What is notalgia paresthesia
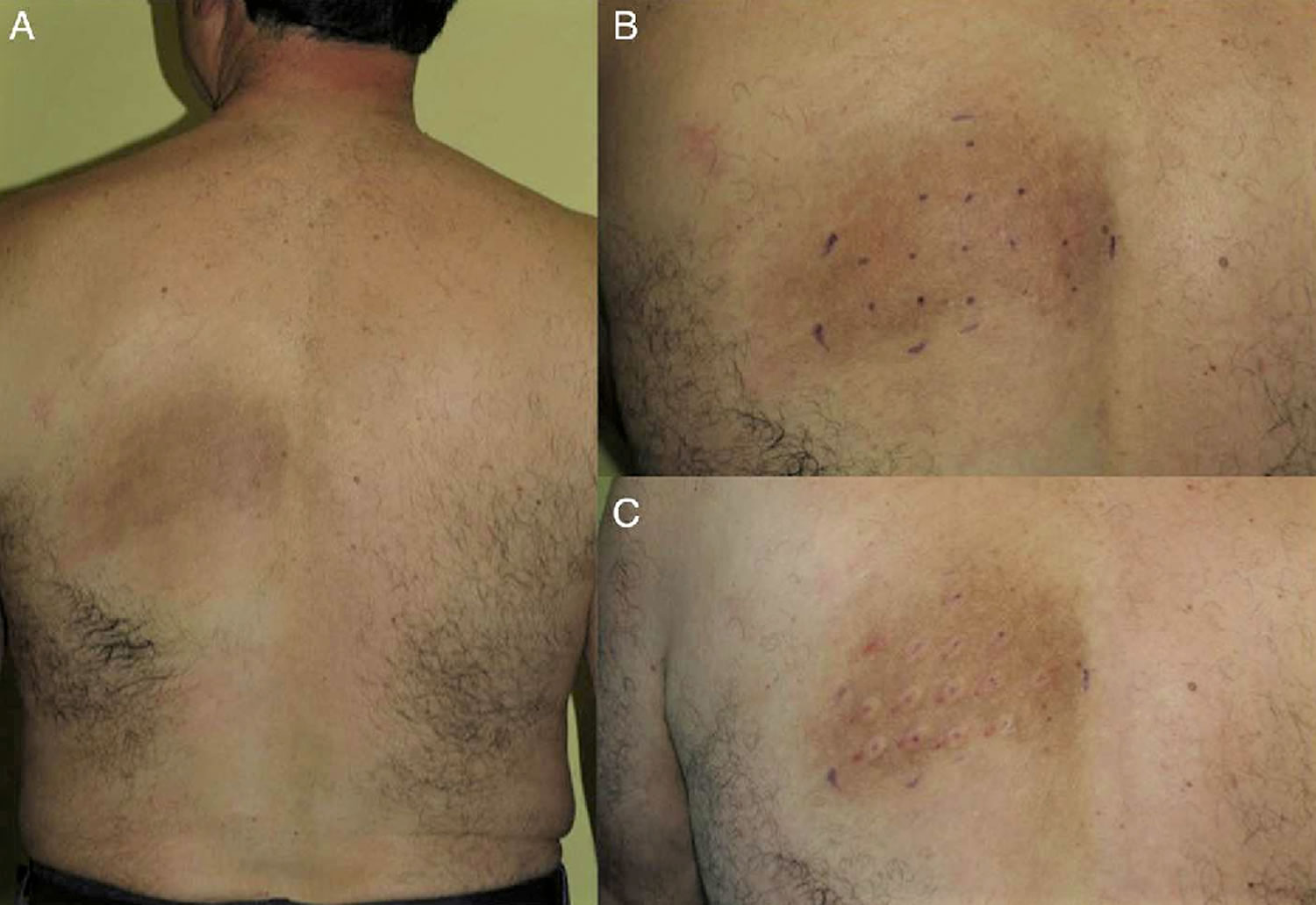
Notalgia paresthetica is a common chronic neurosensory syndrome characterized by localized itch (pruritus), that usually affects patches of skin on the upper back. Occasionally it can be more widespread and involve other parts of the back, the shoulders and upper chest. People feel both the sensation of an itch and paresthesia (a sensation of tingling, pricking, burning, coldness, hypoesthesia, increased pain, or numbness of the skin) 1. The involved skin except is usually hyperpigmented (darker patch of skin on the itchy area) and is associated with chronic scratching and rubbing. Amyloid deposits (a collection of a specific type of protein) may be found in skin biopsies, but this is thought to be a secondary event. The cause of the itch in notalgia paresthetica may be due to the compression of spinal nerves by bones or muscles as the nerves emerge through the vertebrae to the back muscles. In the affected area, the number of nerve fibers may be increased and the cutaneous sensory nerves are altered secondary to localized impingement, central injury, or both 2, 3. Sometimes degenerative changes in the area of the vertebrae that innervate the affected back muscles can be seen, but not always.
Chronic itch (pruritus) is a broad category with multiple causes and a lifetime incidence of over 20%. Notalgia paresthetica falls in the subcategory of a chronic neuropathic pruritus, a subcategory which is thought to constitute approximately 8% of all cases of chronic pruritus. Notalgia paresthetica does not have a racial predilection for other pruritic neuropathic syndromes such as brachioradial pruritus, which favors those with lighter skin tones. Notalgia paresthetica is typically unilateral disease, often present on the contralateral side of the dominant hand. The majority of the population is right hand dominant. Therefore a left-sided parascapular pruritus that is reachable by the dominant hand is highly suggestive of notalgia paresthetica. Notalgia paresthetica can affect people of any age, of any race, and of either sex. However, it is thought to be most common in middle-aged to older adults. Women seem to develop notalgia paresthetica more frequently than men, but small study sizes may be misleading.
Although multiple therapeutic approaches for notalgia paresthetica have been described, none specifically address the essential pathogenesis of the condition—the altered cutaneous nerves 1. Symptoms of notalgia paresthetica may respond to topical capsaicin treatment 4. Cryolipolysis is a well-tolerated nonsurgical technique to reduce the subcutaneous fat layer. Selective apoptosis of adipocytes occurs since the lipid-rich fat cells are more susceptible to cold injury than the surrounding water-rich cells. Not only a marked decrease in pain sensitivity but also a sustained reduction in the density of myelinated and unmyelinated cutaneous nerves has been observed in cryolipolysis-treated skin. Therefore, cryolipolysis is a logical approach to the treatment of notalgia paresthetica. One or more cryolipolysis treatments may be necessary for complete or partial resolution of the individual’s notalgia paresthetica-related cutaneous symptoms.
If you do have a diagnosis of notalgia paresthetica, your doctor may try the following:
- Prescription-strength anesthetic cream
- Prescription-strength corticosteroid (cortisone) cream
If the itching or pain becomes intolerable or interferes with your activities, your doctor may prescribe an oral anti-seizure (anti-epileptic or anti-convulsant) medication, such as:
- Gabapentin
- Topiramate
- Oxcarbazepine
If these approaches are not effective, and if your symptoms are severe enough to justify it, more aggressive procedures may be performed to relieve pressure on the compressed nerve:
- Injection of local anesthetic near the compressed nerves as they exit the spine (paravertebral block)
- Spine surgery
Notalgia paresthetica causes
The cause of notalgia paresthetica has not been completely explained. Most authors agree notalgia paresthetica is a neuropathy, but whether it is radicular or peripheral is unknown 5. Some studies have demonstrated spine disease in the spinal bone (vertebra) at the level of the affected skin. Scientists speculate that spine disease due to age or injury may press on a nerve providing feeling to that area of the skin, which leads to itching.
Many reports state a polyradiculopathy of thoracic nerves 2 to 6 as the primary cause due to suggestive radiographic findings in some patients with notalgia paresthetica. Numerous causes of unilateral thoracic nerve impingement have been reported with the most common being degenerative vertebral changes and herniated intravertebral discs. Other causes include osteoarthritic lesions with resulting kyphosis and vertebral hyperostosis. Professionals who criticize the radiculopathy theory state that a radiculopathy would result in symptoms with a dermatomal pattern not just in an isolated area which is seen in notalgia paresthetica.
Peripheral causes of notalgia paresthetica are more numerous and can be divided into physical, anatomical, metabolic, genetic, and infectious. Physical causes include muscle spasms, which are thought to compress cutaneous itch sensitive nerves resulting in aberrant afferent firing. Some authors attribute the anatomical angle the peripheral histamine-sensitive nerves pierce the multifidus spinae muscles. This angle is thought to predispose them to irritation by normal muscular contraction and muscle spasms. Physical therapy to alter the tone of the paraspinal muscles is thought to change the angle leading to a reduction in nerve irritation, and therefore pruritus. Other less common causes include metabolic disorders, such as type-2 diabetes, genetic causes like MEN2A, and infectious causes such as herpes zoster.
Notalgia paresthetica pathophysiology
The sensation of itch is thought to be a complex process involving sensitive neurons and adjacent cellular mechanisms that modulate the sensation of itch. Dysregulation of this process leads to aberrant firing of itch-transmitting nerve fibers without a typical itch-provoking physical stimulus, a disorder known as alloknesis. Itch is thought to be transmitted along at least two different types of nerve fibers. Small unmyelinated histamine-sensitive nerve fibers, known as C-fibers, are thought to be the primary transmitters of itch. Other nerve fibers are thought to transmit both itch and pain. The second bifunctional nerve fiber may explain why some patients with notalgia paresthetica experience other sensations such as paresthesias and allodynia in addition to pruritus. Additionally, itch-sensitive fibers may have closely coupled thermoreceptors, which may provide a link to why heat exacerbates pruritus. Notalgia paresthetica is most likely a multifactorial process involving a combination of physical nerve irritation and a dysregulated itch control mechanism 6.
Notalgia paresthetica symptoms
The most common location for notalgia paresthetica is the upper back, especially between the shoulder blades. The area may be confined to only one side of the upper back, or it may occur in the middle of the upper back, over the spinal bones.
Notalgia paresthetica often occurs without any obvious changes to the skin. If skin changes do occur, there may be a well-defined patch of darker skin (hyperpigmentation) over the affected area.
Although periodic itching is the main symptom associated with notalgia paresthetica, some people notice pain, tingling, or a change in feeling (sensation) in the affected skin.
Notalgia paresthetica diagnosis
Your doctor may be able to diagnose notalgia paresthetica by taking your history and examining your skin. In addition, your doctor might order an X-ray or another type of radiologic study, such as an MRI or a CT scan. Although imaging tests have traditionally not been a part of the workup of notalgia paresthetica, basic cervical and possibly thoracic radiographs or MRI may be warranted in the initial management of the disorder. Imaging studies may be particularly helpful in patients with contributory spine symptoms of pain, tenderness, spasm, or decreased range of motion and any history of spinal trauma or injury 7.
Skin biopsy and tissue histology are usually not indicated for the diagnosis of notalgia paresthetica. Biopsies may be performed to exclude other diagnoses and neoplasms. No criteria for tissue diagnosis of notalgia paresthetica are described, but some believe the macular amyloidosis of the mid back is part of the spectrum of notalgia paresthetica. Published studies have shown various histologic findings, including, postinflammatory hyperpigmentation and localized amyloid 8.
Notalgia paresthetica treatment
There is no current treatment for notalgia paresthetica that is consistently effective. Evaluation and treatment of notalgia paresthetica will often involve a multidisciplinary team of specialists. There are a wide variety of treatment options for notalgia paresthetica. First-line therapy for notalgia paresthetica will usually include treatment of the underlying spinal disease by orthopedic surgeons or physical therapists. Topical therapies may include steroid creams, tacrolimus, or capsaicin. Additional therapies have included botulinum toxin injections, gabapentin, physical therapy, nerve blocks, and transcutaneous electrical nerve stimulation (TENS). Some have suggested that a combination of approaches, such as medication along with muscular rehabilitation exercises, may work best 9.
The most common method of treatment for notalgia paresthetica is an oral agent 5. Oral medications that target gamma-amino-butyric acid (GABA), serotonin, histamine, and inflammation have been investigated. Gabapentin, which targets GABA, has been reported to be the most efficacious medication in the reduction of pruritus. Patients with notalgia paresthetica treated with gabapentin may report mild gastric discomfort, but this usually does not result in discontinuation of the medication. Anti-histamine medications surprisingly do not provide a significant relief of pruritus; however, the sedative effects of first-generation anti-histamines may help reduce paroxysmal nocturnal or distracted scratching. Oral medications that target serotonin and inflammation are less effective.
Topical medications include capsaicin, steroids, anesthetics, amitriptyline/ketamine, and doxepin. Capsaicin is the most commonly reported topical medication and can be applied as a cream, gel, lotion, solution, and patch in a wide variety of concentrations. Topical capsaicin can provide immediate relief, but the duration of action varies considerably. Additionally, patients may experience a burning sensation with topical capsaicin use. In a small study, capsaicin was found to be less effective than gabapentin in the treatment of notalgia paresthetica. Topical steroids vary in effectiveness and are not useful unless inflammation is present. Anesthetics provided temporary relief and are not widely used. Amitriptyline/ketamine and doxepin are also not widely used.
Like all other treatments in notalgia paresthetica, Botulinum toxin A has varying reports of success. Early reports suggest Botulinum toxin was a viable option with significant improvement in patient’s reported itch. Later studies attempted to replicate these findings, but little to no improvement was reported.
Treatment with TENS was reported to be successful in a Turkish study of notalgia paresthetica. TENS units are usually used in the treatment of neuropathic pain. One afferent itch pathway is postulated to transmit both itch and pain, which is the most likely target of TENS. In a small study using TENS for 20 minutes five times a week resulted in a 60% reduction of itch in one0thirdof patients. In the same study one-fifth of the patients treated with TENS reported no change and one reported worsening of their pruritus while using TENS. Because notalgia paresthetica can present with other neuropathic symptoms such as pain, tingling, and numbness in addition to itch, TENS may be a particularly effective treatment for patients experiencing multiple neuropathic sensations.
Physical therapy specifically targeted at strengthening upper paraspinal muscles and stretching pectoral muscles has been reported effective in a few cases. This approach may be especially useful in patients with atrophied paraspinal muscles or a shoulder with a reduced range of motion. These strengthening and stretching exercises decrease the angle at which cutaneous nerves pierce the paraspinal muscles resulting in a reduction of irritation and then pruritus.
Notalgia paresthetica home remedies
Dry skin (xerosis) is a common cause of itching, so it helps to apply a moisturizer to the itchy area at least twice a day.
If moisturizers are not helpful, try an over-the-counter cream containing an extract of hot peppers, called capsaicin, and follow the package directions carefully. You will probably not get immediate relief, and the capsaicin cream may take up to 6 weeks to have its full effect. If the capsaicin cream is effective, symptoms will likely come back after you stop using the cream.
If moisturizers and capsaicin cream are not helpful, see your doctor for an evaluation.
Notalgia paresthetica prognosis
Notalgia paresthetica tends to be a chronic disease with periodic remissions and exacerbations 10. The prognosis for control of the symptoms is good, although the condition has a natural tendency to wax and wane. Notalgia paresthetica generally is not entirely curable, although it is certainly controllable and complete remissions are possible.
While not life threatening, the cutaneous symptoms of notalgia paresthetica frequently decrease quality of life, causing much discomfort and nuisance to the affected patients. In some cases, notalgia paresthetica may become disabling and result in many secondary manifestations of cutaneous disease such as secondary skin infections, prurigo nodules, and lichen simplex.
Some increased morbidity may occur because of the possible underlying cervical and thoracic spine and disk disease. Notalgia paresthetica tends to be a chronic condition with periodic remissions and exacerbations. No increase in mortality is described for notalgia paresthetica.
Although notalgia paresthetica has not generally been described in association with other nonspine comorbidities, Alai et al have described case reports of notalgia paresthetica occurring in patients with conditions such as atopic dermatitis, elevated IgE, hepatitis C, chronic renal insufficiency, and hypereosinophilia. The exact relationship and causation remains to be elucidated.
References- Cohen PR. Notalgia Paresthetica: A Novel Approach to Treatment with Cryolipolysis. Cureus. 2017;9(9):e1719. Published 2017 Sep 28. doi:10.7759/cureus.1719 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5705169
- Neurocutaneous disease neurocutaneous dysesthesias. Shumway NK, Cole E, Fernandez KH. J Am Acad Dermatol. 2016;74:215–228.
- Notalgia paresthetica, a clinical series and review. Chiriac A, Podoleanu C, Moldovan C, et al. Pain Pract. 2016;16:90–91.
- Greaves, Malcom W. Pathophysiology and Clinical Aspects of Pruritus. In: Freedberg, Irwin, et.al.. Fitzpatrick’s Dermatology in General Medicine, 6th Edition. United States: McGraw-Hill; 2003; 1:398.
- Robbins BA, Ferrer-Bruker SJ. Notalgia Paresthetica. [Updated 2019 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470597
- Howard M, Sahhar L, Andrews F, Bergman R, Gin D. Notalgia paresthetica: a review for dermatologists. Int. J. Dermatol. 2018 Apr;57(4):388-392.
- Savk O, Savk E. Investigation of spinal pathology in notalgia paresthetica. J Am Acad Dermatol. 2005 Jun. 52(6):1085-7.
- Weber PJ, Poulos EG. Notalgia paresthetica. Case reports and histologic appraisal. J Am Acad Dermatol. 1988 Jan. 18(1 Pt 1):25-30.
- Howard M, Sahhar L, Andrews F, Bergman R, and Gin D. Notalgia paresthetica: a review for dermatologists. Int J Dermatol. April, 2018; 57(4):388-392. https://www.ncbi.nlm.nih.gov/pubmed/29243804
- Notalgia paresthetica. https://emedicine.medscape.com/article/1599159-overview