What is a natural birth
Natural childbirth can refer to many different ways of giving birth without using pain medication, either in the home or at the hospital or birthing center 1.
Natural childbirth is a way of giving birth by letting nature take its course. This may include:
- going through labor and delivery without the help of medications, including pain relievers such as epidurals
- using few or no artificial medical interventions such as continuous fetal monitoring or episiotomies (when the area between the vagina and anus, called the perineum, is cut to make room for the baby during delivery)
- allowing the woman to lead the labor and delivery process, dealing with it in any way she is comfortable
Many women with low-risk pregnancies choose to go through natural childbirth to avoid any possible risks that medications could pose for the mother or baby. Pain medications can affect your labor — your blood pressure might drop, your labor might slow down or speed up, you might become nauseous, and you might feel a sense of lack of control.
But many women choose natural childbirth to feel more in touch with the birth experience and to deal with labor in a proactive manner.
Preparation for birth can help to reduce the experience of pain and reduce anxiety, which can help you to better cope with labor.
There are a number of methods you can use to help you cope with your labor pain.
Like the labor experience, this is an individual decision. Some women are keen to avoid medications, others are happy to consider all available options. You need to choose the best coping technique or combination that suits you and your needs. Remember, your plan may change when you are in labor. Labor might hurt more than you had anticipated. Some women who had previously said they want no pain medicine whatsoever end up changing their minds once they’re actually in labor. This is very common and completely understandable.
During your labor, your midwife will continue to guide you and work with you according to your wishes.
A woman should discuss the many aspects of labor with her health care provider well before labor begins to ensure that she understands all of the options, risks, and benefits of pain relief during labor and delivery. It might also be helpful to put all the decisions in writing to clarify the options chosen.
- If you’re having a high-risk pregnancy, it’s best to give birth in a hospital, where you can receive any necessary medical care (especially in the event of an emergency).
How Is Natural Childbirth Done?
How you choose to work through the pain is up to you. Different women find that different methods work best for them. Many can control the pain by channeling their energy and focusing their minds on something else. The two most common childbirth philosophies in the United States are the Lamaze technique and the Bradley method.
The Lamaze technique teaches that birth is a normal, natural, and healthy process but takes a neutral position toward pain medication, encouraging women to make an informed decision about whether it’s right for them.
The Bradley method (also called Husband-Coached Birth) emphasizes a natural approach to birth and the active participation of a birth coach. A major goal of this method is the avoidance of medications unless absolutely necessary. The Bradley method also focuses on good nutrition and exercise during pregnancy and relaxation and deep-breathing techniques as a method of coping with labor. Although the Bradley method advocates a medication-free birth experience, the classes do prepare parents for unexpected complications or situations, like emergency C-sections.
Women who choose natural childbirth can use a number of natural ways to ease pain. These include 2, 3:
- Emotional support
- Relaxation techniques
- A soothing atmosphere
- Moving and changing positions frequently (such as walking around, showering, rocking, or leaning on birthing balls)
- Using a birthing ball
- Using soothing phrases and mental images
- Placing a heating pad or ice pack on the back or stomach
- Massage or counterpressure
- Taking a bath or shower
- Hypnosis (also called “hypnobirthing”)
- Using soothing scents (aromatherapy)
- Acupuncture or acupressure
- Applying small doses of electrical stimulation to nerve fibers to activate the body’s own pain-relieving substances (called transcutaneous electrical nerve stimulation, or TENS)
- Injecting sterile water into the lower back, which can relieve the intense discomfort and pain in the lower back known as back labor.
- Yoga
- Meditation
- Walking
- Immersion in warm water or a jacuzzi
- Distractions via activities that keep the mind otherwise occupied
- Listening to soothing music
- Visual imagery.
What If I Can’t Handle the Pain?
Every woman experiences pain in a different way. The way you experience pain depends on your emotional, psychological, social, motivational and cultural circumstances. Every woman responds and copes differently with the pain of labor and childbirth.
Labor might hurt more than you had anticipated. Some women who had previously said they want no pain medicine whatsoever end up changing their minds once they’re actually in labor. This is very common and completely understandable.
You should be applauded for your willingness and enthusiasm to try to deliver naturally. But if it turns out that the pain is too much to bear, don’t feel bad about requesting medications. And if something doesn’t go according to plan, you may need to be flexible as circumstances change. That doesn’t make you any less brave or committed to your baby or the labor process. Giving birth is a beautiful and rewarding experience, with or without medical intervention.
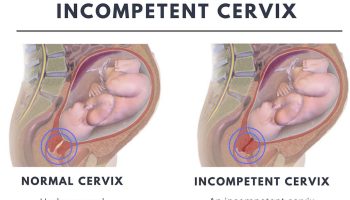
Natural pain relief
- Relaxation: Being relaxed in labor has many benefits. Your body will work better if you’re relaxed. Your natural hormones that help your labor progress (oxytocin), and those ‘natural pain-relief hormones’ (endorphins) that help you cope with labor, will be released more readily. Fear, tension and resistance are a normal response when you feel out of control or you are not sure what to expect next. On the other hand, relaxing and trusting that your body knows what to do will help you manage your pain. Learn how to relax, stay calm and breathe deeply. Breathing techniques may help you to ‘ride the waves’ of each contraction. Remember that a relaxed mind is a relaxed cervix. If your face is relaxed, the muscles through your pelvis are too.
- Active birth: Moving around and changing positions is one of the most helpful things you can do to manage the pain of labor and birth. Being able to move freely and rocking your pelvis can help you to cope with the contractions. If you stay upright, gravity will also help your baby to move down through your pelvis.
- Heat and water: The use of heat can help to ease tension and discomfort in labor. Both hot and cold packs are useful, as is being immersed in water in either a shower or a bath. Healthy women with uncomplicated pregnancies may find that having a warm bath in labor helps with relaxation and pain relief. A warm bath increases relaxation and production of endorphins (your body’s natural pain relief hormone). It reduces the pain of contractions and the pressure on your pelvis and muscles.
- Touch and massage: Feeling stressed and anxious makes pain seem worse. Massage can reduce muscle tension as well as providing a distraction between and during contractions. Practise with your partner during your pregnancy and find out how you like to be massaged. At different stages during labor, massage and touch will feel good and at other times you may find it distracting or annoying.
- Complementary therapies: Alternative therapies such as acupuncture, acupressure or aromatherapy can also be very effective, but should only be practised by qualified practitioners.
Non-medical pain relief
- TENS (Transcutaneous electrical nerve stimulation) also called electrotherapy: A TENS machine delivers a small electrical current to your body through electrodes attached to your skin. It does not involve medicines or injections. The TENS machine is a small, portable, battery-operated device that is worn on your body. The box is attached by wires to sticky pads that are stuck to the skin on your back. The machine has dials that you can adjust to control the frequency and strength of small electrical pulses that are transmitted to your body. These pulses stimulate your body to release your endorphins.
- Water injections for back pain: Many women have lower back pain that persists throughout their labor. Midwives can use a technique where sterile water injections are given in four different places in your lower back, just beneath the skin. The injections cause a strong stinging sensation, like a bee sting. The sting will last for up to 30 seconds before disappearing along with the back pain. The injections can provide a few hours of pain relief to your lower back without any side effects for you or your baby.
Medical pain relief
- Nitrous oxide gas also known as ‘laughing gas’, women in labor can breathe a mixture of nitrous oxide and oxygen through a mouth piece or mask. The gas is inhaled during a contraction and helps take the edge off your pain. Many women choose the gas as it makes them feel in control of their pain-relief and provides them with something to focus on to get through each contraction. There are no after-effects for you or your baby. The mixture of gas can be changed during different stages of your labor to provide better pain relief or if you feel a little nauseous or light-headed.
- Pethidine or morphine injection: Pethidine and morphine are strong painkillers given by injection. You may be offered one of these medications, which work by mimicking the effects of endorphins. Although they help reduce the severity of the pain, they do not take it away completely. Women have varying responses to morphine and pethidine. Some women will say the injection provided pain relief, while others will say it had no effect at all on their level of pain. The injections can take up to 30 minutes to work and can make you feel quite nauseated. Because these drugs cross the placenta to your baby, your baby may become sleepy. Sometimes pethidine may contribute to breathing problems in your baby if given within two hours of birth. For this reason and due to its relatively short period of effect, it is mostly helpful for women who are in well-established labor but not too close to giving birth.
- Epidural: An epidural is a procedure where an anesthetic (a drug that gives either partial or total loss of sensation) is injected into the small space in your back near your spinal cord by a specialist anaesthetist. After an epidural, you will have altered sensation from your waist down. How much you can move your legs after an epidural will depend on the type and dose of anaesthetic used. A very thin tube will be left in your back so the anaesthetic can be topped up. Sometimes the tube is attached to a machine so that you have control over when the epidural is topped up. The benefits of an epidural are that it takes away the pain of contractions, it can be effective for hours and can be increased in strength if you need to have an emergency cesarean. In a long labor, it can allow you to sleep and recover your strength. Epidurals can cause a fall in blood pressure, so you will usually have an intravenous drip (a bag of liquid that enters your body through a tube) put into your arm or the back of your hand, and your blood pressure will be monitored more closely. You may also lose the sensation to pass urine, so you will have a catheter tube inserted into your bladder to drain your urine. Because of the potential side effects such as low blood pressure, the baby’s heart rate will need to be continuously monitored by a cardiotocography (CTG) machine following an epidural. The chance of you needing assistance with the birth of your baby increases once you have had an epidural. A stronger epidural or ‘top up’ will help relieve the pain of these procedures.
Not all birth places can offer every method of pain management. You might like to talk to your care provider about the pain relief options available to you at your planned place of birth and which methods of pain relief can and can’t be used together. You can choose one method or a few, or you change from one to another during labor. Remember it is important to keep an open mind and have a positive attitude and confidence in your ability to labor.
Dealing With Pain During Childbirth
If you’re like most women, the pain of labor and delivery is one of the things that worry you about having a baby. This is certainly understandable, because labor is painful for most women.
It’s possible to have labor with relatively little pain, but it’s wise to prepare yourself by planning some strategies for coping with pain. Planning for pain is one of the best ways to ensure that you’ll stay calm and be able to deal with it when the time comes.
Pain During Labor and Delivery
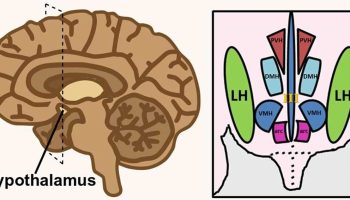
Pain during labor is caused by contractions of the muscles of the uterus and by pressure on the cervix. This pain can be felt as strong cramping in the abdomen, groin, and back, as well as an achy feeling. Some women experience pain in their sides or thighs as well.
Other causes of pain during labor include pressure on the bladder and bowels by the baby’s head and the stretching of the birth canal and vagina.
Pain during labor is different for every woman. Although labor is often thought of as one of the more painful events in human experience, it ranges widely from woman to woman and even from pregnancy to pregnancy. Women experience labor pain differently — for some, it resembles menstrual cramps; for others, severe pressure; and for others, extremely strong waves that feel like diarrheal cramps.
It’s often not the pain of each contraction on its own that women find the hardest, but the fact that the contractions keep coming — and that as labor progresses, there is less and less time between contractions to relax.
Preparing for Pain
To help with pain during labor, here are some things you can start doing before or during your pregnancy:
Regular and reasonable exercise (that your doctor says is OK) can help strengthen your muscles and prepare your body for the stress of labor. Exercise also can increase your endurance, which will come in handy if you have a long labor. The important thing to remember with any exercise is not to overdo it — and this is especially true if you’re pregnant. Talk to your doctor about what he or she considers to be a safe exercise plan for you.
If you and your partner attend childbirth classes, you’ll learn different techniques for handling pain, from visualization to stretches designed to strengthen the muscles that support your uterus. The two most common childbirth philosophies in the United States are the Lamaze technique and the Bradley method.
The Lamaze technique is the most widely used method in the United States. The Lamaze philosophy teaches that birth is a normal, natural, and healthy process and that women should be empowered to approach it with confidence. Lamaze classes educate women about the ways they can decrease their perception of pain, such as through relaxation techniques, breathing exercises, distraction, or massage by a supportive coach. Lamaze takes a neutral position toward pain medication, encouraging women to make an informed decision about whether it’s right for them.
The Bradley method (also called Husband-Coached Birth) emphasizes a natural approach to birth and the active participation of the baby’s father as birth coach. A major goal of this method is the avoidance of medicines unless absolutely necessary. The Bradley method also focuses on good nutrition and exercise during pregnancy and relaxation and deep-breathing techniques as a method of coping with labor. Although the Bradley method advocates a medication-free birth experience, the classes do do discuss unexpected complications or situations, like emergency cesarean sections.
Some ways to handle pain during Natural Birth: see above.
Pain Medications
A variety of pain medications can be used during labor and delivery, depending on the situation. Talk to your health care provider about the risks and benefits of each.
Analgesics. Pain medicines can be given many ways. If they are given intravenously (through an IV) or through a shot into a muscle, they can affect the whole body. These medicines can cause side effects in the mother, including drowsiness and nausea. They also can have effects on the baby.
Regional anesthesia. This is what most women think of when they consider pain medication during labor. By blocking the feeling from specific regions of the body, these methods can be used for pain relief in both vaginal and cesarean section deliveries.
Epidurals, a form of local anesthesia, relieve most of the pain from the entire body below the belly button, including the vaginal walls, during labor and delivery. An epidural involves medicine given by an anesthesiologist through a thin, tube-like catheter that’s inserted in the woman’s lower back. The amount of medication can be increased or decreased according to a woman’s needs. Very little medication reaches the baby, so usually there are no effects on the baby from this method of pain relief.
Epidurals do have some drawbacks — they can cause a woman’s blood pressure to drop and can make it difficult to urinate. They can also cause itching, nausea, and headaches in the mother. The risks to the baby are minimal, but include problems caused by low blood pressure in the mother.
Tranquilizers. These drugs don’t relieve pain, but they may help to calm and relax women who are very anxious. Sometimes they are used along with analgesics. These drugs can have effects on both the mother and baby, and are not often used. They also can make it difficult for women to remember the details of the birth. You should discuss the risks of taking tranquilizers first with your doctor.
Things to Consider
Here are some things to think about when considering pain control during labor:
- Medicines can relieve much of your pain, but probably won’t relieve all of it.
- Labor may hurt more than you anticipated. Some women who have previously said they want no pain medicine whatsoever end up changing their minds once they’re actually in labor.
- Certain medications can affect your baby, causing the baby to be drowsy or have changes in the heart rate.
Talking to Your Health Care Provider
You’ll want to review your pain control options with the person who’ll be delivering your baby. Find out what pain control methods are available, how effective they’re likely to be, and when it’s best not to use certain medications.
If you want to use pain-control methods other than medication, make sure your health care provider and the hospital staff know. You might want to also consider writing a birth plan that makes your preferences clear.
Remember, too, that many women make decisions about pain relief during labor that they abandon — often for very good reason — at the last minute. Your ability to endure the pain of childbirth has nothing to do with your worth as a mother. By preparing and educating yourself, you can be ready to decide what pain management works best for you.
Where is Natural Birth Done ?
Some women who opt for natural childbirth choose to deliver in a non-hospital setting such as a birth center, where natural childbirth is the focus. Women are free to move around during their labor, get in positions that are most comfortable to them, and spend time in the tub or jacuzzi. The baby is monitored frequently, often with a handheld ultrasound device. Comfort measures such as hydrotherapy, massage, warm and cold compresses, and visualization and relaxation techniques are often used. The woman is free to eat and drink as she chooses.
A variety of health care professionals may work in the birth center setting — such as registered nurses, certified nurse midwives, and doulas (professionally trained providers of labor support and/or postpartum care) who act as labor assistants.
Studies indicate that getting continuous support during labor from a trained and experienced companion, such as a midwife or doula, can mean shorter labor, less (or no) medications, less chance of needing a C-section, and a more positive feeling about the labor when it’s over.
These days, it’s also possible to have a more natural childbirth in many hospitals. Some hospitals have birth centers, where a natural approach is taken, but medical intervention is available if needed. Many hospitals have modified their approach for low-risk births, and have rooms with homelike settings where women can labor, deliver, and recover without being moved. They may take their cues from the laboring woman, allowing labor to proceed more slowly and without intervention if all seems to be going well. They may use alternative pain-management techniques if requested and welcome the assistance of labor assistants like midwives or doulas.
In addition to the father, other children, grandparents, and friends may be allowed to attend the births (which is also common practice at birth centers). After birth, babies might remain with the mother longer. In its fullest form, this approach is sometimes called family-centered care.
What Will Natural Birth Feel Like ?
Although labor is often thought of as one of the more painful events in human experience, it varies widely from woman to woman and even from pregnancy to pregnancy. Women experience labor pain differently — for some, it resembles menstrual cramps; for others, severe pressure; and for others, extremely strong waves that feel like diarrheal cramps. First-time mothers are more likely to give their pain a higher rating than women who’ve had babies before.
How Long Will Natural Birth Take ?
There’s no magic timetable when you’re giving birth. For some women, the baby comes in a few hours; for many others it may take all day (or longer). Whether you opt for medications or not, every woman’s body reacts to labor differently.
Risks and Precautions of Natural Birth
Natural childbirth is, in general, very safe. But it becomes risky when a woman ignores her health care provider’s recommendations or if she refuses medical intervention if everything doesn’t go as planned.
It’s important for the well-being of you and your baby to be open to other options if complications occur. In an emergency, refusing medical help could put your life and your baby’s at serious risk.
After Natural Birth Delivery
Like any woman who’s given birth, you’ll probably feel:
- exhausted — both you and your baby will probably want to sleep as much as possible
- shaky or cold — many women shiver after delivery; this is a natural reaction
- sore — you’ll probably feel cramping in your uterus, especially with breastfeeding, and you’ll have some pain and discomfort in and around your vagina
- elated and empowered — you may feel an overwhelming sense of accomplishment knowing that you did it
Natural birth plan
A birth plan is a set of instructions you make about your baby’s birth. Fill out this plan with your partner. Then share it with your provider, your family and other support people. It’s best for everyone to know ahead of time how you want labor and birth to be.
- For a free copy of a birth plan get it here: 4
A birth plan tells your provider how you feel about things like who you want with you during labor, what you want to do during labor, if you want drugs to help with labor pain, and if there are special religious or cultural practices you want to have happen once your baby is born.
- Important: the goal of a birth plan isn’t for you and your partner to decide exactly how the birth of your child will happen — labor involves so many variables, you can’t predict exactly what will happen. A birth plan isn’t a binding agreement — it’s just a guideline.
Note: How can you use your birth plan
Fill out a birth plan with your partner. While completing a birth plan, you’ll be learning about, exploring, and understanding your labor and birthing options well before the birth of your child. This can also improve your communication with the people who’ll be helping during your delivery. By sharing your birth plan with your provider and with the nurses at the hospital or birthing center where you plan to have your baby – you’re letting everyoneknow ahead of time how you want labor and birth to be. Share it with your family and other support people, too.
Your doctor or health care provider may know, from having seen you throughout the pregnancy, what you do and don’t want. But, if you go into labor when there’s an on-call doctor who you don’t know well, a well thought-out birth plan can help you communicate your goals and wishes to the people helping you with the labor and delivery.
Figure 1. Birth Plan


Things to Consider
Before you make decisions about each of your birthing options, you’ll want to talk with your health care provider and tour the hospital or birthing center where you plan to have your baby.
You may find that your obstetrician, nurse-midwife, or the facility where they admit patients already has birth-plan forms that you can fill out. If so, use the form as a guideline for asking questions about how women in their care are routinely treated. If their responses are not what you’re hoping for, you might want to look for a health provider or facility that better matches your goals.
And it’s important to be flexible — if you know one aspect of your birthing plan won’t be met, be sure to weigh that against your other wishes. If your options are limited because of medical needs, insurance, cost, or geography, focus on one or two areas that are really important to you. In the areas where your thinking doesn’t agree with that of your doctor or nurse-midwife, ask why he or she usually does things a certain way and listen to the answers before you make up your mind. There may be important reasons why a doctor believes some birth options are better than others.
Finally, find out if there are things about your pregnancy that might prevent certain choices. For example, if your pregnancy is considered high risk because of your age, health, or problems during pregnancy (current or previous), your health care provider may advise against some of your birthing wishes. You’ll want to discuss, and consider, this information when thinking about your options.
What Are Your Birthing Options ?
In creating your birthing plan, you’re likely to have choices in the following areas:
Where to have the baby. Most women give birth in the hospital. However, most are no longer confined to a cold, sterile maternity ward. Find out if your hospital practices family-centered care. This usually means the patient rooms will have a door, furnishings, a private bathroom, and enough space to accommodate a family.
Additionally, many hospitals now offer birthing rooms that allow a woman to stay in the same bed for labor, delivery, and sometimes, postpartum care (care after the birth). These rooms are fully equipped for uncomplicated deliveries. They’re often attractive and have gentle lighting.
But some women believe that the most comfortable environment is their own home. Advocates of home birth believe that labor and delivery can and should happen at home, but they also stress that a certified nurse-midwife or doctor should attend the birth.
An important thing to remember about home birth is that if something goes wrong, you don’t have the amenities and technology of a hospital. It can take a while to get to the hospital, and during a complicated birth those minutes can be invaluable.
For women with low-risk pregnancies who want something in between the hospital and home, birthing centers are another option. These provide a more homey, relaxed environment with some of the medical amenities of a hospital. Some birthing centers are associated with hospitals and can transfer patients if necessary. It’s a good idea to find out what happens in case of a complication: How would you get to the hospital? How long would the transfer take?
Who will assist at the birth
Most women choose an obstetrician (OB/GYN), a specialist who’s trained to handle pregnancies (including those with complications), labor, and delivery. If your pregnancy is considered high risk, you may be referred to an obstetrician who subspecializes in maternal-fetal medicine. These doctors have specialized training to care for pregnant women with medical conditions or complications, as well as their fetuses.
Another medical choice is a family practitioner who has had training and has maintained expertise in managing non-high-risk pregnancies and deliveries. In some areas of the United States, especially rural areas where obstetricians are less available, family practitioners handle most of the deliveries. As your family doctor, a family practitioner can continue to treat both you and your baby after birth.
And doctors aren’t the only health care providers a pregnant woman can choose to deliver her baby. You might decide that you want your delivery to be performed by a certified nurse-midwife, a health professional who’s medically trained and licensed to handle low-risk births and whose philosophy emphasizes educating expectant parents about the natural aspects of childbirth.
Increasing numbers of women are choosing to have a doula, or birth assistant, present in addition to the medical personnel. This is someone who’s trained in childbirth and is there to provide support to the mother. The doula can meet with the mother before the birth and can help communicate her wishes to the medical staff, should it be necessary.
Your birth plan can also indicate who else you’d like to have with you before, during, and immediately after the birth. In a routine birth, this may be your partner, your other children, a friend, or other family member. You also can make it clear at what points you want no one to be there but your partner.
More Birthing Options
Atmosphere during labor and delivery. Many hospitals and birthing centers now allow women to make some choices about the atmosphere in which they give birth. Do you want music and low lighting? How about the freedom to walk around during labor? If possible, would you like to eat or drink during labor? You might be able to request things that may make you the most comfortable — from what clothes you’ll wear to whether you’ll have a DVD player in your room.
Procedures during labor. Hospitals used to perform the same procedures on all women in labor, but many now show increased flexibility in how they handle their patients. Some examples include:
- enemas. Used to clean out the bowels, enemas used to be routine when women were admitted. Now, you may choose to give yourself an enema or to skip it entirely.
- induction of labor. At times, labor may need to be induced or sped up for medical reasons. But sometimes, practitioners will give women the option of getting some help to move things along, or giving labor a little more time to progress on its own.
- shaving the pubic area. Once routine, shaving is no longer done unless a woman requests it.
Other procedures that you can include in your birth plan are preferences about fetal monitoring, extra birthing equipment you’d like in the room, and how often you have internal exams during labor.
Pain management. This is important for most women and is certainly something you have a lot of control over. It’s also something you’ll want to discuss carefully with your health care provider. Some women change their minds about pain relief during labor only to discover that they’re too far along in their labor to use certain methods, such as an epidural. You’ll also want to be aware of alternative forms of pain relief, including massage, relaxation, breathing, and bathing. Know your options and make your wishes known to your care provider.
Position during delivery. You can try a variety of positions during labor, including the classic semi-recline with the feet in stirrups that you’ve seen in the movies. Other choices include lying on your side, squatting, standing, or simply using whatever stance feels right at the time.
Episiotomies. When necessary, doctors perform episiotomies (when the perineum — the area of skin between the vagina and the anus — is partially cut to ease the delivery). You may have one if you risk tearing or in the case of a medical emergency. But if there is an option, you can discuss your preference with your provider.
Assisted birth. If the baby becomes stuck in the birth canal, an assisted birth (i.e., using forceps or vacuum extraction) may be necessary.
Cesarean section (C-section). You might not want to think about this, but if you have to have a cesarean, you’ll need to consider a few things. Do you want your partner to be present, if possible? What about viewing the birth — do you want to see the baby coming out?
Post-birth. Decisions to be made about the time immediately after birth include:
- Would your partner like to cut the umbilical cord ?
- Does your partner want to hold the baby when the baby emerges ?
- Do you want immediate contact with the baby, or would you like the baby to be cleaned off first ?
- How would you like to handle the delivery of the placenta ? Would you like to keep the placenta ?
- Do you want to feed the baby right away ?
Communicating Your Wishes
Give your health care provider your reasons for creating a birth plan — not because you don’t trust him or her, but to help ensure cooperation and to cover the possibilities if something should go wrong. If your caregiver seems offended or is resistant to the idea of a birth plan, you might want to reconsider whether this is the right caregiver for you.
Also, think about the language of your plan. You can use many online resources to create one or you can make one yourself.
Here are some tips:
- Make your birth plan read like a list of requests or best-case scenarios, not like a set of demands. Phrases such as “I would prefer” and “if medically necessary” will help your health care provider and caregivers know that you understand that they might have to change the plan.
- Think about the other personnel who’ll be using it — hospital staffers might feel more comfortable if you call it your “birth preferences” rather than your “birth plan,” which could seem as though you’re trying to tell them how to do their jobs.
- Try to be positive (“we hope to”) as opposed to negative (“under no circumstances”).
Once you’ve made your birth plan, schedule a time to go over it with your doctor or nurse-midwife. Find out and discuss where you agree or disagree. During your pregnancy, review the birth plan with your partner periodically to make sure that it’s still in line with both of your wishes.
Strive to keep the plan as simple as possible — preferably less than two pages — and list them in order of importance. Focusing on your priorities will help ensure that the most important of your wishes are met.
You may also want to make several copies of the plan: one for you, one for your chart, one for your doctor or nurse-midwife, and one for your birthing coach or partner. And bringing a few extra copies in your labor bag is a good idea, especially if your doctor ends up not being on call when your baby is born.
Although you might not be able to control everything that happens to you during your baby’s birth, you can play a role in the decisions that are made about your body and your baby. A well thought-out birth plan can help you to do that.
Birth Is Intended to Happen Simply, Without Worry or Trouble
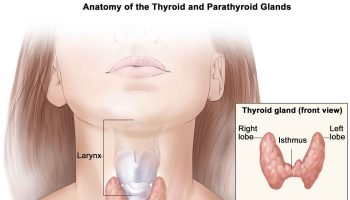
The physiologic process of birth is simply and carefully designed. Women’s bodies are designed to grow, birth, and nourish babies. In the last weeks of pregnancy, a series of physiologic changes occur, mostly, as evidence suggests, orchestrated by the baby. The cervix softens and may begin to dilate and efface. The uterine muscle becomes increasingly responsive to oxytocin. At first, oxytocin levels rise gradually and, when labor starts, more quickly. The pain associated with strong uterine contractions (the result of higher levels of oxytocin) sends a signal to the brain that stimulates the ongoing release of the large amounts of oxytocin required for strong, effective contractions. Coping with the increasingly strong contractions (by movement, relaxation, and other comfort measures) insures the continued release of oxytocin.
Pain plays an important role in helping labor progress by insuring that increasing amounts of oxytocin are released 5. When oxytocin levels are high (and the contractions are painful), beta-endorphins (“nature’s narcotic”) are released. Endorphins help women manage the pain of contractions by inducing an almost dream-like state and decreasing pain perception. In a very real sense, nature does not abandon women during labor.
Stress hormones, however, disrupt the process. Especially in early labor, stress and anxiety can stop labor; in active labor, stress can slow progress. Privacy and feeling safe and protected emotionally as well as physically help keep catecholamine levels low and labor progressing.
Women begin to have an instinctive urge to push as the baby moves down the birth canal. Following the urge, quite naturally, and changing positions in response to what the woman is feeling not only helps the baby descend and rotate but also protects the baby and the birth canal. When the baby is just ready to be born, if oxytocin and endorphin levels are high, a natural release of catecholamines gives women a surge of strength to push the baby out.
The baby is born with high levels of catecholamines and endorphins and is alert and calm. Placed skin-to-skin with his mother, the baby will find the breast and self attach. Even the small movements of the baby, when skin-to-skin with his mother, stimulate the release of maternal oxytocin. Oxytocin facilitates the separation and delivery of the placenta, decreasing the risk of maternal hemorrhage, and sets the stage for efficient milk let down and successful breastfeeding. Babies kept skin-to-skin stay warmer, are less likely to become hypoglycemic, cry less, have more stable heart rates, and breastfeed for a longer duration than babies who are separated from their mother 6.
Every pregnant women needs to know that labor and birth are simply and beautifully designed. In order to keep labor and birth as safe as possible, and to minimize the risk of complications, it is essential to respect the simple, natural, physiologic process of labor and birth and not interfere in any way, unless there is a clear medical indication. There is an optimal way to give birth, and this is it.
How to prepare for natural birth
Every pregnant woman needs to know that birth is intended to happen simply and easily and that six key birth practices make birth safer for mothers and babies.
The World Health Organization (WHO) identifies four care practices that promote, support, and protect normal birth 7. Lamaze International identifies two additional practices. Together, these six practices are supported by research, including systematic reviews from The Cochrane Library and the Coalition for Improving Maternity Services 8. Romano and Lothian 9 provide a detailed overview of the research that supports these six care practices. Written for women and their families, the Lamaze Healthy Birth Practice papers describe the importance of each of the six practices for a healthy, safe birth and provide a synopsis of the evidence that supports each practice. Every pregnant woman needs to know that these six evidence-based birth practices make birth healthier and safer for mothers and babies.
Childbirth education
Childbirth education can simplify pregnancy and birth and help women navigate the maze of modern obstetrics in order to have a safe, healthy birth. Pregnancy is complex and fraught with potential for worry and confusion. It is easy to fall into the trap of thinking that things can go terribly wrong. Excellent childbirth education can help women learn how simple birth can and should be, how to stay confident in their ability to grow and birth their babies, and how to avoid “spoiling the pregnancy” with worry and fear.
Preparation for birth and mothering starts at the beginning of pregnancy 10. It takes 9 months to grow a baby and to prepare emotionally and physically for birth and being a mother. Over the course of the pregnancy, women slowly attach to their babies, getting to know them through kicks and periods of rest and through changes to their own bodies as the pregnancy progresses. The physical growth of the baby happens simply and easily from one day to the next throughout pregnancy, but the emotional and psychological changes of pregnancy can easily be disrupted.
Childbirth education, right from the beginning of pregnancy, can help women choose health-care providers and places of birth that provide evidence-based maternity care, make thoughtful but sometimes difficult decisions about prenatal testing, and deal with fears for themselves and their babies. And, over the course of the pregnancy, childbirth education can help women develop plans for labor so that labor and birth can unfold optimally in the safest, healthiest way possible.
Childbirth education can help women connect with excellent resources and research to help them make decisions about their pregnancies and births that ultimately will make birth healthier and safer for them and their babies. Some of those resources include Lamaze’s weekly pregnancy e-mails 11 and the six Lamaze Healthy Birth Practice papers. Other resources include information provided by the organizations Childbirth Connection 12, the Coalition for Improving Maternity Services 13 and Choices in Childbirth 14.
Healthy Birth Practice #1: Let Labor Begin on Its Own
In most cases, the best way to insure that the baby is ready to be born and the mother’s body is ready to birth her baby is to let labor begin on its own 15. In the last weeks of pregnancy, the baby moves down into the pelvis, the cervix softens, and the uterine muscle becomes more receptive to oxytocin. The baby’s lungs mature, and he puts on a protective layer of fat. Every day makes a difference in how mature the baby is and how well he is able to make the transition to life outside the womb 16.
Elective labor induction not only increases the use of analgesia and epidural anesthesia but also the incidence of nonreassuring fetal heart rate patterns, shoulder dystocia, instrument delivery, and cesarean surgery 17. It is not without risk for the baby either, increasing the need for neonatal resuscitation and increasing the likelihood of low birth weight and admission to the neonatal intensive care unit 17. Although women are told that if a baby is thought to be large it is safer to induce labor early, this is not true. Suspected macrosomia is not an indication for induction, and induction for suspected macrosomia does not reduce the incidence of shoulder dystocia and is associated with an increased risk of cesarean 18.
Every pregnant woman needs to know that it is healthier and safer for both mother and baby to let labor begin on its own.
Healthy Birth Practice #2: Walk, Move Around, and Change Positions Throughout Labor
Moving in labor helps women cope with strong and painful contractions while gently moving the baby into the pelvis and through the birth canal 19. The pain of contractions can be a guide to the laboring woman as she moves in response to what she feels, trying to find comfort as the contractions become increasingly strong. Finding comfort in a variety of ways, including movement, helps labor progress. When women are able to cope with increasingly strong contractions, increasing amounts of oxytocin are released, and this keeps labor progressing. Movement in response to pain also protects the baby and the birth canal, especially during pushing. Research supports that walking, movement, and changing positions may shorten labor, are effective forms of pain relief, and are associated with fewer nonreassuring fetal heart rate patterns, fewer perineal injuries, and less blood loss. Walking during the first stage of labor decreases the likelihood of cesarean surgery and forceps and vacuum extraction deliveries 20.
Every pregnant woman needs to know that walking, movement, and changing positions during labor help labor progress, enhance comfort, and decrease the risk of complications.
Healthy Birth Practice #3: Bring a Loved One, Friend, or Doula for Continuous Support
In labor, women feel better when cared for and encouraged by people they know and trust 21. For most women, that means family or close friends. Family and friends support the laboring woman in simple but important ways: protecting her privacy, helping her get comfortable, creating a cocoon that helps her feel safe and protected. This is especially important in the unfamiliar and often overwhelming hospital environment.
In recent years, doulas have provided continuous emotional and physical support for laboring women and their families. Doulas have the advantage of knowing labor and birth well and knowing countless ways of helping women find comfort and feel protected and safe in labor. This experience is a big advantage, especially in restrictive hospital environments. Research findings demonstrate that labor support reduces the likelihood of requesting pain medication, reduces the likelihood of having severe postpartum pain, and increases the likelihood of having a spontaneous vaginal birth. Women who have continuous labor support are more satisfied with the birth experience, have fewer cesareans, and are less likely to use Pitocin during labor 22.
Every pregnant woman needs to know that continuous emotional and physical support in labor makes birth safer and healthier for mother and baby.
Healthy Birth Practice #4: Avoid Interventions That Are Not Medically Necessary
In most hospitals, women routinely have an intravenous line, continuous electronic fetal monitoring, and an epidural 23. Most hospitals also restrict eating and drinking in labor. Each of these practices has the potential to interfere with the process of labor and birth and create complications.
Intravenous lines and electronic fetal monitoring restrict women’s ability to walk, change positions, and find comfort as the contractions become increasingly painful. Food and fluids are typically restricted to prevent the extraordinarily rare occurrence of aspiration if general anesthesia is required. If women are able to eat and drink in labor, there is no need for intravenous lines. No research suggests that labor and birth are safer if food and fluids are restricted and intravenous lines are in place. In fact, increasing evidence indicates that the routine use of intravenous lines may contribute to fluid overload in labor 24.
The routine use of continuous electronic fetal monitoring compared with intermittent auscultation increases the likelihood of instrument vaginal delivery and cesarean surgery but does not reduce the incidence of cerebral palsy, stillbirth, low Apgar scores, newborn death rates, or admission to the neonatal intensive care unit. In essence, the routine use of electronic fetal monitoring increases the risk of the mother having a cesarean with no difference in outcome for the baby 24.
Epidurals interfere in the process of labor and birth in important ways. Because there is no pain, the brain does not get the message to keep releasing oxytocin. Consequently, contractions need to be stimulated with Pitocin. Pitocin does not pass the blood brain barrier; therefore, the body does not know to release endorphins. Women miss out on the valuable effects of endorphins during labor. Epidural use is associated with longer labors, increased likelihood of instrument delivery, more malpositioned babies, more tearing, and an increased risk of cesarean surgery, especially if the epidural is given early in labor 24.
Every pregnant woman needs to know that each of these interventions has unintended effects. When interventions are used routinely, they set the stage for a cascade of other interventions, the physiologic process of labor and birth is disrupted, and women and babies are exposed to unnecessary risks.
Healthy Birth Practice #5: Avoid Giving Birth on the Back, and Follow the Body’s Urges to Push
Upright positions—including squatting, sitting, or lying on the side—make it easier for the baby to descend and move through the birth canal 25. Changing positions helps wiggle the baby through the pelvis by enlarging pelvic diameters. It is also more comfortable to give birth in positions other than on the back. The use of upright or side-lying positions during second-stage labor is associated with a shorter duration of second-stage labor, fewer forceps or vacuum births, fewer episiotomies, fewer abnormal fetal heart rate patterns, and less chance of having severe pain during pushing 26. The findings of this review suggest several possible benefits for upright posture in women without epidural anaesthesia, such as a very small reduction in the duration of second stage of labour (mainly from the primigravid group), reduction in episiotomy rates and assisted deliveries. However, there is an increased risk blood loss greater than 500 mL and there may be an increased risk of second degree tears, though the review authors cannot be certain of this 26. In view of the variable risk of bias of the trials reviewed, further trials using well-designed protocols are needed to ascertain the true benefits and risks of various birth positions 26.
Directed pushing is more stressful for the baby and is associated with increased risk of pelvic floor dysfunction 27. The alternative is to wait for and follow the instinctive urges to push that happen as the baby moves down the birth canal. Even with an epidural, it is safer to wait until the baby moves through the mother’s pelvis on his own.
Every pregnant woman needs to know that it is safer and healthier for mother and baby when the laboring mother pushes in positions other than on her back and follows her own urges to push rather than pushing in a directed way.
Healthy Birth Practice #6: Keep Mother and Baby Together – It’s Best for Mother, Baby, and Breastfeeding
Physiologically, mothers and babies are meant to be together. Mothers are less likely to hemorrhage and are more satisfied. Babies stay warmer, their heart rates are more stable, and their respirations are more regular. They are less likely to become hypoglycemic or have breastfeeding difficulties 28. The benefits are so clear that it is considered a harmful practice to separate mothers and babies unless there is a serious medical indication 29. All the routine care of the baby right after birth can be done with the baby placed skin-to-skin with his mother.
Every pregnant woman needs to know that keeping her baby with her is not just a nice option, but keeping her baby close makes the early hours and days after birth safer for mothers and babies.
Birthing Centers and Hospital Maternity Services
You’ll make plenty of decisions during pregnancy, and choosing where to give birth — whether in a hospital or in a birth center setting — is one of the most important.
Hospitals
Many women fear that a hospital setting will be cold and clinical, but that’s not necessarily true. A hospital setting can accommodate a variety of birth experiences.
Traditional hospital births (in which the mother-to-be moves from a labor room to a delivery room and then, after the birth, to a semiprivate room) are still the most common option. Doctors “manage” the delivery with their patients. In many cases, women in labor are not allowed to eat or drink for medical reasons, and they may be required to deliver in a certain position.
Pain medications are available during labor and delivery (if the woman chooses); labor may be induced, if necessary; and the fetus is usually electronically monitored throughout the labor. A birth plan can help a woman communicate her preferences about these issues, and doctors will abide by these as much possible.
In response to a push for more “natural” birth events, many hospitals now offer more modern options for low-risk births, often known as family-centered care. These may include private rooms with baths (birthing suites) where women can labor, deliver, and recover in one place without having to be moved.
Although a doctor and medical staff are still present, the rooms are usually set up to create a nurturing environment, with warm, soothing colors and features that try to simulate a home-like atmosphere that can be very comforting for new moms. Rooming in — when the baby stays with the mother most of the time instead of in the infant nursery — also may be available.
In addition, many hospitals offer childbirth and prenatal education classes to prepare parents for the birth experience and parenting classes for after the birth.
The number of people allowed to attend the birth varies from hospital to hospital. In more traditional settings, as many as three support people are permitted to be with the mother during a vaginal birth. In a family-centered approach, more family members, friends, and sometimes even kids might be allowed. During a routine or nonemergency C-section, usually just one support person allowed.
Hospital Births
If you decide to give birth in a hospital, you will see a variety of health professionals:
Obstetrician/gynecologists (OB/GYNs) are doctors with at least 4 additional years of training after medical school in women’s health and reproduction, including both surgical and medical care. They can handle complicated pregnancies and also perform C-sections.
Look for obstetricians who are board-certified, meaning they have passed an examination by the American Board of Obstetrics and Gynecology (ACOG). Board-certified obstetricians who go on to receive further training in high-risk pregnancies are called maternal-fetal specialists or perinatologists.
If you deliver in a hospital, you also might be able to use a certified nurse-midwife (CNM). CNMs are registered nurses who have a graduate degree in midwifery, meaning they’re trained to handle low-risk pregnancies and deliveries. Most CNMs deliver babies in hospitals or birth centers, although some do home births.
In addition to obstetricians and CNMs, registered nurses (RNs) attend births to take care of the mother and baby. If you give birth in a teaching hospital, medical students or residents might be present during the birth. Some family doctors also offer prenatal care and deliver babies.
While you’re in the hospital, if you choose or if it’s necessary for you to receive anesthesia, it will be administered by a trained anesthesiologist. A variety of pain-control measures, including pain medication and local, epidural, and general anesthesia, are available in the hospital setting.
Birth Centers
Women who deliver in a birth center are usually those who have already given birth without any problems and whose current pregnancies are considered low risk (meaning they are in good health and are the least likely to develop complications).
Women giving birth to multiples, who have certain medical conditions (such as gestational diabetes or high blood pressure), or whose baby is in the breech position are considered higher risk and should not deliver in a birth center.
Women are carefully screened early in pregnancy and given prenatal care at the birth center to monitor their health throughout their pregnancy.
Natural childbirth is the focus in a birth center. Since epidural anesthesia usually isn’t offered, women are free to move around in labor, get in the positions most comfortable to them, spend time in the jacuzzi, etc. Comfort measures (such as hydrotherapy, massage, warm and cold compresses, and visualization and relaxation techniques) are often used. The woman is free to eat and drink as she chooses.
A variety of health care professionals operate in the birth center setting. A birth center may employ registered nurses, CNMs, and doulas (professionally trained providers of labor support and/or postpartum care).
Although a doctor is seldom present and medical interventions are rarely done, birth centers may work with a variety of obstetric and pediatric consultants. The professionals affiliated with a birth center work closely together as a team, with the nurse-midwives present and the OB/GYN consultants available if a woman develops a complication during pregnancy or labor that puts her into a higher risk category.
The baby’s heart rate is monitored often during labor, typically with a handheld Doppler device. Birth centers do have medical equipment available, such as IV lines and fluids, oxygen for the mother and the infant, and other equipment necessary to treat sick babies and moms.
A birth center can provide natural pain control and pain control with mild narcotic medications, but if a woman decides she wants an epidural, or if complications develop, she must be taken to a hospital.
Birth centers often provide a homey birth experience for the mother, baby, and extended family. In most cases, birth centers are freestanding buildings, although they may be attached to a hospital. Birth centers may be located in residential areas and generally include amenities such as private rooms with soft lighting, showers, and whirlpool tubs. A kitchen may be available for the family to use.
Look for a birth center that is accredited by the Commission for the Accreditation of Birth Centers (CABC). Some states regulate birth centers, so find out if the birth center you choose has all the proper credentials.
Which One Is Right for You ?
How do you decide whether a hospital or a birth center is the right choice for you? If you’ve chosen a particular health care provider, he or she may only practice at a particular hospital or birth center, so you should discuss your decision. And check with your health insurance carrier to make sure your choice is covered. In many cases, accredited birth centers as well as hospitals are covered by major insurance companies.
If you have any conditions that classify your pregnancy as higher risk (such as being older than 35, carrying multiple fetuses, or having gestational diabetes or high blood pressure, to name a few), your health care provider may advise you to deliver in a hospital where you and your baby can receive medical treatment as necessary. In fact, you might not be eligible to deliver in a birth center because of your risk factors. And if you want interventions such as an epidural or continuous fetal monitoring, a hospital is probably the better choice for you.
For a woman without significant problems in her medical history and whose pregnancy has been classified as low risk, a birth center can be an option. Women who want a natural birth with minimal medical intervention or pain control may feel more comfortable in a birth center, as may those who want friends or family members there for the birthing experience.
Once you’ve decided on either a hospital or a birth center, you may still have to choose which hospital or which birth center. Before you make a choice, be sure that your health care provider — whether he or she is a doctor or a CNM — can deliver at the facilities you’re considering.
Also, try to get a tour of the hospital or birth center so you can see for yourself if the staff is friendly and the atmosphere is one in which you’ll feel relaxed.
Before your labor pains start, get answers to these questions:
If Choosing a Hospital
- Is the hospital easy to get to?
- How is it equipped to handle emergencies?
- What level nursery is available? (Nurseries are rated I, II, or III — a level III neonatal intensive care unit [NICU] is equipped to handle any neonatal emergency. A lower rating may require transportation to a level III NICU.)
- How many deliveries take place at the hospital each year? (A higher number means the hospital has more experience with various birth scenarios.)
- What is the nurse-to-patient ratio? (A ratio of 1:2 is considered good during low-risk labor; a 1:1 ratio is best in complicated cases or during the pushing stage.)
- What are the hospital’s statistics for cesarean sections, episiotomies, and mortality? (Keep in mind, though, that these numbers include high-risk and complicated deliveries.)
- How many labor and support people may be present for the birth?
- What procedures are followed after your baby’s birth? Can you breastfeed immediately if desired? Is rooming in available?
- How long is the typical postpartum stay for vaginal deliveries? For C-sections?
- Can the baby and the father stay with you in your room around the clock, if you desire?
If Choosing a Birth Center
- Is the birth center accredited by the Commission for the Accreditation of Birth Centers?
- Is the birth center easy to get to?
- What situations during labor would lead to a transfer to a hospital? How are transfers handled? What emergencies are the transfer facilities able to handle?
- What professionals (such as midwives, doctors, and nurses) are available on staff? On a consulting basis? Are they licensed?
- What childbirth and prenatal education classes are offered?
- What are the center’s statistics for hospital transfers, episiotomies, and mortality?
- What procedures are followed after your baby’s birth? How long is the typical postpartum stay and how will your baby be examined?
It’s wise to choose where to deliver your baby as early in your pregnancy as possible. That way, if complications do arise, you’ll be well informed and can concentrate on your health and the health of your baby.
What is natural water birth?
A water birth means at least part of your labor, delivery, or both happen while you’re in a birth pool filled with warm water. Water birth can take place in a hospital, a birthing center, or at home. A doctor, nurse-midwife, or midwife helps you through it. If you have any further questions or require additional information please discuss the use of water during labor and/or birth with your midwife or doctor.
The prevalence of water birth in the United States is uncertain because it has not been studied in births outside of the home and birth centers, and the data are not recorded on birth certificates 30. Several professional organizations, including the British Royal College of Obstetricians and Gynaecologists and the American College of Nurse–Midwives, support healthy women with uncomplicated pregnancies laboring and giving birth in water. The United Kingdom’s National Institute for Health and Care Excellence states that women should be informed that there is insufficient high-quality evidence to either support or discourage giving birth in water 31.
You and your baby must fit all of the following criteria to use a bath or pool for your labor and/or birth:
- Be healthy with no complications of pregnancy
- Be having only 1 baby who is presenting head first
- Be at least 37 weeks pregnant
- Not be a carrier of, or infected with, HIV, Hepatitis B or Hepatitis C virus
- Not be excessively overweight
- Not have broken your waters for longer than 18 – 24 hours (unless antibiotics have already been started)
- The color of your broken waters must remain clear
- Your baby’s heart rate must remain within the normal range
- You must not enter water until 4 hours after receiving an injection for pain relief.
Conditions for using water during your labor:
- You must never be alone while immersed in the water.
- The midwife or doctor will advise you about the best time to enter the water, which is when labor is becoming stronger.
- The bath or pool must be filled with only pure tap water with no additives such as:
- bath oils
- gels
- soaps
- salt.
- When sitting in the bath or pool the water should reach the level of your breasts.
- You should feel comfortably warm.
- You can leave the water at any time.
- You must leave the water to urinate.
- You should keep well hydrated throughout labor to avoid dehydration.
- You must leave the water when advised to do so by the midwife and/or doctor.
- You cannot have an injection for pain relief or an epidural when in the water, but it is possible to use gas if desired.
If you choose to birth in water:
- All the conditions for using water during labor must be met at all times.
- You must leave the water if the midwife or doctor is concerned about your wellbeing and safety.
- You must be assisted when you leave the water to avoid any injury to you or your baby.
- Your baby must be brought to the surface as soon as he/she is born and the head must then remain above the water at all times.
- The baby’s umbilical cord must not be cut under water.
- The baby must be kept warm after birth using skin-to-skin contact, drying the head and keeping the rest of the body under water.
- The baby must be removed from the water immediately if he/she needs help to breathe.
- You must leave the water for the delivery of the placenta after the baby is born unless you want to have a natural third stage.
- If you require stitches this procedure will be delayed for at least 1 hour after you leave the water.
Natural water birth key points:
- Water immersion in a bath or a pool during the first stage of labor has been shown to decrease the need for pain relieving drugs 32 and make the experience more enjoyable for women.
- There are strict guidelines for keeping the water clean during labor.
- Waterbirths are associated with low-risks for both the woman and baby when care is provided by midwives and/or doctors who follow best practice guidelines.
- You must never be alone while immersed in the water.
Exploring your choices:
- Firstly find out if your maternity service offers the option of immersion in water for labor and/or birth.
- Write down what you would like in your birth plan.
- Talk to a midwife and/or doctor to find out more information, in particular:
- whether there are any reasons why immersion in water is not advisable for you – the benefits and risks to you and your baby
- details about when you would be required to leave the water.
- You will be asked to sign an agreement form if you choose to use water for your labor and/or birth.
Common concerns about using water for labor and/or birth
- You and your baby may get too hot: If your body overheats your baby may also get too hot and this can cause the baby’s heart rate to increase. You should feel comfortable in the water but not too hot. Your midwife will check the water temperature regularly while you are in the water during labor and/or birth.
- Your baby may develop an infection: There are strict guidelines for keeping the water clean during your labor and for cleaning the bath or pool to minimize the possibility of infection.
- Your baby may inhale water: If you choose to stay in the water to birth, your baby should be born under the water, then gently but immediately lifted out into the air. Your baby’s head should then be kept above the water so that breathing can start and potential inhalation of water can be prevented.
American College of Obstetricians and Gynecologists Recommendations
The American College of Obstetricians and Gynecologists makes the following recommendations 33:
- Immersion in water during the first stage of labor may be associated with shorter labor and decreased use of spinal and epidural analgesia and may be offered to healthy women with uncomplicated pregnancies between 37 weeks and 41 weeks of gestation.
- There are insufficient data on which to draw conclusions regarding the relative benefits and risks of immersion in water during the second stage of labor and delivery. Therefore, until such data are available, it is the recommendation of the College that birth occur on land, not in water.
- A woman who requests to give birth while submerged in water should be informed that the maternal and perinatal benefits and risks of this choice have not been studied sufficiently to either support or discourage her request. She also should be informed of the rare but serious neonatal complications associated with this choice.
- The opinions expressed in this document should not be interpreted in such a manner as to prevent the conduct of well-designed prospective studies of the maternal and perinatal benefits and risks associated with immersion during labor and delivery.
- Facilities that plan to offer immersion during labor and delivery need to establish rigorous protocols for candidate selection; maintenance and cleaning of tubs and pools; infection control procedures, including standard precautions and personal protective equipment for health care personnel; monitoring of women and fetuses at appropriate intervals while immersed; and moving women from tubs if urgent maternal or fetal concerns or complications develop.
What is Cesarean Section (C-Section)?
Every pregnant woman hopes for a short labor and delivery with no complications — manageable contractions, some pushing, then a beautiful baby.
But it doesn’t always work out that way. Some babies need to be delivered via cesarean section (C-section).
Even if you’re hoping for a traditional vaginal birth, it may help to ease some fears to learn why and how C-sections are performed, just in case everything doesn’t go as planned.
What Is a C-Section ?
A C-section is the surgical delivery of a baby that involves making incisions in the mother’s abdominal wall and uterus. Generally considered safe, C-sections do have more risks than vaginal births. Plus, moms can go home sooner and recover quicker after a vaginal delivery.
But C-sections can help women who are at risk for complications avoid dangerous delivery-room situations and can be a lifesaver in an emergency.
C-sections are done by obstetricians (doctors who care for pregnant women before, during, and after birth) and some family physicians. Although more and more women are choosing midwives to deliver their babies, midwives of any licensing degree cannot perform C-sections.
Why Are C-Sections Needed ?
Scheduled C-Sections
Some C-sections are scheduled if the doctor knows that a vaginal birth would be risky. A doctor may schedule one if:
- the baby is in breech (feet- or bottom-first) or transverse (sideways) position in the womb (although some babies can be turned before labor begins or delivered vaginally using special techniques)
- the baby has certain birth defects (such as severe hydrocephalus)
- the mother has problems with the placenta, such as placenta previa (when the placenta sits too low in the uterus and covers the cervix)
the mother has a medical condition that could make a vaginal delivery risky for herself or the baby (such as HIV or an active case of genital herpes)
some multiple pregnancies
- the mother previously had surgery on her uterus or an earlier C-section (although many such women can safely have a vaginal birth after a C-section, called a VBAC)
Emergency C-Sections
Some C-sections are unexpected emergency deliveries done when complications arise with the mother and/or baby during pregnancy or labor. An emergency C-section might be done if:
- labor stops or isn’t progressing as it should (and medicines aren’t helping)
- the placenta separates from the uterine wall too soon (called placental abruption)
- the umbilical cord becomes pinched (which could affect the baby’s oxygen supply) or enters the birth canal before the baby (called umbilical cord prolapse)
- the baby is in fetal distress — certain changes in the baby’s heart rate may mean that the baby is not getting enough oxygen
- the baby’s head or entire body is too big to fit through the birth canal
Of course, each woman’s pregnancy and delivery is different. If your doctor has recommended a C-section and it’s not an emergency, you can ask for a second opinion. In the end, you most often need to rely on the judgment of the doctors.
How Is a C-Section Done ?
Here’s a quick look at what usually happens during a scheduled C-section.
Your labor coach, wearing a surgical mask and gown, can be right by your side during the entire delivery (although partners might not be allowed to stay during emergency C-sections). Before the procedure begins, an anesthesiologist will discuss what will be done so that you don’t feel pain during the C-section.
To prepare for the delivery, you’ll probably have:
- various monitors in place to keep an eye on your heart rate, breathing, and blood pressure
- your mouth and nose covered with an oxygen mask or a tube placed in your nostrils to give you oxygen
- a catheter (a thin tube) inserted into your bladder through your urethra (which may be uncomfortable when it’s placed, but should not be painful)
- an IV in your arm or hand
- your belly washed and any hair between the bellybutton and pubic bone shaved
- a privacy screen put around your belly
After anesthesia is given, the doctor makes an incision on the skin of the abdomen — usually horizontally (1–2 inches above the pubic hairline, sometimes called “the bikini cut”).
The doctor then gently parts the abdominal muscles to get to the uterus, where he or she will make another incision in the uterus itself. This incision can be vertical or horizontal. Doctors usually use a horizontal incision in the uterus, also called transverse, which heals better and makes a VBAC much more possible.
After the uterine incision is made, the baby is gently pulled out. The doctor suctions the baby’s mouth and nose, then clamps and cuts the umbilical cord. As with a vaginal birth, you should be able to see your baby right away. Then, the little one is handed over to the nurse or doctor who will be taking care of your newborn for a few minutes (or longer, if there are concerns).
The obstetrician then removes the placenta from the uterus, closes the uterus with dissolvable stitches, and closes the abdominal incision with stitches or surgical staples that are usually removed, painlessly, a few days later.
If the baby is doing OK, you can hold and/or nurse your newborn in the recovery room. You may need help holding the baby on the breast if you have to stay lying down flat.
Will I Feel Anything ?
You won’t feel any pain during the C-section, although you may feel sensations like pulling and pressure. Most women are awake and simply numbed from the waist down using regional anesthesia (an epidural and/or a spinal block) during a C-section.
That way, they are awake to see and hear their baby being born. A curtain will be over your abdomen during the surgery, but you may be able to take a peek as your baby is being delivered from your belly.
Sometimes, a woman who needs an emergency C-section might require general anesthesia, so she’ll be unconscious (or “asleep”) during the delivery and won’t remember anything or feel any pain.
What Are the Risks of a C-section ?
C-sections today are, in general, safe for both mother and baby. However, there are risks with any kind of surgery. Potential C-section risks include:
- increased bleeding (that could, though rarely, require a blood transfusion)
- infection (antibiotics are usually given to help prevent this)
- bladder or bowel injury
- reactions to medicines
- blood clots
- death (very rare)
- possible injury to the baby
Some of the regional anesthetic used during a C-section does reach the baby, but it’s much less than what the newborn would get if the mother had general anesthesia (which sedates the baby as well as the mother).
Babies born by C-section sometimes have breathing problems (transient tachypnea of the newborn) because labor hasn’t jump-started the clearance of fluid from their lungs. This usually gets better on its own within the first day or two of life.
Having a C-section may — or may not — affect future pregnancies and deliveries. Many women can have a successful and safe vaginal birth after cesarean. But in some cases, future births may have to be C-sections, especially if the incision on the uterus was vertical rather than horizontal. A C-section can also put a woman at increased risk of possible problems with the placenta in future pregnancies.
- In the case of emergency C-sections, the benefits usually far outweigh the risks. A C-section could be lifesaving.
What Is the Recovery Like After a C-section ?
As with any surgery, there’s usually some degree of pain and discomfort after a C-section. The recovery period is also a little longer than for vaginal births. Women who’ve had C-sections usually stay in the hospital for about 3 or 4 days.
Right after, you may feel itchy, sick to your stomach, and sore — these are all normal reactions to the anesthesia and surgery. If you needed general anesthesia for an emergency C-section, you may feel groggy, confused, chilly, scared, alarmed, or even sad. Your health care provider can give you medicines to ease any discomfort or pain.
For the first few days and even weeks, you might:
- feel tired
- have soreness around the incision (the doctor can prescribe medicines and/or recommend over-the-counter pain relievers that are safe to take if you’re breastfeeding)
- be constipated and gassy
- have a hard time getting around and/or lifting your baby
It can help if you support your abdomen near the incision when you sneeze, cough, or laugh. These sudden movements can be painful. You’ll need to avoid driving or lifting anything heavy so that you don’t put any unnecessary pressure on your incision.
Check with your health care provider about when you can get back to your normal activities (typically after about 6 to 8 weeks, when the uterus has healed). As with a vaginal delivery, you shouldn’t have sex until your doctor has given you the go-ahead, usually about 6 weeks after delivery.
Frequent and early walking may help ease some post-cesarean pains and discomfort. It also can help prevent blood clots and keep your bowels moving. But don’t push yourself — take it easy and have someone help you get around, especially up and down stairs. Let friends, family, and neighbors lend a helping hand with meals and housework for a while, especially if you have other children.
Although breastfeeding might be a little painful at first, lying on your side to nurse or using the clutch (or football) hold can take the pressure off your abdomen. Drink plenty of water to help with your milk supply and to help avoid constipation.
C-sections scars fade over time. They’ll get smaller and become a natural skin color in the weeks and months after delivery. And because incisions are often made in the “bikini” area, many C-section scars aren’t even noticeable.
What If I Don’t Feel Better ?
See your health care provider if you have:
- a fever
- signs of infection around your incision (swelling, redness, warmth, or pus)
- pain around your incision or in your abdomen that comes on suddenly or gets worse
- foul-smelling vaginal discharge
- pain when peeing
- trouble pooping
- heavy vaginal bleeding
- leg pains, or swelling or redness of your legs
- trouble breathing or chest pain
- pain in one or both breasts
- feelings of depression
- thoughts of hurting yourself or your baby
Emotionally, you may feel a little disappointed if you’d been hoping for a vaginal birth or had gone through labor that ended in a C-section. Remember that having a C-section does not make the birth of your baby any less special or your efforts any less amazing. After all, you went through major surgery to deliver your baby!
- What is natural childbirth? https://www.nichd.nih.gov/health/topics/labor-delivery/topicinfo/Pages/natural-childbirth.aspx[↩]
- Tournaire, M., & Theau-Yonneau, A. (2007). Complementary and alternative approaches to pain relief during labor. Evidence-Based Complementary and Alternative Medicine, 4(4), 409–417. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2176140/[↩]
- https://www.marchofdimes.org/pregnancy/stages-of-labor.aspx[↩]
- https://www.marchofdimes.org/materials/birth-plan.pdf[↩][↩]
- Lothian JA. Safe, Healthy Birth: What Every Pregnant Woman Needs to Know. The Journal of Perinatal Education. 2009;18(3):48-54. doi:10.1624/105812409X461225. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2730905/[↩]
- Early skin-to-skin contact for mothers and their healthy newborn infants. Moore ER, Anderson GC, Bergman N. Cochrane Database Syst Rev. 2007 Jul 18; (3):CD003519. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003519.pub2/full[↩]
- Assessing effective care in normal labor: the Bologna score. Chalmers B, Porter R. Birth. 2001 Jun; 28(2):79-83. https://www.ncbi.nlm.nih.gov/pubmed/11380378/[↩]
- Step 10: Strives to Achieve the WHO/UNICEF Ten Steps of the Baby-Friendly Hospital Initiative to Promote Successful Breastfeeding: The Coalition for Improving Maternity Services. J Perinat Educ. 2007 Winter; 16 Suppl 1():79S-80S. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2409135/[↩]
- Promoting, protecting, and supporting normal birth: a look at the evidence. Romano AM, Lothian JA. J Obstet Gynecol Neonatal Nurs. 2008 Jan-Feb; 37(1):94-104; quiz 104-5. https://www.ncbi.nlm.nih.gov/pubmed/18226163/[↩]
- The journey of becoming a mother. Lothian JA. J Perinat Educ. 2008 Fall; 17(4):43-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2582416/[↩]
- http://www.lamaze.org/[↩]
- Childbirth Connection. http://www.childbirthconnection.org/[↩]
- Coalition for Improving Maternity Services. http://www.motherfriendly.org/[↩]
- Choices in Childbirth. http://choicesinchildbirth.org/[↩]
- Amis D. Healthy Birth Practice #1: Let Labor Begin on Its Own. The Journal of Perinatal Education. 2014;23(4):178-187. doi:10.1891/1058-1243.23.4.178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235056/[↩]
- Neonatal outcomes after elective cesarean delivery. Kamath BD, Todd JK, Glazner JE, Lezotte D, Lynch AM. Obstet Gynecol. 2009 Jun; 113(6):1231-8.[↩]
- Step 6: does not routinely employ practices, procedures unsupported by scientific evidence: the coalition for improving maternity services: Goer H, Sagady Leslie M, Romano A . J Perinat Educ. 2007 Winter; 16 Suppl 1():32S-64S.[↩][↩]
- Expectant management versus labor induction for suspected fetal macrosomia: a systematic review. Sanchez-Ramos L, Bernstein S, Kaunitz AM. Obstet Gynecol. 2002 Nov; 100(5 Pt 1):997-1002.[↩]
- Ondeck M. Healthy Birth Practice #2: Walk, Move Around, and Change Positions Throughout Labor. The Journal of Perinatal Education. 2014;23(4):188-193. doi:10.1891/1058-1243.23.4.188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235058/[↩]
- Step 4: provides the birthing woman with freedom of movement to walk, move, assume positions of her choice: the coalition for improving maternity services: Storton S. J Perinat Educ. 2007 Winter; 16 Suppl 1():25S-7S. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2409125/[↩]
- Green J, Hotelling BA. Healthy Birth Practice #3: Bring a Loved One, Friend, or Doula for Continuous Support. The Journal of Perinatal Education. 2014;23(4):194-197. doi:10.1891/1058-1243.23.4.194. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235055/[↩]
- Step 1: offers all birthing mothers unrestricted access to birth companions, labor support, professional midwifery care: the coalition for improving maternity services:. Leslie MS, Storton S. J Perinat Educ. 2007 Winter; 16 Suppl 1():10S-9S. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2409134/[↩]
- Lothian JA. Washington, DC: Lamaze International; 2009. Healthy birth practice #4: Avoid interventions that are not medically necessary.[↩]
- Step 6: does not routinely employ practices, procedures unsupported by scientific evidence: the coalition for improving maternity services:. Goer H, Sagady Leslie M, Romano A. J Perinat Educ. 2007 Winter; 16 Suppl 1():32S-64S. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2409136/[↩][↩][↩]
- DiFranco J, Romano AM, Keen R. Washington, DC: Lamaze International; 2009. Healthy birth practice #5: Avoid giving birth on the back, and follow the body’s urges to push.[↩]
- Gupta JK, Sood A, Hofmeyr GJ, Vogel JP. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database of Systematic Reviews 2017, Issue 5. Art. No.: CD002006. DOI: 10.1002/14651858.CD002006.pub4. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002006.pub4/full[↩][↩][↩]
- A randomized trial of the effects of coached vs uncoached maternal pushing during the second stage of labor on postpartum pelvic floor structure and function. Schaffer JI, Bloom SL, Casey BM, McIntire DD, Nihira MA, Leveno KJ. Am J Obstet Gynecol. 2005 May; 192(5):1692-6. https://www.ncbi.nlm.nih.gov/pubmed/15902179/[↩]
- Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No.: CD003519. DOI: 10.1002/14651858.CD003519.pub4. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003519.pub4/full[↩]
- Enkin M, Keirse M, Neilson J, Crowther C, Duley L, Hodnett E, et al. New York: Oxford University Press; 2000. A guide to effective care in pregnancy and childbirth.[↩]
- Bovbjerg ML, Cheyney M, Everson C. Maternal and Newborn Outcomes Following Waterbirth: The Midwives Alliance of North America Statistics Project, 2004 to 2009 Cohort. J Midwifery Womens Health. 2016 Jan-Feb;61(1):11-20. doi: 10.1111/jmwh.12394[↩]
- Intrapartum care for healthy women and babies. https://www.nice.org.uk/guidance/cg190/chapter/Recommendations#first-stage-of-labour[↩]
- Cluett, E. R., Burns, E., & Cuthbert, A. (2018). Immersion in water during labour and birth. The Cochrane database of systematic reviews, 5(5), CD000111. https://doi.org/10.1002/14651858.CD000111.pub4[↩]
- Immersion in Water During Labor and Delivery. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2016/11/immersion-in-water-during-labor-and-delivery[↩]