis studies in loin pain and haematuria syndrome: another diagnostic disappointment. Br J Urol 1993; 72: 291–292
- Kelly B. Psychiatric issues in the “loin pain and haematuria syndrome”. Aust N Z J Psychiatry 1994; 28: 302–306
- Coe FL, Evan AP, Worcester EM, et al. Three pathways for human kidney stone formation. Urol Res 2010; 38: 147–160
- Smith HS, Bajwa ZH. Loin pain hematuria syndrome-visceral or neuropathic pain syndrome? Clin J Pain 2012; 28: 646–651
- Spetie DN, Nadasdy T, Nadasdy G, et al. Proposed pathogenesis of idiopathic loin pain-hematuria syndrome. Am J Kidney Dis 2006; 47: 419–427
- Hebert LA, Betts JA, Sedmak DD, et al. Loin pain-hematuria syndrome associated with thin glomerular basement membrane disease and hemorrhage into renal tubules. Kidney Int 1996; 49: 168–173
- Praga M, Martinez MA, Andres A, et al. Association of thin basement membrane nephropathy with hypercalciuria, hyperuricosuria and nephrolithiasis. Kidney Int 1998; 54: 915–920
- Naish PF, Aber GM, Boyd WN. C3 deposition in renal arterioles in the Loin pain and haematuria syndrome. Br Med J 1975; 3: 746.
- Burden RP, Dathan JR, Etherington MD, et al. The loin-pain/haematuria syndrome. Lancet 1979; 1: 897
- Higgins PM, Aber GM. Renal pain and haematuria. Br J Urol 1974; 46: 601–608
- Leaker BR, Gordge MP, Patel A, et al. Haemostatic changes in the loin pain and haematuria syndrome: secondary to renal vasospasm? Q J Med 1990; 76: 969–979
- Sheil A, Chui A, Verran D, et al. Evaluation of the loin pain/hematuria syndrome treated by renal autotransplantation or radical renal neurectomy. Am J Kidney Dis 1998; 32: 215–220
- Zubair AS, Salameh H, Erickson SB & Prieto M. Loin pain hematuria syndrome. Clinical Kidney Journal. February 1, 2016; 9(1):128–134. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4720203
- Taba Taba Vakili S, Alam T, Sollinger H. Loin pain hematuria syndrome. Am J Kidney Dis. September 2014; 64(3):460-472. https://www.ncbi.nlm.nih.gov/pubmed/24725981
- De Heer EW, Gerrits MMJG, Beekman ATF, et al. The Association of Depression and Anxiety with Pain: A Study from NESDA. Sun HS, ed. PLoS ONE. October 15, 2014; 9(10):e106907. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4198088