What is lymphoma
Lymphoma is a cancer of the lymphatic system 1, which is part of the body’s germ-fighting network (see Figures 1, 2 and 3). Lymphomas are cancers that start in white blood cells called lymphocytes. Lymphocytes are part of the body’s immune system. The lymphatic system includes the lymph nodes (lymph glands), spleen, thymus gland and bone marrow. Lymphoma can affect all those areas as well as other organs throughout the body. The World Health Organization’s (WHO) classification system identifies more than 90 different subtypes of lymphoma (see Table 2) 2.
There are many types of lymphoma. The main types of lymphoma are:
- Hodgkin’s lymphoma (Hodgkin disease): Hodgkin’s lymphoma (Hodgkin disease) is a cancer that starts in white blood cells called lymphocytes. Hodgkin’s lymphomas contain cells called Reed Sternberg cells. Treatment for Hodgkin’s lymphoma is different from other types of lymphoma. Hodgkin’s lymphoma is one of the most curable forms of cancer. The five-year relative survival rate is 94.3 percent for people who were less than 45 years old at diagnosis. Hodgkin lymphoma is most commonly diagnosed at 20 to 34 years of age; however, the median age at death is 68 because of the higher survival rate among younger patients 3.
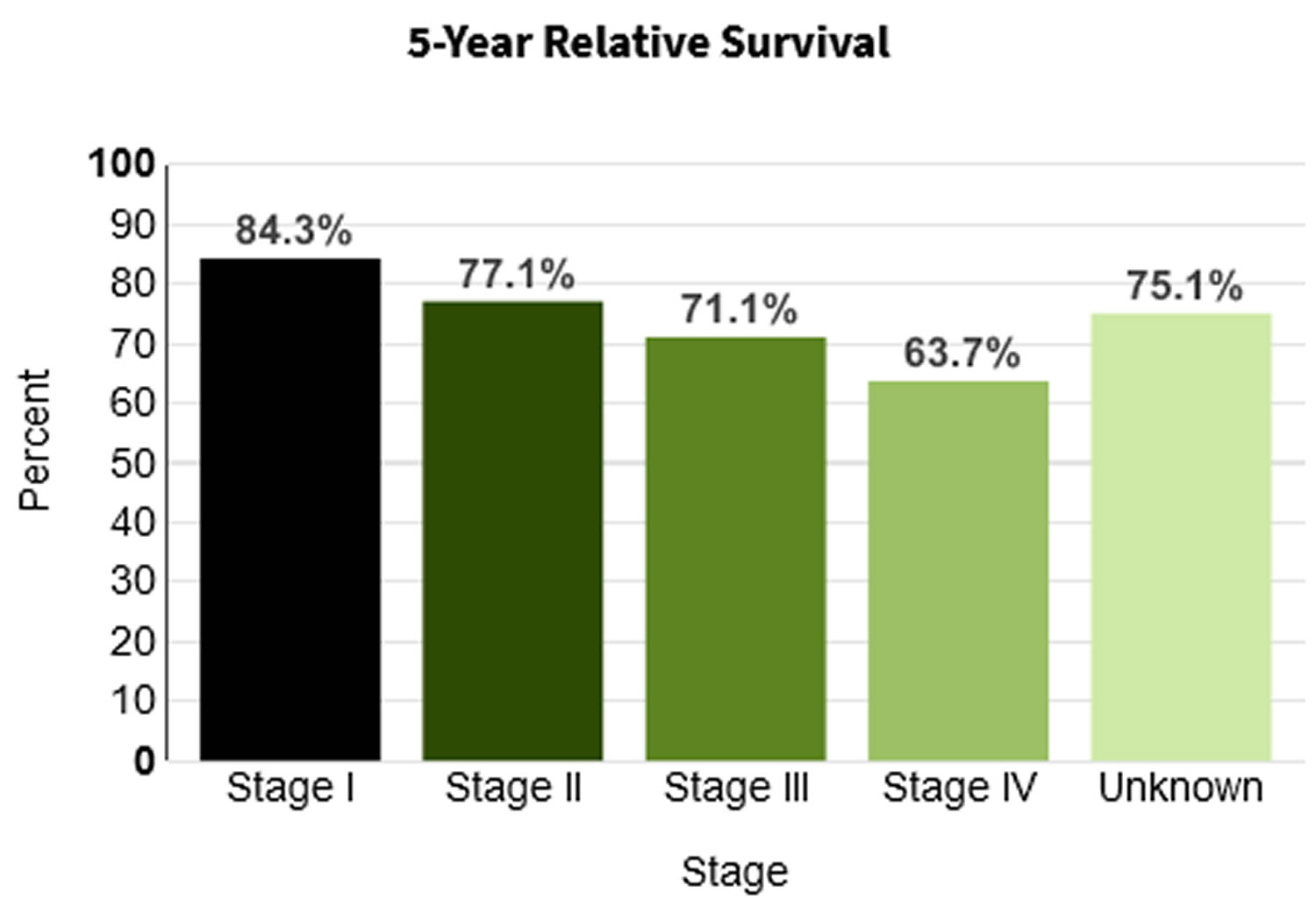
- Non-Hodgkin’s lymphoma (NHL): Non-Hodgkin lymphoma (NHL) is a cancer that starts in cells called lymphocytes, which are part of the body’s immune system. About 90 percent of people diagnosed with lymphoma have non-Hodgkin’s lymphoma (NHL). Incidence of non-Hodgkin lymphoma is higher in men and whites, and it increases with age. The median age of patients at diagnosis of non-Hodgkin lymphoma is 67 years, and the median age at death is 76 4.
They behave, spread, and respond to treatment differently, so it’s important for you to know which one you have. Knowing which type of lymphoma you have is important because it affects your treatment options and your outlook (prognosis). If you aren’t sure which type you have, ask your doctor so you can get the right information.
What lymphoma treatment is best for you depends on your lymphoma type and its severity. Lymphoma treatment may involve chemotherapy, immunotherapy medications, radiation therapy or a bone marrow transplant.
Approximately 82,000 new U.S. patients are diagnosed with lymphoma annually, representing 4.7% of all new cancer cases in the United States 5. Tobacco use and obesity are major modifiable risk factors, with genetic, infectious, and inflammatory causes also contributing 5. Lymphoma typically presents as painless painless swelling in a lymph node, usually in the neck, armpit or groin; with systemic symptoms of fever, unexplained weight loss, and night sweats occurring in more advanced stages of the disease. An open lymph node biopsy is preferred for diagnosis. The Lugano classification system incorporates symptoms and the extent of the disease as shown on positron emission tomography (PET)/computed tomography (CT) to stage lymphoma, which is then used to determine treatment. Chemotherapy treatment plans differ between the main subtypes of lymphoma. Non-Hodgkin’s lymphoma (NHL) is treated with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) with or without rituximab (R-CHOP), bendamustine, and lenalidomide. Hodgkin’s lymphoma is treated with combined chemotherapy with ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine), Stanford V (a chemotherapy regimen consisting of mechlorethamine, doxorubicin, vinblastine, vincristine, bleomycin, etoposide, and prednisone), or BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) with radiotherapy. Subsequent chemotherapy toxicities include neuropathy, cardiotoxicity, and secondary cancers such as lung and breast, and should be considered in the shared decision-making process to select a treatment regimen.
In 2019 the five-year survival rate for non-Hodgkin lymphoma was 72.0%, and for Hodgkin lymphoma was 86.6% 6.
Once remission is achieved, patients need routine surveillance to monitor for complications and relapse, in addition to age-appropriate screenings recommended by the U.S. Preventive Services Task Force. Patients should receive a 13-valent pneumococcal conjugate vaccine followed by a 23-valent pneumococcal polysaccharide vaccine at least eight weeks later with additional age-appropriate vaccinations because lymphoma is an immunosuppressive condition. Household contacts should also be current with their immunizations.
Table 1. Common Lymphoma Subtypes with Incidence and Five-Year Survival
| Lymphoma subtype | Incidence per 100,000 | Five-year survival |
|---|---|---|
| Hodgkin’s lymphoma | 2.8 | 85.70% |
| Non-Hodgkin B-cell lymphomas | ||
| Burkitt | 0.4 | 64.10% |
| Diffuse large B cell | 7.2 | 63.20% |
| Follicular | 3.5 | 88.40% |
| Marginal zone | 2.2 | 90.30% |
| Precursor B cell | 1.5 | 68.90% |
| Non-Hodgkin T-cell and natural killer cell lymphomas | ||
| Mycosis fungoides | 0.6 | 90.90% |
| Peripheral T-cell | 1.2 | 58.40% |
Types of lymphoma
The World Health Organization’s (WHO) classification system identifies more than 90 different subtypes of lymphoma (Table 2) 2. The initial stratification is derived from B-cell, T-cell, or natural killer (NK) cell origin; however, they are ultimately each defined by morphology, immunopheno-type, genetic, molecular, and clinical features into 2:
- Chronic lymphocytic leukemia
- Cutaneous B-cell lymphoma
- Cutaneous T-cell lymphoma
- Hodgkin’s lymphoma (Hodgkin’s disease)
- Non-Hodgkin’s lymphoma (NHL)
- Waldenstrom macroglobulinemia
Table 2. 2016 WHO classification of mature lymphoid, histiocytic, and dendritic neoplasms
| Mature B-cell neoplasms |
|
|
|
|
|
|
| Splenic diffuse red pulp small B-cell lymphoma |
| Hairy cell leukemia-variant |
|
| Waldenström macroglobulinemia |
|
|
|
|
|
|
|
|
|
|
|
| Pediatric nodal marginal zone lymphoma |
|
| In situ follicular neoplasia* |
| Duodenal-type follicular lymphoma* |
|
|
|
|
| In situ mantle cell neoplasia* |
|
| Germinal center B-cell type* |
| Activated B-cell type* |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Mature T and NK neoplasms |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Lymphomatoid papulosis |
| Primary cutaneous anaplastic large cell lymphoma |
|
|
|
|
|
|
|
|
|
|
|
| Hodgkin lymphoma |
|
|
| Nodular sclerosis classical Hodgkin lymphoma |
| Lymphocyte-rich classical Hodgkin lymphoma |
| Mixed cellularity classical Hodgkin lymphoma |
| Lymphocyte-depleted classical Hodgkin lymphoma |
| Posttransplant lymphoproliferative disorders (PTLD) |
|
|
|
|
|
|
| Histiocytic and dendritic cell neoplasms |
|
|
|
|
|
|
|
|
|
Footnotes: *Changes from the 2008 classification. Provisional entities are listed in italics.
[Source 2 ]The Lymphatic System
To understand what lymphoma is, it helps to know about the lymph system (also known as the lymphatic system). The lymph system is part of the immune system, which helps fight infections and some other diseases. The lymphatic system plays a role in:
- fighting bacteria and other infections
- destroying old or abnormal cells, such as cancer cells
The lymphatic system also helps the flow of fluids in the body.
The lymph system is made up mainly of cells called lymphocytes, a type of white blood cell. There are 2 main types of lymphocytes:
- B lymphocytes (B cells): B lymphocytes (B cells) respond to an infection by changing into a different type of cell called a plasma cell. Plasma cells make proteins called antibodies (also called immunoglobulins) that help the body attack and kill disease-causing germs like bacteria and viruses.
- T lymphocytes (T cells): There are several types of T cells. Some T cells destroy germs or abnormal cells in the body. Other T cells help boost or slow the activity of other immune system cells.
- Natural killer (NK) cells, which attack virus-infected cells or tumor cells.
The lymphatic system is a vast collection of cells and biochemicals that travel in lymphatic vessels, and the organs and glands that produce them. The lymphatic system includes a network of vessels (like the arteries and veins that carry blood) that assist in circulating body fluids (a colorless liquid called lymph), so it is closely associated with your cardiovascular system. Lymphatic vessels transport excess fluid away from interstitial spaces in most tissues and return it to the bloodstream (Figure 3). This fluid carries food to the cells and bathes the body tissues to form tissue fluid. The fluid then collects waste products, bacteria, and damaged cells. It also collects any cancer cells if these are present. This fluid then drains into the lymph vessels. Without the lymphatic system, this fluid would accumulate in tissue spaces. Special lymphatic capillaries, called lacteals, are located in the lining of the small intestine. They absorb digested fats and transport them to the venous circulation.
The lymphatic system is a system of thin tubes and lymph nodes that run throughout the body. Lymph nodes are bean shaped glands. The thin tubes are called lymph vessels or lymphatic vessels. Tissue fluid called lymph circulates around the body in these vessels and flows through the lymph nodes.
The lymph system is an important part of your immune system. It plays a role in fighting bacteria and other infections and destroying old or abnormal cells, such as cancer cells.
The major sites of lymphoid tissue are:
- Lymph nodes: Lymph nodes are bean-sized collections of lymphocytes and other immune system cells throughout the body, including inside the chest, abdomen, and pelvis. They are connected to each other by a system of lymphatic vessels.
- Spleen: The spleen is an organ under the lower ribs on your left side. The spleen makes lymphocytes and other immune system cells. It also stores healthy blood cells and filters out damaged blood cells, bacteria, and cell waste.
- Bone marrow: The bone marrow is the spongy tissue inside certain bones. New blood cells (including some lymphocytes) are made there.
- Thymus: The thymus is a small organ behind the upper part of the breastbone and in front of the heart. Thymus is an organ in which T lymphocytes mature and multiply.
- Adenoids and tonsils: These are collections of lymphoid tissue in the back of your throat. They help make antibodies against germs that are breathed in or swallowed.
- Digestive tract: The stomach, intestines, and many other organs also have lymph tissue.
The lymphatic system has a second major function— it enables you to live in a world with different types of organisms. Some of them live in or on the human body and in some circumstances may cause infectious diseases. Cells and biochemicals of the lymphatic system launch both generalized and targeted attacks against “foreign” particles, enabling the body to destroy infectious agents. This immunity against disease also protects against toxins and cancer cells. When the immune response is abnormal, persistent infection, cancer, allergies, and autoimmune disorders may result.
The larger lymphatic vessels lead to specialized organs called lymph nodes. After leaving the lymph nodes, the vessels merge to form still larger lymphatic trunks.
Figure 1. Locations of major lymph nodes
Figure 2. Functions of lymph nodes in the lymphatic system
Figure 3. Schematic representation of lymphatic vessels transporting fluid from interstitial spaces to the bloodstream. Depending on its origin, lymph enters the right or left subclavian vein.
Lymphoma signs and symptoms
Signs and symptoms of lymphoma include:
- Enlarged lymph nodes that can occur in any part of the body but most often occur in the neck, armpit or groin
- Fatigue
- Fever
- Night sweats
- Shortness of breath
- Weight loss
- Itchy skin
The most common early sign of lymphoma is painless enlargement of one or more lymph nodes (also known as painless adenopathy). The enlarged lymph nodes can wax and wane over years in indolent presentations or involve rapidly progressive enlarged lymph nodes in more aggressive subtypes. Hodgkin’s lymphoma typically appears in the supradiaphragmatic lymph nodes. Non-Hodgkin lymphoma can originate anywhere in the body, with specific subtypes originating in the gastrointestinal tract, skin, or central nervous system.
Systemic symptoms of fever, unexplained weight loss, and night sweats occur in a subset of patients with more advanced disease. Lymphoma spreads to extranodal sites by direct invasion or by spreading through blood to the spleen, liver, lungs, or bone marrow 7, 8. High-grade lymphomas can present as oncologic emergencies because of the structural compression from the enlarging tumor, including superior vena cava syndrome, malignant epidural spinal cord compression, or malignant pericardial effusion 9. Paraneoplastic syndrome is a group of symptoms that may develop when substances released by some cancer cells disrupt the normal function of surrounding cells and tissue. Paraneoplastic syndromes are rare with lymphoma, occurring as paraneoplastic cerebellar degeneration in Hodgkin lymphoma and as dermatomyositis and polymyositis in Hodgkin and non-Hodgkin lymphomas 10.
What Causes lymphoma
Doctors aren’t sure what causes lymphoma. Lymphoma begins when a disease-fighting white blood cell called a lymphocyte develops a mutation in its genetic code. The mutation tells the cell to multiply rapidly, causing many diseased lymphocytes that continue multiplying.
The mutations also allow the cells to go on living when other cells would die. This causes too many diseased and ineffective lymphocytes in your lymph nodes and causes the lymph nodes to swell.
Risk factors for lymphoma
Factors that may increase your risk of lymphoma include:
- Increasing age. Your risk of lymphoma increases as you age, though it can occur at any age. Some types of lymphoma are more common in young adults.
- Being male. Lymphoma is more common in men than it is in women.
- Having an impaired immune system. Lymphoma is more common in people with immune system diseases or in people who take drugs that suppress their immune systems.
- Developing certain infections. Some infections are associated with an increased risk of lymphoma, including Epstein-Barr virus and Helicobacter pylori infection.
Tobacco use 11 and obesity (body mass index [BMI] of 30 kg/m² or higher) 12 are major modifiable risk factors, with genetic, infectious, and inflammatory causes also contributing 5. Breast implants and long-term pesticide exposure have also been associated with non-Hodgkin lymphoma 13.
First-degree relatives of patients with non-Hodgkin lymphoma and Hodgkin lymphoma have a respective 1.7-fold and 3.1-fold increased risk of developing lymphoma 5. A family history of a specific subtype of lymphoma is associated with developing that same subtype 14. There are three main mechanisms through which infection increases lymphoma risk: direct transformation of lymphocytes, immunosuppression, and chronic antigenic stimulation 15. Rheumatoid arthritis, systemic lupus erythematosus, Sjögren syndrome, dermatomyositis, and celiac disease are inflammatory conditions that increase the risk of lymphoma through disease-specific causes and the chronic use of immunosuppressive medications 16.
Lymphoma diagnosis
Tests and procedures used to diagnose lymphoma include:
- Physical exam. Your doctor may examine your body to look for signs of enlarged lymph nodes.
- Removing a lymph node for testing. Your doctor may recommend a lymph node biopsy procedure to remove all or part of a lymph node for laboratory testing. Advanced tests can determine if lymphoma cells are present and what types of cells are involved.
- Blood tests. Blood tests to count the number of cells in a sample of your blood can give your doctor clues about your diagnosis.
- Removing a sample of bone marrow for testing. A bone marrow biopsy and aspiration procedure involves inserting a needle into your hipbone to remove a sample of bone marrow. The sample is analyzed to look for lymphoma cells.
- Imaging tests. Imaging tests may be used to look for signs of lymphoma in other areas of your body. Tests may include CT, MRI and positron emission tomography (PET).
Other tests and procedures may be used depending on your situation. Research shows that having a biopsy sample reviewed by an expert pathologist improves the chances for an accurate diagnosis. Consider getting a second opinion from a specialist who can confirm your diagnosis.
The diagnosis of lymphoma is made using an open lymph node biopsy, based off morphology, immunohistochemistry, and flow cytometry 17. Although fine-needle aspiration and core needle biopsy are often part of the initial evaluation of any enlarged lymph node, neither will provide adequate tissue for the diagnosis of lymphoma because of the need to verify Hodgkin lymphoma via the presence of Reed-Sternberg cells 18.
Lymphoma Staging
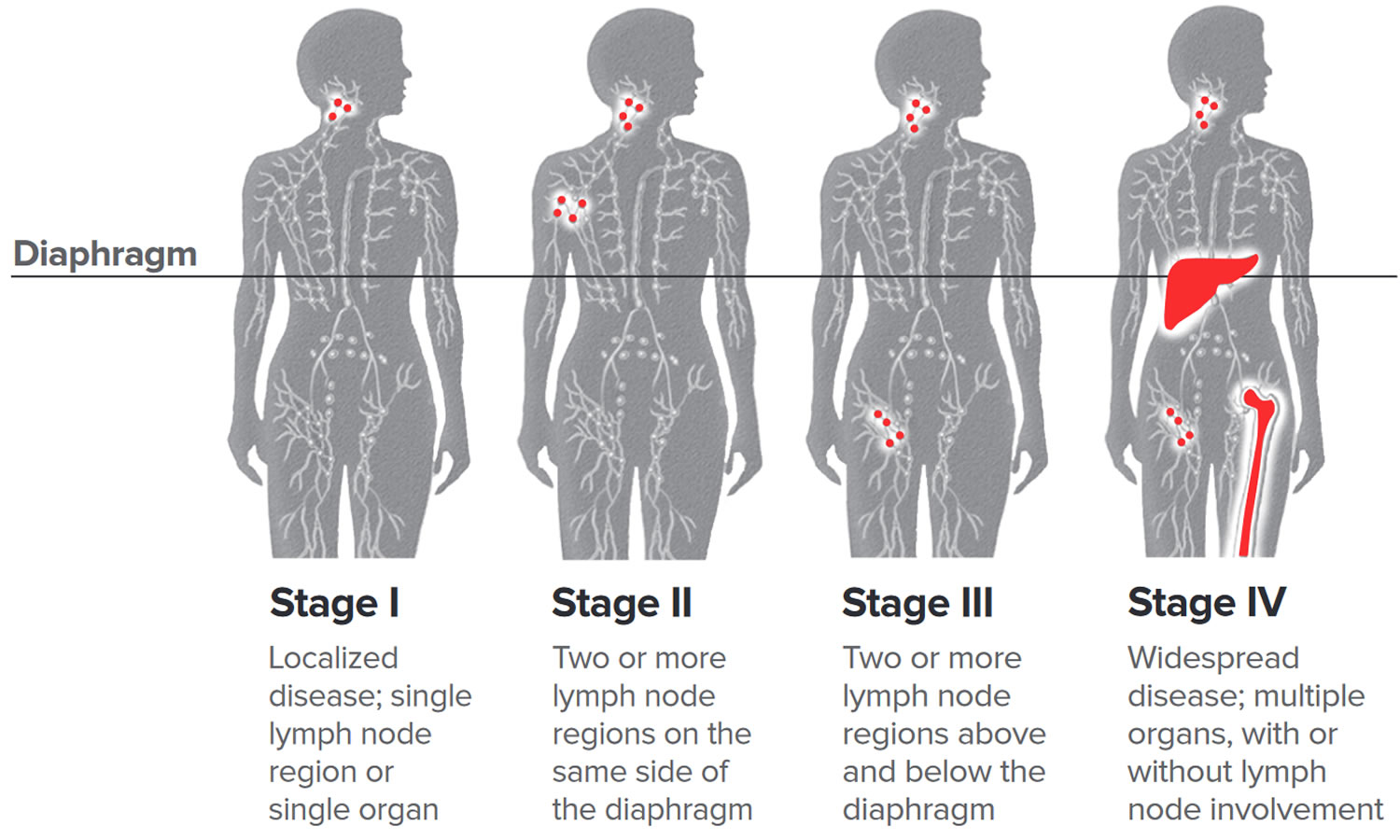
The Ann Arbor staging system was initially developed in 1971 for Hodgkin lymphoma and was later adapted for non-Hodgkin lymphoma. The Lugano classification system further modified staging by incorporating positron emission tomography/computed tomography (PET-CT) results to determine the staging of the lymphoma (Table 3) 19. PET-CT is used for fluorodeoxyglucose-avid lymphoma subtypes, with symptoms alone being used for staging the remaining subtypes. The new staging system incorporates two symptom-based classifications: A (absence of symptoms) and B (presence of fever, weight loss, and night sweats) for Hodgkin lymphoma. A bone marrow biopsy is now recommended only for diffuse large B-cell lymphoma with a negative PET-CT result 19.
Table 3. Lugano Classification for Lymphoma Staging
| Stage* | Description of disease from positron emission tomography/computed tomography results |
|---|---|
| I | Single nodal group or single extralymphatic lesion |
| II† | Multiple nodal groups on same side of diaphragm or with limited contiguous extralymphatic involvement |
| III | Multiple nodal groups on both sides of the diaphragm; may involve the spleen |
| IV | Noncontiguous extralymphatic involvement |
Footnotes:
* Staging for Hodgkin lymphoma is further subdivided for systemic symptoms; A for absence of symptoms or B for fevers > 101.3°F (38.5°C), drenching night sweats, or 10% (of body weight) unintentional weight loss over the past six months.
† Stage II may also be classified as bulky disease (> 10-cm mass), which may be treated as limited or advanced disease based on several prognostic factors.
[Source 19 ]Lymphoma treatment
Your lymphoma treatment options will depend on your type of lymphoma, its aggressiveness, stage, your overall health, and your treatment goals. The goal of lymphoma treatment is to destroy as many cancer cells as possible and bring the disease into remission.
Lymphoma treatments include:
- Active surveillance. Some forms of lymphoma are very slow growing. You and your doctor may decide to wait to treat your lymphoma when it causes signs and symptoms that interfere with your daily activities. Until then, you may undergo periodic tests to monitor your condition.
- Chemotherapy. Chemotherapy is a drug treatment that uses chemicals to kill cancer cells. Chemotherapy is usually administered through a vein, but can also be taken as a pill, depending on the specific drugs you receive.
- Hodgkin’s lymphoma is treated with combined chemotherapy with ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine), Stanford V (a chemotherapy regimen consisting of mechlorethamine, doxorubicin, vinblastine, vincristine, bleomycin, etoposide, and prednisone), or BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) with radiotherapy.
- Non-Hodgkin’s lymphoma (NHL) is treated with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) with or without rituximab (R-CHOP), bendamustine, and lenalidomide.
- Other drug therapy. Other drugs used to treat lymphoma include targeted drugs that focus on specific abnormalities within your cancer cells that allow them to survive. Immunotherapy drugs use your immune system to kill cancer cells. A specialized treatment called chimeric antigen receptor (CAR)-T cell therapy takes your body’s germ-fighting T cells, engineers them to fight cancer and infuses them back into your body.
- Radiation therapy. Radiation therapy uses powerful beams of energy, such as X-rays and protons, to kill cancer cells.
- Bone marrow transplant. Bone marrow transplant, also known as a stem cell transplant, involves using high doses of chemotherapy and radiation to suppress your bone marrow. Then healthy bone marrow stem cells from your body or from a donor are infused into your blood where they travel to your bones and rebuild your bone marrow.
Treatment of lymphoma consists of chemotherapy alone or in combination with radiotherapy 20. Radiotherapy alone is not recommended 21. Toxicity from radiotherapy can lead to serious long-term complications such as secondary cancers in the irradiated area, including breast or lung cancers 21. Additionally, patients receiving chemotherapy can subsequently develop breast or lung cancers, melanoma, or acute myeloid leukemia 22. Patients who are older than 60 years at diagnosis have worse outcomes, regardless of the staging. The National Comprehensive Cancer Network (NCCN) recommends avoiding certain chemotherapeutic agents in patients older than 60 years. The physician should focus on shared decision-making when discussing treatment options with all patients, but particularly for those older than 60 years, including whether the patient should pursue treatment 21.
The standard treatment for Hodgkin’s lymphoma is ABVD (doxorubicin [Adriamycin], bleomycin, vinblastine [Velban], and dacarbazine), but other regimens such as the Stanford V (doxorubicin, vinblastine, mechlorethamine, etoposide [Toposar], vincristine, bleomycin, and prednisone) and escalated-BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine [Matulane], and prednisone) can be used 20. Treatment for non-Hodgkin lymphoma varies depending on the histology, but often uses treatments such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) with or without rituximab (Rituxan; R-CHOP), a monoclonal antibody specific for CD20-positive B lymphocytes 23. Other medications such as bendamustine (Bendeka), an alkylating agent, and lenalidomide (Revlimid) are also used in many non-Hodgkin lymphoma treatments 24, 25. Common complications of these therapies are listed in Table 4 below.
A Cochrane review that examined seven trials consisting of more than 2,500 adult patients with early Hodgkin lymphoma concluded that the use of combined therapy could increase progression-free survival with little difference between the overall survival rates 26. Short-term complications from radiotherapy include nausea, vomiting, headaches, fatigue, and dermatitis. Radiotherapy can also lead to long-term complications, including cardiac and pulmonary toxicity, hypothyroidism, or breast or lung cancers 27. Radiotherapy can be avoided in patients with stage IA or IIA lymphoma without bulky disease (see Table 3 Lugano Classification for Lymphoma Staging above) 21.
Table 4. Common Chemotherapy Regimens for Lymphoma and their complications
| Therapy | Regimen | Short-term complications | Long-term complications |
|---|---|---|---|
| Hodgkin’s lymphoma | |||
| ABVD | Doxorubicin (Adriamycin) | Nausea/vomiting Alopecia Neutropenia Neuropathy Bleomycin-induced pulmonary toxicity | Cardiotoxicity (heart failure) Neuropathy Pulmonary fibrosis Increased risk of myocardial infarction |
| Bleomycin | |||
| Vinblastine (Velban) | |||
| Dacarbazine | |||
| Stanford V | Doxorubicin | Nausea/vomiting Fatigue Pulmonary toxicity Neuropathy | Neuropathy Pulmonary fibrosis Cardiotoxicity Rarely solid secondary malignancies of breast, lung, and skin |
| Vinblastine | |||
| Mechlorethamine | |||
| Etoposide (Toposar) | |||
| Vincristine | |||
| Bleomycin | |||
| Prednisone | |||
| Escalated-BEACOPP | Bleomycin | Anemia Leukopenia Thrombocytopenia Nausea/vomiting Infection Disulfiram reaction between ethanol and procarbazine | Acute myeloid leukemia Sterility/infertility |
| Etoposide | |||
| Doxorubicin (Adriamycin) | |||
| Cyclophosphamide | |||
| Vincristine (Oncovin) | |||
| Procarbazine (Matulane) | |||
| Prednisone | |||
| Non-Hodgkin’s lymphoma | |||
| CHOP | Cyclophosphamide | Heart failure Constipation Hyperglycemia Neuropathy | Cardiomyopathy Myelosuppression Neuropathy |
| Doxorubicin | |||
| (Hydroxydaunorubicin) | |||
| Vincristine (Oncovin) | |||
| Prednisone | |||
| R-CHOP | Rituximab (Rituxan) + CHOP | Reactivate hepatitis B infection | Progressive multifocal leukoencephalopathy |
Immunizations
All patients with lymphoma should receive pneumococcal vaccination initially with a 13-valent pneumococcal conjugate vaccine (Prevnar 13), followed at least eight weeks later by a 23-valent pneumococcal polysaccharide vaccine (PPSV23; Pneumovax 23) and then another PPSV23 at least five years later 28. Patients receiving anti–B-cell antibodies should not receive annual influenza vaccination, and administration of live vaccines is contraindicated during chemotherapy. Routine vaccinations recommended by the Centers for Disease Control and Prevention (CDC) should resume, including any recommended inactivated or live vaccines three months after chemotherapy or six months after anti–B-cell antibody therapy 29. Patients receiving a hematopoietic stem cell transplant should receive a series of three doses of Haemophilus influenzae type B vaccine starting six to 12 months after a successful transplant. Household contacts should receive appropriate CDC-recommended immunizations 30.
Treatment follow-up
PET-CT scans, and subsequent Deauville scoring (Table 5), should be used to assess the response to chemotherapy in non-Hodgkin and Hodgkin lymphoma 21, 24, 25, 31. A score of 3 or less is considered complete remission in non-Hodgkin lymphoma and should conclude the current treatment course. A score of 4 or 5 is an indicator to consider escalating therapy 21. Patients with Hodgkin lymphoma with a Deauville score of 1 or 2 have been shown to have similar progression and mortality outcomes between radiotherapy and no further treatment 26. Patients who receive a score of 3 or 4 should receive additional chemotherapy and/or radiotherapy, and a score of 5 indicates the need for a biopsy (excisional or core needle) in addition to chemotherapy and radiotherapy 21. A positive biopsy should be considered refractory disease 21.
Table 5. Deauville Score for Assessing PET-CT Scans
| PET-CT finding | Score |
|---|---|
| No FDG uptake related to lymphoma | 1 |
| FDG uptake at lymphoma site is ≤ mediastinum FDG uptake | 2 |
| FDG uptake at lymphoma site is > mediastinum FDG uptake but < liver FDG uptake | 3 |
| FDG uptake at lymphoma site is > liver FDG uptake at any site | 4 |
| FDG uptake at lymphoma site is substantially > liver FDG uptake or new FDG uptake sites found | 5 |
Abbreviations: FDG = fluorodeoxyglucose; PET-CT = positron emission tomography/computed tomography
[Source 32 ]Lymphoma Surveillance
Patients who have achieved remission need routine surveillance to monitor for complications and relapse, as well as age-appropriate screenings recommended by the U.S. Preventive Services Task Force 33. Complications of lymphoma treatment include secondary malignancies (e.g., breast, lung, skin, colon), cardiac disease, infertility, and endocrine, neurologic, and psychiatric dysfunctions. Current National Comprehensive Cancer Network guidelines outline specific monitoring parameters for follow-up and prevention of secondary disease (Table 6) 21. The extent and frequency of follow-up specifically depend on the histologic subtype of lymphoma. Patients should follow up with an oncologist every three to six months for the first two years, every six to 12 months until year 3, then annually thereafter. After five years of being cancer free, the patient can be transitioned to a primary care physician 34.
If a patient is asymptomatic, routine surveillance imaging does not improve outcomes or provide a clinical benefit 34, 35. Surveillance imaging should be used in patients who have reported symptoms or who are at high risk of relapse in a place that would not be easily examined, and who would be candidates for treatment. However, National Comprehensive Cancer Network imaging guidelines for lymphoma surveillance state that it is acceptable to perform chest radiography or CT of the chest every six to 12 months for the first two years and then yearly for the next three to five years posttreatment 36. Surveillance imaging with PET-CT scans following complete remission is not recommended 34. Disease marker research is ongoing, examining minimal residual disease measurements, a polymerase chain reaction–based method that looks at identifying tumor-specific DNA sequences 35.
Table 6. Lymphoma Surveillance for up to Five Years Post-Treatment
| Cancer screening | Laboratory screening | Cardiac screening | Counseling | Immunizations |
|---|---|---|---|---|
| Breast: annual screening mammography starting at age 40; history of chest or axilla radiation: start eight to 10 years after treatment or at age 40, whichever comes first; consider annual breast magnetic resonance imaging if chest radiation was received between ages 10 and 30; consider referral to breast subspecialist to discuss possible chemoprevention | Complete blood count, fasting blood glucose, and comprehensive metabolic panel annually | Annual blood pressure screening, lifestyle modification, and treatment of obesity, hypertension, and tobacco use | Annual depression screening | Age-appropriate immunizations per the Centers for Disease Control and Prevention schedule, including annual influenza vaccine; resume live vaccines at least three months after completion of chemotherapy |
| Routine surveillance tests for cervical, colorectal, lung, and prostate cancers per the USPSTF guidelines | Lipid profile per the USPSTF guidelines | Consider stress test and/or echocardiography at 10-year intervals (frequency of testing based on findings and other associated risk factors) | Neurocognitive impairment screening for any patient who is high risk (e.g., history of brain radiation or intrathecal treatment) | PCV13 (Prevnar 13), followed by PPSV23 (Pneumovax 23) at least eight weeks later and again at least five years later |
| Thyroid-stimulating hormone annually if neck irradiation | Carotid ultrasonography every 10 years if neck irradiation | Infertility: consider reproductive endocrinologist referral | Haemophilus influenzae type b: three doses following hematopoietic stem cell transplantation |
Abbreviations: PCV13 = 13-valent pneumococcal conjugate vaccine; PPSV23 = 23-valent pneumococcal polysaccharide vaccine; USPSTF = U.S. Preventive Services Task Force.
[Source 5 ]Lymphoma coping and support
A lymphoma diagnosis can be overwhelming and scary. With time you’ll find ways to cope with the distress and uncertainty of cancer. Until then, you may find it helps to:
- Learn enough about lymphoma to make decisions about your care. Ask your doctor about your lymphoma, including your type, your treatment options and, if you like, your prognosis. As you learn more about lymphoma, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your lymphoma. Friends and family can provide the practical support you’ll need, such as helping take care of your house if you’re in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
- Find someone to talk with. Find a good listener with whom you can talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your doctor about support groups in your area. You might also contact a cancer organization such as the National Cancer Institute (https://www.cancer.org) or the Leukemia and Lymphoma Society (https://www.lls.org).
Lymphoma relapse
Relapse rates for non-Hodgkin lymphoma are variable and based on the specific subtype. The most common subtype, diffuse large B-cell lymphoma, has a 40% lifetime relapse rate 37. Lifetime relapse in Hodgkin lymphoma occurs in 10% to 15% of patients with early stage disease and 40% of patients with advanced stage disease 38.
Lymphoma prognosis
The International Prognostic Index is used broadly for all subtypes of non-Hodgkin lymphoma 39 and the International Prognostic Score is used for Hodgkin lymphoma 40.
Table 7. Lymphoma International Prognostic Index
| Non-Hodgkin lymphoma | Hodgkin lymphoma |
|---|---|
| International Prognostic Index | International Prognostic Score |
| Criteria | Criteria |
| Age > 60 | Age > 45 |
| Elevated serum lactate dehydrogenase | Male sex |
| Eastern Cooperative Oncology | Serum albumin concentration < 4.0 g per dL (40 g per L) |
| Group performance status ≥ 2* | Hemoglobin concentration < 10.5 g per dL (105 g per L) |
| Ann Arbor stage III or IV disease† | |
| Extranodal sites > 1 | Ann Arbor stage IV disease† Leukocytosis (≥ 15,000 μL [15 × 109 white blood cells per L]) Lymphopenia (< 600 lymphocytes per μL [0.6 × 109 per L], or < 8% of total white blood cell count) |
| Total score____ | Total score____ |
| Five-year overall survival rate based on number of criteria from International Prognostic Index/Score | |
| Score 0 or 1 = 73% | Score 0 = 89% |
| Score 2 = 51% | Score 1 = 90% |
| Score 3 = 43% | Score 2 = 81% |
| Score 4 or 5 = 26% | Score 3 = 78% |
| Score 4 = 61% | |
| Score ≥ 5 = 56% | |
Footnote: Each criterion = 1 point.
* Eastern Cooperative Oncology Group performance status: 0 = fully active, 1 = ambulatory but restricted to light work, 2 = ambulatory but unable to carry out activities, 3 = limited self-care only, 4 = bedridden, 5 = dead.
† Ann Arbor stage III = multiple nodal groups on both sides of the diaphragm, may involve the spleen; stage IV = noncontiguous extralymphatic involvement.
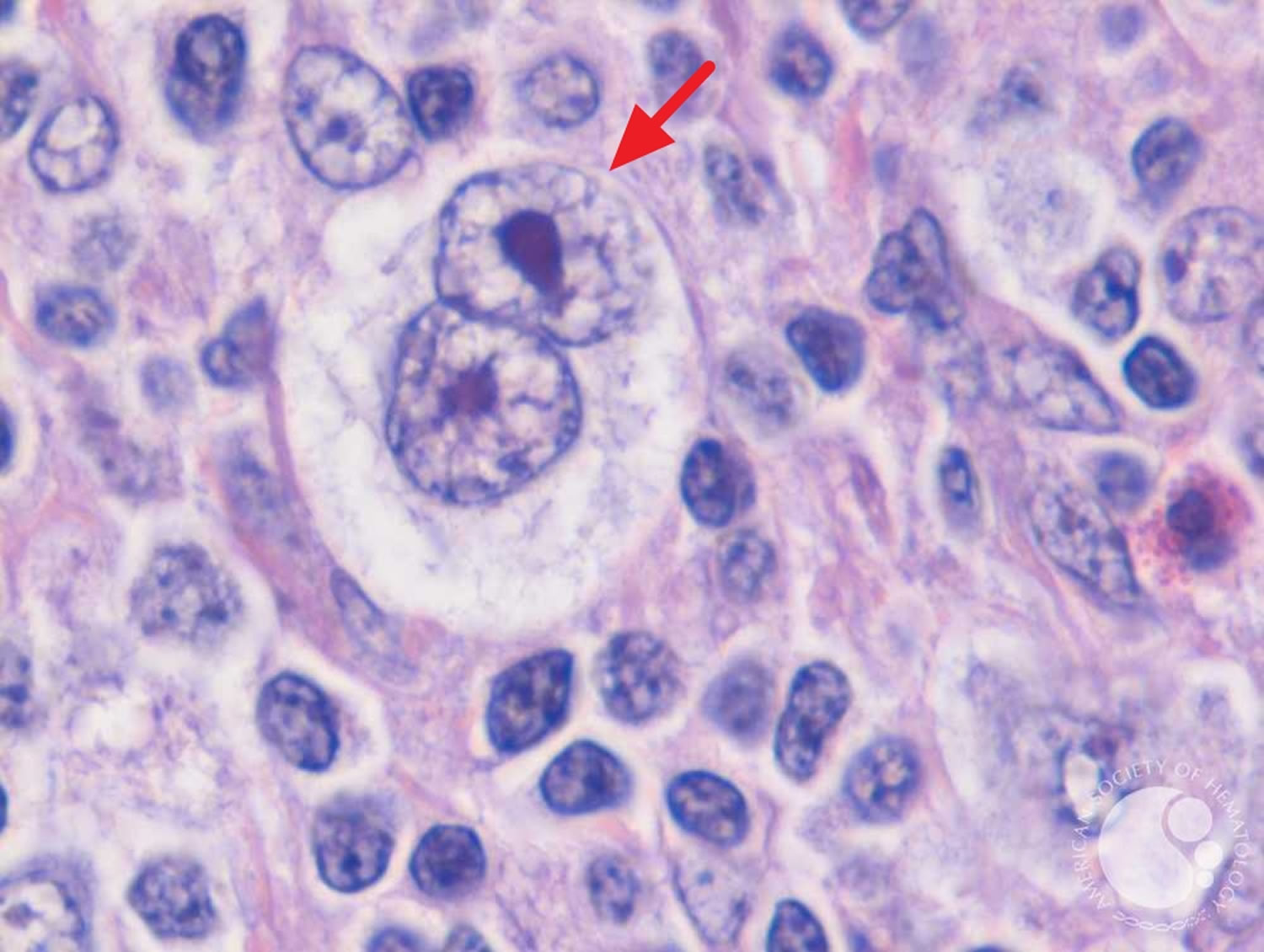
Hodgkin’s lymphoma
Hodgkin lymphoma also called Hodgkin’s disease is an uncommon cancer that develops in the lymphatic system that is marked by the presence of a type of cell called the Reed-Sternberg cell (see Figure 1). The two major types of Hodgkin lymphoma are classic Hodgkin lymphoma and nodular lymphocyte-predominant Hodgkin lymphoma 41. Classical Hodgkin lymphoma accounts for approximately 95% of all Hodgkin’s lymphoma, and it is further subdivided into four subgroups: nodular sclerosis Hodgkin lymphoma (NSHL), lymphocyte-rich Hodgkin lymphoma (LRHL), mixed cellularity Hodgkin lymphoma (MCHL), and lymphocyte-depleted Hodgkin lymphoma (LDHL) 42. Although Hodgkin lymphoma can start almost anywhere, most often it starts in lymph nodes in the upper part of the body. The most common sites are in the chest, neck, or under the arms. Signs and symptoms of Hodgkin lymphoma include painless, swollen lymph nodes (lymphadenopathy), an enlarged spleen, fever, weight loss, fatigue, and night sweats.
Hodgkin lymphoma is named after Dr. Thomas Hodgkin who, in 1832, described several cases of people with symptoms of a cancer involving the lymph nodes. The disease was called “Hodgkin’s disease” until it was officially renamed “Hodgkin lymphoma” in the late 20th century.
Hodgkin lymphoma is distinguished from other types of lymphoma primarily by the presence of two types of cells, referred to as Hodgkin cells and Reed-Sternberg cells, named after the scientists who first identified them. Reed-Sternberg cells are large, abnormal B lymphocytes that often have more than one nucleus and an owl-like appearance (Figure 1). Hodgkin cells are larger than normal lymphocytes, but smaller than Reed-Sternberg cells. These differences can be observed under a microscope and further identified by special pathology tests. This is important information that helps doctors determine a patient’s Hodgkin lymphoma subtype.
Hodgkin lymphoma starts when an abnormal change to the DNA of a white blood cell called a lymphocyte causes it to become a lymphoma cell that, if untreated, results in the uncontrolled growth of cancerous lymphocytes.
- These cancerous cells crowd out normal white cells, and the immune system can’t guard against infection effectively.
- Lymphoma cells grow and form masses, usually in the lymph nodes, located throughout our bodies in the lymphatic system.
- Lymphoma cells can also gather in other areas of the body where lymphoid tissue is found.
- Hodgkin lymphoma is distinguished from other types of lymphoma by the presence of Reed-Sternberg cells (named for the scientists who first identified them). Other cells associated with the disease are called Hodgkin cells.
Hodgkin lymphoma most often spreads through the lymph vessels from lymph node to lymph node. Rarely, late in the disease, it can invade the bloodstream and spread to other parts of the body, such as the liver, lungs, and/or bone marrow.
The American Cancer Society’s estimates for Hodgkin disease (Hodgkin’s lymphoma) in the United States for 2022 are 43, 44:
- New cases: About 8,540 new cases (4,570 in males and 3,970 in females)
- Deaths: About 920 deaths (550 males and 370 females)
- 5-Year Relative Survival: 89.1%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Percentage of All Cancer Deaths: 0.2%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of Hodgkin lymphoma was 2.6 per 100,000 men and women per year. The death rate was 0.3 per 100,000 men and women per year. These rates are age-adjusted and based on 2015–2019 cases and deaths.
- Lifetime Risk of Developing Cancer: Approximately 0.2 percent of men and women will be diagnosed with Hodgkin lymphoma at some point during their lifetime, based on 2017–2019 data.
- In 2019, there were an estimated 218,740 people living with Hodgkin lymphoma in the United States.
Both children and adults can develop Hodgkin lymphoma, but it is most common in early adulthood (especially in a person’s 20s). The risk of Hodgkin lymphoma rises again in late adulthood (after age 55). Overall, the average age of people when they are diagnosed is 39.
Hodgkin lymphoma is rare in children younger than 5 years of age. About 10% to 15% of cases are diagnosed in children and teenagers ages 15 to 19 years.
Survival rates have improved in the past few decades, largely due to advances in treatment. More than 75% of all newly diagnosed patients with adult Hodgkin lymphoma can be cured with combination chemotherapy and/or radiation therapy 45. The 5-year relative survival rate for all patients diagnosed with Hodgkin lymphoma is now about 89.1%, and the 10-year relative survival rate is about 80%. Certain factors such as the stage (extent) of Hodgkin lymphoma and a person’s age affect these rates.
Many types of Hodgkin’s lymphoma exist, including rare forms that are difficult for inexperienced pathologists to identify. Accurate diagnosis and staging are key to developing a treatment plan. Research shows that review of biopsy tests by pathologists who aren’t experienced with lymphoma results in a significant proportion of misdiagnoses. Get a second opinion from a specialist if needed.
Figure 4. Reed Sternberg cells seen in classical Hodgkin’s lymphoma
Footnote: Reed-Sternberg cells are large, abnormal lymphocytes (a type of white blood cell) that may contain more than one nucleus. Reed-Sternberg cells are found in people with Hodgkin lymphoma. Reed-Sternberg cells are also called Hodgkin and Reed-Sternberg cells.
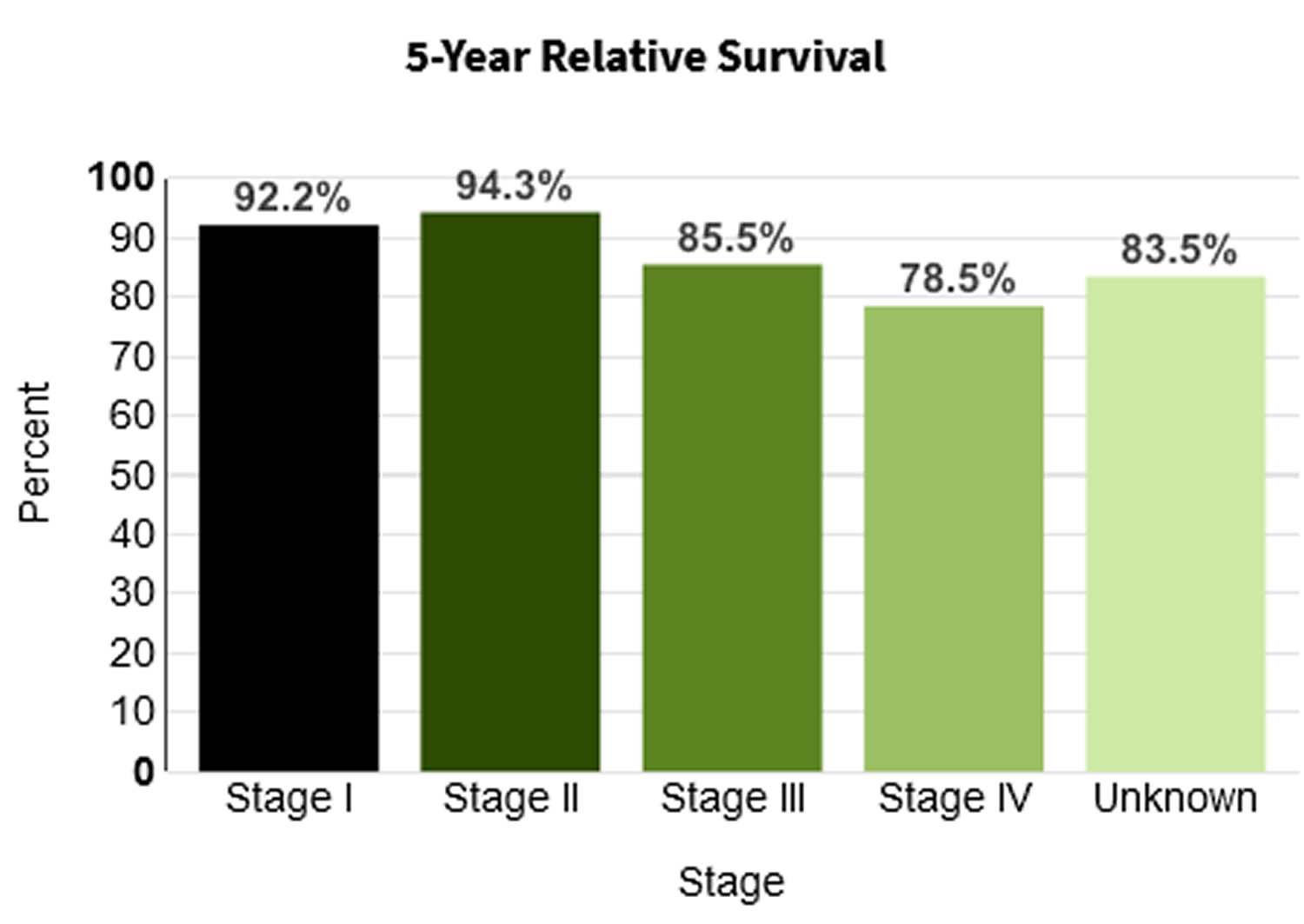
Survival rates for Hodgkin’s lymphoma
The numbers below come from the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program 46 database, looking at more than 8,000 people diagnosed with Hodgkin lymphoma between 1988 and 2001.
- The 5-year survival rate for people with stage I Hodgkin lymphoma is about 92.2%.·
- For stage II Hodgkin lymphoma, the 5-year survival rate is about 94.3%.
- The 5-year survival rate for stage III Hodgkin lymphoma is about 85.5%.
- Stage IV Hodgkin lymphoma has a 5-year survival rate of about 78.5%.
Based on data from SEER (Surveillance, Epidemiology, and End Results Program at the National Cancer Institute) 2011-2017, percent surviving 5 Years is 88.3% 47.
Figure 5. 5-year relative survival rates for Hodgkin lymphoma
Footnote: A relative survival rate compares people with the same type and stage of Hodgkin’s lymphoma to people in the overall population. For example, if the 5-year survival rate for a specific stage of Hodgkin lymphoma is 88.3%, it means that people who have that cancer are, on average, about 88.3% as likely as people who don’t have that cancer to live 5 years after being diagnosed.
- These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment.
- These numbers don’t take everything into account. Survival rates are grouped based on how far the cancer has spread, but your age, overall health, how well the cancer responds to treatment, and other prognostic factors (described below) can also affect your outlook.
- People now being diagnosed with Hodgkin lymphoma may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
Hodgkin’s lymphoma Survival by Stage
Cancer stage at diagnosis, which refers to extent of a cancer in the body, determines treatment options and has a strong influence on the length of survival. In general, if the cancer is found only in the part of the body where it started it is localized (sometimes referred to as stage 1). If it has spread to a different part of the body, the stage is regional or distant. For Hodgkin lymphoma, 15.6% are diagnosed at the local stage. The 5-year survival for localized Hodgkin lymphoma is 92.2%.
Remember, these survival rates are only estimates – they can’t predict what will happen to any individual person. We understand that these statistics can be confusing and may lead you to have more questions. Talk to your doctor to better understand your specific situation.
Other prognostic factors
Along with the stage of the Hodgkin lymphoma, other factors can affect a person’s prognosis (outlook). For example, having some factors means the lymphoma is likely to be more serious:
- Having B symptoms or bulky disease
- Being older than 45
- Being male
- Having a high white blood cell count (above 15,000)
- Having a low red blood cell count (hemoglobin level below 10.5)
- Having a low blood lymphocyte count (below 600)
- Having a low blood albumin level (below 4)
- Having a high erythrocyte sedimentation rate, or ESR (over 30 in someone with B symptoms, or over 50 for someone without B symptoms)
Some of these factors are used to help divide stage I or II Hodgkin lymphoma into favorable and unfavorable groups, which can affect how intense the treatment needs to be (see Hodgkin’s lymphoma staging below).
Types of Hodgkin’s lymphoma
The World Health Organization (WHO) divides Hodgkin lymphoma into two main subtypes. They are:
- Classic Hodgkin lymphoma (cHL)
- Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL)
Classic Hodgkin lymphoma (cHL) is characterized by the presence of Reed-Sternberg cells. Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL) is characterized by the presence of lymphocyte-predominant cells, sometimes termed “popcorn cells,” and Reed-Sternberg cells are not found.
It’s important to know your subtype since it plays a large part in determining the type of treatment you’ll receive.
Classic Hodgkin’s lymphoma
Classic Hodgkin’s lymphoma (cHL) accounts for about 95% of all cases of Hodgkin’s lymphomas in developed countries 48.
The cancer cells in Classic Hodgkin’s lymphoma (cHL) are called Reed-Sternberg cells. These cells are usually an abnormal type of B lymphocyte. Enlarged lymph nodes in people with Classic Hodgkin’s lymphoma (cHL) usually have a small number of Reed-Sternberg cells and a large number of surrounding normal immune cells. These other immune cells make up most of the enlarged lymph nodes.
Classic Hodgkin’s lymphoma has 4 subtypes:
- Nodular sclerosis Hodgkin lymphoma (NSCHL): This is the most common type of Hodgkin lymphoma in developed countries. It accounts for about 7 out of 10 cases. It is most common in teens and young adults, but it can occur in people of any age. It tends to start in lymph nodes in the neck or chest.
- Mixed cellularity Hodgkin lymphoma (MCCHL): This is the second most common type, found in about 4 out 10 cases. Mixed cellularity Hodgkin lymphoma (MCCHL) is seen mostly in people with HIV infection. It’s also found in children or the elderly . It can start in any lymph node but most often occurs in the upper half of the body.
- Lymphocyte-rich Hodgkin lymphoma: Lymphocyte-rich Hodgkin lymphoma isn’t common. It usually occurs in the upper half of the body and is rarely found in more than a few lymph nodes.
- Lymphocyte-depleted Hodgkin lymphoma: This is the least common form of Hodgkin lymphoma. Lymphocyte-depleted Hodgkin lymphoma is seen mainly in older people and those with HIV infection. It’s more aggressive than other types of Hodgkin lymphoma and likely to be advanced when first found. It’s most often in lymph nodes in the abdomen (belly) as well as in the spleen, liver, and bone marrow.
Table 8. Classic Hodgkin’s Lymphoma Subtypes
| Subtype | Characteristics |
|---|---|
| Nodular sclerosis Hodgkin lymphoma (NSCHL) | Accounts for 70 percent of classical Hodgkin lymphoma cases Most common type in young adults Involved lymph nodes contain scar tissue (sclerosis) Incidence similar in males and females Highly curable B symptoms in approximately 40 percent of cases |
| Mixed cellularity Hodgkin lymphoma (MCCHL) | Accounts for 20-25 percent of classical Hodgkin lymphoma cases Most common in older adults More common in males Prevalent in patients with HIV (human immunodeficiency virus) infection Involved lymph nodes contain Reed-Sternberg cells and several other cell types B symptoms common |
| Lymphocyte-rich Hodgkin lymphoma | Accounts for approximately 5 percent of classical Hodgkin lymphoma cases Involved lymph nodes contain numerous normal-appearing lymphocytes and Reed-Sternberg cells Usually diagnosed at an early stage More common in males B symptoms are rare |
| Lymphocyte-depleted Hodgkin lymphoma | Rarest classical Hodgkin lymphoma subtype, less than 1 percent of all classical Hodgkin lymphoma cases Involved lymph nodes contain few normal lymphocytes and numerous Reed-Sternberg cells Median age range 30-37 years Prevalent in patients with HIV infection Usually diagnosed at an advance stage B symptoms common |
Nodular lymphocyte predominant Hodgkin’s lymphoma
Nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) accounts for about 5% of cases. The cancer cells in nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) are large cells called popcorn cells (because they look like popcorn), which are variants of Reed-Sternberg cells. You may also hear these cells called lymphocytic and histiocytic (L&H) cells.
Nodular lymphocyte predominant Hodgkin lymphoma usually starts in lymph nodes in the neck and under the arm. It can occur in people of any age, and is more common in men than in women. This type of Hodgkin’s lymphoma is treated differently from the classic Hodgkin lymphoma (cHL).
The following are some characteristics of nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL):
- Most common in 30 to 50 year-old age group
- More common in male than in female patients
- NLPHL is slow growing (indolent) and highly curable.
- Small risk (3-5 percent of cases) of transformation to aggressive non-Hodgkin lymphoma.
Hodgkin’s Lymphoma causes
The exact cause of Hodgkin’s lymphoma is unknown. Scientists have found some risk factors that make a person more likely to get Hodgkin disease, but it’s not always clear exactly how these factors might increase risk.
Your risk of developing Hodgkin’s lymphoma is increased if:
- you have a medical condition that weakens your immune system
- you take immunosuppressant medicine
- you’ve previously been exposed to a common virus called the Epstein-Barr virus (EBV), which causes infectious mononucleosis or glandular fever. Some researchers think that infection with the Epstein-Barr virus (EBV) may sometimes cause DNA changes in B lymphocytes, leading to the development of Reed-Sternberg cells, which are the cancer cells in Hodgkin lymphoma.
You also have an increased risk of developing Hodgkin lymphoma if a first-degree relative (parent, sibling or child) has had the condition, it’s not clear if this is because of an inherited genetic fault or lifestyle factors. However, these cases are uncommon and some experts are studying whether some people have a genetic predisposition to Hodgkin lymphoma.
Hodgkin lymphoma is caused by a change (mutation) in the DNA of a type of white blood cell called B lymphocytes. The exact reason why this happens isn’t known.
DNA is the chemical in your cells that makes up your genes, which control how your cells function. You look like your parents because they are the source of your DNA. But DNA affects more than just how you look.
Some genes control when cells grow, divide into new cells, and die:
- Genes that help cells grow, divide, and stay alive are called oncogenes.
- Genes that slow down cell division or cause cells to die at the right time are called tumor suppressor genes.
Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes.
Scientists have found many gene changes in Reed-Sternberg cells that help the cells grow and divide or live longer than they should. Reed-Sternberg cells also make substances called cytokines, which attract many other cells into the lymph node, enlarging it. In turn, these non-cancerous cells release substances that further help Reed-Sternberg cells grow.
Despite these advances, scientists do not yet know what sets off these processes. An abnormal reaction to infection with Epstein-Barr virus (EBV) or to other infections may be the trigger in some cases. But more research is needed to understand what causes Hodgkin lymphoma.
Hodgkin’s lymphoma Risk Factors
The following risk factors may increase a person’s likelihood of developing Hodgkin lymphoma:
- The Epstein-Bar virus (EBV), known for causing infectious mononucleosis, is associated with the development of Hodgkin lymphoma. The exact role of EBV in the development of Hodgkin lymphoma is not clear. Many people are infected with EBV, but very few develop Hodgkin lymphoma. Parts of the virus are found in Reed-Sternberg cells in about 1 out of 3 people with Hodgkin lymphoma. But most people with Hodgkin lymphoma have no signs of EBV in their cancer cells.
- Having a medical condition that weakens your immune system, such as being infected with human immunodeficiency virus (HIV), the virus that causes AIDS, have increased probability of developing Hodgkin lymphoma.
- Having medical treatment that weakens your immune system, for example, taking medicine to suppress your immune system after an organ transplant.
- Having previously had non-Hodgkin lymphoma, possibly because of treatment with chemotherapy or radiotherapy
- There are occasional cases of Hodgkin lymphoma in families-having a parent or a sibling with Hodgkin lymphoma may increase the risk of developing the disease. These cases are uncommon, but some experts are studying whether some people have a genetic predisposition to Hodgkin lymphoma.
- Family history: Brothers and sisters of young people with this disease have a higher risk for Hodgkin lymphoma. The risk is very high for an identical twin of a person with Hodgkin lymphoma. But a family link is still uncommon – most people with Hodgkin lymphoma do not have a family history of it. It’s not clear why family history might increase risk. It might be because family members have similar childhood exposures to certain infections (such as Epstein-Barr virus), because they share inherited gene changes that make them more likely to get Hodgkin lymphoma, or some combination of these factors.
- Age: People can be diagnosed with Hodgkin lymphoma at any age, but it is most common in early adulthood (especially in a person’s 20s) and in late adulthood (after age 55).
- Gender: Hodgkin lyphoma occurs slightly more often in males than in females.
- Being very overweight (obese) – this may be more of a risk factor in women than men
- Smoking
- Geography: Hodgkin lymphoma is most common in the United States, Canada, and Europe, and is least common in African and Asian countries.
- Socioeconomic status: The risk of Hodgkin disease is greater in people with a higher socioeconomic background. The reason for this is not clear. One theory is that children from more affluent families might be exposed to some type of infection (such as Epstein-Barr virus) later in life than children from less affluent families, which might somehow increase their risk.
You can not catch Hodgkin lymphoma from someone else.
Hodgkin’s lymphoma prevention
Few of the known risk factors for Hodgkin lymphoma can be changed, so it’s not possible to prevent most cases of Hodgkin lymphoma at this time.
Infection with HIV, the virus that causes AIDS, is known to increase risk, so one way to limit your risk is to avoid known risk factors for HIV, such as intravenous (IV) drug use or unprotected sex with many partners.
Another risk factor for Hodgkin lymphoma is infection with the Epstein-Barr virus (the cause of infectious mononucleosis, or glandular fever), but there’s no known way to prevent this infection.
Hodgkin’s lymphoma signs and symptoms
The most common early sign of Hodgkin lymphoma is painless swelling (enlargement) of one or more lymph nodes. Most people have affected lymph nodes in the upper part of their body, usually the neck or upper chest. Sometimes the affected lymph nodes are in the armpit, stomach area or groin.
Hodgkin’s lymphoma doesn’t usually hurt, but the area may become painful after drinking alcohol. The lump might grow larger over time, or new lumps might appear near it (or even in other parts of the body).
But Hodgkin lymphoma is not the most common cause of lymph node swelling. Most enlarged lymph nodes, especially in children, are caused by an infection. Lymph nodes that grow because of infection are called reactive or hyperplastic nodes. These often hurt when they are touched. If an infection is the cause, the node should return to its normal size within a few weeks after the infection goes away.
Other cancers can also cause swollen lymph nodes. If you have an enlarged lymph node, especially if you haven’t had a recent infection, it’s best to see your doctor so that the cause can be found and treated without delay, if needed.
In addition to swollen lymph nodes, other signs and symptoms of Hodgkin lymphoma may include:
- Unexplained fever (100.4°F [38ºC] or higher)
- Persistent fatigue
- Persistent cough
- Shortness of breath during normal activity
- Drenching sweats, especially at night
- Unexplained weight loss (weight loss of 10% or more of baseline weight in the previous 6 months)
- Decreased appetite
- Itchy skin (pruritus), especially after bathing or after ingesting alcohol
- Abdominal pain or swelling and feeling of fullness (due to an enlarged spleen)
- Lymph node pain after drinking alcohol
A few people with Hodgkin lymphoma have abnormal cells in their bone marrow when they’re diagnosed. This may lead to:
- persistent tiredness or fatigue
- an increased risk of infections
- excessive bleeding – such as nosebleeds, heavy periods and spots of blood under the skin
Treatment of Hodgkin’s lymphoma should relieve these symptoms within days.
B symptoms
Fever, drenching night sweats and loss of more than 10 percent of body weight over six months are sometimes termed “B symptoms.” These symptoms are significant to the prognosis and staging of the disease.
Some Hodgkin lymphoma symptoms are associated with other, less serious illnesses. However, if you’re troubled by any of the above symptoms, see your doctor.
Hodgkin’s lymphoma diagnosis
Hodgkin lymphoma can be a difficult disease to diagnose because it can be confused with some types of non-Hodgkin lymphoma. Having the correct diagnosis is important for getting the right treatment. You may want to get a second medical opinion by an experienced hematopathologist before you begin treatment. A hematopathologist is a specialist who studies blood and bone marrow cells and other tissues to help diagnose diseases of the blood, bone marrow and lymph system.
If a person has signs or symptoms that suggest Hodgkin lymphoma, exams and tests will be done to find out for sure and, if so, to determine the exact type.
Medical history and physical exam
Your doctor will want to get a thorough medical history, including information about symptoms, possible risk factors, family history, and other medical conditions.
Next, the doctor will examine you, paying special attention to the lymph nodes and other areas of the body that might be affected, including the spleen and liver. Because infections are the most common cause of enlarged lymph nodes, especially in children, the doctor will look for an infection in the part of the body near any swollen lymph nodes.
The doctor also might order blood tests to look for signs of infection or other problems. If the doctor suspects that Hodgkin lymphoma might be causing the symptoms, he or she might recommend a biopsy of a swollen lymph node.
Lymph Node Biopsy
Diagnosing Hodgkin lymphoma usually involves performing a lymph node biopsy. The entire lymph node or part of the lymph node is surgically removed using a special needle. A hematopathologist examines the sample of the lymph node under a microscope to look for the identifying characteristics of Hodgkin lymphoma. If the biopsy confirms that you have Hodgkin lymphoma, the hematopathologist will categorize the Hodgkin lymphoma into one of several subtypes. .
The lymph node biopsy’s purpose is to confirm a diagnosis and:
- Identify your Hodgkin lymphoma subtype
- Develop a treatment plan
Immunophenotyping
The hematopathologist may use a lab test called immunophenotyping to distinguish Hodgkin lymphoma from other types of lymphoma or other cancerous or noncancerous conditions based on the antigens or markers on the surface of the cells.
Staging Tests
Once your hematologist-oncologist confirms a Hodgkin lymphoma diagnosis, he or she orders more tests to stage your disease. Staging identifies the extent of your disease and where it’s located in your body.
Staging tests include:
- Imaging tests
- Blood tests
- Bone marrow tests
Imaging Tests
Imaging tests help the doctor evaluate:
- The location and distribution of enlarged lymph nodes
- Whether organs other than lymph nodes are involved
- Whether there are very large masses of tumors in one site or another
Imaging tests may include:
- Chest X-ray
- CT (computed tomography) scan of the neck, chest, pelvis and abdomen (stomach area)
- FDG-PET (fluorodeoxyglucose [FDG] positron emission tomography [PET]) of the entire body with a radioactive tracer
- Combination PET-CT scan
- MRI (magnetic resonance imaging)
Blood Tests
Blood tests are used to:
- Assess blood counts including red blood cells, white blood cells and platelets;
- Determine whether lymphoma cells are present in the blood;
- Determine whether the immunoglobulins (proteins that fight infection) made by lymphocytes are deficient or abnormal;
- Check indicators of inflammation and disease severity such as blood protein levels, uric acid levels and erythrocyte sedimentation rate (ESR);
- Assess kidney and liver functions;
- Some women may have a pregnancy test.
Your doctor might also suggest other blood tests to look for signs of certain infections:
- HIV test: This may be done if you have abnormal symptoms that might be related to HIV infection.
- Hepatitis B and C virus test: Certain chemo drugs could cause problems if you have these infections.
Bone Marrow Tests
Your doctor may decide to examine your bone marrow to see whether the disease has spread to the bone marrow. Your doctor will decide if this procedure is necessary based on certain features such as the location of the disease in your body. Bone marrow testing may not be required for patients with early-stage disease and low-risk clinical features.
- Bone marrow testing involves two steps usually done at the same time in a doctor’s office or a hospital:
- A bone marrow aspiration to remove a liquid sample of bone marrow
Tests of heart and lung function
These tests might be done if certain chemo drugs that could affect the heart or the lungs are going to be used.
- An echocardiogram (an ultrasound of the heart) or a MUGA scan can be used to check heart function.
- Lung (pulmonary) function tests (PFTs) can be used to see how well the lungs are working.
Hodgkin Lymphoma Staging
Doctors use physical examinations, imaging tests, blood test and, sometimes, bone marrow tests to determine the extent of the disease. This determination is called “staging.” Staging provides important information for treatment planning.
Staging for Hodgkin lymphoma is based the Lugano classification, which is based on the older Ann Arbor system. It has 4 stages, labeled I, II, III, and IV.
For limited stage (I or II) Hodgkin’s lymphoma that affects an organ outside of the lymph system, the letter E is added to the stage (for example, stage IE or IIE).
- Stage I: The cancer is limited to one lymph node region or a single organ. Either of the following means that the Hodgkin’s lymphoma is stage I:
- Hodgkin’s lymphoma is found in only 1 lymph node area or lymphoid organ such as the thymus (I).
- The cancer is found only in 1 part of 1 organ outside the lymph system (IE).
- Stage II: In this stage, the cancer is in two lymph node regions or the cancer has invaded one organ and the nearby lymph nodes. But the cancer is still limited to a section of the body either above or below the diaphragm. Either of the following means that the Hodgkin’s lymphoma is stage II:
- Hodgkin’s lymphoma is found in 2 or more lymph node areas on the same side of (above or below) the diaphragm, which is the thin muscle beneath the lungs that separates the chest and abdomen (II).
- The cancer extends locally from one lymph node area into a nearby organ (IIE).
- Stage III: When the cancer moves to lymph nodes both above and below the diaphragm, it’s considered stage III. Either of the following means that the Hodgkin’s lymphoma is stage III:
- Hodgkin’s lymphoma is found in lymph node areas on both sides of (above and below) the diaphragm (III).
- Hodgkin’s lymphoma is in lymph nodes above the diaphragm and in the spleen.
- Stage IV: This is the most advanced stage of Hodgkin’s lymphoma. Hodgkin’s lymphoma has spread widely into at least one organ outside of the lymph system, such as the liver, bone marrow, or lungs.
Other modifiers may also be used to describe the Hodgkin lymphoma stage:
- Bulky disease. This term is used to describe tumors in the chest that are at least ⅓ as wide as the chest, or tumors in other areas that are at least 10 centimeters (about 4 inches) across. It’s usually labeled by adding the letter X to the stage. It’s especially important for stage II lymphomas, because bulky disease may require more intensive treatment.
- A vs. B. Each stage may also be assigned a letter A or B to indicate whether you’re experiencing symptoms of Hodgkin’s lymphoma:
- The letter A means that you don’t have any significant symptoms as a result of the cancer.
- The Letter B is added (for example stage IIIB) if a person has any of these B symptoms:
- Loss of more than 10% of body weight over the previous 6 months (without dieting)
- Unexplained fever of at least 100.4°F (38°C)
- Drenching night sweats
- If a person has any B symptoms, it usually means the lymphoma is more advanced, and more intensive treatment is often recommended. If no B symptoms are present, the letter A is added to the stage.
- Category E: The patient has Hodgkin lymphoma cells in organs or tissues outside the lymphatic system.
- Category S: The patient has Hodgkin lymphoma cells in the spleen.
Your treatment depends on your stage and category. Patients who fall into the B category usually need more aggressive treatment than A category patients do.
Resistant or recurrent Hodgkin lymphoma
Resistant or recurrent Hodgkin’s lymphoma is not part of the formal staging system, but doctors or nurses might use these terms to describe what’s going on with the lymphoma in some cases.
- The terms resistant or progressive disease are used when the lymphoma does not go away or progresses (grows) while you’re being treated.
- Recurrent or relapsed disease means that Hodgkin’s lymphoma went away with treatment, but it has now come back. If the lymphoma returns, it might be in the same place where it started or in another part of the body. This can happen shortly after treatment or years later.
Table 9. Hodgkin Lymphoma Stages
| Stage I | Involvement of one lymph node group or a group of adjacent nodes |
| Stage II | Involvement of two or more lymph node regions on the same side of the diaphragm (a thin muscle below the lungs) |
| Stage III | Involvement of lymph node groups on both sides of the diaphragm (for example, neck, chest and abdomen) |
| Stage IV | Involvement of lymph nodes on both sides of the diaphragm and/or involvement of one or more organs such as the lungs, spleen, liver, bones or bone marrow |
Figure 6. Hodgkin Lymphoma Stages
[Source 49]Hodgkin’s lymphoma Treatment
Which Hodgkin’s lymphoma treatments are right for you depends on the type and stage of your disease, your overall health, and your preferences. Treatment for Hodgkin lymphoma is changing due to new drugs and research findings from clinical trials. Therefore, before treatment begins, it is important to consider getting a second opinion at a center with a Hodgkin lymphoma expert.
It’s important that your doctor is experienced in treating patients with Hodgkin lymphoma or works in consultation with a Hodgkin lymphoma specialist. This type of specialist is called a hematologist-oncologist.
Hodgkin lymphoma is considered one of the most curable forms of cancer. Hodgkin lymphoma can usually be treated successfully with chemotherapy alone or chemotherapy followed by radiotherapy. Occasionally, chemotherapy may be combined with steroid medicine. Overall, treatment for Hodgkin lymphoma is highly effective and most people with the condition are eventually cured. For many people with Hodgkin lymphoma, starting treatment helps them focus on moving ahead and looking forward to recovery.
More than 80 percent of all patients diagnosed with Hodgkin lymphoma can be cured by current treatment approaches. The cure rate is higher, approaching 90 percent, in younger patients and in those with early-stage favorable Hodgkin lymphoma. Even in cases of advanced stage Hodgkin lymphoma, the disease is often highly curable.
Most patients become long-term survivors of Hodgkin’s lymphoma. Other treatment goals are to:
- Maximize cures in all stages of the disease
- Minimize both short-term and long-term side effects and complications
- Weigh the risks of toxicity against treatment benefits
Types of Hodgkin’s lymphoma treatment
Doctors use several types of approaches and treatment combinations for adults and children with Hodgkin lymphoma, some at different stages:
- Chemotherapy
- Radiotherapy also known as “radiation therapy”
- Monoclonal Antibody Therapy
- Immunotherapy
- Stem cell transplantation also known as bone marrow transplant
- Your doctor may suggest that you participate in a clinical trial. Clinical trials can involve therapy with new drugs and new drug combinations or new approaches to stem cell transplantation.
Pretreatment Considerations
Adults of childbearing age and parents of children diagnosed with Hodgkin lymphoma should ask their doctors for information that may lessen the risk of infertility.
Finding the Best Treatment Approach
The goal of Hodgkin lymphoma treatment is to cure the disease.
- The treatment your doctor recommends is based on several factors, including:
- Your disease subtype
- Your disease stage and category
- Whether your disease is either refractory (the disease does not respond to treatment) or relapsed (the disease has recurred after treatment)
- Your age
- Whether you have coexisting diseases or conditions (for example, heart disease, kidney disease, diabetes)
As you develop a treatment plan with your doctor, be sure to discuss:
- The results you can expect from treatment
- The potential side effects, including long-term effects and late-term effects
- The possibility of participating in a clinical trial, where you may have access to advanced medical treatment that may be more beneficial to you than standard treatment
You may find it helpful to bring a loved one with you to your doctor’s visits for support, to take notes and to ask follow-up questions. It’s a good idea to prepare questions you’d like to ask when you visit your doctor. You can also record your conversations with your doctor and listen more closely when you get home.
Chemotherapy Drug Combinations
Chemotherapy (chemo) is a drug treatment that uses chemicals to kill lymphoma cells. Chemotherapy (chemo) is the main treatment for most people with Hodgkin lymphoma (other than some people with nodular lymphocyte-predominant Hodgkin lymphoma, or NLPHL). Chemotherapy drugs travel through your bloodstream and can reach nearly all areas of your body and destroy cancer cells wherever they may be. Chemotherapy (chemo) can be given in a number of different ways, depending on the stage of your lymphoma. If doctors think your lymphoma is curable, you’ll normally receive chemotherapy through a drip directly into a vein (intravenous chemotherapy). If a cure is unlikely, you may only need to take chemotherapy tablets to help relieve your symptoms.
Chemotherapy is often combined with radiation therapy in people with early-stage classical type Hodgkin’s lymphoma. Radiation therapy is typically done after chemotherapy. In advanced Hodgkin’s lymphoma, chemotherapy may be used alone or combined with radiation therapy.
Children and young adults with Hodgkin lymphoma are usually treated with combination chemotherapy and involved field radiation therapy.
Chemo is given in cycles that include a period of treatment followed by a rest period to give the body time to recover. In general, each cycle lasts for several weeks.
Most chemo treatments are given in the doctor’s office, clinic, or hospital outpatient department, but some may require a hospital stay.
Common chemotherapy drug combinations used to treat children and young adults include:
- ABVD: doxorubicin (Adriamycin®), bleomycin (Blenoxane®), vinblastine (Velban®), dacarbazine (DTIC-Dome®). ABVD is the most common regimen used in the United States.
- AV-PC: doxorubicin (Adriamycin®), vincristine (Oncovin®), prednisone and cyclophosphamide (Cytoxan®)
- ABVE: doxorubicin (Adriamycin®), bleomycin (Blenoxane®), vincristine (Oncovin®), and etoposide (Etopophos®, Toposar®, VePesid®, VP-16)
- ABVE-PC: doxorubicin (Adriamycin®), bleomycin (Blenoxane®), vincristine (Oncovin®), etoposide (Etopophos®, Toposar®, VePesid®, VP-16), prednisone and cyclophosphamide (Cytoxan®)
- BEACOPP: bleomycin (Blenoxane®), etoposide (Etopophos®, Toposar®, VePesid®, VP-16), doxorubicin (Adriamycin®), cyclophosphamide (Cytoxan®), vincristine (Oncovin®), procarbazine (Matulane®) and prednisone
- OEPA: vincristine (Oncovin®), etoposide (Etopophos®, Toposar®, VePesid®, VP-16), prednisone, and doxorubicin (Adriamycin®)
- Stanford V: Doxorubicin (Adriamycin), Mechlorethamine (nitrogen mustard), Vincristine, Vinblastine, Bleomycin, Etoposide and Prednisone
- Another drug that can be considered as chemo is brentuximab vedotin (Adcetris). This is an antibody-drug conjugate, which is a monoclonal antibody attached to a chemo drug.
Early-stage classical Hodgkin lymphoma (cHL)
- Chemotherapy combinations
- ABVD (Adriamycin® [doxorubicin], bleomycin, vinblastine, dacarbazine)
- Escalated BEACOPP (bleomycin, etoposide, Adriamycin [doxorubicin], cyclophosphamide, Oncovin® [vincristine], procarbazine, prednisone)
- Combination chemotherapy is administered with or without radiation therapy.
Advanced-stage classical Hodgkin lymphoma (cHL)
- Chemotherapy combinations
- A+AVD (Adcetris® [brentuximab vedotin], Adriamycin [doxorubicin], vinblastine, dacarbazine)
- ABVD
- ABVD followed by escalated BEACOPP
- Occasionally, chemotherapy is followed by involved-site radiation therapy (ISRT).
Side effects of chemotherapy depend on the drugs you’re given. Common side effects are nausea, vomiting and hair loss. The most significant side effect of chemotherapy is potential damage to your bone marrow. This can interfere with the production of healthy blood cells and cause the following problems:
- fatigue
- breathlessness
- increased vulnerability to infection
- bleeding and bruising more easily
If you experience these problems, treatment may need to be delayed so you can produce more healthy blood cells. Growth factor medicines can also stimulate the production of blood cells.
Other possible side effects of chemotherapy include:
- diarrhea
- loss of appetite
- mouth ulcers
- tiredness
- skin rashes
- infertility, which may be temporary or permanent
Serious long-term complications can occur, such as heart damage, lung damage and other cancers, such as leukemia.
If regular chemotherapy is unsuccessful or Hodgkin lymphoma returns after treatment, you may have a course of chemotherapy at a higher dose.
However, this intensive chemotherapy destroys your bone marrow, leading to the problems mentioned above. You’ll need a stem cell or bone marrow transplant to replace the damaged bone marrow.
Table 10. Chemotherapy Regimens Used to Treat Hodgkin Lymphoma
| Combination Name | Drugs Included | Prognostic Group |
|---|---|---|
| ABVD | Doxorubicin, bleomycin, vinblastine, and dacarbazine | Early favorable classic Hodgkin’s lymphoma |
| Early unfavorable classic Hodgkin’s lymphoma | ||
| AVD | Doxorubicin, vinblastine, and dacarbazine | Early favorable classic Hodgkin’s lymphoma |
| Advanced classic Hodgkin’s lymphoma | ||
| BEACOPP | Bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone | Early unfavorable classic Hodgkin’s lymphoma |
| Advanced classic Hodgkin’s lymphoma | ||
| GVD | Gemcitabine, vinorelbine, and liposomal doxorubicin | Recurrent classic Hodgkin’s lymphoma |
| ICE | Ifosfamide, carboplatin, and etoposide | Recurrent classic Hodgkin’s lymphoma |
| MOPP | Mechlorethamine, vincristine, procarbazine, and prednisone | Advanced classic Hodgkin’s lymphoma |
Radiation therapy
Radiation therapy also known as “radiotherapy”, uses high-energy beams, such as X-rays and protons, to kill cancer cells. Radiation therapy is most often used to treat early-stage Hodgkin lymphoma, where the cancer is only in 1 part of the body. Involved-site radiation therapy (ISRT) is sometimes used to treat Hodgkin’s lymphoma. It selectively treats the lymph nodes where the cancer started and the cancerous masses near those nodes. With a special machine, carefully focused beams of radiation are directed at the cancer. This is also called “external beam therapy” (EBT). The size of the targeted area is restricted to minimize radiation exposure to adjacent, uninvolved organs, and to decrease the side effects associated with radiation therapy.
For classical Hodgkin’s lymphoma (cHL), radiation therapy is often used after chemotherapy. People with early-stage nodular lymphocyte-predominant Hodgkin’s lymphoma may undergo radiation therapy alone.
During radiation therapy, you lie on a table and a large machine moves around you, directing the energy beams to specific points on your body. Radiation can be aimed at affected lymph nodes and the nearby area of nodes where the disease might progress. The length of radiation treatment varies, depending on the stage of the disease. A typical treatment plan might have you going to the hospital or clinic five days a week for several weeks. At each visit, you undergo a 30-minute radiation treatment. For example, radiation therapy treatment is normally given in short daily sessions, Monday to Friday, over several weeks. You shouldn’t have to stay in hospital between appointments.
With careful planning, the exposure of uninvolved organs can be either reduced or avoided during radiation therapy. Imaging techniques such as magnetic resonance imaging (MRI), positron emission tomography-computed tomography (PET-CT), and other specialized imaging techniques can enhance treatment planning.
Radiotherapy itself is painless, but it can have some significant side effects. These can vary and will be directly related to the part of your body being treated. For example, treatment to your throat can lead to a sore throat, while treatment to the head can lead to hair loss.
Other common side effects include:
- tiredness
- nausea and vomiting
- dry mouth
- loss of appetite
Most side effects are temporary, but there’s a risk of long-term problems, including infertility and permanently darkened skin in the treatment area. More-serious risks include heart disease, stroke, thyroid problems and other cancers, such as breast or lung cancer.
Steroid medicine
Steroid medicine is sometimes used in combination with chemotherapy as a more intensive treatment for advanced Hodgkin lymphoma, or if initial treatment hasn’t worked.
The steroid medicine is given intravenously, usually at the same time as your chemotherapy.
Common side effects of steroid medicine include:
- increased appetite, which can lead to weight gain
- indigestion
- problems sleeping
- feeling agitated
The side effects of steroid medicine usually start to improve once treatment finishes.
Monocolonal Antibody Therapy
This is a type of targeted therapy. When the body’s immune system identifies something harmful, such as bacteria or a virus, it produces antibodies. Antibodies are proteins that help fight infection. Monoclonal antibodies are a type of protein made in the laboratory that can bind to only one substance. By design, they can only attack a specific target, typically a substance on cancer cells (though sometimes they are designed to bind to a substance on immune cells, in order to improve their function). This targeting can reduce damage to normal, healthy cells.
In patients with classical Hodgkin’s lymphoma, the malignant Hodgkin and Reed-Sternberg cells typically express a protein called CD30. Brentuximab vedotin (Adcetris®) is an anti-CD30 antibody attached to a chemotherapy drug. It binds to cells that express CD30 and then enters the cancer cells. Once inside the cancer cells, it releases the chemotherapy drug. By targeting only cells that express CD30, fewer normal cells are harmed.
Brentuximab vedotin, given intravenously (IV), is approved for the treatment of adult patients with previously untreated Stage III or IV classical Hodgkin lymphoma (cHL), in combination with doxorubicin, vinblastine, and dacarbazine. The drug is also approved for other indications such as some cases of relapsed Hodgkin’s lymphoma and certain other lymphomas with CD30 expression.
Rituximab (Rituxan®) is a monoclonal antibody designed to bind to cells expressing CD20. Rituximab is often combined with chemotherapy drugs. Rituximab (Rituxan®) is not used to treat classical Hodgkin’s lymphoma (cHL) because, in this subtype of the disease, the lymphoma cells do not usually express CD20. However, it is sometimes used to treat nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) because CD20 is expressed by the lymphoma cells in this subtype of the disease. In rituximab therapy, the monoclonal antibodies attach to and kill the lymphoma cells.
Immunotherapy
Immunotherapy uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This cancer treatment is a type of biologic therapy. Immunotherapy can be used to treat some people with Hodgkin lymphoma.
Immune checkpoint inhibitors (PD-1 and PD-L1 inhibitor therapy) are a type of immunotherapy. Checkpoints are molecules found on T-cells, a type of white blood cell. PD-1 is a protein on the surface of T cells that helps keep the body’s immune responses in check. PD-L1 is a protein found on some types of cancer cells. T cells circulate throughout the body looking for signs of infection and diseases, including cancer. When a T cell comes across any type of cell, it probes (looks for) certain proteins on the cell’s surface. If the T cell determines that it is a normal, healthy cell, it moves on to check other cells. If the proteins indicate that the cell is foreign or cancerous, the T cell attacks it. But cancer cells can sometimes send misleading signals to these checkpoints, telling the T cells that they are not harmful. When PD-1 attaches to PD-L1, it stops the T cell from killing the cancer cell.
Checkpoint inhibitors (PD-1 and PD-L1 inhibitors) work by blocking the signals that cancer cells send to T cells. Checkpoint inhibitors (PD-1 and PD-L1 inhibitors) keep PD-1 and PD-L1 proteins from attaching to each other. When the signals are blocked, it is more likely the T cells will distinguish the cancer cells from healthy cells and allows the T cells to kill cancer cells.
Nivolumab (Opdivo®) and pembrolizumab (Keytruda®) are checkpoint inhibitors (PD-1 inhibitors), both given by IV, that can be used for some patients with Hodgkin lymphoma that has become refractory (come back or spread during treatment), or that has relapsed (returned) after completing other treatments. They are also used to treat certain other types of cancer in which their effects on the immune system can be helpful.
Nivolumab is FDA-approved for the treatment of adult patients with classical Hodgkin lymphoma that has relapsed or progressed after:
- Autologous hematopoietic stem cell transplantation (HSCT) and brentuximab vedotin, OR
- 3 or more lines of systemic therapy that includes autologous hematopoietic stem cell transplantation (HSCT).
Pembrolizumab is FDA-approved for the treatment of adult and pediatric patients with refractory classical Hodgkin lymphoma or who have relapsed after 3 or more prior lines of therapy.
Bone marrow transplant
Bone marrow transplant also known as stem cell transplant, is a treatment to replace your diseased bone marrow with healthy stem cells that help you grow new bone marrow. A bone marrow transplant may be an option if Hodgkin’s lymphoma returns despite treatment.
There are two main types of stem cell transplantation:
- Autologous stem cell transplantation, a procedure in which your own blood stem cells are removed, frozen and stored for later use. Next you receive high-dose chemotherapy and radiation therapy to destroy cancerous cells in your body. Finally your stem cells are thawed and injected into your body through your veins. The stem cells help build healthy bone marrow.
- Allogeneic stem cell transplantation, a procedure in which patients receive stem cells from a donor after they undergo intensive chemotherapy
People who undergo bone marrow transplant may be at increased risk of infection.
In almost all cases, autologous stem cell transplantation is used for Hodgkin’s lymphoma. It remains the standard therapy for relapsed and refractory cases of Hodgkin lymphoma.
The first step is to collect the patient’s own stem cells after initial treatment is completed and the patient is in remission. The stem cells are removed from the patient’s bone marrow (inside the bones), and are frozen and stored until they are needed for the transplant. The patient is then given high doses of chemotherapy to destroy any lymphoma cells not killed during the initial treatment. After the high-dose chemotherapy is completed, the stem cells are returned to the patient’s bloodstream by IV infusion (similar to a blood transfusion). The goal is to “rescue” the bone marrow from the effects of the high doses of chemotherapy, reintroducing healthy stem cells into the system in order to restore normal blood cell production.
Brentuximab vedotin is sometimes also given to patients before the bone marrow transplant, or, in select patients, it is administered as maintenance treatment after autologous stem cell transplantation
Allogeneic stem cell transplantation has been successful in some patients with Hodgkin lymphoma after several relapses of the disease, but it is not commonly used as a treatment for Hodgkin lymphoma. It is generally only done if a patient relapses after an autologous transplant.
Treatment Options for Nodular Lymphocyte-Predominant Hodgkin lymphoma (NLPHL)
Nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) is a rare subtype of Hodgkin lymphoma that accounts for only about 5 percent of all Hodgkin lymphoma cases. The cancer cells in NLPHL are a variant of Reed-Sternberg cells. They are larger and are sometimes called “popcorn” cells because their unique shape is similar to pieces of popcorn.
Nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) tends to progress more slowly than classical Hodgkin’s lymphoma (cHL), so the treatment approach is usually different. About 75 percent of patients with NLPHL have stage I disease at diagnosis. It is rare for NLPHL patients to have B symptoms or disease involvement outside of the lymph nodes, and mediastinal masses and bulky disease are also rare.
Because NLPHL is associated with an excellent long-term survival rate, the risk of overtreatment is an important consideration for these patients. Overtreatment may lead to problems and harmful side effects from cancer therapies that are not needed. One option for some patients is the “watch-and-wait” approach, in which the patient is closely monitored for disease progression without getting any treatment until symptoms appear or begin to change. Another option for early-stage NLPHL without any B symptoms or bulky disease is the use of radiation therapy alone.
Combination chemotherapy may be needed in more advanced stages of the disease, with rituximab (Rituxan®) added to the regimen in some cases.
Common treatments used in NLPHL include:
- ABVD + rituximab (Adriamycin® [doxorubicin], bleomycin, vinblastine, dacarbazine + rituximab)
- CHOP + rituximab (cyclophosphamide, doxorubicin, vincristine, prednisone + rituximab)
- CVP + rituximab (cyclophosphamide, vinblastine, prednisone + rituximab)
- Rituximab (Rituxan®) alone
Nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) can sometimes recur many years (or even decades) after initial treatment. In a small percentage of patients, it can transform into diffuse large B-cell lymphoma (DLBCL), a type of non-Hodgkin lymphoma that is usually aggressive. For patients with a suspected relapse of NLPHL, another biopsy should be considered to rule out transformation to DLBCL. Patients with refractory or relapsed NLPHL can be treated with a second-line therapy that includes rituximab, either with or without chemotherapy or radiation therapy.
Treatments for Relapsed or Refractory Hodgkin’s lymphoma
Most patients with classical Hodgkin’s lymphoma (cHL) are cured by their initial (first-line) treatment. However, in a significant percentage of patients—especially those with advanced-stage Hodgkin lymphoma—the disease relapses or is refractory. Relapse means the disease comes back after a remission following treatment. Refractory means the disease has not responded to treatment. For these patients, Hodgkin lymphoma is still potentially curable.
For patients who are not cured with initial therapy, second-line treatment options include:
- Alternate chemotherapy combinations
- Monoclonal antibody therapy with brentuximab vedotin
- Checkpoint inhibitors, nivolumab and pembrolizumab
- Autologous stem cell transplantation
Alternate Chemotherapy Combinations. Traditional chemotherapy-based regimens include:
- ICE (ifosfamide, carboplatin, etoposide)
- DHAP (dexamethasone, High-dose Ara-C [cytarabine], Platinol [cisplatin])
- ESHAP (etoposide, methylprednisolone, high-dose cytarabine, cisplatin)
- IGEV (ifosfamide, gemcitabine, vinorelbine)
- GDP (gemcitabine, dexamethasone, Platinol [cisplatin])
- GVD (gemcitabine, vinorelbine, liposomal doxorubicin)
Brentuximab vedotin (Adcetris®) is a monoclonal antibody drug combination given intravenously (IV). Brentuximab vedotin is approved by the FDA for the treatment of adult patients with previously untreated stage III or stage IV classical Hodgkin lymphoma (cHL), in combination with chemotherapy (doxorubicin, vinblastine and dacarbazine). It is also approved for classical Hodgkin lymphoma (cHL) patients at high risk of relapse or progression as postautologous hematopoietic stem cell transplantation (auto-HSCT) consolidation and for classical Hodgkin lymphoma (cHL) patients after failure of auto-HSCT or after failure of at least two prior multi-agent chemotherapy regimens in patients who are not auto-HSCT candidates.
As a second-line therapy, brentuximab vedotin can be used:
- Alone, as a single agent
- In combination with chemotherapy
- In combination with checkpoint inhibitors
- As maintenance therapy after an autologous stem cell transplantation
Nivolumab (Opdivo®) is a checkpoint inhibitor given by IV, is FDA-approved for the treatment of adult patients with classical Hodgkin’s lymphoma (cHL) that has relapsed or progressed after:
- Autologous stem cell transplantation and brentuximab vedotin, OR
- 3 or more lines of systemic therapy that included autologous stem cell transplant
Pembrolizumab (Keytruda®) is a checkpoint inhibitor given IV. It is approved by the FDA for the treatment of adult and pediatric patients with refractory classical Hodgkin’s lymphoma (cHL), or who have relapsed after 3 or more prior lines of therapy.
Treatment Response Monitoring
During treatment, patients need to be monitored to check their response to therapy. Response to treatment is important in predicting long-term outcomes. Patients who fail to reach complete remission with first-line treatment have a worse prognosis, so there is great value in identifying these patients early in the course of their disease.
Imaging tests are used to distinguish between tumor and fibrous (scar) tissue. PET-CT scans help doctors determine if the disease is responding to treatment. PET-CT has become the standard method for assessment of treatment response in most types of lymphoma.
The Deauville score (see Table 5 above), based on a five-point scale developed in 2009, is now an internationally recognized way of using PET-CT to assess treatment response. This scale determines the “FDG uptake” (the absorption of this radioactive material by tissues) in the involved sites. The Deauville score is then used to determine if any treatment modifications are needed.
Clinical Trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
A clinical trial may be an option when it comes to finding the right treatment for your child’s cancer. Your child may have access to new or improved therapies under study and not yet on the market. Discuss with your child’s doctor the possibility of taking part in a clinical trial, where treatment is administered in a safe, closely monitored environment.
Advances in treating childhood Hodgkin lymphoma, which have improved the cure rate and quality of life for survivors, are due, in large part, to the research of pediatric cooperative groups. The focus of ongoing research and clinical trials is to
- Further improve the cure rate, especially for children with advanced Hodgkin’s lymphoma
- Minimize the risk of long-term and late effects associated with treatment (for example, infertility, impaired cardiac function and secondary cancers).
Survivorship and Special Healthcare Needs
After treatment, most children can expect to have full and productive lives. Many survivors return to school, attend college, enter the workforce, marry and become parents.
You may want to consider a survivorship program for your child that focuses on life after cancer. Many comprehensive cancer centers around the country offer these programs.
Follow-Up Care
Your child should visit his or her pediatrician or doctor at least once a year for a complete physical exam and any additional needed tests. Your child’s oncologist should also regularly examine your child.
Regular doctor visits are encouraged to:
- Enable doctors to assess the full effect of therapy
- Detect and treat disease recurrence
- Identify and manage long-term and late effects of treatment
Your pediatrician should recommend a schedule for having your child’s learning skills assessed. If your child appears to be experiencing learning disabilities, special education methods can help.
Coordination between your child’s pediatrician and oncologist is important for the best care possible. Some treatment centers offer comprehensive follow-up care clinics for childhood cancer survivors.
Long-Term and Late Effects of Treatment
Some side effects of cancer treatment, such as fatigue, can linger for months or years after therapy. Some medical conditions like heart disease and other cancers may not appear until years after treatment ends. Long-term and late effects can affect your child’s physical, mental and cognitive (brain function) health.
Most childhood survivors of lymphoma don’t develop significant long-term or late effects of treatment. However, for some patients the effects can be severe.
Long-Term and Late Effects of Chemotherapy
Children treated for lymphoma may be at increased risk for:
- Fatigue
- Growth delays
- Thyroid dysfunction
- Hearing loss
- A secondary cancer
Some long-term and late effects become evident with maturation (puberty), growth and the normal aging process. Early intervention and healthy lifestyle practices (not smoking, good nutrition, exercise, regular screenings and follow-up) may have a positive effect on the occurrence and/or severity of long-term and late effects.
Long-Term and Late Effects of Radiation Therapy
Girls (as well as women under age 30) who had radiation to the breast area are at risk for developing breast cancer 15 to 20 years after treatment. Male survivors of childhood cancer are at risk for developing secondary cancers, but they don’t have as high a risk for developing breast cancer as female childhood cancer survivors do.
Girls who had radiation therapy in the chest (mediastinal) area should:
- Perform monthly breast self-examinations
- Have yearly breast examinations by a healthcare professional
- Have early baseline mammograms within 8 to 10 years after therapy or by age 40, whichever occurs earlier.
- Have breast MRIs in addition to mammography for women who received irradiation of the chest when they were between 10 and 30 years of age.
Both girls and boys who’ve undergone mediastinal radiation therapy should have baseline testing for heart function. This should be followed by testing every three to five years after treatment or more regularly if any abnormalities are found.
Returning to School
Learning disabilities can begin during treatment or appear months or years after treatment. Educate family members, friends, school personnel and healthcare providers about your child’s possible long-term and late effects of treatment. Talk with teachers about your child’s needs before he or she returns to school. Work with your child’s teachers and medical providers to develop a program tailored to his or her needs that features baseline testing, special accommodations and long-term planning.
Non Hodgkin’s lymphoma
Non-Hodgkin lymphoma also known as NHL or just lymphoma, is a cancer that starts when a type of white blood cell, called lymphocyte (T cell or B cell), becomes abnormal. About 85-90 percent of NHL cases start in the B cells 50. In non-Hodgkin’s lymphoma, lymphocytes undergo a malignant (cancerous) change and then multiplies, eventually crowding out healthy cells and creating tumors. Non-Hodgkin lymphoma generally develop in the lymph nodes or in lymphatic tissue found in organs such as the stomach, intestines or skin. Furthermore, these abnormal cells can spread to almost any other part of the body. In some cases, non-Hodgkin’s lymphoma involves blood and the bone marrow (the spongy tissue in the hollow, central cavity of bones, where blood cell formation occurs). Lymphoma cells may develop in just one place or in many sites in the body. Most of the time, doctors don’t know why a person gets non-Hodgkin lymphoma. You are at increased risk if you have a weakened immune system or have certain types of infections.
More than 60 specific non-Hodgkin lymphoma (NHL) subtypes have been identified and assigned names, so classifying it can be quite confusing (even for doctors). Several different systems have been used, but the most recent system is the World Health Organization (WHO) classification 2. The Revised European American Lymphoma and World Health Organization (REAL/WHO) classification of non-Hodgkin’s lymphoma categorizes non-Hodgkin’s lymphoma subtypes by the characteristics of the lymphoma cells, including their appearance, the presence of proteins on the surface of the cells and their genetic features. One way that non-Hodgkin’s lymphoma subtypes are classified is by cell type. Some non-Hodgkin’s lymphoma subtypes, such as diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), involve lymphocytes called “B cells.” Other subtypes, such as peripheral T-cell lymphoma (PTCL) and cutaneous T-cell lymphoma (CTCL), involve lymphocytes called “T cells” or “natural killer (NK) cells.”
Specialists further classify the non-Hodgkin’s lymphoma subtypes according to the rate of disease progression, either fast growing (aggressive) or slow growing (indolent). Aggressive lymphoma subtypes also called “high-grade non-Hodgkin’s lymphoma”, account for about 60 percent of all non-Hodgkin’s lymphoma cases. Diffuse large B-cell lymphoma is the most common aggressive non-Hodgkin’s lymphoma subtype. Slow-growing (indolent) subtypes account for about 40 percent of all non-Hodgkin’s lymphoma cases. Follicular lymphoma (FL) is the most common subtype of indolent non-Hodgkin’s lymphomas. When indolent lymphomas are first diagnosed, patients have fewer signs and symptoms than patients with aggressive lymphoma subtypes. Whether the diagnosed subtype is aggressive or indolent determines the appropriate treatment, so getting an accurate diagnosis is very important. In some cases, indolent forms of non-Hodgkin’s lymphoma later transform into an aggressive form of the disease.
Non-Hodgkin lymphoma (NHL) is one of the most common cancers in the United States, accounting for about 4.2% of all cancers. The American Cancer Society’s most recent estimates for non-Hodgkin’s lymphoma are for 2022 51:
- New cases: About 80,470 people (44,120 males and 36,350 females) will be diagnosed with non-Hodgkin lymphoma. This includes both adults and children.
- Deaths: About 20,250 people will die from non-Hodgkin lymphoma (11,700males and 8,550 females).
- 5-Year Relative Survival: 73.8%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Percentage of All Cancer Deaths: 3.3%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of non-Hodgkin lymphoma was 19.0 per 100,000 men and women per year. The death rate was 5.3 per 100,000 men and women per year. These rates are age-adjusted and based on 2015–2019 cases and deaths.
- Lifetime Risk of Developing Cancer: Approximately 2.1 percent of men and women will be diagnosed with non-Hodgkin lymphoma at some point during their lifetime, based on 2017–2019 data.
- In 2019, there were an estimated 763,400 people living with non-Hodgkin lymphoma in the United States.
The average American’s risk of developing non-Hodgkin’s lymphoma during a man’s lifetime is about 1 in 42; for a woman, the risk is about 1 in 52 52. But each person’s risk can be affected by a number of risk factors.
Non-Hodgkin’s lymphoma can occur at any age. In fact, it is one of the more common cancers among children, teens, and young adults. Still, the risk of developing non-Hodgkin’s lymphoma increases throughout life, and more than half of patients are 65 or older at the time of diagnosis. The aging of the American population is likely to lead to an increase in non-Hodgkin’s lymphoma cases during the coming years.
Treatment for non-Hodgkin lymphoma depends on which type it is, so it’s important for doctors to find out the exact type of lymphoma you have. The type of lymphoma depends on what type of lymphocyte is affected (B cells or T cells), how mature the cells are when they become cancerous, and other factors.
The prognosis and treatment approach for different non-Hodgkin’s lymphoma subtypes are influenced by findings from studying the diseased cells and tissues under a microscope, so biopsy samples should be examined by a hematopathologist (a doctor who specializes in the diagnosis of blood disorders and blood cancers).
Survival rates for non-Hodgkin lymphoma
The numbers below come from the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program (SEER) database, looking at people diagnosed with non-Hodgkin lymphoma between 2011–2017 53:
- The 5-year survival rate for people with stage I non-Hodgkin lymphoma is about 84.3%.·
- For stage II non-Hodgkin lymphoma, the 5-year survival rate is about 77.1%.
- The 5-year survival rate for stage III non-Hodgkin lymphoma is about 71.1%.
- Stage IV non-Hodgkin lymphoma has a 5-year survival rate of about 63.7%.
Based on data from the National Cancer Institute. Surveillance, Epidemiology, and End Results program (SEER) 2011-2017, percent surviving 5 Years is 73.2% 53.
Figure 7. 5-year relative survival rates for non-Hodgkin lymphoma
Footnote: A relative survival rate compares people with the same type and stage of non-Hodgkin’s lymphoma to people in the overall population. For example, if the 5-year survival rate for a specific stage of non-Hodgkin lymphoma is 73.2%, it means that people who have that cancer are, on average, about 73.2% as likely as people who don’t have that cancer to live 5 years after being diagnosed.
- These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment.
- These numbers don’t take everything into account. Survival rates are grouped based on how far the cancer has spread, but your age, overall health, how well the cancer responds to treatment, and other prognostic factors (described below) can also affect your outlook.
- People now being diagnosed with non-Hodgkin lymphoma may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
Non-Hodgkin’s lymphoma Survival by Stage
Cancer stage at diagnosis, which refers to extent of a cancer in the body, determines treatment options and has a strong influence on the length of survival. In general, if the cancer is found only in the part of the body where it started it is localized (sometimes referred to as stage 1). If it has spread to a different part of the body, the stage is regional or distant. For non-Hodgkin lymphoma, 24.3% are diagnosed at the local stage. The 5-year survival for localized non-Hodgkin lymphoma is 84.3% 53.
Remember, these survival rates are only estimates – they can’t predict what will happen to any individual person. We understand that these statistics can be confusing and may lead you to have more questions. Talk to your doctor to better understand your specific situation.
Prognostic factors for non-Hodgkin lymphoma
The International Prognostic Index (IPI) was first developed to help doctors determine the outlook (prognosis) for people with fast-growing (aggressive) lymphomas (see Table 7 above). However, it has proven useful for most other lymphomas as well (other than slow-growing [indolent] follicular lymphomas). The International Prognostic Index (IPI) allows doctors to plan treatment better than they could just based on the type and stage of the lymphoma. This has become more important as new, more effective treatments have been developed that sometimes have more side effects. The index helps doctors figure out whether these treatments are needed.
The International Prognostic Index (IPI) depends on 5 factors:
- The patient’s age
- The stage of the lymphoma
- Whether or not the lymphoma is in organs outside the lymph system
- Performance status (PS) – how well a person can complete normal daily activities
- The blood level of lactate dehydrogenase (LDH), which goes up with the amount of lymphoma in the body
Table 11. International Prognostic Index non-Hodgkin lymphoma
| Good prognostic factors | Poor prognostic factors |
|---|---|
| Age 60 or below | Age above 60 |
| Stage I or II | Stage III or IV |
| No lymphoma outside of lymph nodes, or lymphoma in only 1 area outside of lymph nodes | Lymphoma is in more than 1 organ of the body outside of lymph nodes |
| Performance status (PS): Able to function normally | Performance status (PS): Needs a lot of help with daily activities |
| Serum lactate dehydrogenase (LDH) is normal | Serum lactate dehydrogenase (LDH) is high |
Footnotes: Each poor prognostic factor is assigned 1 point. People without any poor prognostic factors would have a score of 0, while those with all poor prognostic factors would have a score of 5. The index divides people with lymphomas into 4 risk groups:
- Low risk (0 or 1 poor prognostic factors)
- Low-intermediate risk (2 poor prognostic factors)
- High-intermediate risk (3 poor prognostic factors)
- High risk (4 or 5 poor prognostic factors)
International Prognostic Index for Follicular Lymphoma
The International Prognostic Index (IPI) is useful for most lymphomas, but it’s not as helpful for follicular lymphomas, which tend to be slower growing. Doctors have developed the Follicular Lymphoma International Prognostic Index (FLIPI) specifically for this type of lymphoma. It uses slightly different prognostic factors than the International Prognostic Index (IPI).
Table 12. Follicular Lymphoma International Prognostic Index (FLIPI)
| Good prognostic factors | Poor prognostic factors |
|---|---|
| Age 60 or below | Age above 60 |
| Stage I or II | Stage III or IV |
| Blood hemoglobin 12 g/dL or above | Blood hemoglobin level below 12 g/dL |
| 4 or fewer lymph node areas affected | More than 4 lymph node areas affected |
| Serum lactate dehydrogenase (LDH) is normal | Serum lactate dehydrogenase (LDH) is high |
Footnotes: Patients are assigned a point for each poor prognostic factor. People without any poor prognostic factors would have a score of 0, while those with all poor prognostic factors would have a score of 5. The index then divides people with follicular lymphoma into 3 groups:
- Low risk (no or 1 poor prognostic factor[s])
- Intermediate risk (2 poor prognostic factors)
- High risk (3 or more poor prognostic factors)
Types of Non-Hodgkin’s Lymphoma
More than 60 specific non-Hodgkin lymphoma (NHL) subtypes have been identified and assigned names, so classifying it can be quite confusing (even for doctors). Several different systems have been used, but the most recent system is the World Health Organization (WHO) classification.
The WHO system groups lymphomas based on:
- The type of lymphocyte the lymphoma starts in
- How the lymphoma looks under a microscope
- The chromosome features of the lymphoma cells
- The presence of certain proteins on the surface of the cells
The more common types of lymphoma are listed below according to whether they start in B lymphocytes (B cells) or T lymphocytes (T cells) with B-cell lymphomas being the most common. Some rarer forms of non-Hodgkin lymphoma are not listed here.
Specialists further classify the non-Hodgkin lymphoma subtypes according to the rate of disease progression, either fast growing (aggressive) or slow growing (indolent).
- Indolent lymphomas grow and spread slowly Some indolent lymphomas might not need to be treated right away, but can be watched closely instead. Slow-growing (indolent) subtypes account for about 40 percent of all non-Hodgkin lymphoma cases. The most common type of indolent lymphoma in the United States is follicular lymphoma (FL).
- Aggressive lymphomas also called “high-grade non-Hodgkin lymphoma”, grow and spread quickly, and usually need to be treated right away. Aggressive lymphoma subtypes account for about 60 percent of all non-Hodgkin lymphoma cases. The most common type of aggressive lymphoma in the United States is diffuse large B cell lymphoma (DLBCL).
- Some types of lymphoma, like mantle cell lymphoma, don’t fit neatly into either of these categories.
When indolent lymphomas are first diagnosed, patients have fewer signs and symptoms than patients with aggressive lymphoma subtypes. Whether the diagnosed subtype is aggressive or indolent lymphoma determines the appropriate treatment, so getting an accurate diagnosis is very important. In some cases, indolent forms of non-Hodgkin lymphoma later transform into an aggressive form of the disease 54.
Non-Hodgkin’s lymphoma Subtypes
Mature B-cell lymphomas (about 85%-90% of non-Hodgkin’s lymphoma cases)
- Aggressive lymphomas (high-grade non-Hodgkin lymphomas)
- Diffuse large B-cell lymphoma (DLBCL) (31%)
- Mantle cell lymphoma (MCL) (can present as aggressive or indolent) (6%)
- Lymphoblastic lymphoma (2%)
- Burkitt lymphoma (BL) (2%)
- Primary mediastinal (thymic) large B-cell lymphoma (PMBCL) (2%)
- Transformed follicular and transformed mucosa-associated lymphoid tissue (MALT) lymphomas
- High-grade B-cell lymphoma with double or triple hits (HBL)
- Primary cutaneous DLBCL, leg type
- Primary DLBCL of the central nervous system
- Primary central nervous system (CNS) lymphoma
- Acquired immunodeficiency syndrome (AIDS)-associated lymphoma
- Indolent lymphomas
- Follicular lymphoma (FL) (22%)
- Marginal zone lymphoma (MZL) (8%)
- Chronic lymphocytic leukemia/small-cell lymphocytic lymphoma (CLL/SLL) (6%)
- Gastric mucosa-associated lymphoid tissue (MALT) lymphoma (5%)
- Lymphoplasmacytic lymphoma (1%)
- Waldenström macroglobulinemia (WM)
- Nodal marginal zone lymphoma (NMZL) (1%)
- Splenic marginal zone lymphoma (SMZL)
Mature T-cell and natural killer (NK)-cell lymphomas (about 10%-15% of non-Hodgkin’s lymphoma cases)
- Aggressive lymphomas (high-grade non-Hodgkin lymphomas)
- Peripheral T-cell lymphoma (PTCL), not otherwise specified (6%)
- Systemic anaplastic large-cell lymphoma (ALCL) (2%)
- Lymphoblastic lymphoma (2%)
- Hepatosplenic gamma/delta T-cell lymphoma
- Subcutaneous panniculitis-like T-cell lymphoma (SPTCL)
- Enteropathy-type intestinal T-cell lymphoma
- Primary cutaneous anaplastic large-cell lymphoma
- Indolent lymphomas
- Cutaneous T-cell lymphoma (CTCL) (4%)
- Mycosis fungoides (MF)
- Sézary syndrome (SS)
- Angioimmunoblastic T-cell lymphoma (AITL)
- Adult T-cell leukemia/lymphoma
- Extranodal NK/T-cell lymphoma (ENK/TCL), nasal type
B-cell lymphomas
B-cell lymphomas make up most (about 85%) of non-Hodgkin lymphoma in the United States. These are types of lymphoma that affect B lymphocytes. The most common types of B-cell lymphomas are listed below.
Diffuse large B-cell lymphoma (DLBCL)
This is the most common type of non-Hodgkin lymphoma in the United States, accounting for about 1 out of every 3 lymphomas. The lymphoma cells look fairly large when seen with a microscope.
Diffuse large B-cell lymphoma (DLBCL) can affect people of any age, but it occurs mostly in older people. The average age at the time of diagnosis is mid-60s. It usually starts as a quickly growing mass in a lymph node deep inside the body, such as in the chest or abdomen, or in a lymph node you can feel, such as in the neck or armpit. It can also start in other areas such as the intestines, bones, or even the brain or spinal cord.
Diffuse large B-cell lymphoma (DLBCL) tends to be a fast-growing (aggressive) lymphoma, but it often responds well to treatment. Overall, about 3 out of 4 people will have no signs of disease after the initial treatment, and many are cured.
A common subtype of diffuse large B-cell lymphoma is primary mediastinal B-cell lymphoma. This type of lymphoma occurs mostly in young women. It starts in the mediastinum (the area in the middle of the chest behind the breastbone). It can grow quite large and can cause trouble breathing because it often presses on the windpipe (trachea) leading into the lungs. It can also block the superior vena cava (the large vein that returns blood to the heart from the arms and head), which can make the arms and face swell. This is a fast-growing lymphoma, but it usually responds well to treatment.
There are several other subtypes of diffuse large B-cell lymphoma, but these are rare.
Follicular lymphoma
About 1 out of 5 lymphomas in the United States is a follicular lymphoma. This is usually a slow-growing (indolent) lymphoma, although some follicular lymphomas can grow quickly.
The average age for people with follicular lymphoma is about 60. It’s rare in very young people. Usually, follicular lymphoma occurs in many lymph node sites throughout the body, as well as in the bone marrow.
Follicular lymphomas often respond well to treatment, but they are hard to cure. These lymphomas may not need to be treated when they are first diagnosed. Instead, treatment may be delayed until the lymphoma starts causing problems. Over time, some follicular lymphomas turn into a fast-growing diffuse large B-cell lymphoma.
Chronic lymphocytic leukemia (CLL) /small lymphocytic lymphoma (SLL)
Chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL) are closely related diseases. In fact, many doctors consider them different versions of the same disease. The same type of cancer cell (known as a small lymphocyte) is seen in both chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL) . The only difference is where the cancer cells are found. In chronic lymphocytic leukemia, most of the cancer cells are in the blood and bone marrow. In small lymphocytic lymphoma, the cancer cells are mainly in the lymph nodes and spleen.
Both chronic lymphocytic leukemia and small lymphocytic lymphoma are usually slow-growing (indolent) diseases, although chronic lymphocytic leukemia, which is much more common, tends to grow more slowly. Treatment is the same for chronic lymphocytic leukemia and small lymphocytic lymphoma. They are usually not curable with standard treatments, but many people can live a long time (even decades) with them. Sometimes, these can turn into a more aggressive (fast-growing) type of lymphoma over time.
Mantle cell lymphoma (MCL)
About 5% of lymphomas are mantle cell lymphomas (MCL). Mantle cell lymphoma is much more common in men than in women, and it most often appears in people older than 60. When mantle cell lymphoma is diagnosed, it is usually widespread in the lymph nodes, bone marrow, and often the spleen.
Mantle cell lymphoma (MCL) can be challenging to treat. It tends to grow faster than indolent (slow-growing) lymphomas, but it doesn’t usually respond to treatment as well as aggressive (fast-growing) lymphomas. But newer treatments might offer a better chance for long-term survival for patients now being diagnosed.
Marginal zone lymphomas
Marginal zone lymphomas account for about 5% to 10% of lymphomas. They tend to be slow-growing (indolent). The cells in these lymphomas look small under the microscope. There are 3 main types of marginal zone lymphomas:
- Extranodal marginal zone B-cell lymphoma, also known as mucosa-associated lymphoid tissue (MALT) lymphoma: This is the most common type of marginal zone lymphoma. It starts in places other than the lymph nodes (extranodal). Most MALT lymphomas start in the stomach and are linked to infection by Helicobacter pylori (the bacteria that causes many stomach ulcers). MALT lymphoma might also start in the lung, skin, thyroid, salivary glands, or tissues surrounding the eye. Usually the lymphoma stays in the area where it begins and is not widespread. Many of these other MALT lymphomas have also been linked to infections with bacteria or viruses. The average age of people with MALT lymphoma at the time of diagnosis is about 60. This lymphoma tends to grow slowly and is often curable if found early. Doctors often use antibiotics as the first treatment for MALT lymphoma of the stomach, because treating the Helicobacter pylori infection often cures the lymphoma.
- Nodal marginal zone B-cell lymphoma: This is a rare disease, found mainly in older women. It starts and usually stays in the lymph nodes, although lymphoma cells can also sometimes be found in the bone marrow. Nodal marginal zone B-cell lymphoma tends to be slow-growing (although not usually as slow as MALT lymphoma), and is often curable if found early.
- Splenic marginal zone B-cell lymphoma: This is a rare lymphoma. Most often the lymphoma is found only in the spleen and bone marrow. Splenic marginal zone B-cell lymphoma is most common in older men, and often causes fatigue and discomfort due to an enlarged spleen. Because the disease is slow-growing, it might not need to be treated unless the symptoms become troublesome. This type of lymphoma has been linked to infection with the hepatitis C virus. Sometimes treating the hepatitis C virus can also treat this lymphoma.
Burkitt lymphoma
Burkitt lymphoma is a fast-growing lymphoma is named after the doctor who first described this disease in African children and young adults. Burkitt lymphoma makes up about 1% to 2% of all lymphomas. It is rare in adults, but is more common in children. It’s also much more common in males than in females.
The cells in Burkitt lymphoma are medium-sized. A similar kind of lymphoma, Burkitt-like lymphoma, has slightly larger cells. Because it is hard to tell these lymphomas apart, the WHO classification combines them.
Different varieties of Burkitt lymphoma are seen in different parts of the world:
- In the African (or endemic) variety, Burkitt lymphoma often starts as a tumor of the jaw or other facial bones. It is often linked to infection with the Epstein-Barr virus (EBV, which can also cause infectious mononucleosis or “mono”). This type of Burkitt lymphoma is rare in the United States.
- In the type seen more often in the United States, the lymphoma usually starts in the abdomen (belly), where it forms a large tumor. It can also start in the ovaries, testicles, or other organs, and can spread to the brain and spinal fluid. It is not usually linked to EBV infection.
- Another type (immunodeficiency-associated) of Burkitt lymphoma is associated with immune system problems, such as in people with HIV or AIDS or who have had an organ transplant.
Burkitt lymphoma grows very quickly, so it needs to be treated right away. But more than half of patients can be cured by intensive chemotherapy.
Lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia)
Lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) is a slow-growing lymphoma is not common, accounting for only 1% to 2% of lymphomas. Lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) is rare, with an incidence rate of about 3 cases per million people per year in the United States. About 1,000 to 1,500 people are diagnosed with lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) each year in the United States. Lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) is more common in men than it is in women and it is much more common among Whites than African Americans.
There are few cases of lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) in younger people, but the chance of developing this disease goes up as people get older. The average age of people when they are diagnosed with lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) is 70.
Lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) cells make large amounts of a certain type of antibody (immunoglobulin M, or IgM), which is known as a macroglobulin. Each antibody (protein) made by the lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) cells is the same, so it is called a monoclonal protein or just an M protein. The buildup of this M protein in the body can lead to many of the symptoms of Waldenstrom macroglobulinemia, including excess bleeding, problems with vision, and nervous system problems.
The lymphoplasmacytic lymphoma (Waldenstrom macroglobulinemia) cells grow mainly in the bone marrow, where they can crowd out the normal cells that make the different types of blood cells. This can lead to low levels of red blood cells (called anemia), which can make people feel tired and weak. It can also cause low numbers of white blood cells, which makes it hard for the body to fight infection. The numbers of platelets in the blood can also drop, leading to increased bleeding and bruising.
Hairy cell leukemia
Despite the name, hairy cell leukemia (HCL) is sometimes considered to be a type of lymphoma. Hairy cell leukemia (HCL) is rare – about 700 people in the United States are diagnosed with it each year. Men are much more likely to get hairy cell leukemia (HCL) than women, and the average age at diagnosis is around 50.
Hairy cell leukemia (HCL) cells are small B lymphocytes with projections coming off them that give them a “hairy” appearance. They are typically found in the bone marrow and spleen and in the blood.
Hairy cell leukemia is slow-growing, and some people may never need treatment. An enlarging spleen or low blood cell counts (due to cancer cells invading the bone marrow) are the usual reasons to begin treatment. If treatment is needed, it’s usually very effective.
Primary central nervous system (CNS) lymphoma
This lymphoma involves the brain or spinal cord (the central nervous system, or CNS). The lymphoma is also sometimes found in tissues around the spinal cord or the eye. Over time, it tends to become widespread in the central nervous system.
Primary CNS lymphoma is rare overall, but it’s more common in older people and in people with immune system problems, such as those who have had an organ transplant or who have AIDS. Most people develop headaches and confusion. They can also have vision problems; weakness or altered sensation in the face, arms, or legs; and in some cases, seizures.
Historically, the outlook for patients with primary CNS lymphoma has not been as good as for many other lymphomas, but this is at least partly because people with CNS lymphoma tend to be older or have other serious health problems. However, the outlook for patients with primary CNS lymphoma has improved over the years mainly due to advances in treatment.
Primary intraocular lymphoma (lymphoma of the eye)
This is a rare type of lymphoma that starts in the eyeball and is often seen along with primary CNS lymphoma. It is the second most common cancer of the eye in adults, with ocular melanoma (eye melanoma) being the first. Most people with primary intraocular lymphoma are elderly or have immune system problems which may be due to AIDS or anti-rejection drugs after an organ or tissue transplant.
People may notice bulging of the eyeball without pain, vision loss, or a blurry vision. Many of the tests done to diagnose ocular melanoma are the same used to diagnose lymphoma of the eye.
The main treatment for lymphoma of the eye is external radiation therapy if the cancer is limited to the eye. Chemotherapy (chemo) or chemotherapy in combination with radiation may be used depending on the type of lymphoma and how far it has spread outside of the eye.
T-cell lymphomas
T-cell lymphomas make up less than 15% of non-Hodgkin lymphomas in the United States. These are types of lymphoma that affect T lymphocytes. There are many types of T-cell lymphoma, but they are all fairly rare.
T-lymphoblastic lymphoma/leukemia
T-lymphoblastic lymphoma accounts for about 1% of all lymphomas. It can be considered either a lymphoma or a type of acute lymphoblastic leukemia (ALL), depending on how much of the bone marrow is involved (leukemias have more bone marrow involvement). The cancer cells are very early forms of T cells.
T-lymphoblastic lymphoma often starts in the thymus (a small organ behind the breastbone and in front of the heart, which is where many T cells are made), and can grow into a large tumor in the mediastinum (the area between the lungs). This can cause trouble breathing and swelling in the arms and face.
T-lymphoblastic lymphoma is most common in teens or young adults, with males being affected more often than females.
T-lymphoblastic lymphoma is fast-growing, but if it hasn’t spread to the bone marrow when it is first diagnosed, the chance of cure with chemotherapy is quite good.
Often, the lymphoma form of this disease is treated in the same way as the leukemia form. For more information, see Acute Lymphocytic Leukemia.
Peripheral T-cell lymphomas
Peripheral T-cell lymphomas are uncommon types of lymphomas that develop from more mature forms of T cells.
Cutaneous T-cell lymphomas (mycosis fungoides, Sezary syndrome, and others): These lymphomas start in the skin. Skin lymphomas account for about 5% of all lymphomas.
- Mycosis fungoides (MF): Nearly half of all skin lymphomas are mycosis fungoides. Mycosis fungoides can occur in people of any age, but most who get it are in their 50s or 60s. Men are almost twice as likely as women to develop this lymphoma. The first sign of mycosis fungoides is one or more patchy, scaly, red lesions (abnormal areas) on the skin. Mycosis fungoides lesions can be very itchy. Often these lesions are the only symptom of mycosis fungoides. But in some people the disease can progress to more solid, raised tumors on the skin (called plaques). Because mycosis fungoides can be confused with other skin problems, it can be hard to diagnose at first. Several biopsies of the lesions might be needed before the diagnosis is confirmed. Over time, mycosis fungoides can spread across the skin or invade lymph nodes and organs like the liver. In many people this disease grows slowly, but it can sometimes grow more quickly, especially in older people. Some people with mycosis fungoides go on to develop Sezary syndrome. Rare variants of mycosis fungoides include folliculotropic mycosis fungoides, pagetoid reticulosis, and granulomatous slack skin.
- Sezary syndrome (SS): This is often thought of as an advanced form of mycosis fungoides, but these are actually different diseases. In Sezary syndrome, most or all of the skin is affected, instead of just patches of skin. People with Sezary syndrome typically have a very itchy, scaly red rash that can look like a severe sunburn. This is called generalized erythroderma. The skin is often thickened. Lymphoma cells, called Sezary cells, can be found in the blood (as well as in the lymph nodes). Whereas mycosis fungoides. is usually slow growing, Sezary syndrome tends to grow and spread faster, and is harder to treat. People with Sezary syndrome also often have further weakened immune systems, which increases their risk of serious infections.
- Adult T cell leukemia-lymphoma (ATLL): This rare type of T-cell lymphoma is more likely to start in other parts of the body, but it can sometimes be confined to the skin. It is linked to infection with the HTLV-1 virus (although most people infected with this virus do not get lymphoma). It is much more common in Japan and the Caribbean islands than other parts of the world. Adult T cell leukemia-lymphoma often grows quickly, but in some cases it advances slowly, or even shrinks on its own for a time.
- Primary cutaneous anaplastic large cell lymphoma (C-ALCL): This lymphoma usually starts as one or a few tumors on the skin, which can vary in size. Some of these may break open (ulcerate). Most people with this disease are in their 50s or 60s, but it can also occur in children. It is found at least twice as often in men as in women. In most cases it does not spread beyond the skin, and the prognosis (outlook) is very good.
- Lymphomatoid papulosis: This is a benign, slow-growing disease that often comes and goes on its own, even without treatment. In fact, some doctors think of it not as a lymphoma, but rather as an inflammatory disease that might progress to a lymphoma. But under a microscope, it has features that look like primary cutaneous anaplastic large cell lymphoma (C-ALCL). Lymphomatoid papulosis often begins as several large pimple-like lesions that may break open in the middle. Lymphomatoid papulosis is seen in younger people more often than other T-cell skin lymphomas, with an average age of around 45. Men get this disease more often than women. Lymphomatoid papulosis often goes away without treatment, but it can take anywhere from a few months to many years to go away completely. Lymphomatoid papulosis doesn’t spread to internal organs and is not fatal. Rarely, some people with this skin disorder develop another, more serious type of lymphoma.
- Subcutaneous panniculitis-like T-cell lymphoma: Subcutaneous panniculitis-like T-cell lymphoma is a rare lymphoma that invades the deepest layers of the skin, where it causes nodules (lumps) to form. Most often these are on the legs, but they can occur anywhere on the body. Subcutaneous panniculitis-like T-cell lymphoma affects all ages and both sexes equally. It usually grows slowly and tends to have a good outlook.
- Extranodal NK/T-cell lymphoma, nasal type: Extranodal NK/T-cell lymphoma, nasal type is a rare type of lymphoma can start in T-cells or in other lymphocytes known as natural killer (NK) cells. It typically starts in the nose or sinuses, but sometimes it can start in the skin. Extranodal NK/T-cell lymphoma, nasal type has been linked to infection with the Epstein-Barr virus (EBV), and is more common in Asia and Central and South America. It tends to grow quickly.
- Primary cutaneous peripheral T-cell lymphoma, rare subtypes: This is a group of rare skin lymphomas that don’t fit into any of the above categories. There are several types.
- Primary cutaneous gamma/delta T-cell lymphoma develops as thickened plaques (raised lesions) or actual tumors, mainly on skin of the arms and legs, but sometimes in the intestines or lining of the nose. This type of lymphoma tends to grow and spread quickly.
- Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T-cell lymphoma develops as widespread patches, nodules and tumors that often break open in the middle. This type of lymphoma can sometimes look like mycosis fungoides, but a biopsy can tell them apart. This lymphoma tends to grow and spread quickly.
- Primary cutaneous acral CD8+ T-cell lymphoma is very rare, and typically starts as a nodule on the ear, although it can also start on other parts of the body, such as the nose, hand, or foot. It tends to grow slowly and can often be cured with treatment.
- Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder often starts as a single area of thickening of the skin or a tumor on the head, neck, or upper body. This disease tends to grow slowly and can often be cured with treatment.
Adult T-cell leukemia/lymphoma: This lymphoma is caused by infection with a virus called HTLV-1. It is rare in the United States, and much more common in Japan, the Caribbean, and parts of Africa – where infection with HTLV-1 is more common. It can affect the bone marrow (where new blood cells are made), lymph nodes, spleen, liver, skin, and other organs. There are 4 subtypes:
- The smoldering subtype tends to grow slowly and has a good prognosis.
- The chronic subtype also grows slowly and has a good prognosis.
- The acute subtype is the most common. It grows quickly like acute leukemia, so it needs to be treated right away.
- The lymphoma subtype grows more quickly than the chronic and smoldering types, but not as fast as the acute type.
Angioimmunoblastic T-cell lymphoma: This lymphoma accounts for about 4% of all lymphomas. It is more common in older adults. It tends to involve the lymph nodes as well as the spleen or liver, which can become enlarged. People with this lymphoma usually have fever, weight loss, and skin rashes and often develop infections. This lymphoma often progresses quickly. Treatment is often effective at first, but the lymphoma tends to come back (recur).
Extranodal natural killer/T-cell lymphoma, nasal type: This rare type often involves the upper airway passages, such as the nose and upper throat, but it can also invade the skin, digestive tract, and other organs. It is much more common in parts of Asia and South America. Cells of this lymphoma are similar in some ways to natural killer (NK) cells, another type of lymphocyte.
Enteropathy-associated intestinal T-cell lymphoma (EATL): EATL is a lymphoma that occurs in the lining of the intestine. This lymphoma is most common in the small intestine, but can also occur in the colon. Symptoms can include severe abdominal (belly) pain, nausea, and vomiting. There are 2 subtypes of this lymphoma:
- Type I enteropathy-associated intestinal T-cell lymphoma (EATL) occurs in some people with celiac disease (also called gluten-sensitive enteropathy). Celiac disease is an autoimmune disease in which eating gluten, a protein found mainly in wheat and barley, causes the immune system to attack the lining of the intestine and other parts of the body. Type I EATL is rare among people who have had celiac disease since childhood, and is more common in people diagnosed as older adults. This lymphoma is more common in men than women.
- Type II enteropathy-associated intestinal T-cell lymphoma (EATL) is not linked to celiac disease and is less common than type I.
Anaplastic large cell lymphoma (ALCL): About 2% of lymphomas are of this type. It is more common in young people (including children), but it can also affect older adults. This type of lymphoma tends to be fast-growing, but many people with this lymphoma can be cured.
There are different forms of anaplastic large cell lymphoma (ALCL):
- Primary cutaneous anaplastic large cell lymphoma (ALCL) only affects the skin. This is discussed in more detail in Lymphoma of the Skin.
- Systemic anaplastic large cell lymphoma (ALCL) can affect the lymph nodes and other organs, including the skin. Systemic ALCL is divided into 2 types based on whether the lymphoma cells have a change in the ALK gene. ALK-positive ALCL is more common in younger people and tends to have a better prognosis (outlook) than the ALK-negative type.
- Breast implant-associated anaplastic large cell lymphoma (ALCL) is a rare type of ALCL that can develop in the breasts of women who have had implants. It seems to be more likely to occur if the implant surfaces are textured (as opposed to smooth).
Peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS): This name is given to T-cell lymphomas that don’t readily fit into any of the groups above. Most people diagnosed with these lymphomas are in their 60s. These lymphomas often involve the lymph nodes, but they can affect the skin, bone marrow, spleen, liver, and digestive tract, as well. As a group, these lymphomas tend to be widespread and grow quickly. Some patients respond well to chemotherapy, but over time these lymphomas tend to become harder to treat.
Non hodgkin’s lymphoma signs and symptoms
The most common symptom of non-Hodgkin lymphoma is a painless swelling in a lymph node, usually in the neck, armpit or groin.
Some people have no symptoms and the disease may only be discovered during a routine medical examination or while the patient is under care for an unrelated condition.
B Symptoms. Fever, drenching night sweats and loss of more than 10 percent of body weight over six months are sometimes termed “B symptoms” and are significant to the prognosis and staging of the disease. Other non-Hodgkin’s lymphoma symptoms, such as itching and fatigue, do not have the same prognostic importance as the symptoms designated as B symptoms. Furthermore, they are not considered to be B symptoms.
Non-Hodgkin lymphoma can cause many symptoms, such as:
- Painless swelling in one or more lymph node(s)
- Unexplained weight loss
- Fever
- Soaking night sweats
- Coughing, trouble breathing or chest pain
- Weakness and tiredness that don’t go away
- Loss of appetite
- Pain, swelling or a feeling of fullness in the abdomen (due to an enlarged spleen)
- Itchy skin
- Enlargement of the spleen or liver
- Rashes or skin lumps
A few people with lymphoma have abnormal cells in their bone marrow when they’re diagnosed.
This may lead to:
- persistent tiredness or fatigue
- an increased risk of infections
- excessive bleeding, such as nosebleeds, heavy periods and spots of blood under the skin
Non-Hodgkin’s lymphoma causes
Non-Hodgkin lymphoma is caused by a change (mutation) in the DNA of a type of white blood cell called lymphocytes, although the exact reason why this happens isn’t known. Non-Hodgkin lymphoma can occur at any age, but a third cases are diagnosed in people 60 or over and the condition is slightly more common in men than women.
Non-Hodgkin’s lymphoma usually starts with an abnormal change in a white cell in a lymph node or lymphoid tissue called a lymphocyte. It can start in one of three major types of lymphocytes:
- B lymphocytes (B cells): B cells normally help protect the body against germs (bacteria or viruses) by making proteins called antibodies. The antibodies attach to the germs, marking them for destruction by other parts of the immune system.
- T lymphocytes (T cells): There are several types of T cells. Some T cells destroy germs or abnormal cells in the body. Other T cells help boost or slow the activity of other immune system cells.
- Natural killer (NK) cells, which attack virus-infected cells or tumor cells
About 85 percent of non-Hodgkin’s lymphoma cases start in the B cells. Your doctor plans your treatment according to the type of cell your non-Hodgkin’s lymphoma developed in.
The abnormal lymphocyte grows out of control and produces more abnormal cells like it.
- These abnormal lymphocytes (lymphoma cells) accumulate and form masses (tumors). If non-Hodgkin’s lymphoma isn’t treated, the cancerous cells crowd out normal white cells, and the immune system can’t guard against infection effectively.
- Non-Hodgkin’s lymphoma that develops in or spreads to other areas of the body where lymphoid tissue is found, such as the spleen, digestive tract and bone marrow, is called primary extranodal lymphoma.
- Non-Hodgkin’s lymphoma is classified into more than 30 different subtypes. Doctors classify the non-Hodgkin’s lymphoma subtypes into categories that describe how rapidly or slowly the disease is progressing:
- Aggressive non-Hodgkin’s lymphoma
- Indolent (slow-growing) non-Hodgkin’s lymphoma
Risk Factors non-Hodgkin’s lymphoma
The exact cause of non-Hodgkin’s lymphoma is not known but there are risk factors that may increase a person’s likelihood of developing the disease.
Immune suppression is one of the most clearly established risk factors for non-Hodgkin’s lymphoma. People with autoimmune disease, acquired immunodeficiencies including human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS), and organ transplant recipients have an elevated risk for non-Hodgkin’s lymphoma. In addition, factors that suppress the immune system, such as chemical exposures or treatments for autoimmune diseases, may contribute to the development of non-Hodgkin’s lymphoma.
Farming communities have a higher incidence of non-Hodgkin’s lymphoma. Some studies suggest that specific ingredients in herbicides and pesticides such as organochlorine, organophosphate and phenoxy acid compounds, are linked to lymphoma. The number of lymphoma cases caused by such exposures has not been determined. More studies are needed to understand these associations.
Exposure to certain viruses and bacteria is associated with non-Hodgkin’s lymphoma. It is thought that infection with either a virus or a bacterium can lead to intense lymphoid cell proliferation, increasing the probability of a cancer-causing event in a cell. Here are some examples:
- Epstein-Barr virus (EBV) infection
- Human T-cell lymphotropic virus-1 (HTLV-1)
- Human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS)
- The bacterium Helicobacter Pylori (H Pylori)
- Hepatitis C
Other conditions, such as Sjögren syndrome, Wiskott-Aldrich syndrome and Klinefelter syndrome can predispose individuals to later development of non-Hodgkin’s lymphoma.
Non-Hodgkin lymphoma isn’t infectious and isn’t thought to run in families, although your risk may be slightly increased if a first-degree relative (such as a parent or sibling) has had lymphoma.
Non-Hodgkin lymphoma diagnosis
Most people with non-Hodgkin lymphoma (NHL) see their doctor because they have felt a lump that hasn’t gone away, they develop some of the other symptoms of non-Hodgkin’s lymphoma, or they just don’t feel well and go in for a check-up.
Your doctor will likely ask you about your personal and family medical history. He or she may then have you undergo tests and procedures used to diagnose non-Hodgkin’s lymphoma, including:
- Physical exam. Your doctor checks for swollen lymph nodes, including in your neck, underarm and groin, as well as for a swollen spleen or liver.
- Blood and urine tests. Blood and urine tests may help rule out an infection or other disease.
- Imaging tests. Your doctor may recommend imaging tests to look for signs of lymphoma cells elsewhere in your body. Tests may include CT, MRI and positron emission tomography (PET).
- Lymph node test. Your doctor may recommend a lymph node biopsy procedure to remove all or part of a lymph node for laboratory testing. Analyzing lymph node tissue in a lab may reveal whether you have non-Hodgkin’s lymphoma and, if so, which type.
- Bone marrow test. A bone marrow biopsy and aspiration procedure involves inserting a needle into your hipbone to remove a sample of bone marrow. The sample is analyzed to look for non-Hodgkin’s lymphoma cells.
- Lumbar puncture (spinal tap). If there’s a concern that the lymphoma may affect the fluid around your spinal cord, your doctor might recommend a procedure to remove some of the fluid for testing. During a spinal tap, the doctor inserts a small needle into the spinal canal in your lower back.
Other tests and procedures may be used depending on your situation.
The only way to confirm a diagnosis of non-Hodgkin lymphoma is by carrying out a biopsy. This is a minor surgical procedure where a sample of affected lymph node tissue is removed and studied in a laboratory.
Lymph Node Biopsy
Diagnosing non-Hodgkin lymphoma usually involves performing a lymph node biopsy. If the biopsy confirms that you have the disease, your doctor performs additional tests to stage the lymphoma.
A lymph node biopsy’s purpose is to confirm a diagnosis and:
- Identify your non-Hodgkin’s lymphoma subtype
- Develop a treatment plan
Lab Tests to Confirm a Diagnosis
After your doctor takes samples of your lymph node and tissues, a hematopathologist examines them under a microscope to look for identifying characteristics of non-Hodgkin’s lymphoma. He or she confirms a diagnosis and identifies the NHL subtype. A hematopathologist is a specialist who studies blood cell diseases by looking at samples of blood and bone marrow cells and other tissues.
The hematopathologist uses one or more lab tests such as those below to examine your cells:
- Immunophenotyping
- Flow cytometry
- Cytogenetic analysis
- Gene expression profiling and microarray analysis
- Polymerase chain reaction (PCR)
Since non-Hodgkin’s lymphoma is a difficult disease to diagnose, you may want to get a second medical opinion by an experienced hematopathologist before you begin treatment. Some types of NHL can be confused with each other. The appropriate treatment depends on having the correct diagnosis.
Staging Tests
Once your doctor confirms an non-Hodgkin’s lymphoma diagnosis, he or she runs more tests to stage your disease. Staging identifies the extent of your disease and where it’s located in your body.
Staging tests include:
- Physical exam
- Biopsies of enlarged lymph nodes or other abnormal areas
- Blood tests
- Imaging tests, such as PET and CT scans
- Bone marrow aspiration and biopsy (often but not always done)
- Lumbar puncture (spinal tap – this may not need to be done)
Imaging Tests
Your doctor conducts one or more imaging tests (also called diagnostic radiology), along with a physical exam, to look for:
- The location and distribution of lymph node enlargement
- Whether organs other than the lymph nodes are involved
- If there are very large masses of tumors in one site or another.
Imaging tests may include:
- Chest x-rays
- CT (computed tomography) scan
- FDG-PET (fluorodeoxyglucose (FDG) positron emission tomography) scan
- Magnetic resonance imaging (MRI)
- PET-CT scan
Blood Tests
After your blood is taken, it’s sent to a lab for a complete blood count (CBC) and more blood work. Blood tests are used to:
- Determine whether lymphoma cells are present in the blood and if the special proteins (called “immunoglobulins”) made by lymphocytes are either deficient or abnormal
- Check indicators of disease severity by examining blood protein levels, uric acid levels and erythrocyte sedimentation rate (ESR)
- Assess kidney and liver functions
- Measure two important biological markers, lactate dehydrogenase (LDH) and beta2-microglobulin which are helpful prognostic indicators for several NHL subtypes
A complete blood count (CBC) may show:
- Anemia (low red blood cell counts)
- Neutropenia (low levels of neutrophils, a type of white blood cells)
- Thrombocytopenia (low platelet levels)
Bone Marrow Biopsy
Most patients diagnosed with NHL undergo a bone marrow biopsy to make sure there is no spread of the disease to the bone marrow and to evaluate the use of specific therapies including radioimmunotherapy (a combination of radiation therapy and immunotherapy). A bone marrow biopsy may not always be required for patients with early-stage disease who also have low-risk features, for example, NHL with no B symptoms and no large masses.
Other Tests for Specific Subtypes
Certain tests are performed for specific subtypes only and not necessary for all patients with NHL. They include:
- Full evaluation of the gastrointestinal (GI) tract, including upper and lower endoscopies for patients who have disease involving the GI tract, such as MALT lymphoma
- Colonoscopy for patients with mantle cell lymphoma (routine colonoscopy is important for all persons beginning at age 50, or earlier if there is a family history of colon cancer)
- Testicular ultrasound for patients who have a testicular mass
- Spinal tap (lumbar puncture) and/or MRI of the brain or spinal column may be required for patients with certain subtypes or symptoms that suggest central nervous system involvement.
Non-Hodgkin’s lymphoma Staging
After someone is diagnosed with Non-Hodgkin Lymphoma, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Staging helps your doctor predict the disease’s progression and develop a treatment plan.
The current staging system for non-Hodgkin lymphoma in adults is known as the Lugano classification, which is based on the older Ann Arbor system. The stages are described by Roman numerals I through IV (1-4). Limited stage (I or II) lymphomas that affect an organ outside the lymph system (an extranodal organ) have an E added (for example, stage IIE).
Non-Hodgkin’s lymphoma doesn’t always begin in stage I and spread to more advanced stages. More than half of all patients with intermediate or aggressive disease and more than 80 percent of all patients with indolent disease are diagnosed with stage III or IV non-Hodgkin lymphoma. And if someone is diagnosed in stage IV, it doesn’t mean that the disease is incurable – it may be highly curable depending on the subtype. “Stage IV” does not have the same implications in non-Hodgkin lymphoma as it does for many other cancers.
Table 13. Non-Hodgkin’s lymphoma stages
| Stage | Number and Location of Affected Lymph Nodes and Organs |
|---|---|
| Stage I | Involvement of one lymph node or a group of adjacent nodes The cancer is found only in 1 area of a single organ outside of the lymph system (IE). |
| Stage II | Involvement of two or more lymph node regions on the same side of the diaphragm (the thin band of muscle that separates the chest and abdomen) The lymphoma is in a group of lymph node(s) and in one area of a nearby organ (IIE). It may also affect other groups of lymph nodes on the same side of the diaphragm. |
| Stage III | Involvement of two or more lymph node regions above and below the diaphragm (for example, neck, chest and abdomen) |
| Stage IV | Involvement of lymph node regions on both sides of the diaphragm and involvement of organs such as the lungs, liver or bones |
Categories A, B, X, S and E
The four stages of Non-Hodgkin’s lymphoma can be divided into categories:
- A Category: “A” is put after your stage if you have no additional symptoms other than swollen lymph nodes.
- B Category: “B” is put after your stage if you have additional symptoms of fever, drenching night sweats, loss of more than 10 percent of body weight over the previous six months (without dieting)
- X Category: “Bulky disease”. This term is often used to describe large tumors in the chest. This is a nodal mass whose greatest size is usually more than 10 cm or more than onethird of the chest diameter by x-ray. It is especially important for stage II lymphomas, as bulky disease might need more intensive treatment.
- E Category: Involvement of organs or tissues beyond the lymph system
- S Category: “S” stands for spleen and means the lymphoma is found in this organ.
For example, stage IIB indicates that the patient has
- Two lymph node sites near each other with disease involvement (for example, enlarged lymph nodes in the neck and near the collarbone, or in the neck and the armpit)
- Fever, excessive sweating and/or weight loss (any one of these symptoms).
When all the diagnostic and staging tests are completed, the doctor will evaluate the information, identify the non-Hodgkin’s lymphoma subtype, determine which areas of the body are involved and begin to discuss treatment options with the patient.
Figure 8. Non-Hodgkin Lymphoma Stages
Non-Hodgkin’s lymphoma Subtypes
More than 60 specific Non-Hodgkin’s lymphoma subtypes have been identified and assigned names by the World Health Organization (WHO). NHL subtypes are categorized by the characteristics of the lymphoma cells, including their appearance, the presence of proteins on the surface of the cells and their genetic features. It’s important to know your subtype since it plays a large part in determining the type of treatment you’ll receive. A hematopathologist, a doctor who specializes in the diagnosis of blood disorders and blood cancers, should review your biopsy specimens.
Specialists further characterize the Non-Hodgkin’s lymphoma subtypes according to how the disease progresses:
- Aggressive lymphomas are fast-moving and account for about 60 percent of all NHL cases. Diffuse large B-cell lymphoma (DLBCL) is the most common aggressive NHL subtype.
- Indolent lymphomas are slow-moving and tend to grow more slowly and have fewer signs and symptoms when first diagnosed. Slow-growing or indolent subtypes represent about 40 percent of all NHL cases. Follicular lymphoma (FL) is the most common subtype of indolent Non-Hodgkin’s lymphoma.
The treatments for aggressive and indolent lymphomas are different. When a patient’s rate of disease progression is between indolent and aggressive, he or she is considered to have “intermediate grade” disease. Some cases of indolent Non-Hodgkin’s lymphoma can transform into aggressive Non-Hodgkin’s lymphoma.
Table 14. Most Common Subtypes of Non-Hodgkin’s Lymphoma
| Most Common Subtypes of Non-Hodgkin Lymphoma |
|---|
Aggressive
|
Indolent
|
Below are the Non-Hodgkin’s lymphoma diagnostic designations of the subtypes for non-Hodgkin lymphoma. The descriptive part of the names (eg, follicular, mantle cell or marginal zone) in some disease subtypes refers to the specific areas of the lymph nodes (the follicle, mantle and marginal zones) where the lymphoma appears to have originated.
Table 15. Diagnostic Designations for Non-Hodgkin’s Lymphoma Subtypes
| Diagnostic Designations for Non-Hodgkin Lymphoma (NHL) Subtypes |
|---|
Mature B-cell lymphomas
|
Mature T-cell and NK-cell lymphomas
|
Non-Hodgkin’s lymphoma Treatment
It’s important that your doctor is experienced in treating patients with non-Hodgkin lymphoma (NHL) or works in consultation with an NHL specialist. This type of specialist is usually called a hematologist oncologist.
Types of Treatment
Doctors use several types of approaches and treatment combinations for non-Hodgkin’s lymphoma, some at different stages:
- Chemotherapy and other drug therapy. Chemotherapy is a widely used treatment for non-Hodgkin lymphoma that involves using medicine to kill cancer cells. Chemotherapy may be used on its own, combined with biological therapy, or combined with radiotherapy. The medication can be given in a number of different ways, depending on the stage of your cancer. You’ll normally get chemotherapy through a drip directly into a vein (intravenous chemotherapy), as tablets taken by mouth, or a combination of both. If there’s a risk of the cancer spreading to your brain, you may have chemotherapy injections directly into the cerebrospinal fluid around your spine. Chemotherapy is usually given over a period of a few months on an outpatient basis, which means you get treatment during the day and shouldn’t have to stay in hospital overnight.
- Steroid medication. Steroid medication is commonly used in combination with chemotherapy to treat non-Hodgkin lymphoma. This is because research has shown that using steroids makes the chemotherapy more effective. The steroid medication is normally given as tablets or injections, usually at the same time as your chemotherapy. You’ll usually take the steroids for a few days or 1 week during each cycle of chemotherapy, and take breaks in between. This helps to reduce the side effects.
- Radiation therapy (radiotherapy), usually combined with chemotherapy. Radiotherapy is most often used to treat early-stage non-Hodgkin lymphoma, where the cancer is only in 1 part of the body. Treatment is normally given in short daily sessions, Monday to Friday, usually for no more than 3 weeks. You shouldn’t have to stay in hospital between appointments. Radiotherapy itself is painless, but it can have some significant side effects. These can vary, depending on which part of your body is being treated.
- Targeted drug therapy. Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. For non-Hodgkin’s lymphoma, targeted drugs can be used alone, but are often combined with chemotherapy. This combination can be used as your initial treatment and as a second treatment if your lymphoma comes back.
- Immunotherapy. Immunotherapy is treatment that either boosts the patient’s own immune system or uses man-made versions of the normal parts of the immune system to kill lymphoma cells or slow their growth. Immunotherapy drugs may be an option for certain types of non-Hodgkin’s lymphoma if other treatments haven’t helped.
- Monoclonal antibody therapy. For some types of non-Hodgkin lymphoma, you may have a type of medication called a monoclonal antibody. These medications attach themselves to both healthy and cancerous cells, and signal to the immune system to attack and kill the cells. You may be given monoclonal antibody therapy as your only treatment, or they’re sometimes given in combination with chemotherapy to make the treatment more effective. For some types of non-Hodgkin lymphoma, you may continue having monoclonal antibody treatment regularly for up to 2 years after initial treatment, in combination with chemotherapy. This can reduce the chances of the cancer coming back in the future.
- Chimeric antigen receptor (CAR)-T cell therapy. A specialized treatment called chimeric antigen receptor (CAR)-T cell therapy takes your body’s germ-fighting T cells, engineers them to fight cancer and infuses them back into your body. CAR-T cell therapy might be an option for certain types of B-cell non-Hodgkin’s lymphoma that haven’t responded to other treatments.
- Stem cell transplantation (bone marrow transplant). Bone marrow transplant or stem cell transplant, involves using high doses of chemotherapy and radiation to suppress your bone marrow and immune system. Then healthy bone marrow stem cells from your body or from a donor are infused into your blood where they travel to your bones and rebuild your bone marrow. For people with non-Hodgkin’s lymphoma, a bone marrow transplant might be an option if other treatments haven’t helped.
- Watch-and-wait. If the disease is low grade (slow developing) and you’re well, a period of “watch and wait” is often recommended. This is because some people take many years to develop troublesome symptoms and starting treatment immediately is often felt to be unnecessary. If watch and wait is recommended, you’ll be seen regularly for reviews and invited to come back at any stage if you feel your symptoms are getting worse.
- Your doctor may suggest that you participate in a clinical trial. Clinical trials can involve therapy with new drugs and new drug combinations or new approaches to stem cell transplantation.
Some common drug combinations used in the treatment of Non-Hodgkin Lymphoma (NHL)
- CHOP: cyclophosphamide, doxorubicin (hydroxydoxorubicin), Oncovin® (vincristine), prednisone
- B+R: bendamustine hydrochloride (Bendeka®) plus rituximab
- R+ICE: rituximab plus ifosfamide, carboplatin, etoposide
- R-CHOP: rituximab plus cyclophosphamide, doxorubicin (hydroxydoxorubicin), Oncovin® (vincristine), prednisone
- R-HCVAD: rituximab plus cyclophosphamide, vincristine, adriamycin (doxorubicin), dexamethasone
- R-EPOCH: rituximab plus adjusted etoposide, prednisone, vincristine (Oncovin®), cyclophosphamide, doxorubicin
- DHAP: dexamethasone, high-dose cytarabine (ara-C®) and cisplatin (Platinol®)
- ICE: ifosfamide, carboplatin, etoposide
There can also be vast differences between treatment for aggressive non-Hodgkin’s lymphoma and treatment for indolent non-Hodgkin’s lymphoma. Every patient should discuss treatment options with his or her doctor and ask for help to understand the benefits and risks of different treatment approaches. The most effective treatment plan for each patient with non-Hodgkin lymphoma is individualized based on:
- The subtype of non-Hodgkin lymphoma—knowing whether the lymphoma cells are related to T cells, B cells or natural killer (NK) cells gives the doctor important clues about appropriate treatments
- The stage and category of the disease, which is important information that is factored into treatment decisions
- The presence or absence of fever, drenching night sweats and loss of more than 10 percent of body weight over 6 months, referred to as “B symptoms”
- Whether there is lymphoma in areas of the body outside of the lymph nodes (extranodal involvement)
- Other prognostic factors, such as age and any underlying medical conditions.
The patient’s age may be a factor, but older age is no longer a major determinant in treatment decisions for most patients. However, the patient’s overall health status, including other medical problems, and also his or her wishes concerning treatment are significant considerations. When making treatment decisions, it is important to discuss effects on fertility and other possible long-term and late effects of treatment.
Pretreatment Considerations
Adults of childbearing age and parents of children diagnosed with non-Hodgkin’s lymphoma should ask their doctors for information that may lessen the risk for infertility.
Finding the Best Treatment Approach
The goal of non-Hodgkin’s lymphoma treatment is to destroy as many lymphoma cells as possible to induce a complete remission (no trace of the disease). Patients who go into remission are sometimes cured of the disease.
Treatment can keep non-Hodgkin’s lymphoma in check for many years, even if tests show some lingering lymphoma cells. This is called partial remission.
The treatment your doctor recommends is based on several factors, including:
- Your disease subtype
- Whether your disease is aggressive (fast growing) or indolent (slow growing)
- Your disease stage and category
- Whether the lymphoma is in areas of your body other than your lymph nodes (extranodal involvement)
- Your overall health and whether you have any conditions like heart disease, kidney disease, lung disease, diabetes or anemia
As you develop a treatment plan with your doctor, be sure to discuss:
- The results you can expect from treatment
- Potential side effects, including long-term and late-term effects
- The possibility of participating in a clinical trial, where you’ll have access to advanced medical treatment that may be more beneficial to you than standard treatment
You may find it helpful to bring a loved one with you to your doctor’s visits for support, to take notes and ask follow-up questions. It’s a good idea to prepare questions you’d like to ask when you visit your doctor. You can also record your conversations with your doctor and listen more closely when you get home.
Treatment for Aggressive Non-Hodgkin’s lymphoma Subtypes
Aggressive non-Hodgkin lymphoma (NHL) progresses rapidly. It makes up about 60 percent of all non-Hodgkin’s lymphoma cases in the United States. Aggressive subtypes include:
- AIDS-associated lymphoma
- Burkitt lymphoma
- Central nervous system (CNS) lymphoma
- Diffuse large B-cell lymphoma (DLBCL)
- Mantle cell lymphoma
- Peripheral T-cell lymphoma (PTCL)
Patients with fast-growing non-Hodgkin’s lymphoma are frequently treated with chemotherapy that consists of four or more drugs. In most cases, this is the combination therapy called R-CHOP (rituximab [Rituxan®], cyclophosphamide [Cytoxan®], doxorubicin [hydroxydoxorubicin], Oncovin® [vincristine] and prednisone). This intensive, multidrug chemotherapy can be very effective for aggressive lymphoma, and cures have been achieved. Chemotherapy can be supplemented by radiation therapy in select cases, for instance, when large NHL masses are found during the diagnostic and staging process.
Treating Specific Aggressive Subtypes
AIDS-Associated Lymphoma
The types of non-Hodgkin lymphoma that are most often seen in people with acquired immune deficiency syndrome (AIDS) are diffuse large B-cell lymphoma, Burkitt lymphoma and primary central nervous system (CNS) lymphoma. Treatment outcomes depend on how well the patient with AIDS responds to therapy and manages the effects of chemotherapy on blood counts. Because AIDS already leads to low blood cell counts, chemotherapy must be carefully considered to determine whether the chemotherapy’s additional effects on blood levels can be managed. The number of people developing AIDS-associated non-Hodgkin lymphoma has decreased in the last several years because of improved treatment of HIV, the virus that can lead to AIDS.
The use of highly active anti-retroviral therapy (HAART) to treat HIV has helped patients to better tolerate treatments such as chemotherapy and immunotherapy.
Burkitt Lymphoma
This B-cell subtype is considered to be highly aggressive. It may involve the jaw, bones of the face, bowel, kidneys, ovaries, bone marrow, blood, central nervous system (CNS) and other organs. Burkitt lymphoma was named after Dr. Dennis Burkitt, a surgeon who first identified the disease in children in Africa. In Africa, the disease usually appears in children as a mass in a facial bone, especially the jaw.
Doctors typically use highly aggressive chemotherapy to treat this subtype of non-Hodgkin’s lymphoma. Commonly used regimens include:
- CODOX-M/IVAC (cyclophosphamide, vincristine, doxorubicin and high-dose methotrexate) alternating with IVAC (ifosfamide, etoposide and high-dose cytarabine)
- Hyper-CVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin and dexamethasone) alternating with methotrexate and cytarabine
- DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin plus rituximab)
Participation in clinical trials is recommended for all patients with Burkitt lymphoma.
Central Nervous System Lymphoma
There are two types of central nervous system (CNS) lymphoma: primary and secondary. Primary CNS lymphoma starts in the brain and/or the spinal cord. It is often a feature of AIDS-associated lymphoma, although it may be related to other non-Hodgkin’s lymphoma subtypes as well. Secondary CNS lymphoma starts in another area of the body and spreads to the brain and/or spinal cord.
Both primary and secondary CNS lymphomas are uncommon. Standard treatment may include chemotherapy, glucocorticoid drugs and/or radiation therapy. Immunotherapy and high-dose chemotherapy with stem cell transplantation are being studied in clinical trials.
Diffuse Large B-Cell Lymphoma
Diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin’s lymphoma subtype, making up about 30 percent of all non-Hodgkin’s lymphoma cases in the United States. It affects mostly middle-aged and older adults. DLBCL usually starts in lymph nodes in the neck or abdomen and is characterized by masses of large B cells (lymphocytes). DLBCL grows rapidly and frequently involves the spleen, liver, bone marrow or other organs.
For some patients, DLBCL may be the initial diagnosis. For other patients, their indolent lymphomas such as small lymphocytic lymphoma or follicular lymphoma transform and become DLBCL.
DLBCL is frequently treated with a chemotherapy regimen that is made up of four or more drugs. One regimen is R-CHOP. Another more intense regimen is DA-EPOCH-R, which is a combination of dose-adjusted etoposide (Etopophos®, VePesid®, Toposar®), prednisone, vincristine (Oncovin®), cyclophosphamide, hydroxydoxorubicin (doxorubicin) plus rituximab.
Mantle Cell Lymphoma
Mantle cell lymphoma begins in the lymph nodes and spreads to the spleen, blood, bone marrow and sometimes the esophagus, stomach and intestines. This subtype originates from a lymphocyte in the mantle zone of the lymph node. This subtype usually occurs in people over age 50 and is found in more frequently in men than in women. Standard treatment is combination chemotherapy, either with or without autologous stem cell transplantation.
Peripheral T-Cell Lymphoma
Peripheral T-cell lymphoma (PTCL) refers to a group of aggressive non-Hodgkin’s lymphoma subtypes that originate in mature T-cell lymphocytes. PTCL generally affects people age 60 and older. The most common subtypes include:
- Peripheral T-cell, not otherwise specified (PTCL NOS) – This is the most common subtype of PTCL. It often involves lymph node sites but can also involve other areas such as the liver, bone marrow, gastrointestinal track and skin.
- Anaplastic Large Cell Lymphoma (ALCL) – This subtype usually starts in the lymph nodes and can spread to the skin. There are two main subtypes of ALCL:
- Systemic ALCL ALK-1 positive anaplastic large cell lymphoma – About 80 percent of patients with this subtype are cured. This disease is more common in young people.
- Systemic ALCL ALK-1 negative anaplastic large cell lymphoma – This subtype occurs mainly in older patients. Treatment with chemotherapy or radiation therapy is often less successful and a stem cell transplant may be discussed.
- Primary cutaneous anaplastic large cell lymphoma – This subtype mostly affects the skin, but other parts of the body may be involved.
- Hepatosplenic T-cell lymphoma – This subtype of PTCL starts in the liver and spleen and usually affects young men.
- Angioimmunoblastic T-cell lymphoma – This type of T-cell lymphoma often involves lymph nodes and the bone marrow. Many patients have “paraneoplastic symptoms” including fevers, rashes and abnormal protein levels in their blood.
- Extranodal natural killer/T-cell lymphoma – This subtype of lymphoma can occur in the nasal sinuses or in other parts of the body. It is usually a very aggressive lymphoma that requires both chemotherapy and radiation.
- Enteropathy-type intestinal T-cell lymphoma – This subtype develops in the small bowel of patients with untreated celiac disease.
Peripheral T-cell lymphoma is commonly treated with the regimens used for diffuse large B-cell lymphoma (DLBCL). Chemotherapy with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) or other drug combinations is the standard treatment for newly diagnosed peripheral T-cell lymphoma. For early-stage disease, radiation therapy may be added. Another option for some of these lymphomas might be the chemo combination of cyclophosphamide, doxorubicin, and prednisone, along with the monoclonal antibody brentuximab vedotin (Adcetris). A stem cell transplant may be recommended when possible.
If other treatments are no longer working, newer chemo drugs such as pralatrexate (Folotyn), targeted drugs such as bortezomib (Velcade) or belinostat (Beleodaq), or immunotherapy drugs such as alemtuzumab (Campath) and denileukin diftitox (Ontak) may be tried.
The outlook for these lymphomas is usually not as good as in diffuse large B-cell lymphoma (DLBCL), so taking part in a clinical trial of newer treatments is often a good option.
Treatment for Indolent Non-Hodgkin’s lymphoma Subtypes
Indolent non-Hodgkin lymphoma (NHL) subtypes progress slowly. They make up about 40 percent of all NHL cases in the United States. Indolent subtypes include:
- Cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome)
- Follicular lymphoma (FL)
- Lymphoplasmacytic lymphoma and Waldenström macroglobulinemia
- Marginal zone lymphoma and mucosa-associated lymphoid tissue (MALT) lymphoma
- Small cell lymphocytic lymphoma (SLL) and chronic lymphocytic leukemia (CLL)
Treatment for indolent NHL ranges from observation with careful monitoring (the watch-and-wait approach) to aggressive therapy. Indolent NHL management or treatment is highly individual. Your doctor considers a number of factors such as:
- Prognostic factors
- Stage of disease
- Age and other medical conditions.
Treating Specific Indolent Subtypes
Cutaneous T-Cell Lymphoma (Mycosis Fungoides and Sézary Syndrome)
Cutaneous T-cell lymphomas (CTCLs) are a group of non-Hodgkin’s lymphomas that develop primarily in the skin and may grow to involve lymph nodes, blood and other organs. This type of lymphoma originates in a T-cell. Mycosis fungoides is the most common type of CTCL, and is characterized by prominent skin involvement. When the malignant lymphocytes enter and accumulate in the blood, the disease is called Sézary syndrome.
Therapy for CTCL depends on the nature of the skin lesions and whether disease is present in the lymph nodes. Topical therapies are among the approaches used to treat the skin lesions. These include drugs applied directly to the skin combined with either ultraviolet light therapy or electron beam therapy. Ultraviolet light is used in conjunction with psoralen (a drug that becomes active when it is exposed to light); the combination therapy is often referred to as “PUVA” (psoralen and ultraviolet A) therapy.
If there is widespread involvement of lymph nodes and other sites, single- or multi-drug chemotherapy or extracorporeal photopheresis can be used. Extracorporeal photopheresis (ECP) is a method of removing blood from the body and treating it with ultraviolet light before returning it to the body. This treatment is recommended for patients either with, or at risk for, blood involvement such as that seen in Sézary syndrome.
Follicular Lymphoma (FL)
Follicular lymphoma (FL) is the second most common subtype of non-Hodgkin lymphoma (NHL), making up about 20 percent of all NHL cases. Most patients with FL are age 50 or older at diagnosis. Most follicular lymphoma cells have a specific chromosomal abnormality (a translocation between parts of chromosomes 14 and 18) that causes the production (overexpression) of the gene, BCL-2, which can make the cells resistant to therapy.
FL is a very slow-growing disease. Some patients may not need treatment for several years, whereas others may have extensive lymph node or organ involvement and need treatment right away. In a small percentage of patients, FL may transform into a more aggressive disease.
Stage I or stage II FL may be treated with:
- Watch-and-wait approach; patients with less advanced disease can be observed with periodic examinations and imaging tests.
- Radiation therapy
- Chemotherapy with rituximab (Rituxan®) followed by radiation therapy
- For patients with stage II FL who have large lymph nodes, stage III or stage IV FL or advanced-stage relapsed FL, treatment will be based on symptoms, the patient’s age and health status and the extent of the patient’s disease. Taking part in a clinical trial can also be a good treatment option. Other treatment options include:
- Radiation therapy to lymph nodes that are causing symptoms, or to a large localized mass, if one is present
- Single chemotherapy drugs in combination with rituximab. Examples of drugs used for treatment include cyclophosphamide (Cytoxan®), chlorambucil (Leukeran®) or bendamustine (Bendeka™)
- Chemotherapy combinations plus rituximab, such as R-CVP (rituximab plus cyclophosphamide, vincristine [Oncovin®], and prednisone) or R-CHOP (rituximab plus cyclophosphamide, hydroxydoxorubicin [doxorubicin], vincristine and prednisone)
- A radioactive monoclonal antibody, such as yttrium-90+ibritumomab tiuxetan (Zevalin®)
- Stem cell transplantation for some patients
- Idelalisib (Zydelig®) to treat patients who have relapsed FL and who have received at least two prior therapies
- Copanlisib (AliqopaTM) to treat adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies.
Doctors have created a scoring system called the Follicular Lymphoma International Prognostic Index that is used to predict which patients have a higher risk of the disease returning (recurring). Doctors design a treatment plan based upon the patients’ score. Factors that raise the risk for FL patients include:
- Older than 60
- Stage III or IV disease
- More than five lymph nodes involved
- An elevated level of lactic dehydrogenase (a type of protein) in the blood
- Hemoglobin concentration less than 12 g/dL.
Lymphoplasmacytic Lymphoma and Waldenström Macroglobulinemia
Lymphoplasmacytic lymphoma and Waldenström macroglobulinemia are both slow-growing types of lymphoma that originate in a B-lymphocyte precursor. Both subtypes can become more advanced and involve the lungs, the gastrointestinal tract and other organs.
One option for patients without symptoms is to take a watch-and-wait approach. Active treatment begins for patients only if symptoms develop. Therapy regimens may then include a combination of biological agents (monoclonal antibodies such as rituximab), signaling inhibitors (drugs that block cell growth and survival signals), and chemotherapy with alkylating agents such as chlorambucil (Leukeran®), melphalan (Alkeran®) and cyclophosphamide (Cytoxan®). The Bruton tyrosine kinase (BTK) inhibitor ibrutinib (Imbruvica®) has been approved by the FDA for the treatment of patients with symptomatic Waldenström macroglobulinemia.
A serious complication of both diseases is called hyperviscosity syndrome. Hyperviscosity syndrome may occur when the malignant cells secrete an abnormal protein that can thicken the blood. This leads to inadequate blood flow, causing such symptoms as headache, blurred vision and mental confusion. Hyperviscosity syndrome can be treated with plasmapheresis, a process of removing plasma from the blood. This is followed by treatment to control the lymphoma.
Marginal Zone Lymphoma and Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma
Marginal zone lymphoma can develop in either the lymph nodes (nodal) or outside the lymph nodes (extranodal). It begins in B lymphocytes in a part of the lymph tissue called the “marginal zone.” The disease tends to remain localized.
Marginal zone lymphoma includes several subtypes, each categorized by the type of tissue where the lymphoma forms.
- Gastric mucosa-associated lymphoid tissue (MALT) lymphoma usually develops in the stomach. Patients with MALT lymphoma may have a history of an autoimmune disease such as Hashimoto thyroiditis or Sjögren syndrome. A higher incidence of MALT lymphoma involving the stomach is seen in patients who have been infected with the bacterium H. pylori. Bacteria have also been implicated in other forms of MALT lymphoma. Treatment often includes potent combinations of antibiotics, which both eradicate the H. pylori infection and cause the lymphoma to regress. Many patients with H. pylori have been cured of MALT lymphoma without radiation or chemotherapy. For a small subset of patients, MALT lymphoma can transform into diffuse large B-cell lymphoma (DLBCL). These patients can benefit from treatments used for Diffuse Large B-cell Lymphoma.
- Extragastric MALT lymphoma begins outside the stomach and may form in almost any part of the body including other areas of the GI tract, salivary glands, thyroid, lung, skin and around the eye.
- Monocytoid B-cell lymphoma, also known as “nodal marginal zone B-cell lymphoma,” may be found in the spleen and blood. This form of NHL is generally treated like follicular lymphoma.
- Splenic marginal zone lymphoma (SMZL) begins in the spleen and may spread to the blood and bone marrow. One of the first signs of SMZL is an enlarged spleen; however, symptoms can be slow to develop. Splenic marginal zone lymphoma has been associated with hepatitis C infection. Treatment for hepatitis C with interferon (either alone or in combination with ribavirin) may result in a remission of the patient’s lymphoma.
For patients with splenic marginal zone lymphoma who do not have hepatitis C or any symptoms of lymphoma, the first treatment may be the watch-and-wait approach. Treatment is generally started when an enlarged spleen starts to cause symptoms or produces low white blood cell counts. For symptomatic patients who are hepatitis-C negative, treatment may include:
- Removal of the spleen
- Single-agent chemotherapy
- Combination chemotherapy
- Immunotherapy with rituximab
- Rituximab combined with chemotherapy.
Small Cell Lymphocytic Lymphoma (SLL) and Chronic Lymphocytic Leukemia (CLL)
Small cell lymphocytic lymphoma (SLL) and chronic lymphocytic leukemia (CLL) are similar NHL subtypes. They tend to affect the same age groups (median age of patients is 65 years), have common signs and symptoms and be slow-growing. The differences lie in where they develop: SLL mostly affects the lymph nodes and lymphoid tissue; CLL mostly affects blood and bone marrow but can spread to the lymph nodes.
Rituximab or a rituximab-containing regimen is used as first-line therapy for CLL/SLL . The Bruton’s tyrosine kinase (BTK) inhibitor ibrutinib (Imbruvica®) has also been approved as first-line therapy. The PI3K inhibitor idelalisib (Zydelig®) in combination with rituximab and the BCL-2 inhibitor venetoclax (Venclexta®) have been approved for use in patients with relapsed CLL/SLL. Bendamustine hydrochloride is a chemotherapy agent that has been approved for the treatment of CLL patients who have progressed during or within six months of treatment with rituximab or a rituximab-containing regimen.
- Lymphoma. https://www.cancer.org/cancer/lymphoma.html[↩]
- Swerdlow, S. H., Campo, E., Pileri, S. A., Harris, N. L., Stein, H., Siebert, R., Advani, R., Ghielmini, M., Salles, G. A., Zelenetz, A. D., & Jaffe, E. S. (2016). The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood, 127(20), 2375–2390. https://doi.org/10.1182/blood-2016-01-643569[↩][↩][↩][↩][↩]
- National Institutes of Health, National Cancer Institute. Surveillance, epidemiology, and end results program cancer stat facts: Hodgkin lymphoma. https://seer.cancer.gov/statfacts/html/hodg.html[↩][↩]
- National Institutes of Health, National Cancer Institute. Surveillance, epidemiology, and end results program cancer stat facts: Non-Hodgkin Lymphoma. https://seer.cancer.gov/statfacts/html/nhl.html[↩]
- Lymphoma: Diagnosis and Treatment. Am Fam Physician. 2020 Jan 1;101(1):34-41. https://www.aafp.org/afp/2020/0101/p34.html[↩][↩][↩][↩][↩]
- National Institutes of Health, National Cancer Institute. Surveillance, epidemiology, and end results program cancer stat facts: non-Hodgkin lymphoma. https://seer.cancer.gov/archive/csr/1975_2016/results_merged/sect_19_nhl.pdf[↩][↩]
- Ansell SM. Non-Hodgkin lymphoma: diagnosis and treatment. Mayo Clin Proc. 2015;90(8):1152–1163.[↩]
- Ansell SM. Hodgkin lymphoma: diagnosis and treatment. Mayo Clin Proc. 2015;90(11):1574–1583.[↩]
- Higdon ML, Atkinson CJ, Lawrence KV. Oncologic emergencies: recognition and initial management. Am Fam Physician. 2018;97(11):741–748. https://www.aafp.org/afp/2018/0601/p741.html[↩]
- Graus F, Ariño H, Dalmau J. Paraneoplastic neurological syndromes in Hodgkin and non-Hodgkin lymphomas. Blood. 2014;123(21):3230–3238.[↩]
- Sergentanis TN, Kanavidis P, Michelakos T, et al. Cigarette smoking and risk of lymphoma in adults: a comprehensive meta-analysis on Hodgkin and non-Hodgkin disease. Eur J Cancer Prev. 2013;22(2):131–150.[↩]
- Lichtman MA. Obesity and the risk for a hematological malignancy: leukemia, lymphoma, or myeloma. Oncologist. 2010;15(10):1083–1101.[↩]
- Questions and Answers about Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). https://www.fda.gov/medical-devices/breast-implants/questions-and-answers-about-breast-implant-associated-anaplastic-large-cell-lymphoma-bia-alcl[↩]
- Cerhan JR, Slager SL. Familial predisposition and genetic risk factors for lymphoma. Blood. 2015;126(20):2265–2273.[↩]
- Suarez F, Lecuit M. Infection-associated non-Hodgkin lymphomas. Clin Microbiol Infect. 2015;21(11):991–997.[↩]
- Yadlapati S, Efthimiou P. Autoimmune/inflammatory arthritis associated lymphomas: who is at risk? Biomed Res Int. 2016; 2016:8631061.[↩]
- Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 2011;117(19):5019–5032.[↩]
- Gaddey HL, Riegel AM. Unexplained lymphadenopathy: evaluation and differential diagnosis. Am Fam Physician. 2016;94(11):896–903. https://www.aafp.org/afp/2016/1201/p896.html[↩]
- Cheson BD, Fisher RI, Barrington SF, et al.; Alliance, Australasian Leukaemia and Lymphoma Group; Eastern Cooperative Oncology Group; European Mantle Cell Lymphoma Corsortium, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–3068.[↩][↩][↩]
- Torok JA, Wu Y, Chino J, et al. Chemotherapy or combined modality therapy for early-stage Hodgkin lymphoma. Anticancer Res. 2018;38(5):2875–2881.[↩][↩]
- National Comprehensive Cancer Network. NCCN guidelines & clinical resources. Hodgkin lymphoma guideline. https://www.nccn.org/professionals/physician_gls/pdf/hodgkins.pdf[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Swerdlow AJ, Higgins CD, Smith P, et al. Second cancer risk after chemotherapy for Hodgkin’s lymphoma: a collaborative British cohort study. J Clin Oncol. 2011;29(31):4096–4104.[↩]
- Pfreundschuh M, Trümper L, Osterborg A, et al.; MabThera International Trial Group. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol. 2006;7(5):379–391.[↩]
- National Comprehensive Cancer Network. NCCN guidelines & clinical resources. B-cell lymphomas guideline. https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf[↩][↩]
- National Comprehensive Cancer Network. NCCN guidelines & clinical resources. T-cell lymphoma. https://www.nccn.org/professionals/physician_gls/pdf/t-cell.pdf[↩][↩]
- Blank O, von Tresckow B, Monsef I, et al. Chemotherapy alone versus chemotherapy plus radiotherapy for adults with early stage Hodgkin lymphoma. Cochrane Database Syst Rev. 2017;(4):CD007110.[↩][↩]
- Torok JA, Wu Y, Chino J, et al. Chemotherapy or combined modality therapy for early-stage Hodgkin lymphoma. Anticancer Res. 2018;38(5):2875–2881[↩]
- Centers for Disease Control and Prevention. Adult immunization schedule: pneumococcal vaccine. https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html#note-pneumo[↩]
- Rubin LG, Levin MJ, Ljungman P, et al.; Infectious Diseases Society of America. . 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host [published correction appears in Clin Infect Dis. 2014;59(1):144]. Clin Infect Dis. 2014;58(3):e44–e100.[↩]
- Kroger AT, Duchin J, Vázquez M. General Best Practice Guidelines for Immunization. Best practices guidance of the Advisory Committee on Immunization Practices. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/downloads/general-recs.pdf[↩]
- Van Heertum RL, Scarimbolo R, Wolodzko JG, et al. Lugano 2014 criteria for assessing FDG-PET/CT in lymphoma: an operational approach for clinical trials. Drug Des Devel Ther. 2017;111719–1728.[↩]
- Armitage JO, Gascoyne RD, Lunning MA, et al. Non-Hodgkin lymphoma. Lancet. 2017;390(10091):298–310[↩]
- U.S. Preventive Services Task Force. Published recommendations. https://www.uspreventiveservicestaskforce.org/uspstf/[↩]
- Hiniker SM, Hoppe RT. Post-treatment surveillance imaging in lymphoma. Semin Oncol. 2017;44(5):310–322.[↩][↩][↩]
- Cohen JB, Kurtz DM, Staton AD, et al. Next-generation surveillance strategies for patients with lymphoma. Future Oncol. 2015;11(13):1977–1991.[↩][↩]
- El-Galaly TC, Jakobsen LH, Hutchings M, et al. Routine imaging for diffuse large B-cell lymphoma in first complete remission does not improve post-treatment survival: a Danish-Swedish population-based study. J Clin Oncol. 2015;33(34):3993–3998.[↩]
- Sarkozy C, Sehn LH. Management of relapsed/refractory DLBCL. Best Pract Res Clin Haematol. 2018;31(3):209–216.[↩]
- Bröckelmann PJ, Goergen H, Kohnhorst C, et al. Late relapse of classical Hodgkin lymphoma: an analysis of the German Hodgkin study group HD7 to HD12 trials. J Clin Oncol. 2017;35(13):1444–1450.[↩]
- Armitage JO, Gascoyne RD, Lunning MA, et al. Non-Hodgkin lymphoma. Lancet. 2017;390(10091):298–310.[↩]
- International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl JMed. 1993;329(14):987–994.[↩]
- Kaseb H, Babiker HM. Hodgkin Lymphoma. [Updated 2022 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499969[↩]
- What Is Hodgkin Lymphoma? https://www.cancer.org/cancer/hodgkin-lymphoma/about/what-is-hodgkin-disease.html[↩]
- American Cancer Society: Cancer Facts and Figures 2022. American Cancer Society, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf[↩]
- Hodgkin Lymphoma — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/hodg.html[↩]
- Brenner H, Gondos A, Pulte D. Ongoing improvement in long-term survival of patients with Hodgkin disease at all ages and recent catch-up of older patients. Blood. 2008 Mar 15;111(6):2977-83. doi: 10.1182/blood-2007-10-115493[↩]
- Surveillance, Epidemiology, and End Results Program. https://seer.cancer.gov/[↩]
- Cancer Stat Facts: Hodgkin Lymphoma. https://seer.cancer.gov/statfacts/html/hodg.html[↩][↩]
- Hodgkin Lymphoma Subtypes. http://www.lls.org/lymphoma/hodgkin-lymphoma/diagnosis/hodgkin-lymphoma-subtypes[↩][↩]
- Hodgkin Lymphoma Staging. http://www.lls.org/lymphoma/hodgkin-lymphoma/diagnosis/hodgkin-lymphoma-staging[↩][↩]
- Non-Hodgkin Lymphoma. https://www.lls.org/lymphoma/non-hodgkin-lymphoma[↩]
- Non-Hodgkin Lymphoma — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/nhl.html[↩]
- Key Statistics for Non-Hodgkin Lymphoma. https://www.cancer.org/cancer/non-hodgkin-lymphoma/about/key-statistics.html[↩]
- Cancer Stat Facts: Non-Hodgkin Lymphoma. https://seer.cancer.gov/statfacts/html/nhl.html[↩][↩][↩][↩]
- Non-Hodgkin Lymphoma. https://www.lls.org/sites/default/files/file_assets/PS58_NHL_Booklet_2020FINAL_rev.pdf[↩]