Masseter muscle
Masseter muscle is a powerful muscle of chewing (mastication) that elevates the mandible (lower jawbone). Masseter muscle is located laterally to the mandibular ramus, and thus plays an important role in facial esthetics. Masseter muscle is a powerful superficial quadrangular muscle originating from the zygomatic arch and inserts along the angle and lateral surface of the mandibular ramus. The masseter is primarily responsible for the elevation of the mandible and some protraction of the mandible. Masseter muscle receives its motor innervation from the mandibular division of the trigeminal nerve (V3). The blood supply is primarily from the masseteric artery, a branch of the internal maxillary artery.
The masseter muscle is one of the muscles of mastication. It is a powerful superficial quadrangular muscle with two divisions: superficial and deep. The superficial portion of the masseter muscle originates from a thick aponeurosis on the temporal process of the zygomatic bone and the anterior two-thirds of the inferior border of the zygomatic arch. The fibers of the superficial portion pass inferior-posteriorly over the deep portion and insert onto the angle of the mandible (masseteric tubercle) and the inferior portion of the lateral surface of the mandibular ramus. The superficial masseter muscle has a quadrangular shape appearance on gross examination due to its origins and insertions. The deep portion of the masseter muscle originates from the entire surface of the zygomatic arch. The fibers run inferiorly and insert along the mandibular ramus superior to the masseter muscle’s superior portion. Anteriorly, the deep portion is covered by the superior portion of the masseter, while posteriorly, the parotid gland covers the deep portion.
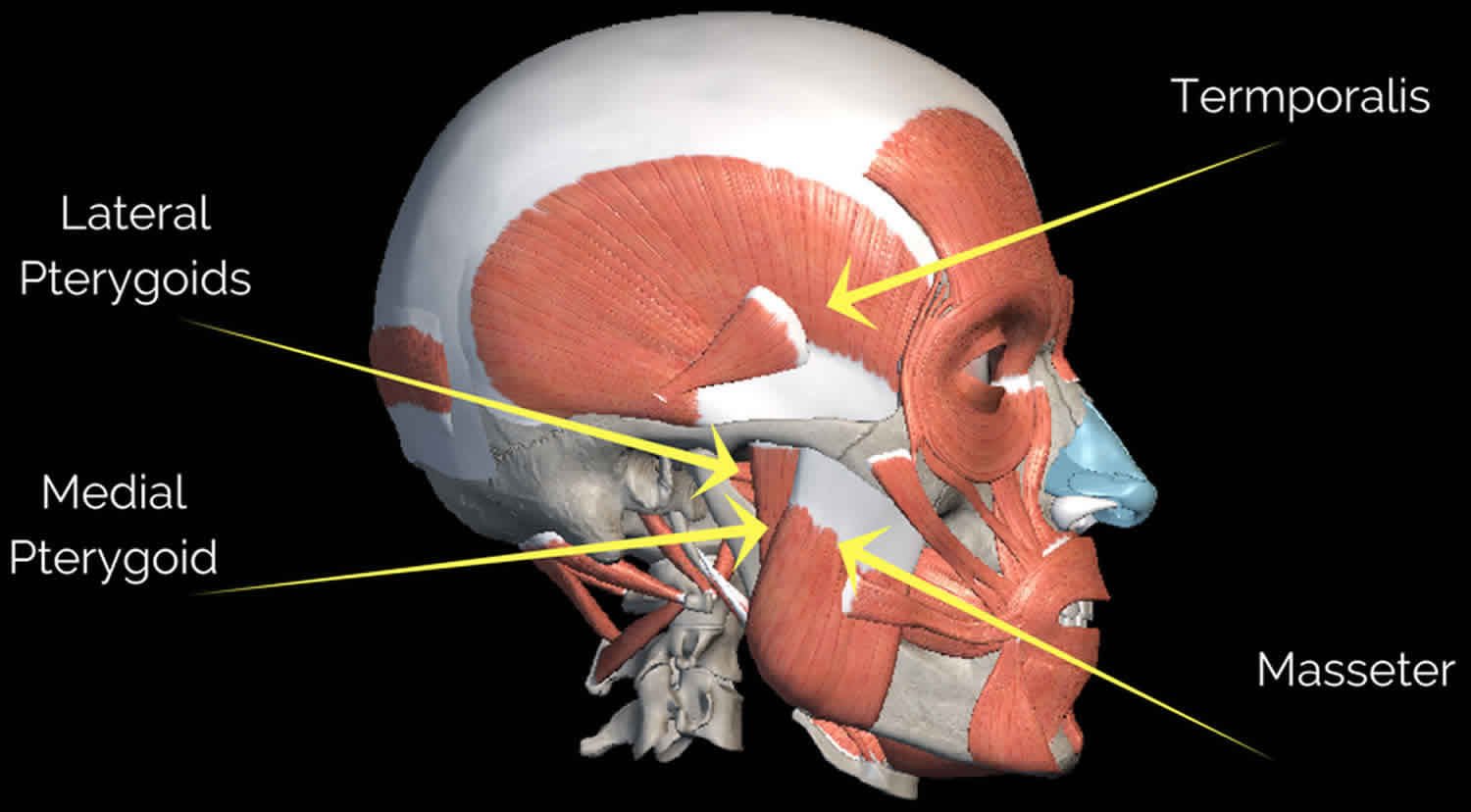
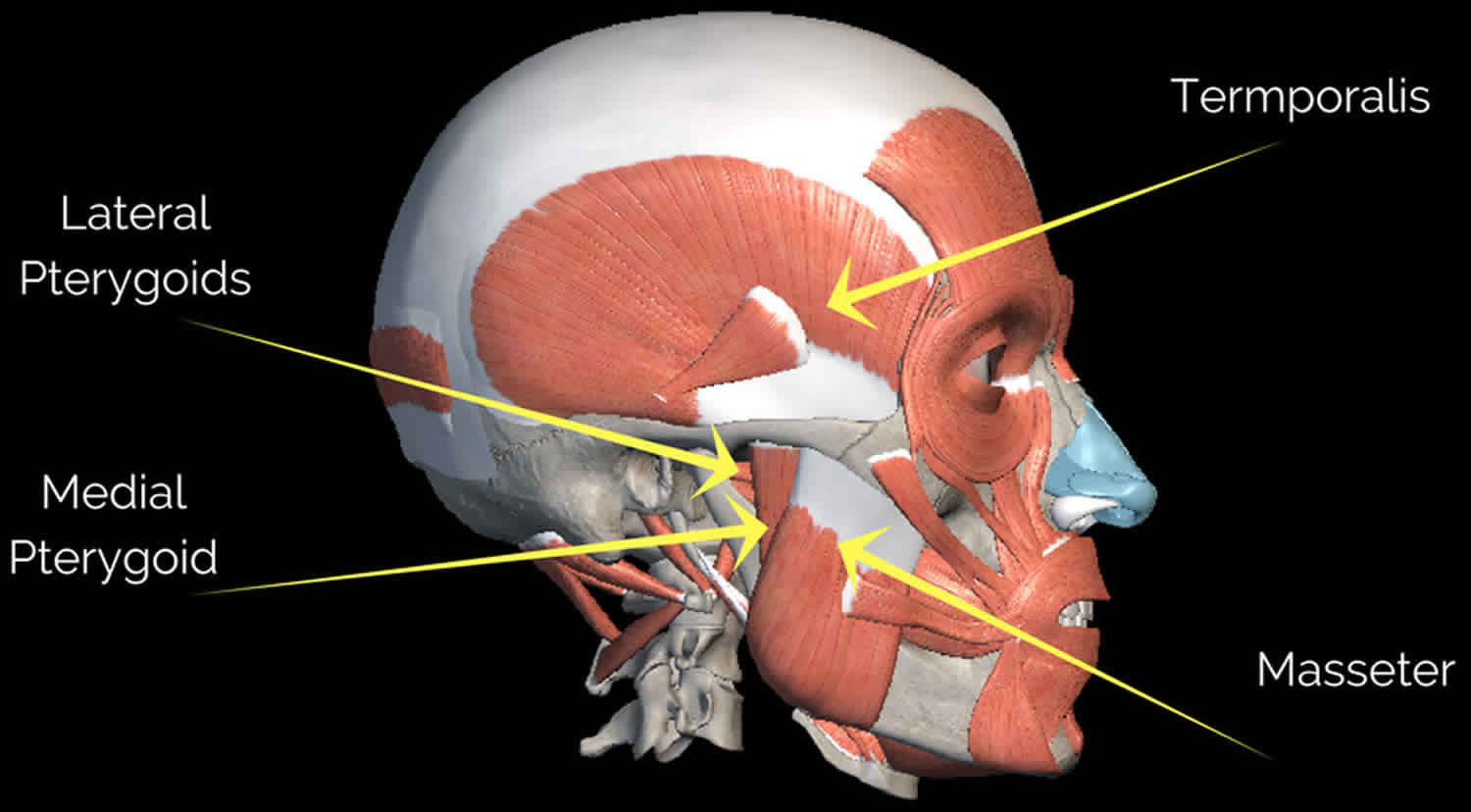
Figure 1. Masseter muscle
Masseter origin and insertion
Masseter origin
- Zygomatic arch and maxillary process of the zygomatic bone
Masseter insertion
- Angle and the lateral surface of ramus of mandible
Masseter function
The Masseter muscle elevates of mandible as in closing the mouth. Its insertion along the angle and lateral surface of the ramus also allows it to aid in the protrusion of the mandible allowing for the anterior motion of the jaw. The masseter muscle is one of the four muscles responsible for the action of mastication (chewing). The Masseter muscle together with other muscles of mastication move the mandible at the at the temporomandibular joint (TMJ). Of the four pairs of muscles involved in mastication, three are powerful closers of the jaw and account for the strength of the bite: masseter, temporalis, and medial pterygoid. Of these, the masseter is the strongest muscle of mastication. The medial and lateral pterygoid muscles assist in mastication by moving the mandible from side to side to help grind food. Additionally, the lateral pterygoid muscles protract (protrude) the mandible.
Masseter hypertrophy
Idiopathic hypertrophy of the masseter muscle is a rare disorder of unknown cause. Some authors associate it with defective teeth, habit of chewing gum, temporo-mandibular joint disorder, congenital and functional hypertrophies, and emotional disorders (stress and nervousness) 1. Idiopathic masseter muscle hypertrophy was first described by Legg in 1880, reporting on the case of a 10-year-old girl with concurrent idiopathic temporalis muscle hypertrophy 2. Anatomically, most of the masseteric thickness is along the inferior portion of the mandibular ramus, where the facial contour normally tapers. With masseter hypertrophy, the patient’s face takes on a characteristic rectangular configuration 3. A hypertrophied masseter will alter facial lines, generating discomfort and negative cosmetic impacts for many patients 4.
Benign masseter hypertrophy is a relatively uncommon condition that can occur unilaterally or bilaterally 2. Unilateral- or bilateral masseter hypertrophy is characterized by an increase in the volume of the muscle mass. This condition is benign, asymptomatic, and must be differentiated from parotid gland illnesses, odontogenic problems, and rare tumors of muscular tissue. The reasons why patients request a medical consultation are predominantly related to aesthetics, especially if the hypertrophy is unilateral due to a noticeable asymmetry of the lower third of the face 5.
Masseter muscle hypertrophy diagnosis can be produced from clinical examination, directed interview, panoramic x-ray, and muscle palpation 2. This last diagnostic test consists of palpating the muscle with the fingers while the patient clenches his/her teeth so that the muscle is more prominent during contraction. With the muscle relaxed and the patient’s mouth slightly open, extra-oral palpation using both hands will pinpoint the intramuscular location of the hypertrophy. In this case during physical examination the enlargement of masseter muscle was detected and the antro -posterior x-ray shows bone growth at the angle of mandible on the affected side. According to Seltzer and Wang 6, CT and MRI scans produce excellent images for the diagnosis of various masseter muscle conditions. In our case, the diagnosis was made by palpating the fiber of masseter muscle at the insertion especially at the angle of mandible during clenching. Antro -posterior x-ray view of the patent shows bone growth at the angle of the mandible 4.
The bone spurs at the mandible angle are commonly associated findings and they can be observed in the anteroposterior radiograph. However, Bloem and Hoof 7 stated that approximately 20% of normal people have this finding and that it cannot be considered as diagnostic aid. Guggenheim and Cohen 8 reported that bone spurs are caused by periostal irritation and new bone deposition responding to increased forces exerted by the muscles bundles. Idiopathic masseter muscle hypertrophy must be accurately diagnosed, as it may be mistaken for other diseases. Among them are unilateral compensatory hypertrophy (due to hypotrophy or hypoplasia in the contralateral side), masseter tumor, salivary gland disease, parotid tumor, parotid inflammatory disease, and masseter muscle intrinsic myopathy 4.
Therapy for masseter muscle hypertrophy is usually unnecessary, non-surgical modality of treatment include reassurance tranquilizer or muscle relaxant, psychiatric care and injection of very small dose of botulin toxin type A 9.
Excision of the internal layer of the masseter muscle and reduction of the thickened bone in the region of the mandibular angle via intraoral approach is the treatment of choice. Complication from surgical incision of master includes Hematoma, facial nerve paralysis, infection, trismus and sequelae from general anesthesia 10.
Injection of botulinum toxin type A (botox) in to the masseter muscle is also another alternative as a treatment. Botulinum toxin type A injection is reported to be safe and effective treatment modality in orofacial dystonies, sialorrhea, Frey’s syndrome, muscle hypertrophies, etc. Botulinum toxin type A, a power full neurotoxin, is produced by the anaerobic organism Clostridium botulinum .When injected in to muscle it causes interference with the neurotransmitter mechanism producing selective paralysis and subsequent atrophy of muscle 11.
Masseter muscle botox
Botox or botulinum toxin injection into the masseter muscle is ideal for patients who are grinding, clenching, and wearing out their teeth (bruxism) and need a lot of dental work, for patients who have frequent tension or migraine headaches, and for patients who do not like the shape of their face because of square or thick jaw line and who want to appear more feminine.
The amount of Botox needed to treat this area ranges between 60 and 100 units of Botox, depending on the thickness of the muscle. Patients can expect headaches and clenching to go away within a week and will see the full effects of jaw thinning about one month after treatment, when the muscle has had time to atrophy.
Side effect may include some bruising, which is a potential side effect whenever you inject into the face. There’s no swelling, no downtime. Patients can go back to their normal activities. They can exercise. They can do whatever they want that day. Most people come in during their lunch break, they get injected. You can’t even see the pinprick of the needle.
Patients should be counseled to return to the office for treatment every six months, which is longer than the typical two-month interval for injecting Botox in other areas. Under-dosing the muscle in efforts to get by with a smaller dose or because a patient wants to spend less money will definitely lead to the patient coming back sooner for follow-up treatment, and s/he won’t see the ideal effect for headaches.
When injecting into the masseter, it’s important to feel where the masseter muscle starts and ends. The masseter muscle is like a quadrangle, so doctors actually go into each vertex of the quadrangle and test it for the masseter. It’s also essential to know where the risorious muscle is, which holds the corner of the mouth out when you smile. It’s important to not hit the risorious muscle or that side will not move, resulting in a crooked smile.
For optimal results, be sure to use a high enough dose—if you under-dose, treatment will not be effective. It’s not like other injection areas where you can say, “OK, we’ll just inject 10 units and see what it looks like.” It doesn’t work the same way—you have to use a higher dose to ensure optimal results.
References- Kebede B, Megersa S. Idiopathic masseter muscle hypertrophy. Ethiop J Health Sci. 2011;21(3):209–212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3275871/
- Kebede B, Megersa S. Idiopathic masseter muscle hypertrophy. Ethiop J Health Sci. 2011;21(3):209–212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3275871
- Yu C-C, et al. Botulinum Toxin A for Lower Facial Contouring: A Prospective Study. Aesth Plast Surg. 2007;31:445–451
- Daniel Z R, Paulo MC, José L, Pires JR, Vinicius RF, Mandelli Karina K, Marcela AC. Benign masseter muscle hypertrophy. Rev Bras Otorrinolaringol. 2008;74(5):790–793
- Rispoli DZ, Camargo PM, Pires JL, Fonseca VR, Mandelli KK, Pereira MA. Benign masseter muscle hypertrophy. Braz J Otorhinolaryngol. 2008;74(5):790–793
- Modern imaging of the masseter muscle: normal anatomy and pathosis on CT and MRI. Oral Surg Oral Med Oral Pathol. 1987 May;63(5):622-9. https://www.ncbi.nlm.nih.gov/pubmed/3473385
- [Hypertrophy of the masseter muscle]. Ned Tijdschr Tandheelkd. 1972 Aug-Sep;79(8):308-15. https://www.ncbi.nlm.nih.gov/pubmed/4506860
- Eduardo KS, Marcelo G, Marcelo PC. Masseter Muscle Hypertrophy – Case Report. Braz Dent J. 2006;17(4):347–350
- Al-Ahmad HT, Al-Qudah MA. The treatment of masseter hypertrophy with botulinum toxin type A. Saudi Med J. 2006;27:397–400
- Ham JW. Masseter muscle reduction procedure with radiofrequency Coagulation. J Oral Maxillofac Surg. 2009;67:457–463
- Al-Muharraqi MA, Fedorowicz Z, Al Bareeq J, Al Bareeq R, Nasser M. Botulinum toxin for masseter hypertrophy. Cochrane Database Syst Rev. 2009;1:CD007510