Obliterative bronchiolitis
Obliterative bronchiolitis also known as bronchiolitis obliterans or constrictive bronchiolitis, is a type of bronchiolitis and refers to bronchiolar inflammation with submucosal peribronchial fibrosis associated with luminal stenosis and occlusions 1. Obliterative bronchiolitis is a type of obstructive lung disease of the small airways 2. Obliterative bronchiolitis is a rare disease with characteristic features of fibrosis of terminal and distal bronchioles and spirometry showing airflow obstruction. It usually leads to progressive decline in lung function and has variable outcomes 3. Obliterative bronchiolitis should not be confused with bronchiolitis obliterans organizing pneumonia (BOOP), which is a completely different disease and is now referred to as cryptogenic organizing pneumonia (COP) 4. Breathing in harmful substances is the main cause of developing obliterative bronchiolitis. In addition, obliterative bronchiolitis is an obstructive process targeted at terminal bronchioles and rarely associated with infiltrates, cryptogenic-organizing pneumonia (COP) is generally a restrictive process targeted at alveoli and is almost always associated with alveolar infiltrates.
The very small airways of the lungs are called bronchioles. Bronchioles can become injured as a result of inhaling a harmful substance or due to an infection. Most of the time, the injury heals normally. Occasionally the cellular repair process goes into overdrive, causing the build-up of scar tissue. The thick scar tissue blocks the bronchioles and prevents air from passing through to the alveoli, or air sacs. This impairs the body’s ability to absorb oxygen. The scarring and narrowing of the bronchioles may continue to worsen over time, eventually resulting in respiratory failure.
Obliterative bronchiolitis was first discovered in workers at a microwave popcorn plant who had inhaled the flavoring chemical diacetyl. Thus, the obliterative bronchiolitis became known as ‘popcorn lung’. Obliterative bronchiolitis is not restricted to butter flavor and popcorn workers. Diacetyl is used to make many other flavors, including fruit and candy flavors, and workers in other industries who inhaled diacetyl have also been diagnosed with obliterative bronchiolitis.
When obliterative bronchiolitis occurs after lung transplantation or allogenic bone marrow transplantation (donor hematopoietic stem cell transplantation) it is called bronchiolitis obliterans syndrome 5.
Several risk factors can lead to the development of obliterative bronchiolitis. Obliterative bronchiolitis is one of the most common noninfectious complications after lung transplant and hematopoietic stem cell transplantation. Other causes of obliterative bronchiolitis include exposure to inhaled toxins and gases including sulfur mustard gas, nitrogen oxides, diacetyl (used as popcorn flavoring), fly ash and fiberglass. Bronchiolitis obliterans is also associated with autoimmune disorders, especially rheumatoid arthritis, systemic lupus erythematosus (SLE or lupus) and less commonly with inflammatory bowel disease. Obliterative bronchiolitis is also known to occur after a respiratory viral infection (adenovirus, respiratory syncytial virus [RSV]), especially in children. Other infections associated with obliterative bronchiolitis are HIV, Postinfectious (mycoplasma, bacteria, fungi) and Human Herpes Virus (HHV) 8 3. Rare conditions like Castleman disease and paraneoplastic pemphigus have also been associated with obliterative bronchiolitis. Other associations include microcarcinoid tumorlets and cryptogenic constrictive bronchiolitis 3.
The symptoms of patients with obliterative bronchiolitis is characterized by progressive shortness of breath (dyspnea) and nonproductive cough over a period of weeks to months and abnormal pulmonary function that is frequently characterized by an obstructive airflow pattern 6. Computed tomography (CT) performed on expiration shows air trapping.
Obliterative bronchiolitis is characterized by concentric luminal narrowing of the membranous and respiratory bronchioles as a result of submucosal and peribronchiolar inflammation and fibrosis without any intraluminal granulation tissue or polyps/polyposis. There is an absence of diffuse parenchymal inflammation.
Figure 1. Healthy bronchioles and alveoli
Footnote: Panel C shows a normal bronchiole connecting to an alveolus. Panel D shows a cross section of a normal bronchiole, and Panel E shows a cross section of a bronchiole affected by obliterative bronchiolitis.
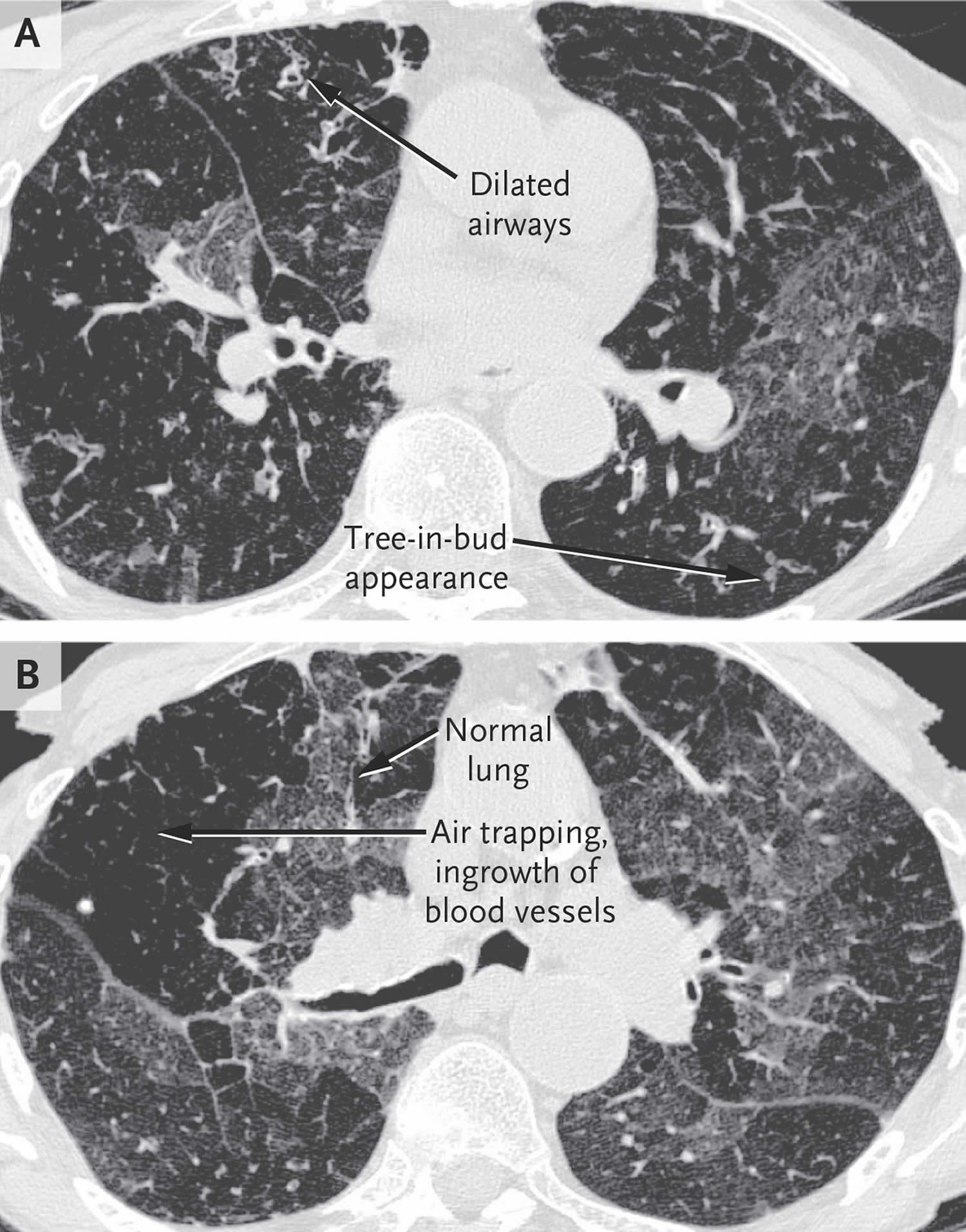
Figure 2. Obliterative bronchiolitis (advanced obliterative bronchiolitis)
Footnote: High-Resolution Computed Tomographic (HRCT) images of the lung from a patient with Graft-versus-Host Disease and Advanced Obliterative Bronchiolitis. In Panel A, an image obtained during inspiration reveals dilated airways and the tree-in-bud appearance of obstructed bronchioles. In Panel B, an image obtained during an expiratory breathhold shows patchy, hyperlucent areas between areas of normal lung tissue, which is characteristic of air trapping and is referred to as mosaic attenuation.
Bronchiolitis obliterans syndrome
Bronchiolitis obliterans syndrome is a progressive obliterative bronchiolitis or constrictive bronchiolitis occurring in a subset of patients after lung transplantation and allogeneic bone marrow transplant (donor hematopoietic stem cell transplant) 7. Bronchiolitis obliterans syndrome results in progressive circumferential fibrosis and ultimate scarring of the small terminal airways, manifesting as new fixed airflow obstruction.
Allorecognition of lung antigens is the suspected cause of bronchiolitis obliterans syndrome because lung transplantation and bone marrow transplant both involve alloimmunity—host (hematopoietic cells)-vs-graft (lung) disease for lung transplantation and graft (hematopoietic cells)-vs-host (lung) disease for bone marrow transplant (hematopoietic stem cell transplant). Additionally, when bronchiolitis obliterans syndrome occurs after bone marrow transplant, it is typically accompanied by alloimmune manifestations in other organs (eg, liver, eyes, or skin).
Patients lack respiratory symptoms during mild stages of bronchiolitis obliterans syndrome, resulting in rare detection in the earliest stages of disease. Most patients present when the degree of airflow obstruction is severe, causing significant dyspnea on exertion, decreased exercise tolerance, and a persistent nonproductive cough 8. Physical examination is rarely helpful, but may reveal hyperinflation, diffuse crackles, or wheeze.12 Because these symptoms are nonspecific, other clinical processes, such as respiratory tract infections, should be considered.
In particular, bronchiolitis obliterans syndrome must be differentiated from cryptogenic-organizing pneumonia, also known as bronchiolitis obliterans organizing pneumonia (BOOP).
Clinical evaluation should include pulmonary function tests, inspiratory and expiratory high-resolution chest CT, and comprehensive infectious disease evaluation (including bronchoalveolar lavage with stains and cultures for viral, bacterial, fungal, and mycobacterial pathogens; blood cultures; cytomegalovirus polymerase chain reaction; and nasopharyngeal wash for respiratory viruses), and a thorough chronic graft-vs-host disease evaluation. Finally, echocardiography should be used to assess pulmonary artery pressure and a 6-minute walk evaluation for oxygenation status should be considered in the workup.
The diagnosis of bronchiolitis obliterans syndrome remains a significant challenge. While transbronchial biopsy is often performed, this test is hindered by low sensitivity (17%) and poor predictive value 9. Lung biopsy remains the criterion standard, demonstrating damage to the bronchiolar epithelium, obliteration of bronchiolar lumens, inflammation between the epithelium and smooth muscle, and pulmonary fibrosis 10. However, lung biopsy may result in severe complications in up to 13% of patients with chronic graft-vs-host disease and bronchiolitis obliterans syndrome 11, leading to pneumothoraces, persistent airleak syndrome, pneumomediastinum, or even death 12. Thus, noninvasive sensitive and specific methods would be the preferred diagnostic approach.
Studies suggest that less than 20% of patients improve and 65% of patients with bronchiolitis obliterans syndrome and chronic graft-vs-host disease will die within 3 years of the diagnosis of bronchiolitis obliterans syndrome regardless of the therapies instituted 13. In these studies, standard treatments included immunosuppressive agents such as corticosteroids, cyclosporine, azathioprine, and antithymocyte globulin. For patients not responding to the initial course of immunosuppressive treatment, the 2-year and 5-year survival rates were 20% and 13%, respectively 14. Recommended therapy includes high-dose systemic corticosteroids (1 mg/kg/d) for a protracted course with expected improvements in 8% to 20% of patients, of which few are likely durable given the poor overall survival 15. The addition of other immunosuppressants (eg, calcineurin inhibitors, sirolimus) seems logical and may be beneficial although this has not been tested in trials of bone marrow transplant recipients.
In lung transplantation, T-cell immunosuppressive agents such as tacrolimus and antithymocyte globulin have delayed progression of bronchiolitis obliterans syndrome after lung transplantation 16. There are some data for regular use of azithromycin, which has anti-inflammatory as well as anti-infectious properties, to treat bronchiolitis obliterans syndrome after lung transplantation 17. However, these studies are small and inconsistent 18. Anecdotal evidence has accumulated for extracorporeal photopheresis (6/7 patients with stable disease) and tumor necrosis factor blockade (1/1 patient with stable disease) 19. A retrospective study also suggested that statins, which can exhibit anti-inflammatory properties, may decrease the incidence of bronchiolitis obliterans syndrome after lung transplantation 20. From studies of mice and human bronchoalveolar lavage, leukotriene inhibitors have emerged as a potential therapy. Elevated levels of leukotrienes have been implicated in bronchiolitis obliterans syndrome after lung transplantation and pulmonary fibrosis in human and murine studies 21. Published data reveal that 3 of 5 patients with bronchiolitis obliterans syndrome had improvements with montelukast, an agent that inhibits leukotriene activity 22. Collectively, these agents represent candidate treatments that need to be evaluated rigorously in clinical trials.
Obliterative bronchiolitis causes
Obliterative bronchiolitis is most commonly caused by breathing in toxicants over time, the most common being diacetyl. Some other toxicants linked to causing obliterative bronchiolitis are:
- Acetaldehyde, found in cannabis and e-cigarette smoke
- Formaldehyde, a highly irritating chemical used in adhesives and building materials and emitted from e-cigarette smoke
- Metal oxide fumes, a byproduct of welding
- Sulfur dioxide, released by burning fossil fuels
- Ammonia
- Chlorine
- Nitrogen oxides
- Hydrochloric acid
- Mustard gas, or sulfur mustard
Besides environmental exposure, obliterative bronchiolitis can be caused by severe respiratory infections, such as respiratory syncytial virus (RSV) and adenovirus and some forms of pneumonia (e.g. Mycoplasma pneumonia) or bronchitis. Patients that suffer from rheumatic diseases, such as rheumatoid arthritis, are also at a higher risk of developing popcorn lung as well 23.
Additionally, lung transplant patients are at risk of developing the condition if their body rejects the new organ and about 50% of lung transplant recipients develop the condition within five years. This is called bronchiolitis obliterans syndrome. Other transplant patients can also be vulnerable, about 10% of people who receive a bone marrow transplant (hematopoietic stem cell transplant) from a donor develop obliterative bronchiolitis within five years of the transplant procedure 24.
Obliterative bronchiolitis recognized associations include:
- Inflammatory bowel disease (IBD)
- Rheumatoid arthritis: considered the commonest connective tissue disease to be associated with obliterative bronchiolitis 23
- Medications, e.g. penicillamine
- As a complication following lung transplantation: post lung transplant bronchiolitis obliterans 25; can occur in up to 10% of patients, usually within 6-12 months following bone marrow transplantation 26
- Swyer-James syndrome 27
Obliterative bronchiolitis symptoms
Not everyone with obliterative bronchiolitis will have symptoms. The most common symptoms include shortness of breath, dry cough and sometimes wheezing and fatigue in the absence of a cold or asthma. Symptoms will normally develop over a few weeks or months and can flare up while exercising or doing manual labor. Depending on the exposure, other parts of the body may experience irritation. For example, a skin rash may develop in addition to respiratory problems. As the condition progresses, symptoms will worsen.
Obliterative bronchiolitis diagnosis
Symptoms of obliterative bronchiolitis are similar to other lung diseases which is why your doctor will need a detailed medical history, including the mention of environmental exposure, to determine if obliterative bronchiolitis is likely. Additionally, your doctor will need to do a physical exam and listen to your breathing. They will order diagnostic tests such as a chest X-ray or CT scan of the chest, as well as non-invasive lung function tests to measure the amount of air you can breathe in and out. If the diagnosis is still unclear, a lung biopsy may be necessary.
Pulmonary function testing is essential for obliterative bronchiolitis diagnosis. Spirometry demonstrates airflow obstruction that does not reverse with inhaled bronchodilator challenge. Forced expiratory volume in one second (FEV1) will be reduced and the ratio of FEV1 to Forced vital capacity (FEV1/FVC) is also reduced. Hyperinflation may occur, and hence Total lung capacity (TLC) may be increased with air trapping. Diffusion capacity (DLCO) is usually reduced 28. The degree of FEV1 decline from post-transplant value determines the stage of bronchiolitis obliterans syndrome in lung transplant.
Chest radiographs may be normal in early disease or show signs of hyperinflation. Chest CT imaging may show bronchial wall thickening, mosaic pattern with patchy areas of hypo attenuation. If there are dynamic images with inspiratory and expiratory films, a mosaic pattern persists due to air trapping from small airway disease.
Bronchoscopy can be performed if other causes of airflow obstruction are suspected like endobronchial tumor or sarcoid, but may be unrevealing in obliterative bronchiolitis. A lung biopsy is usually not necessary for diagnosis in the setting of classic symptoms, air trapping on imaging, airflow obstruction on spirometry in the setting of organ transplantation or toxic inhalational injury. If required for diagnosis, surgical lung biopsy is preferred over transbronchial biopsy since it involves distal bronchioles and not parenchyma. In addition, the sensitivity by transbronchial biopsy for the diagnosis of obliterative bronchiolitis is low (range 15 to 87%). In cases following lung transplantation, a biopsy is not required for the diagnosis of bronchiolitis obliterans syndrome but may be required to exclude other causes of deterioration lung function like infection or acute rejection. Spirometry showing obstructive pattern is necessary for diagnosis.
Obliterative bronchiolitis treatment
Obliterative bronchiolitis is an irreversible and chronic lung condition, with available treatments that can slow progression and reduce the severity of your symptoms. It is important to catch the disease early when treatment is more likely to keep the disease from worsening. In non-transplant related obliterative bronchiolitis, removal from offending agents is essential. If obliterative bronchiolitis was caused by breathing in a harmful chemical, it is essential to reduce your exposure to that chemical and any other toxin.
Corticosteroids, specifically prednisone, is the most common treatment of obliterative bronchiolitis. Corticosteroids work by reducing inflammation through suppressing the immune system.
Additionally, your doctor may suggest using an inhaler or an inhaled medication like albuterol. These medications dilate the bronchial tubes and can improve wheezing and shortness of breath by causing the airways to slightly open.
When symptoms are severe, steroids may be prescribed. Steroids are strong medications used to fight inflammation. They work by suppressing the immune system. While often effective, steroids may also have side effects. Oxygen may be prescribed to increase low blood oxygen levels. Lung transplantation is very rarely recommended, and only for the sickest patients whose bronchiolitis is life-threatening, and who do not respond to other medications.
Immunosuppression with corticosteroids and cytotoxic agents like cyclophosphamide have been used for bronchiolitis obliterans related to rheumatoid arthritis, but have not been beneficial for bronchiolitis obliterans from toxic inhalation or post infectious cause. In these patients, symptomatic treatment should be provided with cough suppressants, inhaled bronchodilators, and oxygen supplementation if needed.
The combination of inhaled fluticasone, oral montelukast and azithromycin triple therapy has also shown to decrease decline in lung function in bronchiolitis obliterans syndrome post-hematopoietic stem cell transplant. In addition to these therapies, controlling gastro esophageal reflux is also recommended to decrease bronchiolitis obliterans syndrome. In cases where bronchiolitis obliterans syndrome is progressive and severe, then retransplantation of a lung may be indicated 29. Extracorporeal photopheresis has also been successfully used to slow the decline in lung function from bronchiolitis obliterans syndrome.
Obliterative bronchiolitis prognosis
The natural history of obliterative bronchiolitis is highly variable and cannot be predicted in individual patients. The earliest reported cases of occupational obliterative bronchiolitis were recognized because of acute, intense toxic exposure. More recent examples suggest a prolonged exposure that can occasionally lead to severe respiratory insufficiency 30. The incidence of obstructive abnormalities on spirometry was shown to increase with increasing cumulative exposure to airborne flavoring chemicals 31. Increased mortality from respiratory disease has recently been found at a microwave popcorn-production facility where there was a risk of obliterative bronchiolitis among workers, especially those employed before the company reduced exposure to diacetyl 32. In fact, obliterative bronchiolitis is generally nonprogressive once exposure ceases 30.
Transplant-related obliterative bronchiolitis (bronchiolitis obliterans syndrome) has been associated with an increased risk of death, especially when it develops soon after transplantation 33. If bronchiolitis obliterans syndrome develops within two years of lung transplantation, it is seen as predictive of worse outcome. Although transplant-related obliterative bronchiolitis is generally characterized by a rapid decline in lung function, FEV1 stabilizes in a subset of patients 33. The clinical course of bronchiolitis obliterans syndrome related to transplant is variable with some patients being asymptomatic or stable after diagnosis and some patients with the slow and steady decline and others with an episodic drop in FEV1.
References- Aguilar, Patrick R. MD; Michelson, Andrew P. MD; Isakow, Warren MD Obliterative Bronchiolitis, Transplantation: February 2016 – Volume 100 – Issue 2 – p 272-283 doi: 10.1097/TP.0000000000000892
- Chambers DC. Bronchiolitis obliterans syndrome ‘endotypes’ in haematopoietic stem cell transplantation. Respirology. 2019 May;24(5):408-409.
- Krishna R, Anjum F, Oliver TI. Bronchiolitis Obliterans (Obliterative Bronchiolitis, Constrictive Bronchiolitis) [Updated 2020 Jul 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441865
- Learn About Bronchiolitis Obliterans. https://www.lung.org/lung-health-diseases/lung-disease-lookup/popcorn-lung/learn-about-popcorn-lung
- Rao U, Sharma M, Mohanakumar T, Ahn C, Gao A, Kaza V. Prevalence of antibodies to lung self-antigens (Kα1 tubulin and collagen V) and donor specific antibodies to HLA in lung transplant recipients and implications for lung transplant outcomes: Single center experience. Transpl. Immunol. 2019 Jun;54:65-72.
- Obliterative Bronchiolitis. N Engl J Med 2014; 370:1820-1828 DOI: 10.1056/NEJMra1204664 https://www.nejm.org/doi/full/10.1056/nejmra1204664
- Nicod LP. Mechanisms of airway obliteration after lung transplantation. Proc Am Thorac Soc. 2006; 3(5):444–449.
- Clark JG, Crawford SW, Madtes DK, Sullivan KM. Obstructive lung disease after allogeneic marrow transplantation: clinical presentation and course. Ann Intern Med. 1989;111 (5):368–376.
- Chamberlain DA, Maurer J, Chaparro C, Idolor L. Evaluation of transbronchial lung biopsy specimens in the diagnosis of bronchiolitis obliterans after lung transplantation. J Heart Lung Transplant. 1994; 13(6):963–971.
- Williams KM, Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation. JAMA. 2009;302(3):306-314. doi:10.1001/jama.2009.1018 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7357209
- White DA, Wong PW, Downey R. The utility of open lung biopsy in patients with hematologic malignancies. Am J Respir Crit Care Med. 2000; 161(3 pt1):723–729.
- Chadwick C, Marven SM, Vora AJ. Autologous blood pleurodesis for pneumothorax complicating graft-versus-host disease-related bronchiolitis obliterans. Bone Marrow Transplant. 2004;33(4): 451–453.
- Chien JW, Martin PJ, Gooley TA, et al. Airflow obstruction after myeloablative allogeneic hematopoietic stem cell transplantation. Am J Respir Crit Care Med. 2003;168(2):208–214.
- Dudek AZ, Mahaseth H, DeFor TE, Weisdorf DJ. Bronchiolitis obliterans in chronic graft-versus-host disease: analysis of risk factors and treatment outcomes. Biol Blood Marrow Transplant. 2003;9(10): 657–666.
- Duncan CN, Buonanno MR, Barry EV, Myers K, Peritz D, Lehmann L. Bronchiolitis obliterans following pediatric allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008; 41(11):971–975.
- Hollmén M, Tikkanen JM, Nykanen AI, Koskinen PK, Lemstrom KB. Tacrolimus treatment effectively inhibits progression of obliterative airway disease even at later stages of disease development. J Heart Lung Transplant. 2008;27(8):856–864.
- Gottlieb J, Szangolies J, Koehnlein T, Golpon H, Simon A, Welte T. Long-term azithromycin for bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2008;85(1):36–41.
- Porhownik NR, Batobara W, Kepron W, Unruh HW, Bshouty Z, Effect of maintenance azithromycin on established bronchiolitis obliterans syndrome in lung transplant patients. Can Respir J. 2008; 15(4): 199–202.
- Ilhan O, Arat M, Arslan O, et al. Extracorporeal photoimmunotherapy for the treatment of steroid refractory progressive chronic graft-versus-host disease. Transfus Apheresis Sci. 2004;30(3):185–187.
- Johnson BA, lacono AT, Zeevi A, McCurry KR, Duncan SR. Statin use is associated with improved function and survival of lung allografts. Am J Respir Crit Care Med. 2003;167(9):1271–1278.
- Islam SA, Thomas SY, Hess C, et al. The leukotriene B4 lipid chemoattractant receptor BLT1 defines antigen-primed T cells in humans. Blood. 2006; 107(2):444–453.
- Or R, Gesundheit B, Resnick I, et al. Sparing effect by montelukast treatment for chronic graft versus host disease: a pilot study. Transplantation. 2007;83 (5):577–581.
- Devouassoux G, Cottin V, Lioté H, et al. Characterisation of severe obliterative bronchiolitis in rheumatoid arthritis. Eur Respir J. 2009;33(5):1053-1061. doi:10.1183/09031936.00091608
- Gunn ML, Godwin JD, Kanne JP, Flowers ME, Chien JW. High-resolution CT findings of bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. J Thorac Imaging. 2008;23(4):244-250. doi:10.1097/RTI.0b013e3181809df0
- Worthy SA, Park CS, Kim JS, Müller NL. Bronchiolitis obliterans after lung transplantation: high-resolution CT findings in 15 patients. AJR Am J Roentgenol. 1997;169(3):673-677. doi:10.2214/ajr.169.3.9275875
- Wah TM, Moss HA, Robertson RJ, Barnard DL. Pulmonary complications following bone marrow transplantation. Br J Radiol. 2003;76(906):373-379. doi:10.1259/bjr/66835905
- Brant WE, Helms CA. Fundamentals of Diagnostic Radiology. Lippincott Williams & Wilkins. (2007) ISBN:0781761352
- Kavaliunaite E, Aurora P. Diagnosing and managing bronchiolitis obliterans in children. Expert Rev Respir Med. 2019 May;13(5):481-488.
- Sheth JS, Belperio JA, Fishbein MC, Kazerooni EA, Lagstein A, Murray S, Myers JL, Simon RH, Sisson TH, Sundaram B, White ES, Xia M, Zisman D, Flaherty KR. Utility of Transbronchial vs Surgical Lung Biopsy in the Diagnosis of Suspected Fibrotic Interstitial Lung Disease. Chest. 2017 Feb;151(2):389-399.
- Akpinar-Elci M, Travis WD, Lynch DA, Kreiss K. Bronchiolitis obliterans syndrome in popcorn production plant workers. Eur Respir J 2004;24:298-302
- From the Centers for Disease Control and Prevention: fixed obstructive lung disease in workers at a microwave popcorn factory — Missouri, 2000-2002. JAMA 2002;287:2939-2940
- Halldin CN, Suarthana E, Fedan KB, Lo YC, Turabelidze G, Kreiss K. Increased respiratory disease mortality at a microwave popcorn production facility with worker risk of bronchiolitis obliterans. PLoS One 2013;8:e57935-e57935
- Bergeron A, Godet C, Chevret S, et al. Bronchiolitis obliterans syndrome after allogeneic hematopoietic SCT: phenotypes and prognosis. Bone Marrow Transplant 2013;48:819-824