Oculocardiac reflex
The oculocardiac reflex also known as trigeminovagal reflex, Aschner phenomenon, Aschner reflex, or Aschner-Dagnini reflex, is a reduction in heart rate (bradycardia) associated with traction applied to extraocular muscles and/or compression of the eyeball 1. The oculocardiac reflex is defined by a decrease in heart rate by greater than 20% following globe pressure or traction of the extraocular muscles. The oculocardiac reflex most commonly results in sinus bradycardia. However, it also has a reported association with reduced arterial pressure, arrhythmia, asystole, and even cardiac arrest. The oculocardiac reflex has most notably been depicted during ophthalmologic procedures, more specifically during strabismus surgery; however, it also may be activated by facial trauma, regional anesthetic nerve blocks, and during mechanical stimulation 2. It is also important to note that a globe need not be present for the reflex to occur and there are reported cases of reflex bradycardia with tense orbital hematoma following an enucleation procedure (Dewar KMS. The Oculocardiac Reflex. Proc. Roy. Soc. Med. 1976; 6: 13-14.)). Oculocardiac reflex fatigues with repeated stimulation.
The oculocardiac reflex is mediated by nerve connections between the trigeminal cranial nerve and the vagus nerve of the parasympathic nervous system 3. The afferent tracts derive mainly from the ophthalmic division of the trigeminal nerve, although tracts from the maxillary and mandibular division have also been documented. These afferents synapse with the visceral motor nucleus of the vagus nerve, located in the reticular formation of the brain stem. The efferent portion is carried by the vagus nerve from the cardiovascular center of the medulla to the heart, of which increased stimulation leads to decreased output of the sinoatrial node 4. The oculocardiac reflex is especially sensitive in neonates and children, and must be monitored, usually by an anaesthesiologist, during paediatric ophthalmological surgery, particularly during strabismus correction surgery 5. However, this reflex may also occur with adults. Bradycardia, junctional rhythm, asystole, and very rarely death 6, can be induced through this reflex.
The incidence of the oculocardiac reflex is reported to be anywhere from 14% to 90% and decreases with age, meaning pediatric patients are most at risk. Pediatric patients are also more susceptible to the detrimental consequences of this reflex secondary to having a greater dependency on heart rate to maintain cardiac output. The wide range of incidence and the severity of oculocardiac reflex is reportedly attributed to the effects of hypoxia, hypercarbia, acidosis, and the anesthetic agents used during surgery 7.
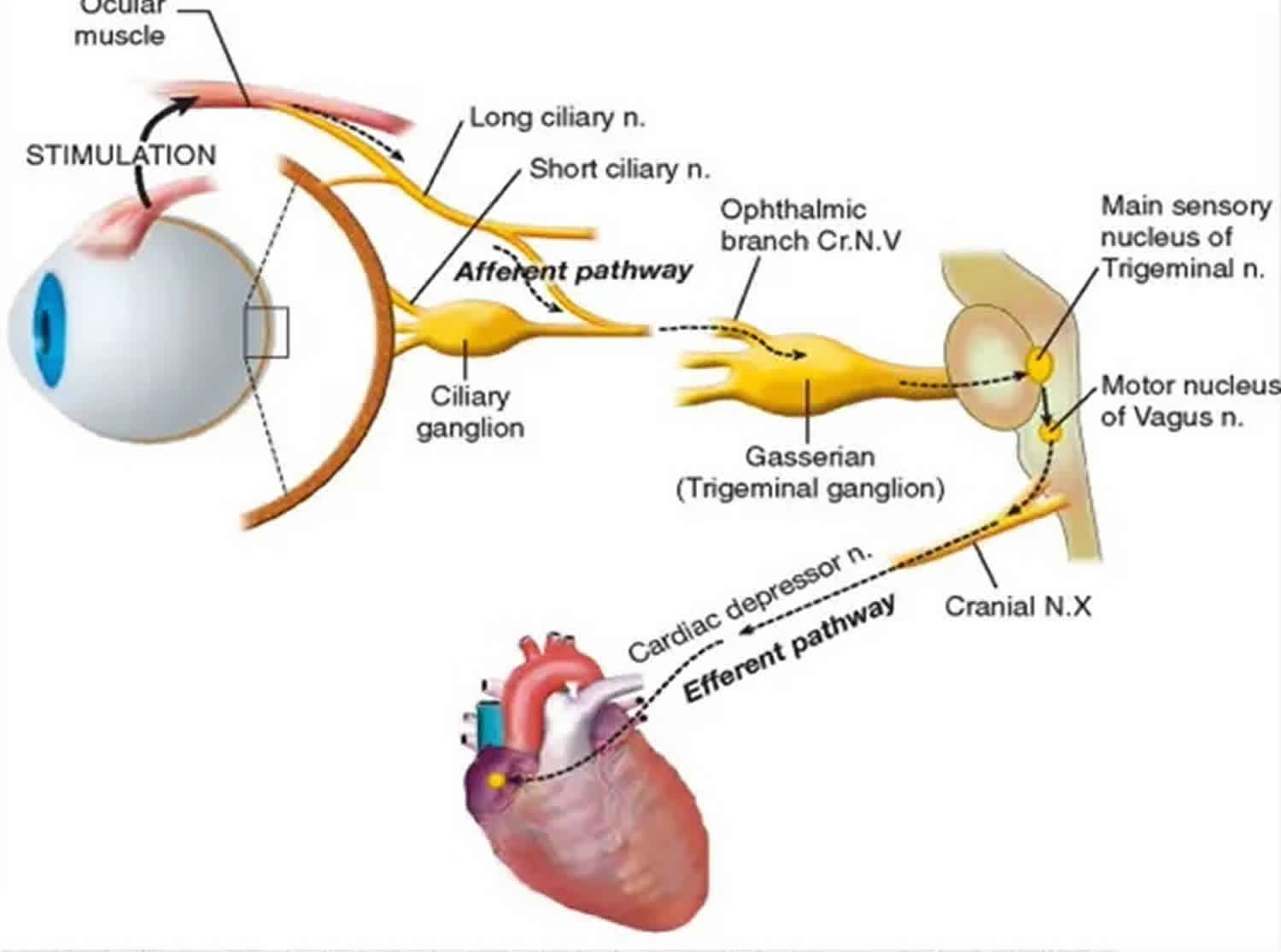
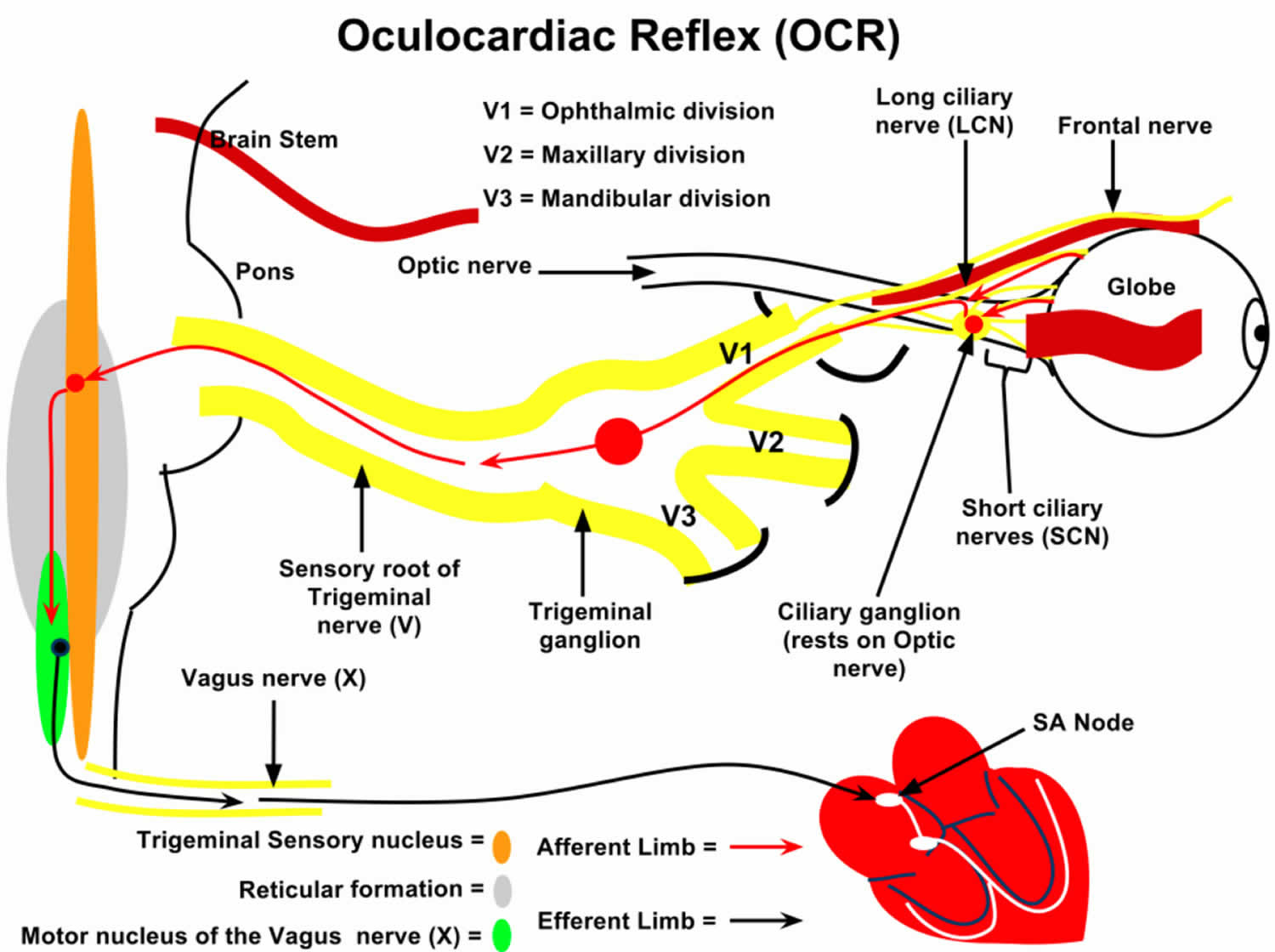
Oculocardiac reflex pathway
The oculocardiac reflex pathway consists of an afferent and efferent limb. The trigeminal nerve, otherwise known as the fifth cranial nerve, serves as the sensory afferent limb. The vagus nerve, also known as cranial nerve ten, comprises the efferent limb of the oculocardiac reflex. The pathway is initiated by activation of stretch receptors in the ocular and periorbital tissues. The short and long ciliary nerves conduct impulses that carry the sensory message to the ciliary ganglion. From there the impulses are transported by way of the ophthalmic division of the trigeminal nerve to the Gasserian ganglion, followed by the trigeminal nucleus, where the afferent limb will terminate in the central nervous system (CNS). The central nervous system will then process this sensory information, and internuclear communication will occur between the trigeminal sensory nucleus and the visceral motor nucleus of the vagus nerve. This stimulates the efferent limb, causing impulses to exit the brainstem and transmit to the myocardium to synapse as the sinoatrial node and activate the vagal motor response. The resultant effects include negative chronotropy, leading to bradycardia.
Afferent Limb
Trigeminal Nerve (ciliary ganglion to ophthalmic division of trigeminal nerve to gasserian ganglion to the main trigeminal sensory nucleus). Also afferent tracts from maxillary and mandibular divisions of trigeminal nerve have been documented.
Efferent Limb
Vagus Nerve (afferents synapse with visceral motor nucleus of vagus nerve located in the reticular formation and efferents travel to the heart and decrease output from the sinoatrial node).
Triggering Stimuli
Triggered by traction on the extraocular muscles (especially medial rectus), direct pressure on the globe, ocular manipulation, ocular pain.
Can also be triggered by retrobulbar block (pressure associated with local infiltration), ocular trauma, or manipulation of tissue in orbital apex after enulcleation.
Figure 1. Oculocardiac reflex pathway
Oculocardiac reflex causes
The oculocardiac reflex has been associated with various triggering stimuli, with the most common being traction to the extraocular muscles. Multiple studies have reported an increased incidence with medial rectus traction when compared to other ocular muscles. However, there also have been studies reporting no increased association with traction to a specific extraocular muscle over another.
Additional stimuli that have been linked to triggering the oculocardiac reflex include direct pressure to the globe, ocular manipulation, and ocular pain. Secondary to increased pressure, retrobulbar blocks, ocular hematomas, and facial or orbital trauma also may induce activation of the reflex. It is also important to note that this is a fatigable reflex, meaning its intensity will decrease with multiple, repeated stimuli 8.
Oculocardiac reflex may occur during both local and general anesthesia. The retrobulbar block may prevent arrythmias by blocking the afferent limb, but may also stimulate the oculocardiac reflex with pressure of local injection.
The incidence of the oculocardiac reflex decreases with age and tends to be more pronounced in young, healthy patients, which is clinically significant for pediatric aanesthesiologists as it is observed with greatest incidence in young healthy neonates and infants undergoing strabismus surgery 9.
Hypoxia, hypercarbia, acidosis, and light anesthesia can worsen the severity of the oculocardiac reflex.
As the oculocardiac reflex is a vagal response, clinicians have attempted to abolish the vagal stimulation of the heart using atropine and gallamine. Of the two anticholinergic medications used, there appears to be less bradycardia with atropine as opposed to gallamine, 0% vs. 5% incidence, respectively 10.
Some clinicians have also attempted to minimize or reduced the effect of the reflex by inducing very deep anesthesia, which appears to be clinically significant at bispectral index (BIS) values below 50 9.
Others have attempted to use short acting opioid narcotics, i.e. remifentanil, to abalate the response to ocular pressure and have reported this to actually increase the incidence and severity of the reflex 11.
Oculocardiac reflex symptoms
The oculocardiac reflex is a reduction in heart rate associated with traction applied to extraocular muscles and/or compression of the eyeball 1. The oculocardiac reflex is defined by a decrease in heart rate by greater than 20% following globe pressure or traction of the extraocular muscles. The oculocardiac reflex most commonly results in sinus bradycardia. However, it also has a reported association with reduced arterial pressure, junctional rhythm, ectopic beats, atrioventricular block, ventricular tachycardia, asystole, and even cardiac arrest. The oculocardiac reflex has most notably been depicted during ophthalmologic procedures, more specifically during strabismus surgery; however, it also may be activated by facial trauma, regional anesthetic nerve blocks, and during mechanical stimulation 2.
Though the most common side effect of the oculocardiac reflex is bradycardia, with a further decline to potentially fatal arrhythmias, asystole, and even cardiac arrest. In two studies, one in 1973 by Apt et al. and another in 2015 by Espahbodi et al. 12 reported the oculocardiac reflex occurrence rate of oculocardiac reflex in patients undergoing ophthalmologic surgeries as 67.9% and 63% respectively. Though the majority of these patients do not experience detrimental outcomes following activation of the oculocardiac reflex, the potential makes this phenomenon important to note 13.
Activation of the oculocardiac reflex also has been associated with noncardiac consequences. Due to activation of the vagal motor response, other vagal effects reported include hypotensive episodes, syncope, and gastrointestinal responses such as nausea and vomiting. This has been questioned to have an impact on the severity of postoperative nausea and vomiting. In the pediatric population, the incidence of postoperative nausea and vomiting has been reported to be as high as 85% following strabismus surgery and is the most common reason for inpatient admission following an outpatient procedure.
Oculocardiac reflex complications
The complications secondary to the oculocardiac reflex are related to the vagal responses and may include the following:
- Sinus bradycardia
- Arrhythmia
- Reduced atrial pressure
- Ventricular tachycardia
- Ventricular fibrillation
- Multifocal premature ventricular contractions
- Ventricular bigeminy
- Asystole
- Cardiac arrest
- Dizziness
- Lightheadedness
- Nausea
- Weakness
Oculocardiac reflex treatment
The only definitive treatment for oculocardiac reflex is the immediate cessation of the triggering stimulus. When in the operating room, immediate removal of pressure to the globe of the eye or surrounding orbital tissues can terminate the reflex. The next step of the procedure is to proceed with caution. Unfortunately, in less controlled circumstances, such as trauma, cessation of the triggering stimulus can be more challenging. In these instances, pharmacologic management may be required, and cardiac monitoring should be initiated.
Additionally, it is important to know what anesthetic agents can be used to help decrease oculocardiac reflex occurrence, as the incidence may vary with each agent used. Multiple studies have shown that pretreatment with intravenous anticholinergics, such as atropine or glycopyrrolate, decreases the incidence of oculocardiac reflex. Atropine works by blocking peripheral muscarinic receptors of the heart and causes increased firing at the sinoatrial node as well as conduction through the AV node. This opposes the vagal response, or the efferent limb, of the oculocardiac reflex. Through its stimulation of sympathetic activity, ketamine may counteract vagal stimulation caused by oculocardiac reflex. A study by Choi et al. 14 reported a lower incidence of oculocardiac reflex when a ketamine infusion was used as the primary anesthetic agent when compared to sevoflurane, halothane, and propofol. Ketamine was reported by Espahbodi et al. 12 in 2015 to be superior to atropine in decreasing the incidence of oculocardiac reflex. In another study, ketamine also was associated with a lower incidence of postoperative nausea, vomiting, and agitation.
Blunting the afferent limb of the reflex arc can also decrease oculocardiac reflex occurrence. This can be done using a retro or peribulbar block with xylocaine hydrochloride to block the ciliary ganglion. This in combination with another agent shown to decreased oculocardiac reflex incidence, such as atropine, can provide further protection from oculocardiac reflex activation.
It is important to note that administration of fast-acting opioids, such as fentanyl, sufentanil, and remifentanil, can potentially facilitate bradycardia caused by the oculocardiac reflex. Many anesthetic agents have been studied regarding their effects on oculocardiac reflex, and it is crucial to know how each acts on the reflex. Many still require further investigation. However, it has repeatedly been reported that preanesthetic medication with atropine, retrobulbar blocks, or other agents used to blunt the oculocardiac reflex should be routinely utilized during procedures or traumas related to the eye. This is to protect patients against the potential consequences of oculocardiac reflex activation.
References- Dunville LM, Kramer J. Oculocardiac Reflex. [Updated 2019 May 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499832
- Waldschmidt B, Gordon N. Anesthesia for pediatric ophthalmologic surgery. J AAPOS. 2019 Jun;23(3):127-131.
- Lang S, Lanigan D, van der Wal M (1991). “Trigeminocardiac reflexes: maxillary and mandibular variants of the oculocardiac reflex”. Can J Anaesth. 38 (6): 757–60.
- Paton J, Boscan P, Pickering A, Nalivaiko E (2005). “The yin and yang of cardiac autonomic control: vago-sympathetic interactions revisited”. Brain Res Brain Res Rev. 49 (3): 555–65.
- Kim H, Kim S, Kim C, Yum M (2000). “Prediction of the oculocardiac reflex from pre-operative linear and nonlinear heart rate dynamics in children”. Anaesthesia. 55 (9): 847–52.
- Smith R (1994). “Death and the oculocardiac reflex”. Can J Anaesth. 41 (8): 760.
- Rahimi Varposhti M, Moradi Farsani D, Ghadimi K, Asadi M. Reduction of oculocardiac reflex with Tetracaine eye drop in strabismus surgery. Strabismus. 2019 Mar;27(1):1-5.
- Shakil H, Wang AP, Horth DA, Nair SS, Reddy KKV. Trigeminocardiac Reflex: Case Report and Literature Review of Intraoperative Asystole in Response to Manipulation of the Temporalis Muscle. World Neurosurg. 2019 Feb;122:424-427.
- Yi C, Jee D. Influence of the anaesthetic depth on the inhibiton of the oculocardiac reflex during sevoflurane anesthesia for pediatric strabismus surgery. Brit. Journ. Anes. 2008; 101(2): 234-238.
- Dewar KMS. The Oculocardiac Reflex. Proc. Roy. Soc. Med. 1976; 6: 13-14.
- Chung CJ, Lee JM, Choi SR, Lee SC, Lee JH. Effect of remifentanil on oculocardiac reflex in pediatric strabismus surgery. Acta Anaesthesiol Scand 2008; 52: 1273-1277.
- Espahbodi E, Sanatkar M, Sadrossadat H, Darabi Vafsi ME, Azarshahin M, Shoroughi M. Ketamine or atropine: which one better prevents oculocardiac reflex during eye surgery? A prospective randomized clinical trial. Acta Med Iran. 53(3):158-161. acta.tums.ac.ir/index.php/acta/article/view/4917/4351
- Bloch M. Oculocardiac reflex: ‘My heart just stopped’. Emerg Med Australas. 2018 Aug;30(4):592-593.
- Choi SR, Park SW, Lee JH, et al. Effect of different anesthetic regimes on the oculocardiac reflex during pediatric strabismus surgery. J Anesth 2000;23(4):489-93.