What is plethysmography
Plethysmography is used to measure changes in volume in different parts of the body. Plethysmography may be done to check for blood clots in the arms and legs. Plethysmography is also done to measure how much air you can hold in your lungs.
Penile pulse volume recording is a type of plethysmography test. Plethysmography is done on the penis to check for causes of erectile dysfunction.
Most commonly, plethysmography test is performed to check blood flow in the arteries of the legs. This is done in people with conditions like hardening of the arteries (atherosclerosis). Atherosclerosis causes pain during exercise or poor healing of leg wounds.
Air displacement plethysmography
Air displacement plethysmography is used to measure body volume. With air displacement plethysmography you’re enclosed in a computerized, egg-shaped chamber (Bod Pod, others). The device measures your weight and volume to determine your body density, then uses these figures to calculate your percentage of body fat. Air displacement plethysmography often underestimates fat mass compared to other physique assessment techniques; however, this may be due to poor standardization practices 1. When undertaken in a well-controlled standardized manner, Bod Pod has proven to be an accurate and reliable technique for tracking physique changes over time. It is valuable in large athletes who may be more comfortable undertaking physique assessment via Bod Pod compared to other techniques where reliability in this population might be an issue.
Figure 1. Air displacement plethysmography
Whole-body plethysmography
Whole-body plethysmography also called lung plethysmography or body plethysmography is a test used to measure how much air you can hold in your lungs. Whole-body plethysmography is done to see how much air you can hold in your lungs during rest. Whole-body plethysmography measures intrathoracic gas volume, total lung capacity, functional residual capacity, and (specific) airway resistance RAW (sRAW), which requires no active cooperation of the patient to be captured 2. Whole-body plethysmography helps your doctor determine if a lung problem is due to damage to the lung structure, or a loss of the lungs’ ability to expand (get bigger as air flows in).
Whole-body plethysmography is regarded as highly important in routine clinical practice for the diagnostic evaluation in asthma 3 and chronic obstructive pulmonary disease (COPD) 4, which is also reflected in German guidelines 5, whereas it is barely mentioned in international guidelines. Renowned scientists in international pneumology keep casting doubt on its diagnostic usefulness 6. However, Decramer et al. 7 showed recently on the basis of decision scenarios in focus groups that whole-body plethysmography contributed significantly to establishing the diagnosis. The specific role of whole-body plethysmography in the diagnosis of bronchial asthma has remained unclear 8.
Although whole-body plethysmography is the most accurate way to measure how much air you can hold in your lungs, it is not often used because of its technical difficulties.
You will sit in a large airtight cabin known as a body box. The chamber resembles a glass-walled telephone box in shape and volume (about 700–1000 L). During measurement the body box is closed with an airtight seal, except for a small controlled leak that is used to stabilize the internal pressure by allowing for equilibration of slow pressure changes, e.g. due to warming-up. One pressure transducer serves to measure the pressure inside the box relative to ambient pressure, another one is placed close to the mouth for recording mouth pressure during a shutter maneuver. The shutter mechanism can be used to deliberately block the airflow by transient occlusion. Moreover, respiratory flow rate is recorded by conventional equipment, such as pneumotachograph, anemometer, or ultrasound measurement, all of which is calibrated via syringes delivering a defined volume.
The walls of the cabin are clear so that you and the health care provider can see each other. You will breathe or pant against a mouthpiece. Clips will be put on your nose to close off your nostrils. Depending on the information your doctor is looking for, the mouthpiece may be open at first, and then closed.
You will breathe against the mouthpiece in both the open and closed positions. The positions give different information to the doctor. As your chest moves while you breathe or pant, it changes the pressure and amount of air in the room and against the mouthpiece. From these changes, the doctor can get an accurate measure of the amount of air in your lungs.
Depending on the purpose of the whole-body plethysmography, you may be given medicine before the test.
The principle of measurement of the commonly used whole-body plethysmographs relies on detecting changes in box pressure in combination with either changes of mouth pressure or with flow rate under defined breathing conditions. These signals are evaluated in order to determine static lung volumes and airflow resistance.
The basic physical principle exploited by body plethysmography is the law of Boyle-Mariotte. According to Boyle-Mariotte’s law the unknown volume of a closed compartment can be determined if absolute changes of volume can be induced and the corresponding relative changes in pressure can be measured. Therefore, the determination of thoracic gas volume would be possible if the lung could be treated as a closed compartment and if one could measure the changes in alveolar pressure in parallel to the changes in volume.
This relationship bears information on lung volume. When moving a plunger a certain distance (volume difference) in a short versus a long cylinder of given cross section, pressure change will be greater in the short cylinder. Translated to the lung: the larger the lung volume for a given shift volume, the smaller the pressure change. Conversely, the greater the pressure change, the smaller the lung volume must be relative to the shift volume. Therefore, in a large lung the occlusion pressure curve will be more flat, and in a small lung more steep.
In more detail this can be described as follows. The relative change in pressure is the ratio of the alveolar pressure change to the equilibrium alveolar pressure. Correspondingly, the relative change in volume is the ratio of the shift volume to the lung volume. According to Boyle-Mariotte’s law the two relative changes are equal in magnitude. Thus, if one has measured the relative pressure change, one also knows the relative volume change. If additionally the absolute volume change has been measured, which is just the shift volume, then one can compute the absolute volume that produces the given relative change. The determination of absolute and relative pressure changes is equivalent as the reference pressure is always barometric pressure.
The question arises how to assess the change in alveolar pressure. This is determined by measuring the pressure generated at the mouth during respiratory efforts, while the airflow is blocked. The zero-flow condition implies mouth pressure to be equal to alveolar pressure, because occurrence of a pressure gradient and occurrence of airflow are necessarily linked to each other. To achieve this condition, a shutter is used that prevents air from entering or leaving the lung (occlusion pressure maneuver). Normal inspiratory and expiratory efforts against the closed shutter lead to decompression and compression of the air in the lung.
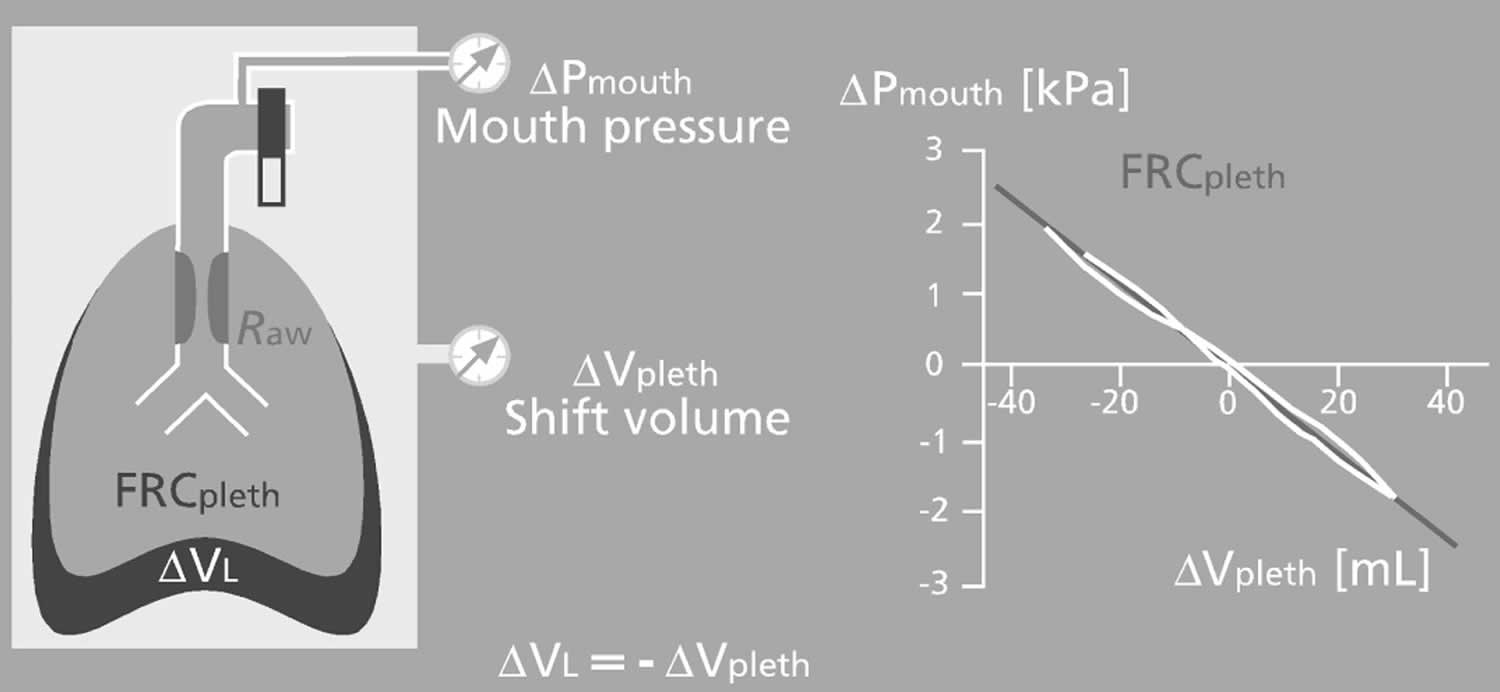
Compared to the volume at equilibrium pressure, this air mass now occupies different volumes. Therefore a volume difference, i.e. shift volume, is generated. This is transmitted to the box through the movement of the thorax, as in the case of uninhibited airflow. Under the zero-flow assumption the change in alveolar pressure can be measured at the shutter as change in mouth pressure. Since shift volume (the amount of compression and decompression) and alveolar pressure change are proportional to each other, the result is a linear relationship between mouth occlusion pressure on one hand and shift volume or box pressure on the other hand (Figure 3).
For the present purpose this law can be concisely expressed as the statement that for a fixed amount of gas in a closed compartment the relative changes in the compartment’s volume are always equal in magnitude but opposite in sign to the relative changes in pressure. Thus one can infer relative volume changes from pressure changes and, even more, absolute volumes if the absolute volume changes are known. A summary of the terms used, their abbreviations and units, and a short description of their use is given in Table 1.
Figure 2. Whole-body plethysmography
Table 1. Short description of specific terms used in the text and figures.
| Parameter | Abbreviation | Unit | Short description |
|---|---|---|---|
| Shift volume | mL | Change of volume by which the lung generates positive or negative alveolar pressure, i.e. deviation from the volume at which equilibrium of alveolar and box pressures would hold; represents a small part of tidal volume during free breathing | |
| Alveolar pressure | kPa | Mean pressure generated in the peripheral lung; provides the driving force for the airflow | |
| Mouth pressure | kPa | Pressure measured at the mouth during the shutter maneuver; used as proxy for alveolar pressure under the zero-flow condition | |
| Box pressure | kPa | Pressure measured in the body plethysmographic box during free breathing or the shutter maneuver; inversely related to alveolar pressure and generated by the shift volume | |
| Flow rate | L/s | Airflow rate measured at the mouth; also used to derive inspired and expired volumes by integration | |
| Specific airway resistance | sRaw | kPa s | Inverse slope of the plot of flow rate versus box pressure (specific resistance loops); indicates volume- and resistance-dependent work of breathing needed in order to generate a reference flow rate of 1 L/s |
| Airway resistance | Raw | kPa s L−1 | Flow resistance of the airways, i.e. ratio of alveolar driving pressure minus mouth pressure to flow rate; computed from sRaw and FRC; indicates the alveolar pressure needed to generate a reference flow rate of 1 L/s |
| Intrathoracic gas volume | TGV or ITGV | L | Lung volume at which the shutter is closed (in principle deliberate); this closure is conventionally performed at the end of a normal expiration |
| Functional residual capacity | FRCpleth | L | Lung volume at the end of a normal expiration, i.e. upon mechanical equilibrium of the opposite forces exerted by the lung tissue and thorax |
| Residual volume | RV | L | Lung volume reached upon maximum expiration |
| Total lung capacity | TLC | L | Lung volume reached upon maximum inspiration |
| Expiratory reserve volume | ERV | L | Volume of air exhaled by maximum expiration starting from FRC; used to derive RV from FRC |
| Inspiratory vital capacity | VC or IVC | L | Volume inspired starting from maximum expiration up to maximum inspiration; added to RV in order to obtain TLC |
| Expired (slow) vital capacity | EVC | L | Maximum volume that can be slowly exhaled after maximum inspiration; assessed in patients who can only inspire, and not expire, after opening of the shutter |
| Inspiratory capacity | IC | L | Volume of air that can be maximally inspired starting from FRCpleth; assessed either directly after opening of the shutter or by the difference IVC minus ERV |
| Tidal volume | VT | L | Volume of air moved during normal breathing; used to compute the mean volume at which specific resistance loops are recorded, by adding VT/2 to FRCpleth |
Figure 3. Plethysmographic shift volume
Footnote: Mouth pressure (denoted by ΔPmouth) versus shift volume (ΔVpleth) during respiratory efforts against the closed shutter for determination of FRCpleth.. The plethysmographic shift volume is the mirror image of that of the lung (ΔVL) (for details see text).
[Source 9 ]Shift volume and box pressure
The shift volume provides the link to the box pressure that is at the heart of body plethysmography and allows the determination of two primary measures: thoracic gas volume and specific airway resistance. Both measurements rely on the fact that the volume defect within the lung represented by the shift volume is necessarily equal in magnitude but opposite in sign to a volume defect in the body box. Thus, the shift volume in the box is the mirror image of the shift volume of the lung. This is the consequence of the fact that the box is hermetically sealed and has stable walls. Therefore, any change in lung volume must be equivalent to an opposite change in the free volume of the box outside the body, independent of the fact whether pressure equilibration has been achieved or not.
As the free volume of the box is known (total box volume minus body volume as estimated from body weight), Boyle-Mariotte’s law is applicable and allows to derive the shift volume from the pressure change. Specifically, the relative change in the free box volume is equal but opposite in sign to the relative change in box pressure. This relationship can be used only because the box volume is known. In reality, the relationship is determined empirically by using a motorized pump that changes the volume in the body by defined amounts and by recording the concomitant changes in box pressure. It is important to understand that conceptually shift volume and change in box pressure are physically equivalent and interchangeable, and both might be used in diagrams without loss or gain of information. While for an initial intuitive understanding box pressure might offer the best approach, the physiological interpretation benefits more from shift volume. This is a major reason why the present description focuses on this measure.
Abnormal results point to a problem in the lungs. This problem can be due to a breakdown of the lung structure, a problem with the chest wall and its muscles, or a problem with the lungs being able to expand and contract.
Whole-body plethysmography will not find the cause of the problem. But it helps the doctor narrow down the list of possible problems.
Risks of whole-body plethysmography test may include feeling:
- Anxiety from being in the closed box
- Dizzy
- Lightheaded
- Short of breath
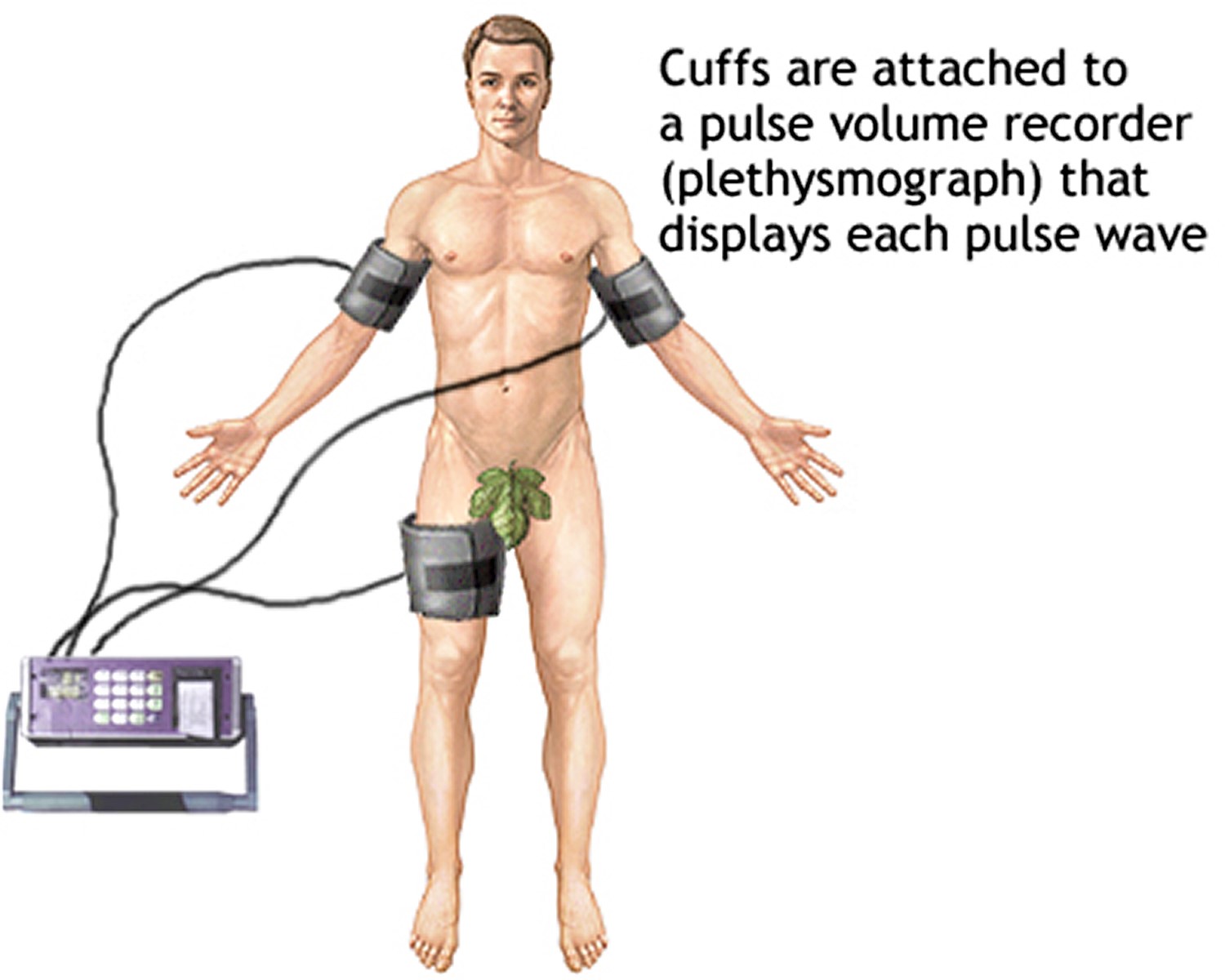
Pulse plethysmography
Pulse plethysmography also called limb plethysmography is a test that compares blood pressure in the legs and arms. Pulse plethysmography is most often done to check for narrowing or blockages of blood vessels (arteries) in your arms or legs. Pulse plethysmography is not as accurate as an arteriography. Pulse plethysmography may be done for very ill people who cannot travel to the arteriography lab. Pulse plethysmography can be used to screen for vascular disease or to follow up earlier abnormal tests. The test is noninvasive, and it does not use x-rays or injection of dye. It is also less expensive than an angiogram.
Pulse plethysmography may be done in the health care provider’s office or in a hospital. You will be asked to lie with the upper part of your body slightly raised.
Pulse plethysmography test is performed by placing three or four blood pressure cuffs around your arms and leg to measure the systolic pressure. The cuffs are then attached to a pulse volume recorder (plethysmograph) that displays each pulse wave. Your doctor inflates the blood pressure cuffs, and a machine called a plethysmograph measures the pulses from each cuff. The test records the maximum pressure produced when the heart contracts (systolic blood pressure). The test compares the systolic blood pressure of the lower extremity to the upper extremity, to help rule out disease that blocks the arteries in the extremities.
Differences between the pulses are noted. If there is a decrease in the pulse between the arm and leg, it may indicate a blockage.
When the test is complete, the blood pressure cuffs are removed.
Normal results: There should be less than a 20 to 30 mm Hg difference in the systolic blood pressure of the leg compared with that of the arm.
Abnormal results may be due to:
- Arterial occlusive disease
- Blood clots
- Blood vessel changes due to diabetes
- Injury to an artery
- Other blood vessel disease (vascular disease)
Other conditions for which the limb plethysmography may be performed:
- Deep venous thrombosis
If you have an abnormal result, you may need to have more testing to find the exact site of the narrowing.
Figure 4. Pulse plethysmography
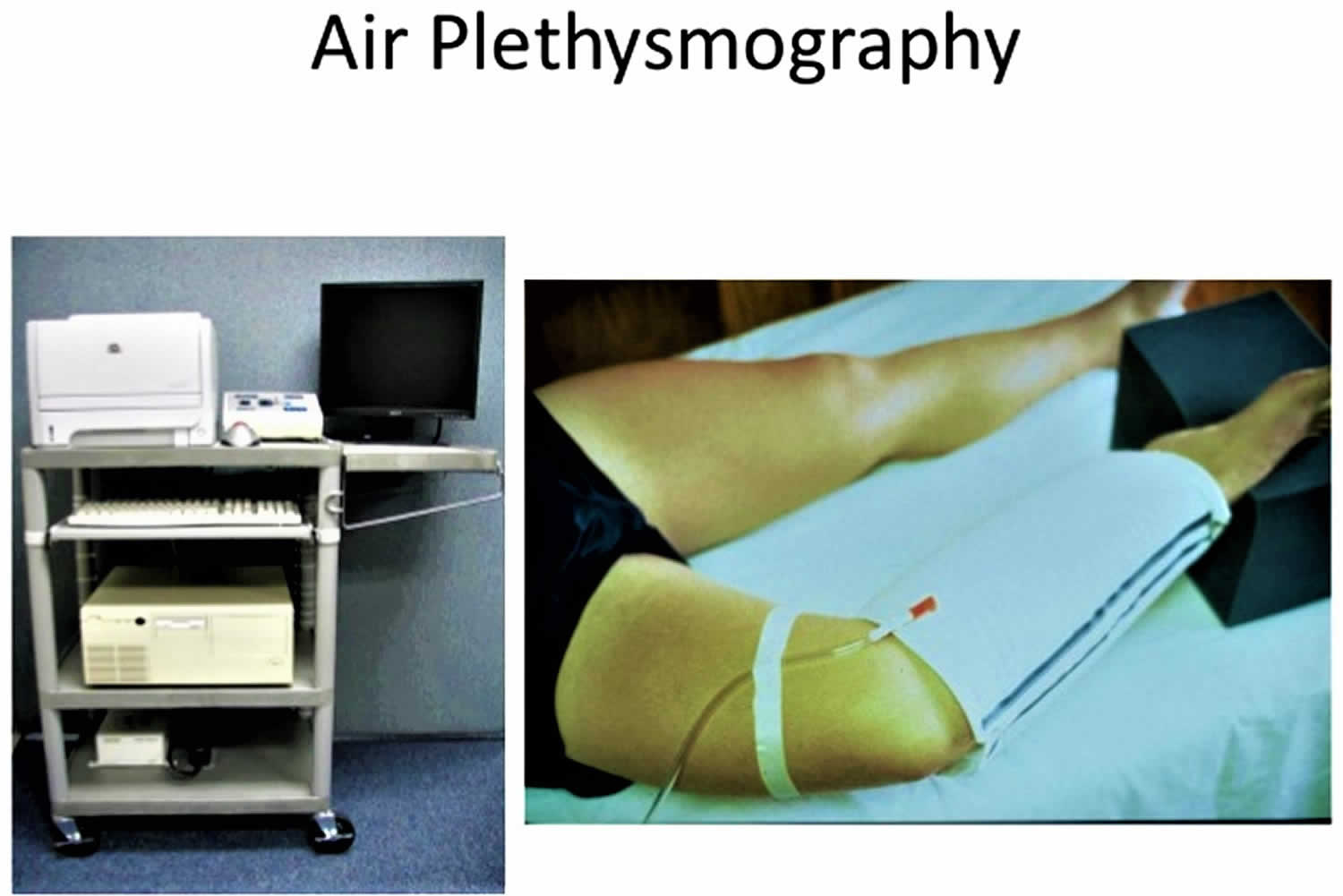
Air plethysmography
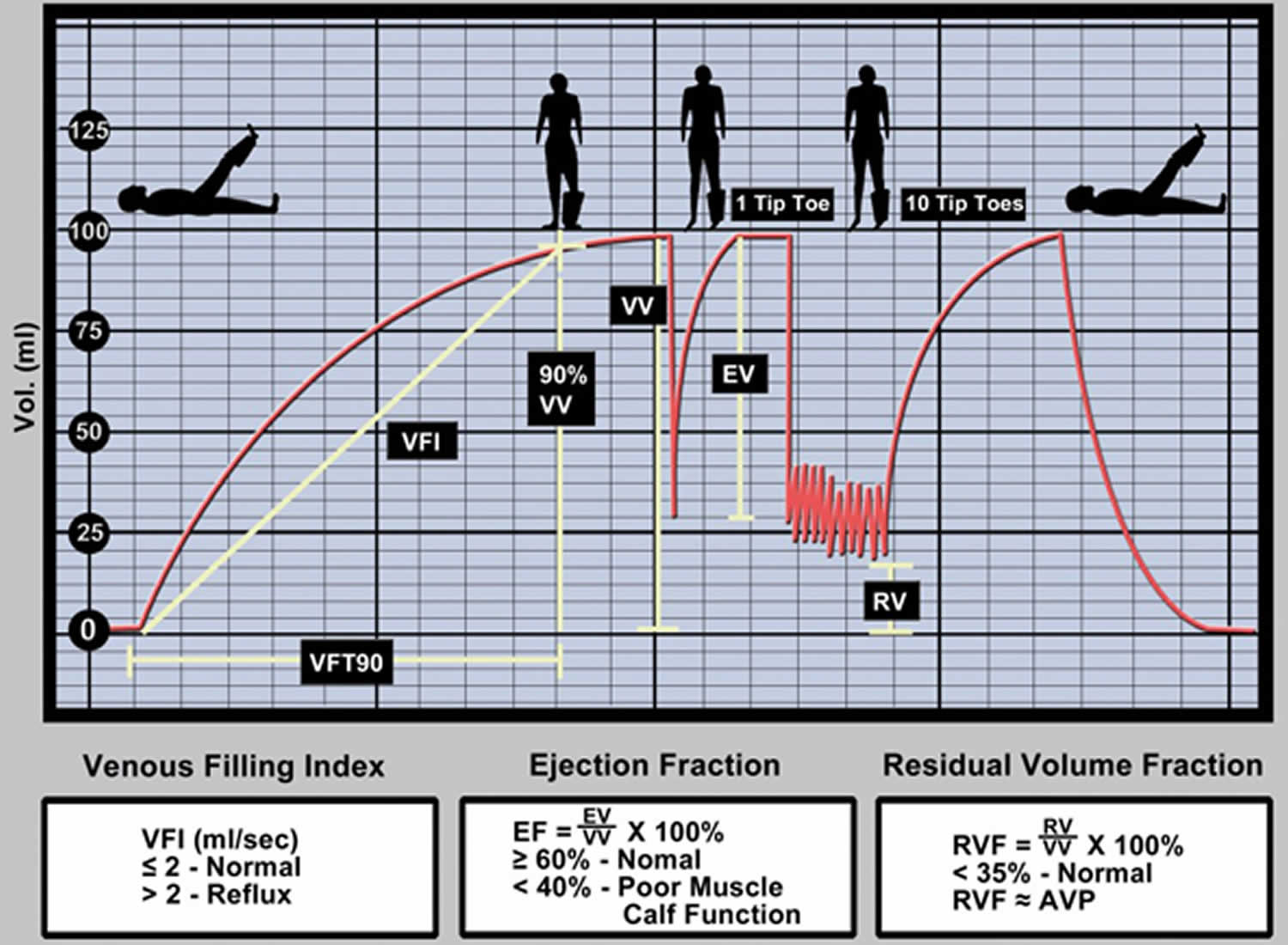
Air-plethysmography consisted of a tubular air chamber that surrounded the whole leg from the knee to the ankle. This was inflated with air and connected to a pressure transducer, amplifier, and recorder. The air-plethysmograph was fitted, with the patient in the supine position and the leg elevated (45 degrees) to empty the veins. A baseline value was obtained and the subject was asked to stand with the weight on the opposite leg. An increase in the leg volume was observed until a plateau was reached, indicating that the veins were full (see Figures 5 and 6).
This increase represents the functional venous volume (VV). The time taken to achieve 90% of filling has been defined as venous filling time 90 (VFT90). The venous filling index (VFI) was obtained from VFI = 90%VV/VFT90.
The subject was then asked to do one tiptoe movement and return to rest (Figure 7). The recorded decrease was the ejected volume (EV) resulting from the calf muscle contraction. After a new plateau was reached, the subject did 10 tiptoe movements at the rate of one per second (Figure 7). A volume decrease to a new steady state was observed. The residual volume (RV) was calculated from the original base-line and the volume at the end of exercise. The ejection fraction (EF) was derived from EF = (EV/VV) × 100 and the residual volume fraction (RVF) from RVF = (RV/VV) × 100.
Air-plethysmography is a non-invasive diagnostic tool that quantifies the physiological components of chronic venous disease including:
- Chronic obstruction
- Valvular reflux
- Calf muscle pump function
- Venous hypertension
Air-plethysmography has been recently reported as a new noninvasive technique that can measure the venous volume of the leg (expressed in milliliters), venous reflux (in milliliters per second), and the ejecting capacity of the calf muscle pump as a result of one tiptoe movement (ejection fraction) or continuous exercise (residual volume fraction) 10. Results of air-plethysmography have been shown to correlate well with ambulatory venous pressure 11 and venous reflux measurements with the severity of the clinical symptoms 12.
The test protocol for the air-plethysmography has three phases:
- First, the patient is supine and outflow testing identifies obstruction and the degree of superficial collateralization.
- Next, the patient is asked to stand and the filling rate of the veins by reflux through incompetent valves is measured. The patient is then asked to do a toe-up exercise and the calf muscle pump function is measured as an ejection fraction.
- Finally, the patient does 10 toe-ups quickly and a non-invasive measure of ambulatory venous pressure is completed.
The presence of chronic obstruction usually indicates a post-thrombotic limb. If the saphenous system is measured to be the limb’s primary outflow collateral by the air-plethysmography, its removal may become problematic for the patient. Reflux in the deep and superficial veins are separately quantified to allow the physician to understand how the two systems contribute to the patient’s symptoms. Poor calf muscle pump function may be due to obstruction, varicose veins calf perforator reflux or the patient’s inability to perform exercise from arthritis, stroke, etc. Air-plethysmography is now used in studies to identify patients for the new subfacial endoscopic perforator surgery. Both reflux and poor calf pump function are related to clinical manifestations of the disease.
Figure 5. Air-plethysmography
Figure 6. Air-plethysmography graph
Abbreviations: VC = venous capacitance; LSV = long saphenous vein; VV = Functional venous volume; VFT = venous filling time; VFI = venous filling index; EV= ejected volume; RV = residual volume; EF = ejection fraction; RVF = residual volume fraction.
Figure 7. Air-plethysmography graph results
Footnote: Diagrammatic representation of typical recording of volume changes during standard sequence of postural changes and exercise. Patient in supine position with leg elevated 45 degrees (a); patient standing with weight on nonexamined leg (b); single tiptoe movement (c); 10 tiptoe movements (d); same as in (b).
Abbreviations: VC = venous capacitance; LSV = long saphenous vein; VV = Functional venous volume; VFT = venous filling time; VFI = venous filling index; EV= ejected volume; RV = residual volume; EF = ejection fraction; RVF = residual volume fraction.
References- Shaw G., Kerr A. (2018) Non-imaging Method: Air Displacement Plethysmography (Bod Pod). In: Hume P., Kerr D., Ackland T. (eds) Best Practice Protocols for Physique Assessment in Sport. Springer, Singapore
- Body plethysmography–its principles and clinical use. Criée CP, Sorichter S, Smith HJ, Kardos P, Merget R, Heise D, Berdel D, Köhler D, Magnussen H, Marek W, Mitfessel H, Rasche K, Rolke M, Worth H, Jörres RA, Working Group for Body Plethysmography of the German Society for Pneumology and Respiratory Care. Respir Med. 2011 Jul; 105(7):959-71. https://www.resmedjournal.com/article/S0954-6111(11)00055-2/fulltext
- Lommatzsch M, Virchow CJ. Severe asthma: definition, diagnosis and treatment. Dtsch Arztebl Int. 2014;111:847–855.
- Burkhardt R, Pankow W. The diagnosis of chronic obstructive pulmonary disease. Dtsch Arztebl Int. 2014;111:834–845
- Vogelmeier C, Buhl R, Criee CP, et al. Leitlinie der Deutschen Atemwegsliga and Deutschen Gesellschaft fur Pneumologie und Beatmungsmedizin zur Diagnostik und Therapie von Patienten mit chronisch obstruktiver Bronchitis und Lungenemphysem. Pneumologie. 2007;61:e1–e40.
- Enright P. Spirometer + body box = VW beetle + Mercedes? Respir Med. 2011;105:957–958.
- Decramer M, Janssens W, Derom E, et al. Contribution of four common pulmonary function tests to diagnosis of patients with respiratory symptoms: a prospective cohort study. Lancet Respir Med. 2013;1:705–713.
- Schneider A, Schwarzbach J, Faderl B, Hautmann H, Jörres RA. Whole-Body Plethysmography in Suspected Asthma: A Prospective Study of Its Added Diagnostic Value in 302 Patients. Dtsch Arztebl Int. 2015;112(24):405-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4500056/
- Body plethysmography – Its principles and clinical use. Criée, C.P. et al. Respiratory Medicine , Volume 105 , Issue 7 , 959 – 971 https://www.resmedjournal.com/article/S0954-6111(11)00055-2/fulltext
- Objective noninvasive evaluation of venous surgical results. Christopoulos, D. et al. Journal of Vascular Surgery , Volume 8 , Issue 6 , 683 – 687 https://www.jvascsurg.org/article/0741-5214(88)90075-4/fulltext
- Christopoulos, D, Nicolaides, AN, Szendro, G, Irvine, AT, Bull, ML, and Eastcott, HHG. Air-plethysmography and the effect of elastic compression on venous hemodynamics of the leg. J Vasc Surg. 1987; 5: 148–159
- Christopoulos, D, Nicolaides, AN, and Szendro, G. Venous reflux: quantification and correlation with the clinical severity of chronic venous disease. Br J Surg. 1988; 75: 352–356