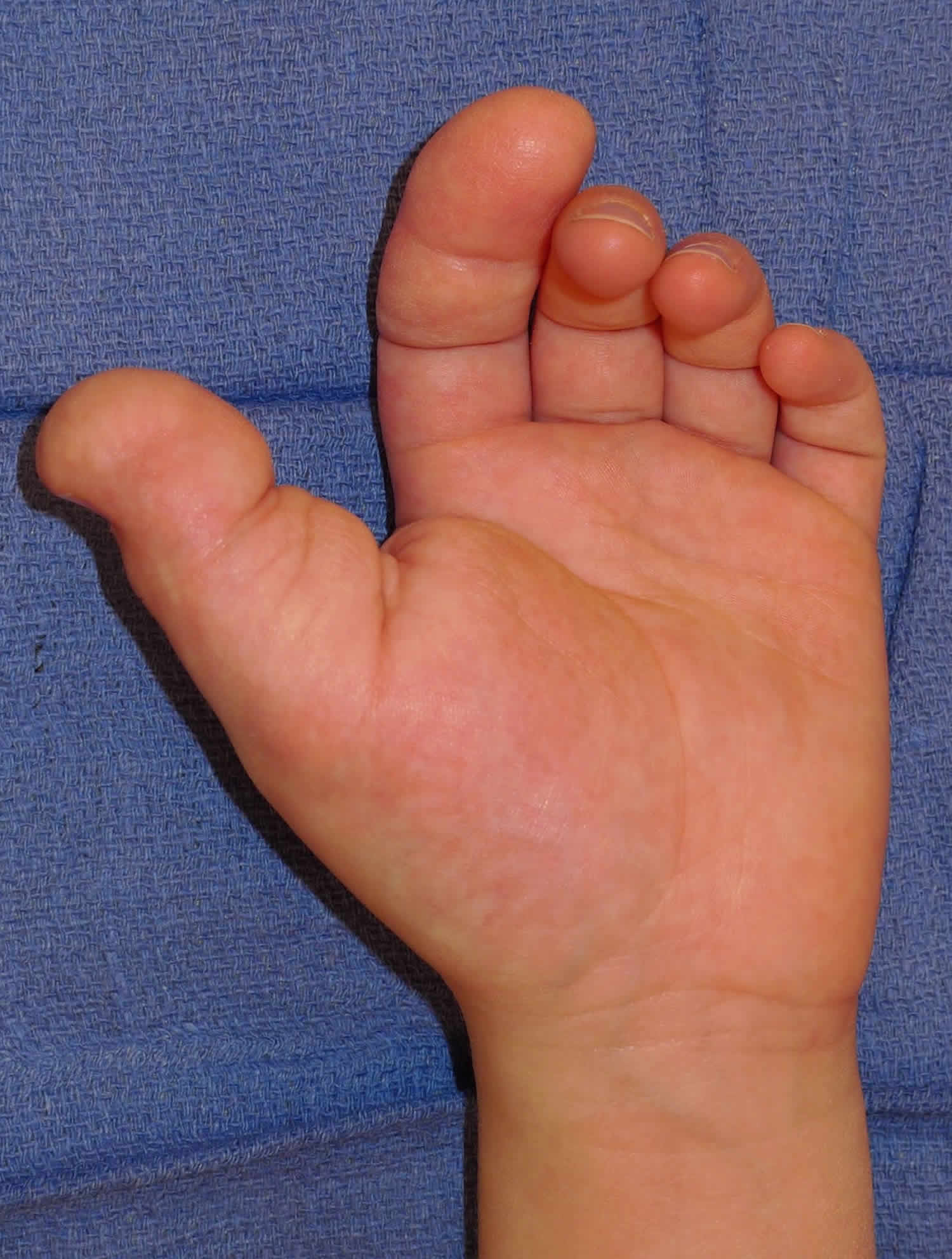
Macrodactyly
Macrodactyly is a rare congenital condition in which a baby is born with abnormally large fingers or toes due to an overgrowth of the underlying bones and soft tissue 1. The abnormality develops in one or more toes and involves thickening of both soft tissue and bone of the affected digit. (Figures 1 and 2). Macrodactyly is further characterized by increased size of all elements – tendons, nerves, vessels, subcutaneous fat, nails, skin and phalanges – all but the metatarsals. The increase of nerve size is
noticeable and the digit appears to be infiltrated with fatty tissue 2. In macrodactyly toe, accumulation of fat appears to be the most striking feature 3 and histopathological findings suggest that excessive proliferation of fatty tissue is the basis of cause for this abnormality whereas macrodactyly of the hand involves hypertrophied and tortuous digital nerves 4.
Macrodactyly occurs more often in hands than the feet. One or more fingers or toes may be involved. Macrodactyly can occur on one side only, or may affect both hands or both feet. Often macrodactyly is equated with its most common cause, macrodystrophia lipomatosa 5. Rarely macrodactyly can be seen as a form of Proteus syndrome 6.
Macrodactyly can be divided into two types – static and progressive macrodactyly.
- Static macrodactyly is present at birth and the digit appears to have increased in size and grows at the same pace as unaffected fingers or toes.
- Progressive macrodactyly is characterized by disproportionate growth – the affected fingers or toes grow at a much faster rate than unaffected digits 2. The affected fingers or toes can become enormous and severely impact a child’s ability to perform normal activities.
In some cases, a child’s macrodactyly-affected limb may appear to have a static growth pattern during infancy, but then can rapidly progress when the child is about 2 years old. In these cases, the affected fingers or toes grow very quickly, and often involve abnormally growth in the adjacent palm or forefoot. Macrodactyly foot tends to be of the progressive type. Most reported cases indicate a slight male preponderance 7 and the condition can occur unilaterally, bilaterally, symmetrically, or asymmetrically 8.
Children with macrodactyly may also have other musculoskeletal differences. One study showed that macrodactyly may be associated with syndactyly (two or more digits are fused together or webbed or conjoined fingers or toes) of the adjacent digit in as much as 10% of cases reported 8.
A number of conditions may manifest with asymmetric limb hypertrophy, including:
- Neural fibrolipoma (some term any macrodactyly with a neural fibrolipoma as macrodystrophia lipomatosa) 9
- Angiomatosis
- Neurofibromatosis type 1
Though macrodactyly is a benign condition, it does cause deformities, appear cosmetically different, and may affect your child’s normal hand or foot function.
Treatment for macrodactyly is on a case by case basis but generally includes surgery and the major aim is the reconstruction of a pain-free functioning foot 10. The growth of affected digit in children may be retarded by destroying, stapling, or wiring the epiphyseal plate 11. The accepted treatment for foot macrodactyly is reduction of the fibro-fatty bulk via dissection and ablation combined with removal of as much fat as possible 12. De-fatting occurs in a two step procedure where the first stepinvolves only the convex side of the digit and reducing its thickness by 10% to 20% while taking care to preserve its vascularity. The second procedure involves de-fatting the remaining side and performing a phalangectomy – shortening of the bone and resectioning and suturing of the excess skin. However there are new one-step procedures which greatly reduce compromising vascularity. Amputationis also an option, though it is reserved as a last option in most cases 10. Complications with surgery include delayed wound healing and inadequate initial de-fatting could cause subsequent re-growth of the fibro-fatty tissue and may require a second and more proximal amputation 12.
Figure 1. Macrodactyly finger
Figure 2. Macrodactyly toe
Macrodactyly causes
The cause of macrodactyly remains unknown. Researchers believe the condition is not inherited, but may instead be linked to disruptions in prenatal development. Streeter 13 hypothesizes that the condition might be a “consequence of germ plasm abnormality or pathology; by accident during cell cleavage or organogenisis, certain areas become supersensitive to growth stimulus.” During fetal development, some disturbance of growth limiting factor occurs in areas affected and because of this lack of inhibitor the part affected continues to increase in size and accounts for progressive overgrowth in later years. Barsky 2 also states that the “condition might be caused by interaction of genetic and environmental factors and may be the result of interaction of two or more extrinsic agents each incapable of producing teratological effects by themselves.”
Enlargements may also be due to hemangiomas where soft tissues, skin and x-rays do not show any increased size of the digits affected 2. Some propose that the development of neuorfibromatomas in the periosteal nerves due to bony destruction and regeneration may be the cause of rapid localized overgrowth 12.
Macrodactyly can occur in conjunction with other conditions and syndromes, including neurofibromatosis, lipofibromatous hamartoma, vascular conditions, and tuberous sclerosis complex.
The fatty tissues in foot macrodactyly found in children resemble adult subcutaneous fat – dark lobules fixed by many fine vessels which traverse the tissue – rather than the fat of the normal child’s age 7. Most of the abnormal bulk is due to excessive fibrofatty tissues and is abundant on the sides and plantar aspects of the toe. The fibro-fatty tissue extends from the toe in the forefoot and causes the bulk to expand laterally. The skin is markedly thickened and the digits involved have a soft and rubbery consistency 12. The bone age, as denoted by epiphyseal centers in the phalanges of affected digits, is increased when compared to unaffected bone 14. There is also an increased length and breadth of phalanges 12 with proliferation of fibroblastic tissue between the cortex and periosteum and accounted for cortical thickening and gigantism of phalanges in affected digits 14.
As previously stated, macrodactyly may be related to several neurogenic disorders. Abnormalities of peripheral nerves are uncommon in the pedal form though there are nerves more prominent with much proliferation of epineural and perineural tissues 12.
Macrodactyly signs and symptoms
The main symptom of macrodactyly is the appearance of one or more abnormally large fingers or toes. The larger digits may grow at the same rate as other non-affected fingers/toes, or have much faster growth. Macrodactyly may also result in reduced function owing to the secondary degenerative joint disorders and may cause compressions of adjacent nerves and vessels as well as disfigurement 4.
Other symptoms of macrodactyly may include:
- Abnormal growth in the affected hand or foot
- Stiffness
- Difficulty moving, grasping, or using the affected hand/foot
- Swelling
- Pain (though this is rare).
Macrodactyly diagnosis
Most children are born with obvious signs of macrodactyly. Occasionally, this condition presents a bit later, when the child is a year or two old. Diagnosing macrodactyly typically begins with a physical examination of your child’s affected hand or foot. A referral to the genetics team is sometimes necessary.
In most cases, clinicians will recommend an X-ray to confirm the diagnosis. X-rays produce images of bones and help doctors identify the underlying structure of the hand or foot.
In addition to a physical exam and X-rays, your child may also undergo:
- Magnetic resonance imaging (MRI), which uses a combination of large magnets, radiofrequencies and a computer to produce detailed images of organs, soft tissues, muscles, ligaments and other structures within the body. This test can help determine which underlying tissue is enlarged. Your child is exposed to no radiation during an MRI.
- Range of motion tests to determine if the condition is affecting movement and dexterity
Nerve assessment tests to determine if the condition has damaged or compressed any nerves
Accurate diagnosis helps your doctor determine the best course of treatment for your child.
Macrodactyly treatment
Treatment for macrodactyly will depend on the severity of your child’s condition, as well as the age and development of your child. Your child’s physician will discuss specific treatment options with you, and treatment depends on whether the condition occurs in the hand or the foot. Most of the time, however, surgery is required to correct macrodactyly. Your child’s doctor will discuss whether staged surgical treatment could benefit your child.
Your doctor’s goal will be to give your child optimal function of the affected area.
A hand can still be quite functional with a finger or two larger than the rest. Even a slightly enlarged toe may make wearing shoes impossible.
In mild cases, treatment for macrodactyly may involve observation or, in the case of an enlarged foot, shoe modification alone.
Nonsurgical interventions
If the growth of your child’s affected fingers or toes is static — meaning it is not getting worse — and is not interfering with their mobility, clinicians may recommend ongoing observation to ensure the condition doesn’t worsen.
Macrodactyly surgery
Because macrodactyly often produces an obvious deformity and can progressively worsen, many families seek more active treatment. For the bulk of children with macrodactyly, this includes surgery. Surgery for macrodactyly is complex because it involves multiple layers of tissue. It may take several surgical procedures to achieve the goals of halting the abnormal growth and creating a close-to-normal looking hand or foot.
Size-altering surgery will involve extensive observation and planning, because doctors will want to plot the rate of growth of your child’s normal digits versus the enlarged digits.
Surgery can involve debulking extra skin and subcutaneous tissue to narrow the width of the affected digits.
Epiphysiodesis could also be required when the hand bones reach adult length. In this procedure, the growth plates of individual hand bones are closed in order to prevent continued increase in length. In the most severe progressive cases, partial hand amputation may be required if all other means to control the growth of the finger(s) have been exhausted.
Your child’s doctor may recommend some combination of the following surgical procedures:
- Soft tissue debulking: To help correct width, this procedure involves the surgical removal of the thickened layers of skin and fat and the replacement of skin with skin grafts harvested from healthy skin in a nearby area. This procedure is usually performed in several stages around three months apart. It’s more often used to treat the milder forms of macrodactyly or as a part of the treatment of the more progressive forms.
- Shortening procedures: To help correct length, shortening procedures usually involve either surgical removal of one of the phalanges of the finger or toe, or removal of a metacarpal (hand bone) or metatarsal (foot bone).
- Ray resection: Surgical removal of the entire digit or digits is sometimes necessary, particularly when the condition is progressive. It is also an option if there is excessive widening of the forefoot, where the digital shortening and debulking procedures may not be effective.
After surgery, your child’s affected hand or foot will be immobilized with a cast or splint.
Surgery can dramatically improve the long-term outcomes for your child with macrodactyly, but it can also be a stressful experience for you and your child.
Follow-up care
Follow-up care for macrodactyly will depend on the treatment needed. If your child received nonsurgical treatment, they should be monitored regularly to ensure the condition does not begin to significantly affect their daily activities.
If your child needs surgery, they will be examined a few times in the first 2 to 3 months after surgery, and then every 6 to 12 months to monitor function and continued growth.
Additional operations will be performed as needed. Your child’s doctor will give you specific information about a recovery program for your child and how soon they can return to daily activities.
Macrodactyly prognosis
The long-term outlook for a child treated for macrodactyly varies from child to child, depending on how severe his problem is. You and your child can expect an overall improvement in appearance and function. In most cases, surgery can control hand growth, improve hand function, and help children better manage their daily activities. However, it’s rare that a child’s affected digits look and move perfectly.
References- P. P. Kotwal et.al, Macrodactyly, J Bone Joint Surg [Br] 1998;80-B:651-3.
- Barsky AJ. Macrodactyly. JBJS 1967 49A: 1255-1266.
- Fengdong Z, Rongrong Z, Peihua S, Shunwu F. Macrodactyly of the great toe for thirty-five years. J Plas Recon Aes Surg 2009 62: e520-e522.
- Yuksel A, Yagmur H, Kural BS. Prenatal diagnosis of isolated macrodactyly. Ultrasound Obstet Gynecol 2009 33: 360-362.
- Ellise Natividad and Kinna Patel. A Literature Review of Pedal Macrodactyly. The Foot and Ankle Online Journal 3 (5): 2 http://faoj.org/wp-content/uploads/2010/04/literature-review-of-macrodactyly.pdf
- Rosalind B et.al, The Proteus Syndrome: CNS Manifestations, AJNR 19:987–990, May 1998
- Syed A, Sherwani R, Quamar A, Haque F, Akhter K. Congenital macrodactyly: A clinical study. Acta Orthop Belg 2005 71: 399-404.
- Kotwall PP, Farooque M. Macrodactyly. JBJS 1998; 80B: 651-653.
- Mark D. Murphey et.al, From the Archives of the AFIP, Imaging of Musculoskeletal Neurogenic Tumors: Radiologic-Pathologic Correlation, September 1999 RadioGraphics, 19, 1253-1280.
- Uemura T, Kazuki K, Okada M, Egi T, Takaoka K. A case of toe macrodactyly treated by application of vascularized nail graft. Br J Plast Surg 2005 58: 1020-1024.
- Tsuge K. Treatment of macrodactyly. Plast Reconstr Surg 1967 39: 590-599.
- Dennyson WG, Bear JN, Bhoola KD. Macrodactyly in the foot. JBJS 1977 59B: 355-359.
- Streeter GL. Focal deficiencies in fetal tissues and their relations to intrauterine amputation. Contrib. Embryol. 1930 22: 1-44.
- Ben-Bassat M, Casper J, Kaplan I, Laron Z. Congenital Macrodactyly. JBJS 48A: 359-364.