What is melasma
Melasma is also known as chloasma or pigmentation of pregnancy, is a common cause of symmetrical, blotchy, brownish facial darkening (hyperpigmentation) in approximately 70% of women, especially those of dark complexion. Melasma can lead to considerable embarrassment and distress. Melasma is related to hormonal changes with increased facial pigmentation occurs during the second half of pregnancy (the mask of pregnancy) and can be worsened by oral contraceptives. Melasma generally starts between the age of 20 and 40 years, but it can begin in childhood or not until middle age.
Melasma is a common disorder of unknown cause that causes dark brown (hyperpigmented) patches, primarily on sun exposed areas of the face. Melasma is marked by brown patches that worsen in response to increases of the hormone estrogen, such as during pregnancy or with the use of birth control pills. Other medications, such as anti-seizure medications, may also cause melasma. Increased sun exposure can also be a cause.
Melasma key facts
- Although melasma is more common in women, men can also have melasma. Only 1-in-4 to 1-in-20 affected individuals are male, depending on the population studied.
- People with darker skin are generally more likely to have melasma. Melasma is more common in people that tan well or have naturally brown skin (Fitzpatrick skin types 3 and 4) compared with those who have fair skin (skin types 1 and 2) or black skin (skin types 5 or 6).
- Family history increases likelihood of developing melasma.
- Melasma usually gets worse in summer.
- Melasma can fade on its own. This usually happens when a trigger, such as a pregnancy or birth control pills, causes the melasma. When a woman delivers her baby or stops taking the birth control pills, melasma can fade.
Table 1. Fitzpatrick skin type
| Skin type | Typical features | Tanning ability |
|---|---|---|
| I | White; very fair; red or blond hair; blue eyes; freckles | Always burns, never tans |
| II | White; fair; red or blond hair; blue, hazel, or green eyes | Usually burns, tans with difficulty |
| III | Cream white; fair with any eye or hair color; very common | Sometimes mild burn, gradually tans |
| IV | Brown; typically Mediterranean skin | Rarely burns, tans easily |
| V | Dark brown; Middle-Eastern skin types | Very rarely burns, tans darkly easily |
| VI | Black skin | Never burns, always tans darkly |
Some people, however, have melasma for years — or even a lifetime. If the melasma does not go away or a woman wants to keep taking birth control pills, melasma treatments are available. These include:
Hydroquinone: This medicine is a common first treatment for melasma. It is applied to the skin and works by lightening the skin. You will find hydroquinone in medicine that comes as a cream, lotion, gel, or liquid. You can get some of these without a prescription. These products contain less hydroquinone than a product that your dermatologist can prescribe.
Tretinoin and corticosteroids: To enhance skin lightening, your dermatologist may prescribe a second medicine. This medicine may be tretinoin or a corticosteroid. Sometimes a medicine contains 3 medicines (hydroquinone, tretinoin, and a corticosteroid) in 1 cream. This is often called a triple cream.
Other topical (applied to the skin) medicines: Your dermatologist may prescribe azelaic acid or kojic acid to help lighten melasma.
Procedures: If medicine you apply to your skin does not get rid of your melasma, a procedure may succeed. Procedures for melasma include a chemical peel, microdermabrasion, dermabrasion, laser treatment, or a light-based procedure. Only a dermatologist should perform these procedures.
New skin problems can occur when the person who gives the treatment does not tailor it to the patient’s skin type.
Ask your dermatologist about possible side effects (health problems that can result from the treatment).
If you notice any of the following after getting treatment for melasma, be sure to call your dermatologist:
- Skin irritation
- Darkening of the skin
- Other problems
Figure 1. Melasma on face
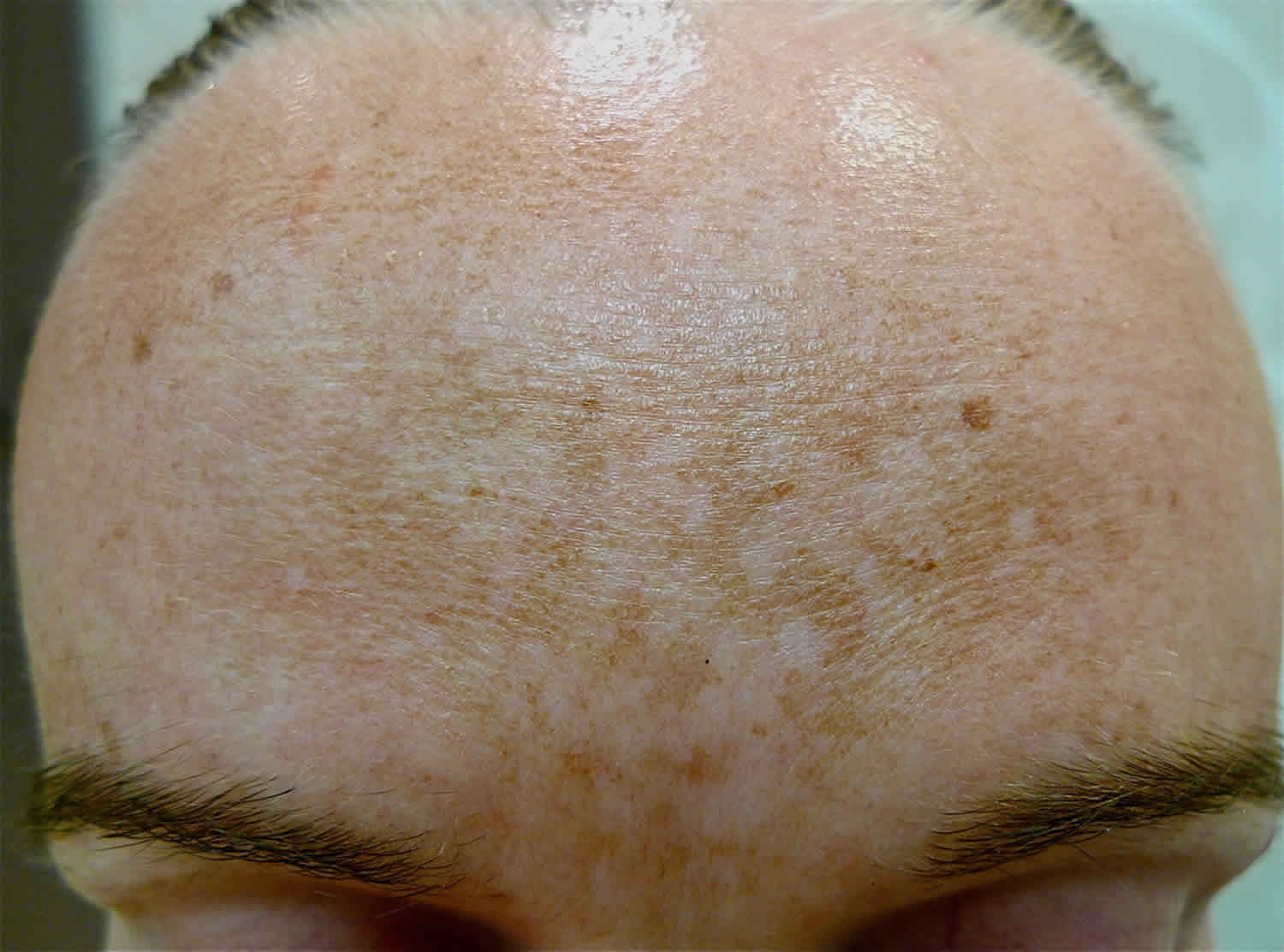
Figure 2. Melasma in men
Figure 3. Skin structure
Figure 4. Structure and skin cells of the Epidermis
What causes melasma
The cause of melasma is complex. The pigmentation is due to overproduction of melanin by the pigment cells, melanocytes, which is taken up by the keratinocytes (epidermal melanosis) and/or deposited in the dermis (dermal melanosis, melanophages) 2. There is a genetic predisposition to melasma, with at least one-third of patients reporting other family members to be affected. In most people melasma is a chronic disorder.
Known triggers for melasma include:
- Sun exposure and sun damage—this is the most important avoidable risk factor. Ultraviolet (UV) light from the sun stimulates the melanocytes. In fact, just a small amount of sun exposure can make melasma return after fading. Sun exposure is why melasma often is worse in summer. It also is the main reason why many people with melasma get it again and again.
- Pregnancy—in affected women, the pigment often fades a few months after delivery
- Hormone treatments—oral contraceptive pills containing estrogen and/or progesterone, hormone replacement, intrauterine devices and implants are a factor in about a quarter of affected women
- Certain medications (anti-seizure medications and the new targeted therapies for cancer), scented or deodorant soaps, toiletries and cosmetics—these may cause a phototoxic reaction that triggers melasma, which may then persist long term
- Hypothyroidism (low levels of circulating thyroid hormone)
- Skin care products: If a product irritates your skin, melasma can worsen.
Melasma commonly arises in healthy, non-pregnant adults. Lifelong sun exposure causes deposition of pigment within the dermis and this often persists longterm. Exposure to ultraviolet radiation (UVR) deepens the pigmentation because it activates the melanocytes to produce more melanin.
Research is attempting to pinpoint the roles of stem cell, neural, vascular and local hormonal factors in promoting melanocyte activation.
What are the clinical features of melasma?
Melasma presents as macules (freckle-like spots) and larger flat brown patches.These are found on both sides of the face and have an irregular border. There are several distinct patterns.
- Centrofacial pattern: forehead, cheeks, nose and upper lips
- Malar pattern: cheeks and nose
- Lateral cheek pattern
- Mandibular pattern: jawline
- Reddened or inflamed forms of melasma (also called erythrosis pigmentosa faciei)
- Poikiloderma of Civatte: reddened, photoaging changes seen on the sides of the neck, mostly affecting patients older than 50 years
- Brachial type of melasma affecting shoulders and upper arms (also called acquired brachial cutaneous dyschromatosis).
Melasma is sometimes separated into epidermal (skin surface), dermal (deeper) and mixed types. A Wood lamp that emits black light (UVA1) may be used to identify the depth of the pigment.
Epidermal melasma
- Well-defined border
- Dark brown colour
- Appears more obvious under black light
- Responds well to treatment
Dermal melasma
- Ill-defined border
- Light brown or bluish in colour
- Unchanged under black light
- Responds poorly to treatment
Mixed melasma
- The most common type
- Combination of bluish, light and dark brown patches
- Mixed pattern seen under black light
- Partial improvement with treatment
Figure 5. Melasma epidermal
Melasma signs and symptoms
Common signs (what you see) of melasma are brown or gray-brown patches on the face. These patches most commonly appear on the:
- Cheeks.
- Forehead.
- Bridge of the nose.
- Above the upper lip.
- Chin.
Some people get patches on their forearms or neck. This is less common.
Melasma does not cause any symptoms (what people feel). But many people dislike the way melasma makes their skin look. If you dislike these patches, sun protection and treatment can help.
Melasma diagnosis
The characteristic appearance of melasma means diagnosis is usually straightforward and made clinically. Other disorders that may be considered instead of melasma or as well as melasma include:
- Postinflammatory pigmentation
- Solar lentigines and other forms of lentigo
- Drug-induced pigmentation, e.g. due to minocycline or nonsteroidal antiinflammatory drugs
- Lichen planus
- Naevus of Ota and naevus of Hori
- Guttate hypomelanosis, in which pale spots are prominent
Occasionally, skin biopsy may be performed to make or confirm the diagnosis of melasma. Histology varies with the type of melasma. But some degree of each of the following features is usually found.
- Melanin deposited in basal and suprabasal keratinocytes
- Highly dendritic (branched) deeply pigmented melanocytes
- Melanin in the dermis within melanophages
- Solar elastosis and elastic fibre fragmentation
The extent and severity of melasma can be described using the Melasma Area and Severity Index (MASI).
How to get rid of melasma
Melasma can be very slow to respond to treatment, especially if it has been present for a long time. Treatment may result in irritant contact dermatitis in patients with sensitive skin, and this can result in post-inflammatory pigmentation.
Generally a combination of the following measures is helpful.
General measures
- Discontinue hormonal contraception.
- Year-round life-long sun protection. Wear a broad-brimmed hat.
- Use broad-spectrum very high protection factor (SPF 50+) sunscreen applied to the whole face daily, year-round. It should be reapplied every 2 hours if outdoors during the summer months. Sunscreens containing iron oxides are preferred, as they screen out some visible light as well as ultraviolet radiation.
- Alternatively or as well, use a make-up that contains sunscreen.
- Use a mild cleanser, and if the skin is dry, a light moisturizer.
- Cosmetic camouflage (make-up) is invaluable to disguise the pigment.
Topical therapy
Tyrosinase inhibitors are the mainstay of treatment. The aim is to prevent new pigment formation by inhibiting formation of melanin by the melanocytes.
- Hydroquinone 2–4% as cream or lotion, applied accurately to pigmented areas at night for 2–4 months. This may cause contact dermatitis (stinging and redness) in 25% of patients. It should not be used in higher concentration or for prolonged courses as it has been associated with ochronosis (a bluish grey discoloration similar to that seen in alkaptonuria).
- Azelaic acid cream, lotion or gel can be applied twice daily long term, and is safe in pregnancy. This may also sting.
- Kojic acid or kojic acid dipalmitate is often included in formulations, as it binds copper, required by L-DOPA (a cofactor of tyrosinase). Kojic acid can cause irritant contact dermatitis and less commonly, allergic contact dermatitis.
- The mechanism of action of cysteamine cream is unclear, but is thought to involve inhibition of tyrosinase. A study of 50 patients with melasma found cysteamine cream to be significantly more effective than placebo cream.
- Ascorbic acid (vitamin C) also acts through copper to inhibit pigment production. It is well tolerated but highly unstable, so is usually combined with other agents.
- Methimazole (antithyroid drug) cream has been reported to reduce melanin synthesis and pigmentation in hydroquinone-resistant melasma.
- New agents under investigation include zinc sulfate mequinol, arbutin and deoxyarbutin (from berries), licorice extract, rucinol, resveratrol, 4-hydroxy-anisole, 2,5-dimethyl-4-hydroxy-3(2H)-furanone and/or N-acetyl glucosamine
Other active compounds used for melasma include:
- Topical corticosteroids such as hydrocortisone. These work quickly to fade the color and reduce the likelihood of contact dermatitis caused by other agents. Potent topical steroids are best avoided due to their potential to cause adverse effects.
- Soybean extract, which is thought to reduce the transfer of pigment from melanocytes to skin cells (keratinocytes) and to inhibit receptors.
- Tranexamic acid has been used experimentally for melasma as a cream or injected into the skin (mesotherapy), showing some benefit. It may cause allergy or irritation.
Superficial or epidermal pigment can be peeled off. Peeling can also allow tyrosinase inhibitors to penetrate more effectively. These must be done carefully as peels may also induce post-inflammatory pigmentation.
- Topical alpha hydroxyacids including glycolic acid and lactic acid, as creams or as repeated superficial chemical peels, remove the surface skin and their low pH inhibits the activity of tyrosinase.
- Topical retinoids, such as tretinoin (a prescription medicine) are effective. Tretinoin can be hard to tolerate and sometimes causes contact dermatitis. Do not use during pregnancy.
- Salicylic acid, a common peeling ingredient in skin creams, can also be used for chemical peels, but it is not very effective in melasma.
The most successful formulation has been a combination of hydroquinone, tretinoin, and moderate potency topical steroid. This has been found to result in improvement or clearance in up to 60–80% of those treated. Many other combinations of topical agents are in common use, as they are more effective than any one alone. However, these products are often expensive.
Oral treatment of melasma
Oral medications for melasma are under investigation, including tranexamic acid. Tranexamic acid is a lysine analogue that inhibits plasmin and is usually used orally to stop bleeding. It reduces production of prostaglandins, the precursors of tyrosine. In low dose, tranexamic acid has been reported to be effective and safe in the treatment of melasma, providing patients have been carefully selected and are at low risk of thromboembolic disease.
Glutathione is also under investigation as a systemic skin whitening agent, but has potentially serious adverse effects.
Melasma laser treatment
The ideal treatment for melasma would destroy the pigment, while leaving the cells alone. Unfortunately, this is hard to achieve. Machines can be used to remove epidermal pigmentation but with caution—over-treatment may cause postinflammatory pigmentation. Patients should be pretreated with a tyrosinase inhibitor (see above).
Fractional lasers, Q-switched Nd:YAG lasers and intense pulsed light (IPL) appear to be the most suitable options. Several treatments may be necessary and post-inflammatory hyperpigmentation may complicate recovery.
Carbon dioxide or erbium:YAG resurfacing lasers, pigment lasers (Q-switched ruby and Alexandrite devices) and mechanical dermabrasion and microdermabrasion should be used with caution in the treatment of melasma.
What is the outcome of treatment of melasma?
Under a dermatologist’s care, many people with melasma have a good outcome. Melasma can be stubborn, though. Results take time and the above measures are rarely completely successful. It may take a few months of treatment to see improvement. It is important to follow your dermatologist’s advice. This ensures that you get the most benefit from treatment. It also can help avoid skin irritation and other side effects.
After your melasma clears, you may need to keep treating your skin. Your dermatologist may call this maintenance therapy. Maintenance therapy can prevent melasma from returning.
You can help prevent your melasma from returning by wearing sunscreen (broad-spectrum SPF 50+ sunscreen) and a wide-brimmed hat every day.
Unfortunately, even in those that get a good result from treatment, pigmentation may reappear on exposure to summer sun and/or because of hormonal factors. New topical and oral agents are being studied and offer hope for effective treatments in the future.
Home remedies for melasma
Melasma is a common skin problem that causes brown to gray-brown patches on the face. Although the exact causes of melasma are unclear, common triggers include sun exposure, pregnancy, birth control pills, and cosmetics.
If you have melasma, dermatologists recommend the following tips for achieving a more even skin tone:
- Wear sunscreen daily: One of the most common treatments for melasma is sun protection. Since sunlight triggers melasma, it is important to wear sunscreen every day, even on cloudy days and after swimming or sweating. Choose a sunscreen that offers broad-spectrum protection, a Sun Protection Factor (SPF) of 30 or more, and zinc oxide and/or titanium dioxide to physically limit the effects of the sun’s rays on your skin. Apply sunscreen 15 minutes before going outside and reapply at least every two hours.
- Wear a wide-brimmed hat and sunglasses when you’re outside: As a recent study in the journal Nature illustrates, sunscreen alone may not give you the sun protection you need. Whenever possible, seek shade and wear protective clothing in addition to applying sunscreen.
- Choose gentle skin care products: Choose skin care products that don’t sting or burn, as products that irritate the skin may worsen melasma.
- Avoid waxing: Waxing may cause skin inflammation which can worsen melasma, so it’s important to avoid waxing areas of the body affected by the condition. Ask a dermatologist about other types of hair removal that may be right for you.
If your melasma does not go away, see a board-certified dermatologist to discuss available treatments for melasma, such as prescription medications or in-office procedures.
References- Del Bino S, Duval C, Bernerd F. Clinical and Biological Characterization of Skin Pigmentation Diversity and Its Consequences on UV Impact. Int J Mol Sci. 2018;19(9):2668. Published 2018 Sep 8. doi:10.3390/ijms19092668 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6163216/
- Melasma. https://www.dermnetnz.org/topics/melasma/