What is nail patella syndrome
Nail-patella syndrome is a rare genetic disorder that is usually apparent at birth or during early childhood. Nail-patella syndrome involves a classic clinical tetrad of changes in the nails, knees, and elbows, and the presence of iliac horns 1. The features of nail-patella syndrome vary in severity between affected individuals, even among members of the same family. Nail changes are the most constant feature of nail patella syndrome. The fingernails and toenails may be absent (aplasia), underdeveloped (hypoplastic) or dystrophic; ridged longitudinally or horizontally; pitted; discolored; separated into two halves by a longitudinal cleft or ridge of skin; and thin or (less often) thickened. The patellae (knee caps) may be small, irregularly shaped, or absent. Elbow abnormalities may include limitation of extension, pronation, and supination; cubitus valgus; and antecubital pterygia, caused by underdevelopment or dislocation of the radius (a forearm bone that is part of the elbow) and/or webbing of skin at the bend of the elbow(s). Abnormal projections of bone from the upper (superior) portion of both sides of the hipbone (bilateral iliac horns).
Approximately 30 -50% of individuals with nail patella syndrome may also develop abnormalities in kidney function (nephropathy) that may be apparent during childhood or later in life. Kidney involvement, first manifest as proteinuria with or without hematuria, occurs in 30%-50% of affected individuals; kidney failure may occur in about 5% of all nail patella syndrome patients.
In addition, some individuals within certain families with nail patella syndrome may have abnormally increased fluid pressure of the eyes (primary open-angle glaucoma) and ocular hypertension occur at increased frequency and at a younger age than in the general population. The condition results due to progressive blockage of the outflow of fluid (aqueous humor) from the front chamber of the eyes (open-angle glaucoma). Without appropriate treatment, the gradual increase in fluid pressure may cause increased narrowing of visual fields and eventual blindness. Another common eye (ocular) difference associated with nail patella syndrome is an abnormally dark (hyperpigmented) and “cloverleaf” shape discoloration around the inner margin (pupillary margin) of the colored portion of the eyes (irides). This is known as (Lester’s sign) and does not cause any problems with vision.
The prevalence of nail-patella syndrome is estimated to be 1 in 50,000 individuals 2.
Nail-patella syndrome is caused by genetic changes (pathogenic variants or mutations) in the LMX1B gene. Nail patella syndrome is inherited in an autosomal dominant manner 2. This means any individual with nail patella syndrome, regardless of gender, has a 50% chance of passing this condition on to each of his/her offspring.
Diagnosis is usually suspected when a person has symptoms of the nail-patella syndrome. The diagnosis can be confirmed by genetic testing.
After a diagnosis of nail-patella syndrome, a person may be recommended to undergo screening for health problems that are more common in people with the syndrome. This may include having regular blood pressure checks, urine tests to watch for the development of kidney problems, and examinations by a medical eye doctor (ophthalmologist) to check for signs of glaucoma.
Symptoms of nail-patella syndrome affecting the knee and elbow (orthopedic problems) may be treated with physical therapy, braces, splints, or surgeries. Before a person with nail-patella syndrome has surgery for orthopedic problems, an MRI is recommended to make sure the doctors understand the unique anatomy of the joint or body part. Other symptoms of the syndrome, such as glaucoma or high blood pressure (hypertension), can be treated with medications as the medical problem would in people who do not have the syndrome. In some cases, people with nail-patella syndrome may require a kidney transplant. It is recommended that people with the syndrome avoid non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, due to their increased risk of kidney problems. Other treatments depend on the symptoms present in each person.
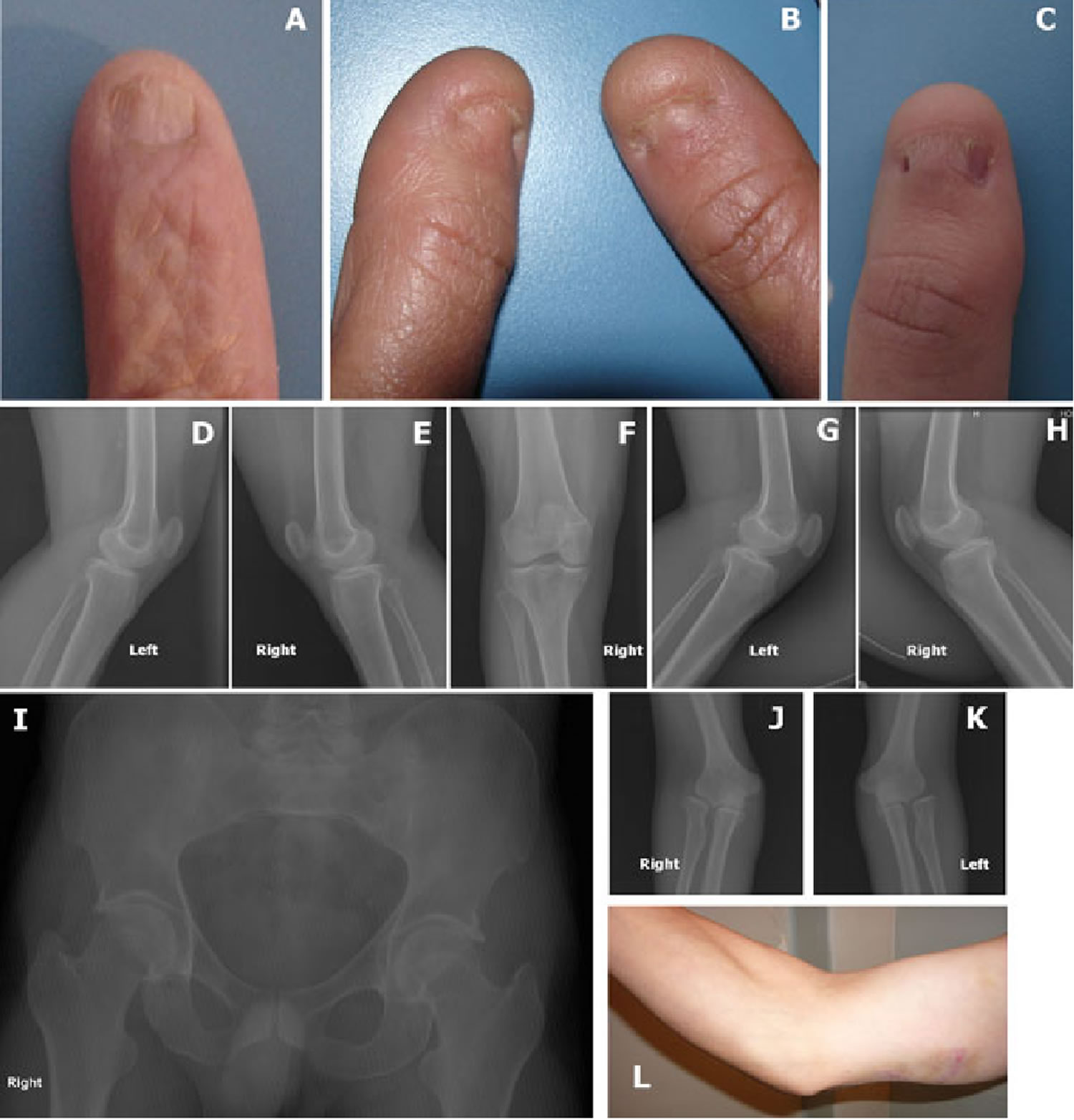
Figure 1. Nail-patella syndrome
Footnote: Photographs of the nails and radiographs of knees, hips and elbows of some of the subjects. Nail involvement in these cases includes dystrophic, thin, hypoplastic discolored nails with longitudinal ridges. Case III-2 shows decreased creases over the skin of distal interphalangeal joints, which is a sensitive sign of digital involvement in this patient (A). Thumbs are most severly affected in case III-7 (B), and IV-9 (C). The radiographs of knee involvement in Case III-2 shows bilateral involvement of the patella, with hypoplastic, higher than normal missplaced patella (D-F). A small 6 mm bone fragment can be observed on the lateral border of right patella (E). Knee radiographs of Case III-7 show slight bilateral patellar hypoplasia, mostly on the transverse diameter (G and H). Hip radiography of Case IV-2 shows loss of the normal concavity at the junction between the head and femoral neck bilaterally. The radiographs reveal an elbow involvement of subject IV-2 (J and K) and include a prominent medial epicondyle and hypoplasia of the capitellum on both sides (J and K). They also show a hypoplasia of the lateral epicondyle and capitellum with a slight deformity of the radial head (J and K). Underdeveloped triceps and prominent medial epicondyle are observed (L).
[Source 3 ]Nail patella syndrome causes
Nail-patella syndrome is caused by genetic changes (pathogenic variants or mutations) in the LMX1B gene in about 95% of people with the nail-patella syndrome. The LMX1B gene provides instructions for producing a protein that attaches (binds) to specific regions of DNA and regulates the activity of other genes. On the basis of this role, the LMX1B protein is called a transcription factor. The LMX1B protein appears to be particularly important during early embryonic development of the limbs, nails, kneecaps, elbows, kidneys, and eyes. Mutations in the LMX1B gene lead to the production of an abnormally short, nonfunctional protein or affect the protein’s ability to bind to DNA. It is unclear how mutations in the LMX1B gene lead to the signs and symptoms of nail-patella syndrome.
In rare cases, people who have symptoms of nail-patella syndrome do not have a pathogenic variant in the LMX1B gene. Therefore it is thought that there may be other genes in which pathogenic variants cause nail-patella syndrome.
Nail-patella syndrome inheritance pattern
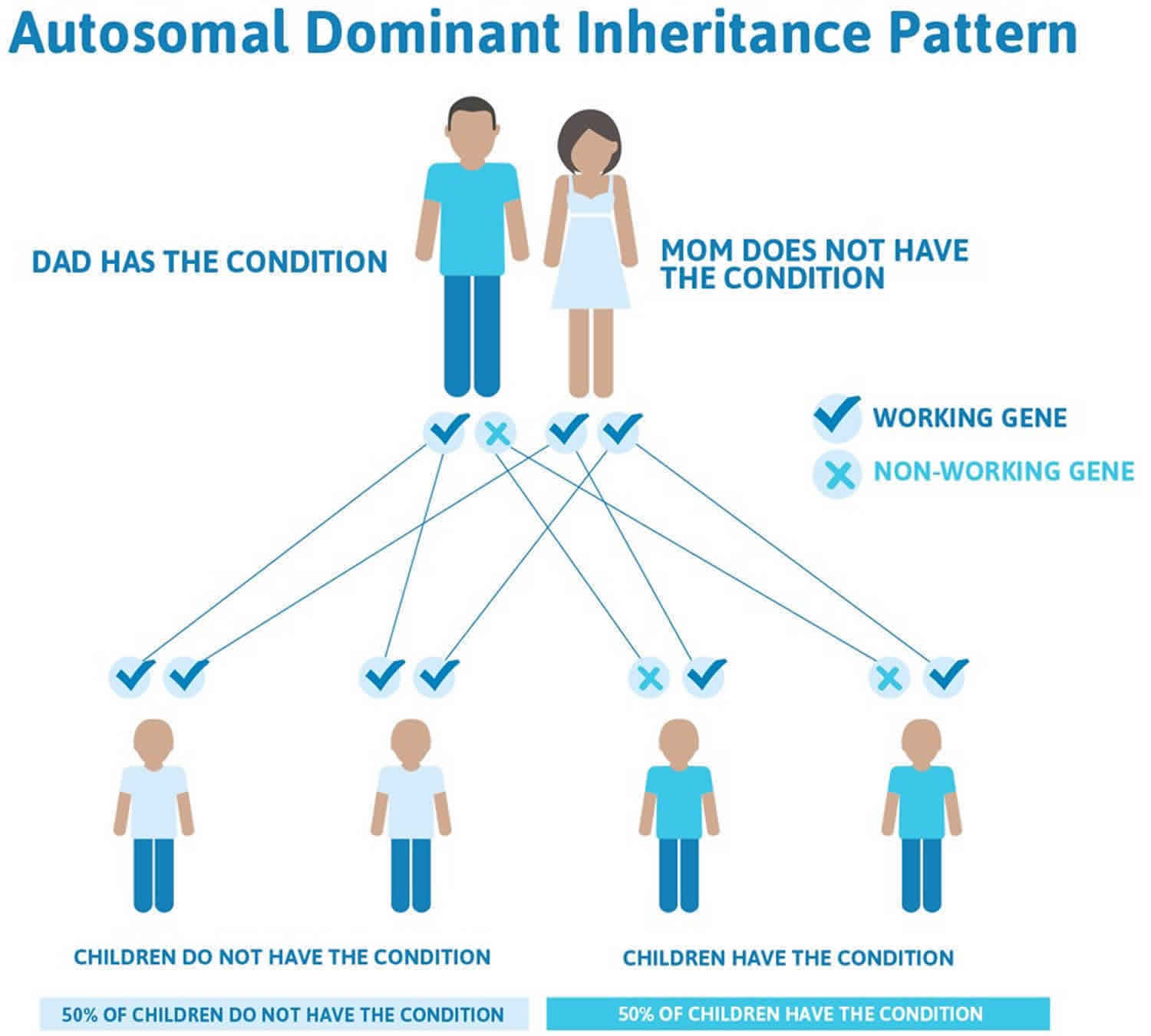
Nail-patella syndrome is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person inherits the mutation from one affected parent. Other cases may result from new mutations in the LMX1B gene. This is called a de novo mutation. These cases occur in people with no history of the disorder in their family.
In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
Figure 2 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 2. Nail-patella syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Nail patella syndrome symptoms
The symptoms of nail-patella syndrome most commonly affect the way the nails, kneecaps (patellae), elbows, and hip bone form. Almost all people with nail-patella syndrome have nails that are missing, underdeveloped, discolored, split, or ridged. The fingernails are more likely to be affected than the toenails. The thumbnails tend to be the most severely affected.
The first symptom that usually causes the patient to seek medical care is knee pain, instability, or an inability to completely extend the knee joint 4. Most people who have nail-patella syndrome have kneecaps that are small, absent, or irregularly shaped. This can cause problems such as frequent kneecap dislocation or early-onset arthritis. One kneecap may be affected more than the other. Most people with the nail-patella syndrome also have problems with one or both of their elbows because different parts of the elbow did not develop correctly. Some people are not able to fully extend their elbows or may have a hard time turning (rotating) the lower part of the arm when their arm is straight. The elbow may dislocate easily.
Changes in the pelvic bones called iliac horns can often be seen on x-ray and are found in 70% of people with nail-patella syndrome. Iliac horns are small pointy growths of bone (bony projections) that are not normally found on people’s hip bones. Although these changes do not cause any health problems, iliac horns, if present, can be used to diagnose nail-patella syndrome.
Other less common symptoms may include gastrointestinal problems such as constipation or irritable bowel syndrome. There may be nerve (neurological) problems affecting the hands and feet, such as reduced sensitivity to pain and temperature, numbness, tingling, or burning sensations. The hands and feet may be unusually cold, even in warm weather. Dental problems may include weak, crumbling teeth and thin dental enamel.
People with nail-patella syndrome are at a higher risk to develop increased pressure in the eye (glaucoma). About 30-50% of people with nail-patella syndrome have kidney disease. The most common feature of kidney disease is having high levels of protein in the urine (proteinuria). High blood pressure (hypertension) is also common in people with kidney disease. In about 5% of people with nail-patella syndrome, the kidney disease may progress to end-stage kidney disease.
The symptoms associated with nail-patella syndrome can vary widely, even among people in the same family. This concept is called variable expressivity.
Nail patella syndrome diagnosis
The diagnosis of nail-patella syndrome is based on clinical findings. LMX1B is the only gene in which pathogenic variants are known to cause nail patella syndrome. Molecular genetic testing for mutations in the LMX1B gene is available to confirm the diagnosis.
Nail patella syndrome may be suspected at birth or early childhood based upon the identification of certain characteristic findings (e.g., nail dysplasia, hypoplastic or absent patellae, antecubital pterygium, bilateral symmetrical iliac spurs/horns). However, in others, the disorder may not be suspected until later in life. Nail patella syndrome may be confirmed based upon a thorough clinical evaluation, identification of characteristic physical findings, a detailed patient and family history, advanced imaging techniques, and laboratory testing.
Specialized imaging techniques such as x-ray studies, computerized tomography (CT) scanning, and/or magnetic resonance imaging (MRI) may confirm the presence and/or extent of certain bone abnormalities characteristically associated with nail patella syndrome (e.g., patellae hypoplasia and/or aplasia, hypoplastic capitellum and head of radius, bilateral iliac spurs, etc.). During CT scanning, a computer and x-rays are used to create a film showing cross-sectional images of certain tissue structure. During MRI, a magnetic field and radio waves are used to create cross-sectional images.
Nail patella syndrome treatment
The treatment of nail patella syndrome is directed toward the specific symptoms that are apparent in each individual. Treatment may require the coordinated efforts of a team of specialists. Pediatricians, surgeons, physicians who diagnose and treat abnormalities of the bones (orthopedists), specialists who diagnose and treat disorders of the kidneys (nephrologists), eye specialists (ophthalmologists), physical therapists, dietitians, and/or other health care professionals may need to systematically and comprehensively plan an affected child’s treatment.
Specific therapies for the treatment of nail patella syndrome are symptomatic and supportive. In some cases, treatment for associated bone abnormalities may include surgical stabilization or replacement of knee caps with artificial devices (prosthetics) and/or correction and/or reconstruction of hypoplastic bones within the knee and/or elbow areas. Abnormal webbing at the bend of the elbow (antecubital pterygium) may also be surgically released to help improve arm extension. However, further surgical manipulation of the elbows may be quite difficult because the internal elbow structures may be misplaced due to its abnormal embryologic development. For this reason, magnetic resonance imaging is recommended prior to undertaking surgery on the elbow (or knee, for that matter). Scoliosis may be treated with a combination of exercises and physical therapy, other supportive techniques, braces, casts, and/or corrective surgery.
In individuals with open-angle glaucoma, treatment measures may include the use of medicated eye drops to help reduce fluid pressure in the eyes, certain medications by mouth, and/or surgery. In affected children with other ocular abnormalities associated with nail patella syndrome, corrective glasses, contact lenses, and/or surgery may be used in some cases to help improve vision.
Affected individuals with nephropathy, particularly those who have been diagnosed with nephrotic syndrome, should be referred to physicians who specialize in diseases affecting the kidneys (nephrologists). Blood pressure and kidney function must be monitored closely and treated if abnormal.
Early intervention is important to ensure that children with nail patella syndrome reach their potential. Special services that may be beneficial to affected children may include physical therapy, special social support, and other medical, social, and/or vocational services.
Genetic counseling is recommended for affected individuals and their families. Family members of individuals with nail patella syndrome should also receive thorough clinical examinations and other appropriate tests to detect certain abnormalities potentially associated with the disorder. Other treatment for this disorder is symptomatic and supportive.
Long term monitoring
Children and adolescents with nail patella syndrome should be carefully monitored for abnormal sideways curvature of the spine (scoliosis) to ensure prompt detection and appropriate preventive and/or corrective treatment. Affected individuals should also receive thorough eye examinations to confirm and/or detect the presence of certain ocular abnormalities that may be associated with nail patella syndrome (e.g., open-angle glaucoma, microcornea, cataracts). For example, in many cases, open-angle glaucoma may initially cause no apparent symptoms and therefore may only be detected during an eye examination, including specialized testing to measure eye pressure. Early detection of glaucoma is important in ensuring prompt treatment to reduce eye fluid pressure and prevent progressive visual impairment.
In addition, physicians may closely monitor individuals with nail patella syndrome beginning in early infancy to ensure prompt detection of abnormal kidney function and implementation of immediate, appropriate treatment measures to help prevent potential progressive kidney disease. Laboratory tests may confirm certain findings that may indicate renal insufficiency, such as blood tests to check BUN and creatinine levels. Screening for nephropathy may include urinary analysis which may reveal small traces of blood (hematuria) and/or abnormally high levels of protein (proteinuria), specifically albumin (albuminuria), in the urine. Additional laboratory studies may reveal unusually low levels of albumin in an affected individual’s blood (hypoalbuminemia). Such findings, occurring in association with anemia and edema, may indicate a diagnosis of nephrotic syndrome in some individuals with nail patella syndrome.
Microscopic examination (e.g., immunofluorescence and electron microscopy) of samples of kidney tissue (renal biopsy) may reveal certain characteristic structural abnormalities that may be present even in some individuals with nail patella syndrome who may not exhibit observable symptoms or clinical findings indicating renal involvement. For example, in many affected individuals both with and without apparent clinical renal involvement, microscopic examination may reveal certain abnormal changes of the clusters of capillaries (renal glomeruli) that filter blood passing through the kidneys. Such changes may include an increased number of cells (hypercellularity), abnormal thickening of the capillary walls, abnormal deposits of the protein collagen, and/or replacement of normal tissue with scar tissue (focal and segmental sclerosis). In some cases, confirmation of certain glomerular changes may reveal impairment of the glomeruli’s filtering ability and may help to confirm a diagnosis of nephrotic syndrome.
Nail patella syndrome life expectancy
Nail-patella syndrome life expectancy is determined by the associated abnormalities, mainly kidney disease 5. The incidence of nephropathy in nail-patella syndrome is reported to be approximately 40% among patients with various degrees of dysfunction. Of these patients, 10% die of kidney failure 6. About 5% of people with nail-patella syndrome develop end-stage kidney disease, meaning that the kidneys stop working and the person may require a kidney transplant. In general, people with the nail-patella syndrome do well after kidney transplants.
References- Sweeney E, Hoover-Fong JE, McIntosh I. Nail-Patella Syndrome. 2003 May 31 [Updated 2014 Nov 13]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1132
- Nail-patella syndrome. https://ghr.nlm.nih.gov/condition/nail-patella-syndrome
- Romero, P.L., Sanhueza, F.A., López, P.R., Reyes, L.F., & Herrera, L.M. (2011). c.194 A>C (Q65P) mutation in the LMX1B gene in patients with nail-patella syndrome associated with glaucoma. Molecular vision. https://pdfs.semanticscholar.org/3830/4d178f725c9543ea2c514bdaf890f3bf1ef6.pdf
- Louboutin L, Wascher D, Neyret P. Management of patellar problems in skeletally mature patients with nail-patella syndrome. Knee Surg Sports Traumatol Arthrosc. 2016 Feb 12.
- Pascoe VL, Fenves AZ, Wofford J, Jackson JM, Menter A, Kimball AB. The spectrum of nephrocutaneous diseases and associations: Inflammatory and medication-related nephrocutaneous associations. J Am Acad Dermatol. 2016 Feb. 74 (2):247-70; quiz 271-2.
- Nail-patella syndrome. https://emedicine.medscape.com/article/1106294-overview