What is nail biting disorder
Nail biting also called onychophagia, is one of the most common childhood and young adults habits 1. Some studies estimate that 45–60% of children chew on their nails! And, occasionally, a child may also bite his or her toenails. However, there are very few epidemiological data analyzing the frequency of nail biting (onychophagia) in the population, and most data are limited to children and adolescents. It is estimated that 28–33% of children between 7 and 10 years of age and approximately 45% of teenagers are nail-biters 2. By the age of 18 years the frequency of this behaviour decreases, although it may persist in some adults 3. The prevalence of nail biting among people in the age range 60–69 years is believed to be between 4.5% and 10.7% 4. In most cases nail biting seems to be only a cosmetic problem. However, if uncontrolled, it can cause serious morbidity. The most common complications are severe damage to the cuticle and nail plate, leading to shortening of nails, chronic paronychia (inflammation of the fingers or toes) and secondary bacterial infections, self-inflicted gingival injuries, and dental problems 5. Temporomandibular joint pain and dysfunction and osteomyelitis (bone infection) have also been reported as a consequence of chronic nail biting 6. In addition, nail biting may lead to psychological problems in some patients (e.g. significant distress). Nail biting is often embarrassing and socially undesirable.
Boys and girls appear equally prone to the nail biting habit in earlier years; however, as they get older, boys are more likely to be nail biters. By the age of 18 years the frequency of nail biting (onychophagia) behavior decreases, but it may persist in some adults 7.
A habit is a pattern of behavior that’s repeated, and the child doing it usually isn’t even aware of it. But while kids may be blissfully unaware of a habit, their parents aren’t so lucky.
Many children have habits that can be downright annoying. Four of the most common are:
- nail biting
- hair twirling
- nose picking
- thumb sucking
Although these habits may bother or even worry you, relax. In most cases, a habit is just a phase in the normal developmental process and is not cause for alarm.
However, most habits don’t cause any significant problems and tend to improve as kids get older. But if you’re concerned about your child’s habits, talk with your doctor.
Nail biting, like most habits, often disappears on its own as children outgrow the urge to do it. In the meantime, avoid threatening or punishing your child — these tactics tend to backfire. Instead, tell your child why you don’t like the behavior and offer him/her rewards for self-control.
You can also try having you child wiggle their fingers for 30 seconds before he/she bites his/her nails — it may become too tedious of an activity for your child to continue. Your child may bite her nails when she’s under stress, so try to see if there’s a pattern to her biting or if something is bothering her.
Although unsanitary, chronic nail biting (onychophagia) isn’t likely to cause long-term nail damage.
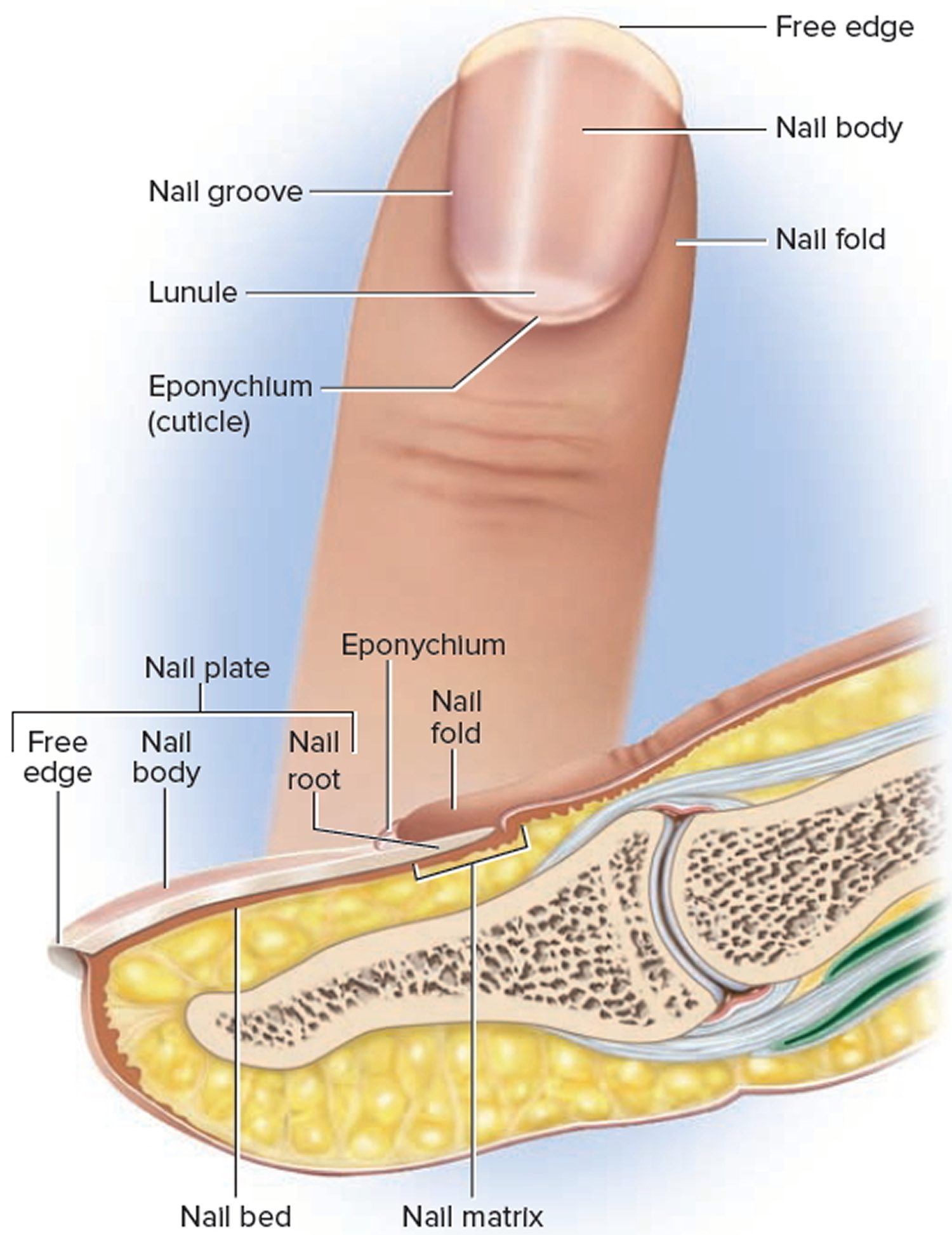
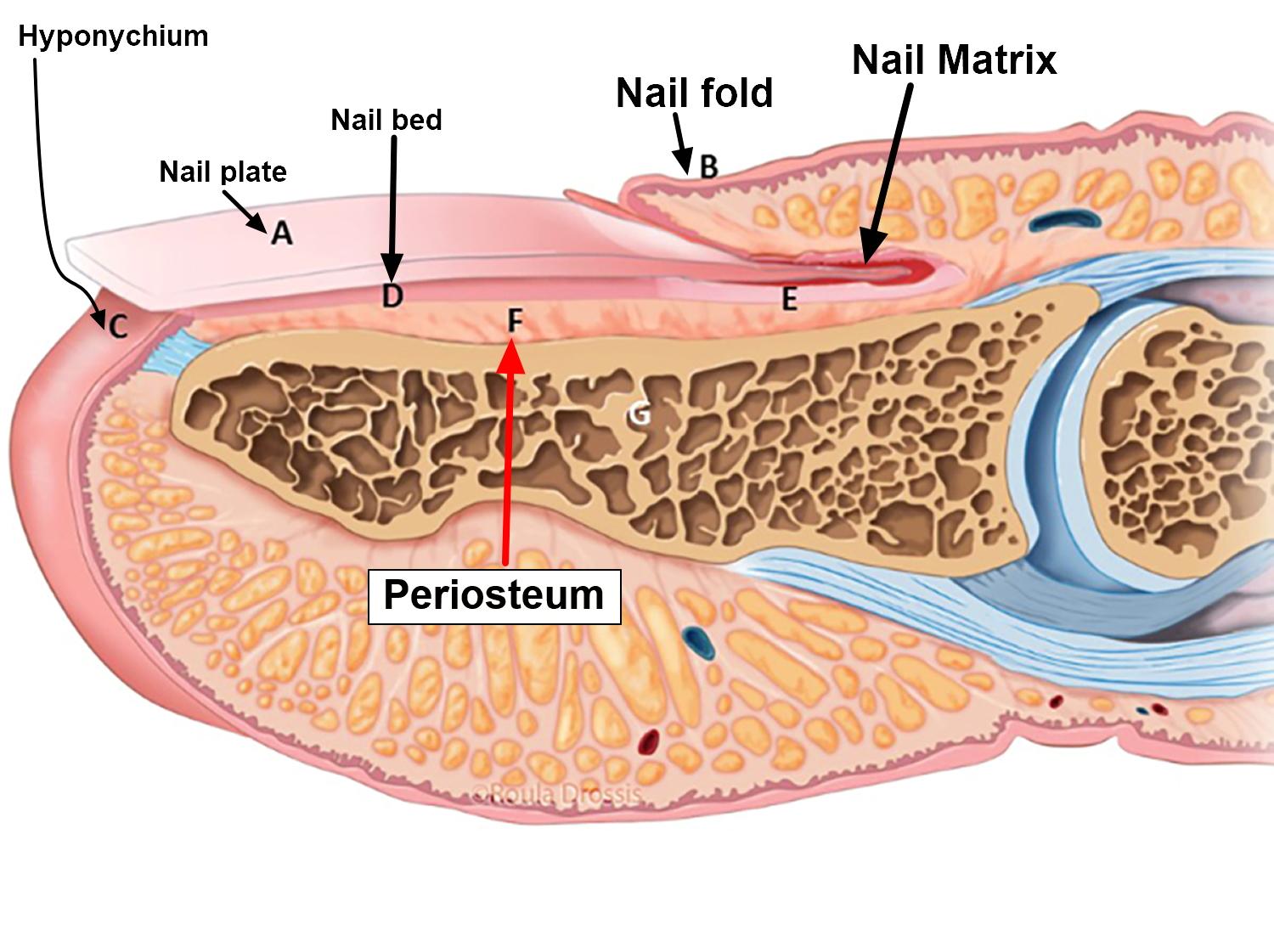
Nails are formed within the nail bed — just beneath where the U-shaped cuticles begin. As long as the nail bed remains intact, nail biting isn’t likely to interfere with fingernail growth. In fact, some research suggests that nail biting might even promote faster nail growth.
Nail biting isn’t without risks, however. For example, nail biting can:
- Damage the skin around the nail, increasing the risk of infection
- Increase the risk of colds and other infections by spreading germs from your fingers to your mouth
- Harm your teeth
Figure 1. Fingernail
Nail biting causes
Experts aren’t always sure what causes a habit, but do know that they’re learned behaviors that usually provide a positive outcome for the child.
Habits may develop as entertainment for a bored child or, more commonly, as a coping mechanism to soothe an anxious one. The next time you see nail biting or hair twirling, try to recall if your child has recently had a stressful experience. If so, the behavior might be your child’s attempt to relieve tension, much as you would by working out at the gym. On the other hand, some children engage in habits when they’re relaxed, such as before falling to sleep or quietly listening to music.
Some habits may be leftovers from infancy. In infants, thumb sucking is a common self-comfort behavior that has pleasurable associations with feedings and the end of hunger. So it may linger into childhood because of its positive associations.
Or perhaps the explanation for your child’s nail biting is in your mirror. Do you bite your nails? Studies suggest that nail biting may have a strong familial or genetic component.
Other children engage in habits to attract attention or to manipulate their parents. If kids feel that their parents are ignoring them, they may engage in the annoying habit because they know that it will get a reaction from Mom or Dad.
There are a lot of controversies about the causes of nail biting. While some studies related nail biting to behavioral problems 8 and anxiety 9, others did not believe so 10. Anxiety in children with nail biting is not a trait; it is a state 11. The trait which is accompanied with nail biting is oral aggression 11. Oral habits including nail biting have an environmental etiology, and are risk factors for malocclusion development, especially in children older than preschool years 12. Inadequate motor activity is supposed to be a cause of an increase in nail biting 13.
Although, it was suggested that nail biting might reduce anxiety or tension 14, recent studies do not support the anxiety theory for nail biting 13. Nail biting usually occurs as a result of boredom or working on difficult problems rather than anxiety. Nail biter do not bite their nail when they are engaged in social interactions, or when they are reprimanded for the behavior.24 It is suspected that smoking and gum chewing in adults are substitutes for nail biting in childhood 15. Severe and mild nail biting appear to have some differences in terms of the basis of physical and social consequences, severity, frequency, and physiological mechanisms 16.
According to some studies 6, nail biting (as well as hair pulling or skin picking) may be caused by over-stimulation (due to stress or excitement) or under-stimulation (due to boredom or inactivity). Nail biting (onychophagia) can be treated as a kind of a compulsion that may cause destruction of the nails. This disorder seems to be related to obsessive-compulsive spectrum disorder. Obsessive-compulsive spectrum disorder overlaps with obsessive-compulsive disorder (OCD) in terms of clinical symptoms, associated features (age of onset, clinical course and comorbidity) and response to specific psychopharmacological and behavioral treatment 17. Obsessive-compulsive disorder (OCD) is a type of anxiety disorder. If you have obsessive-compulsive disorder (OCD), you have frequent, upsetting thoughts called obsessions. To try to control the thoughts, you feel an overwhelming urge to repeat certain rituals or behaviors. These are called compulsions. Obsessive-compulsive spectrum disorders are characterized by obsessive thoughts or preoccupations with body appearance (body dysmorphic disorder), body weight (anorexia nervosa) or body illnesses (hypochondriasis), or by stereotyped ritualistic behaviours, such as tics (Tourette’s syndrome), hair pulling (trichotillomania), sexual compulsions and pathological gambling. Besides nail biting (onychophagia), obsessive-compulsive tendencies may manifest in dermatology as onychotillomania, trichotillomania, skin picking, and acne excoriée 3. Recently these problems have been termed body focused repetitive behaviors 6. It has been suggested that nail biting is related to high anxiety and low self-esteem 18. Patients with nail biting (onychophagia) have been scored higher on obsessive-compulsiveness, especially those who regarded their nail biting as a serious problem 18. Grant and Christenson 19 found that comorbid psychiatric disorders are frequent in trichotillomania (hair pulling) and chronic skin picking, but they did not focus on nail biting (onychophagia). Therefore, further studies are needed to assess co-occurring anxiety and obsessive-compulsive disorder (OCD) among patients with chronic nail biting (onychophagia). It would also be interesting to investigate whether nail biting in childhood could predispose to obsessive-compulsive disorder (OCD) or other psychiatric disorders in adulthood. Because of the lack of systematic surveys evaluating this problem, case reports are very helpful in clinical practice to better understand the nature of nail biting (onychophagia) and choose the proper treatment strategy.
Nail biting treatment
The good news is that most habits disappear, usually by the time a child reaches school age, because the child no longer needs it or outgrows it.
But if you think it’s time to help your child break a habit, consider these steps:
- Calmly point out what you don’t like about the behavior and why. This approach can be used with kids as young as 3 or 4 to help increase awareness of the problem. Say something like, “I don’t like it when you bite your nails. It doesn’t look nice. Could you try to stop doing that?” Most important, the next time you see the nail biting, don’t scold or lecture. Punishment, ridicule, or criticism could cause the behavior to increase.
- Involve your child in the process of breaking the habit. If your 5-year-old comes home crying from kindergarten because the other kids made fun of his thumb sucking, understand that this is a way of asking you for help. Parents can ask their kids what they think they could do to stop the habit or if they want to stop the habit. Come up with some ways to work on breaking the unwanted habit together.
- Suggest alternative behaviors. For example, when if your child is a nail-biter, instead of saying, “Don’t bite your nails,” try saying, “Let’s wiggle our fingers.” This will increase awareness of the habit and may serve as a reminder. To occupy your child’s attention, try providing a distraction, like helping you in the kitchen or working on a craft.
- Reward and praise self-control. For example, allow your little girl to use nail polish if she lets her nails grow. Or every time your son refrains from sucking his thumb, reinforce the positive behavior by praising him and giving him a sticker or other small prize.
- Be consistent in rewarding good behavior. If you fail to notice good behavior, it will disappear over time. The new, positive habit must be firmly established before the old one will disappear.
For the best success, it’s important that kids be motivated to break the habit. And because habits take time to develop, they’re also going to take time to be replaced by alternative behavior, so be patient.
How to stop biting your nails
To help you stop biting your nails, experts recommend the following tips:
- Keep your nails trimmed short: Having less nail provides less to bite and is less tempting.
- Apply bitter-tasting nail polish to your nails: Available over-the-counter, this safe, but awful-tasting formula discourages many people from biting their nails.
- Get regular manicures: Spending money to keep your nails looking attractive may make you less likely to bite them. Alternatively, you can also cover your nails with tape or stickers or wear gloves to prevent biting.
- Replace the nail-biting habit with a good habit: When you feel like biting your nails, try playing with a stress ball or silly putty instead. This will help keep your hands busy and away from your mouth.
- Identify your triggers: These could be physical triggers, such as the presence of hangnails, or other triggers, such as boredom, stress, or anxiety. By figuring out what causes you to bite your nails, you can figure out how to avoid these situations and develop a plan to stop. Just knowing when you’re inclined to bite may help solve the problem.
- Try to gradually stop biting your nails: Some doctors recommend taking a gradual approach to break the habit. Try to stop biting one set of nails, such as your thumb nails, first. When that’s successful, eliminate your pinky nails, pointer nails, or even an entire hand. The goal is to get to the point where you no longer bite any of your nails.
For some people, nail biting may be a sign of a more serious psychological or emotional problem. If you’ve repeatedly tried to quit and the problem persists, consult a doctor or a psychologist. If you bite your nails and develop a skin or nail infection, consult a doctor or board-certified dermatologist.
How to stop nail biting in adults
In adults nail biting disorder seems to be related to obsessive-compulsive spectrum disorder 7. Psychiatric evaluation of co-occurring psychopathological symptoms in patients with nail biting (onychophagia), especially those with chronic, severe or complicated nail biting, may be helpful in making a choice of individual therapy. Serotonin re-uptake inhibitors (SRIs) seem to be the treatment of choice in severe onychophagia 7. In addition, serotonin re-uptake inhibitors (SRIs) were documented to be effective in other psychodermatoses, such as trichotillomania or body dysmorphic disorder 20. It has been suggested that pharmacotherapy is effective in approximately 60–70% of patients with nail biting (onychophagia) 7. On the other hand, behavioral therapy, including self-monitoring and habit reversal also resulted in a short-term reduction in nail biting behavior 21.
If you’re concerned about nail biting, consult your doctor or a mental health provider. To stop nail biting, he or she might suggest:
- Avoiding factors that trigger nail biting, such as overstimulation
- Taking healthy steps, such as getting active, to manage stress and anxiety
- Keeping your nails neatly trimmed or manicured
- Occupying your hands or mouth with alternate activities, such as playing a musical instrument or chewing gum
- Apply a bitter tasting lacquer to nails to discourage biting
In some cases, treatment with behavior therapy might be needed.
Psychotherapy
Psychotherapy — particularly cognitive behavioral therapy (CBT) — can be an effective treatment. Cognitive behavioral therapy (CBT) helps you learn skills to manage nail biting disorder and find different ways to manage your worries other than excessive nail biting.
The Royal College of Psychiatrists defines cognitive behavioral therapy as a way of talking about:
- How you think about yourself, the world and other people
- How what you do affects your thoughts and feelings.
They say that cognitive behavioral therapy (CBT) can help you to change how you think (the cognitive part) and what you do (the behavioral part). These changes can help you to feel better. Unlike some of the other talking treatments, it focuses on the “here and now” difficulties. Instead of focusing on the causes of your distress or symptoms in the past, it looks for ways to improve your state of mind now.
Other therapies such as behavioral stress management and exposure therapy also may be helpful.
Cognitive behavioral therapy (CBT) can help you:
- Identify your fears and beliefs about having a serious medical disease
- Learn alternate ways to view your body sensations by working to change unhelpful thoughts
- Become more aware of how your worries affect you and your behavior
- Change the way you respond to your body sensations and symptoms
- Learn skills to cope with and tolerate anxiety and stress
- Reduce avoidance of situations and activities due to physical sensations
- Reduce behaviors of frequently checking your body for signs of illness and repeatedly seeking reassurance
- Improve daily functioning at home, at work, in relationships and in social situations
- Address other mental health disorders, such as depression
If you are not sure you want to commit to a long course of sessions with a clinical psychologist, there are various resources on the Internet which will provide an introduction to CBT or even a course of computer-aided CBT sessions:
- Developed by the Australian National University, MoodGYM (https://moodgym.com.au/) is a fun, free interactive web program that teaches the principles of CBT using flashed diagrams and online exercises. MoodGYM (https://moodgym.com.au/) demonstrates the relationship between thoughts and emotions, and works through dealing with stress and relationship break-ups, as well as teaching relaxation and meditation techniques. It consists of five modules (why you feel the way you do, changing the way you think, changing ‘warped’ thoughts, knowing what makes you upset, assertiveness and interpersonal skills training), an interactive game, anxiety and depression assessments, downloadable relaxation audio, a workbook and feedback assessment. Scientific trials have shown that using two or more modules is linked to significant reductions in depression and anxiety symptoms. These benefits last after 12 months. MoodGYM has won several IT and health awards, and has over 1,000,000 users worldwide. MoodGYM (https://moodgym.com.au/)
- Living Life to the Full (https://llttf.com/) is a free online life skills course for people feeling distressed. It aims to provide easy access to CBT skills in a way that cuts through jargon. It helps you understand why you feel as you do, and to learn new ways of improving how you feel, by making changes in your thinking, activities, sleep and relationships. The course is based on the idea of helping you to help yourself. It is supported by a series of CBT self-help workbooks that can be used between the e-learning sessions. These encourage you to put what you are learning into practice, and to stop, think and reflect on what you are learning. Living Life to the Full (https://llttf.com/)
- FearFighter (http://www.fearfighter.com/) delivers CBT over the internet, useful for those who may be concerned about the stigma associated with seeing a therapist. Taking only three months to complete, with minimal telephone support, FearFighter helps you improve even if you have virtually no computer skills. You are encouraged to use FearFighter as often as you wish but for at least once a week. It helps you identify specific problems, work on realistic treatment goals, and monitor achievement of those goals by repeated self-exposure. You get scheduled brief helpline support to a total of one hour over 10 weeks. FearFighter helps you to work out exactly what brings on your fear, so you can learn how to face it until it subsides. This is called exposure therapy. It consists of nine steps that need to be worked through one by one to obtain the greatest benefits. Like a therapist, FearFighter asks you to return every week to report on how you’ve been doing. You can ask it to print out questionnaires and graphs of your progress. It guides you through CBT as much as a therapist does.
- Step 1: Welcome to FearFighter – Introduces the system, asks you to rate your problem on the Fear Questionnaire (FQ) and Work & Social Adjustment Scale (WSA), and asks about suicidal feelings and alcohol misuse.
- Step 2: How to Beat Fear – Explains the principles of CBT, with case examples. You are asked to keep a daily record of your triggers.
- Step 3: Problem Sorting – Helps you identify your triggers, shows you scenarios relevant to your problem, and helps you personalise your triggers and rate them on a 0-8 scale.
- Step 4: How to Get a Helper – Explains the value of recruiting a CBT co-therapist and gives hints on how to find one.
- Step 5: Setting Goals – Guides you through the process of setting good goals and tests them. You record and rate these on the system and can print personalised homework diaries.
- Step 6: Managing anxiety – Offers a menu of coping strategies for use during CBT homework.
- Step 7: Rehearsing Goals – Guides you on how to practise personal coping strategies during both imagined and live CBT homework.
- Step 8: Carrying On – Reviews progress with the help of graphs, allows new goals to be devised, and offers feedback and advice.
- Step 9: Troubleshooting – Offers a menu of tips on overcoming common sticking points in treatment.
You may have found that when you avoid things that make you panic or feel uncomfortable, the situation tends to get worse and worse. FearFighter can teach you how to face your fear until you adapt and no longer want to run away from it. It helps you learn to face the things that make you panic, such that, with time, you’ll find that, one by one, they’ll get easier.
Self-exposure therapy guided by computer is as effective as clinician-guided therapy and both are superior to relaxation to improve phobia/panic. FearFighter has been tested in four clinical trials and is as effective as the best CBT therapists.
Approved by the National Institute of Clinical Excellence (NICE), free access can only be prescribed by your doctor in England and Wales. FearFighter (http://www.fearfighter.com/)
References- Fıçıcıoğlu S, Korkmaz S. Onychophagia Induced Melanonychia, Splinter Hemorrhages, Leukonychia, and Pterygium Inversum Unguis Concurrently. Case Reports in Dermatological Medicine. 2018;2018:3230582. doi:10.1155/2018/3230582. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5831699/
- Leung AK, Robson WL. Nailbiting. Clin Pediatr (Phila) 1990; 29: 690–692.
- Gregory LH. Stereotypic movement disorder and disorder of infancy, childhood, or adolescence NOS. in: Kaplan HI, Sadock BJ, editors. Comprehensive textbook of psychiatry. 6th edition. Baltimore: Williams & Wilkins; 1995: p. 2360–2362.
- Heaton KW, Mountford RA. Nail-biting in the population and its relationship to irritable bowel syndrome. J R Soc Med 1992; 85: 457.
- Lee DY. Chronic nail biting and irreversible shortening of the fingernails. J Eur Acad Dermatol Venereol 2009; 23: 185.
- Williams TI, Rose R, Chisholm S. What is the function of nail biting: an analog assessment study. Behav Res Ther 2006; 45: 989–995.
- Onychophagia as a Spectrum of Obsessive-compulsive Disorder. Acta Derm Venereol 2009; 89: 278–280. https://www.medicaljournals.se/acta/content/html/10.2340/00015555-0646
- Ghanizadeh A. ADHD, bruxism and psychiatric disorders: does bruxism increase the chance of a comorbid psychiatric disorder in children with ADHD and their parents? Sleep Breath. 2008;12:375–80
- Joubert CE. Relationship of self-esteem, manifest anxiety, and obsessive-compulsiveness to personal habits. Psychol Rep. 1993;73:579–583.
- Teng EJ, Woods DW, Marcks BA, Twohig MP. Body-focused repetitive behaviors: The proximal and distal effects of affective variables on behavioral expression. Journal of Psychopathology and Behavioral Assessment. 2004;26:55–64.
- Gilleard E, Eskin M, Savasir B. Nailbiting and oral aggression in a Turkish student population. Br J Med Psychol. 1988;61:197–201.
- Winocur E, Littner D, Adams I, Gavish A. Oral habits and their association with signs and symptoms of temporomandibular disorders in adolescents: a gender comparison. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:482–7
- Dufrene BA, Steuart WatsonT, Kazmerski JS. Functional analysis and treatment of nail biting. Behav Modif. 2008;32:913–27.
- Klatte KM, Deardorff PA. Nail-biting and manifest anxiety of adults. Psychol Rep. 1981;48:82.
- Tanaka OM, Vitral RW, Tanaka GY, et al. Nailbiting, or onychophagia: a special habit. Am J Orthod Dentofacial Orthop. 2008 Aug;134:305–8.
- Wells JH, Haines J, Williams CL, Brain KL. The self-mutilative nature of severe onychophagia: a comparison with self-cutting. Can J Psychiatry. 1999;44:40–7.
- Hollander E, Benzaquen SD. The obsessive-compulsive spectrum disorder. In: Boer JA, Westenberg HG, editors. Focus on obsessive-compulsive spectrum disorders. Amsterdam: Syn-Thesis Publishers; 1997, p. 33–36.
- Joubert CE. Relationship of self-esteem, manifest anxiety, and obsessive-compulsiveness to personal habits. Psychol Rep 1993; 73: 579–583.
- Grant JE, Christenson GA. Examination of gender in pathologic grooming behaviors. Psychiatr Q 2007; 78: 259–267
- Bloch MH, Landeros-Weisenberger A, Dombrowski P, Kelmendi B, Wegner R, Nudel J, et al. Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry 2007; 62: 839–846.
- Arnowitz B. Psychotherapies for compulsive self-injurious behavior. In: Hollander E, Simeon D, editors. Self-injurious behaviours: assessment and treatment. Washington DC, London: American Psychiatric Pub 2001; 97–112.