Reflux nephropathy
Reflux nephropathy is kidney scarring caused by urine flowing backward from the bladder into a ureter and toward a kidney. Reflux nephropathy was previously called chronic pyelonephritis as it was believed to result from childhood recurrent urinary tract infections (UTIs). Reflux nephropathy occurs in approximately 1% to 3% of children and is associated with 7% to 17% of children developing the end-stage renal disease (ESRD) across the world 1. Reflux nephropathy may account for up to 10% of end-stage renal disease caueses in adult patients. Reflux nephropathy is often found when a child is checked for repeated bladder infections. If vesicoureteral reflux is discovered, the child’s siblings may also be checked, because reflux can run in families.
In children, reflux nephropathy can be acquired or congenital. Acquired urinary tract infection is more common among female children and is diagnosed mostly after febrile urinary tract infection. Whereas, the congenital reflux nephropathy is diagnosed during antenatally diagnosed hydronephrosis follow-up, with no prior urinary tract infection and is more common in male children.
Reflux nephropathy often presenting in early adulthood with various clinical manifestations of chronic kidney disease, has pathological findings of patchy interstitial scarring, tubular atrophy, and loss of nephron mass 2. Reflux nephropathy is often detected during a routine evaluation in early adulthood or during pregnancy 3.
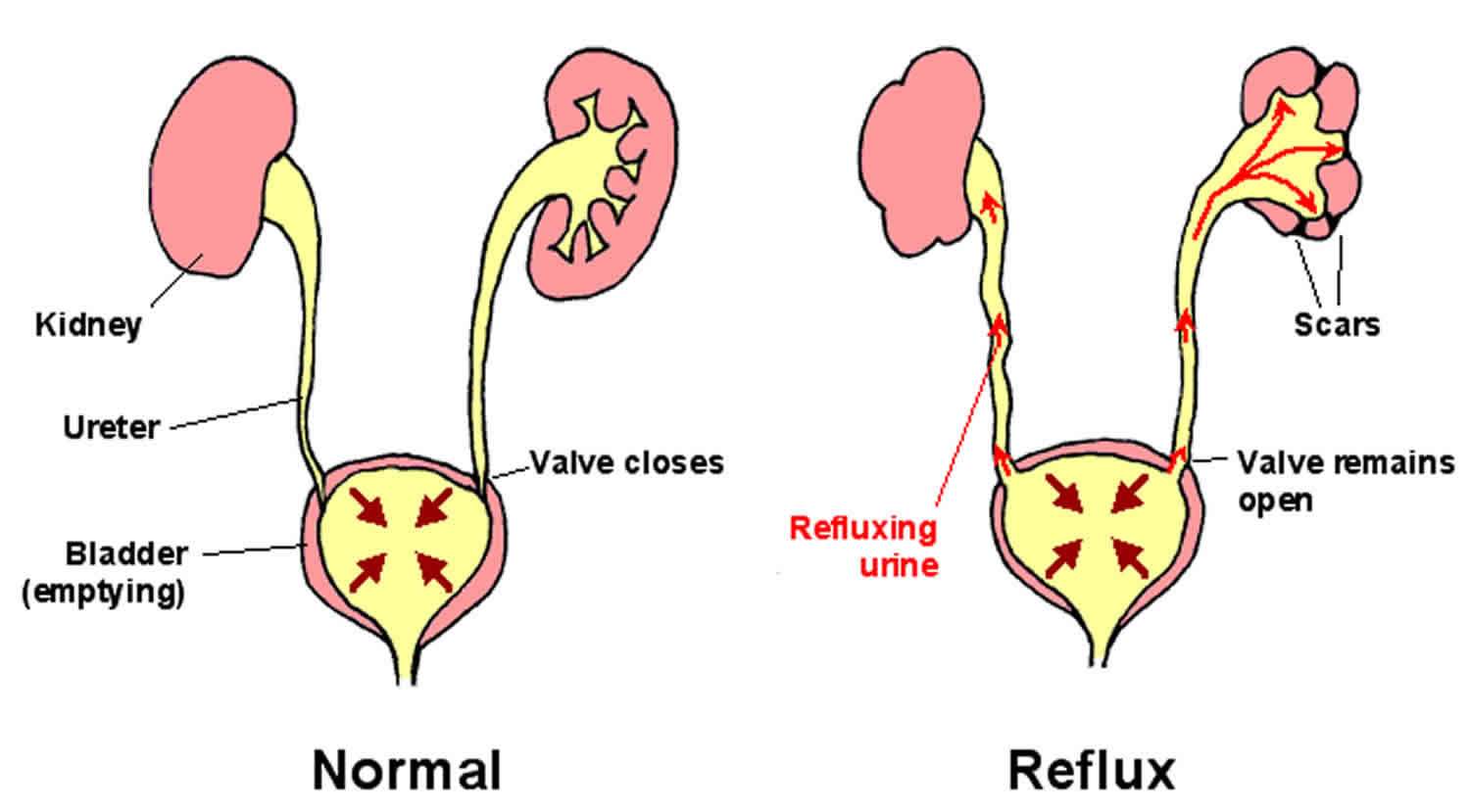
Normally, where the bladder and the ureter join, the ureter tunnels slightly sideways through the bladder wall. The muscles of the bladder wall help keep the end of the ureter shut so that urine flows in only one direction—from the ureter into the bladder. Some people are born with abnormalities of the junction between the ureter and bladder that allow the urine to flow backward during urination—from the bladder into the ureters. This condition is called vesicoureteral reflux (VUR). It can occur in one or both ureters. The backward flow of urine makes urinary tract infections (UTIs) more likely to develop and to cause kidney inflammation and scarring, a condition called reflux nephropathy.
About 30 to 45% of children and about 1% of newborns who have a urinary tract infection that causes a fever have vesicoureteral reflux. Vesicoureteral reflux sometimes tends to run in families and is less common among blacks. Children usually outgrow vesicoureteral reflux by about age 5 years.
The exact incidence and prevalence of reflux nephropathy are not known 2. Reflux nephropathy is primarily a disorder of childhood or early adulthood and is more common in females than males. Vesicoureteral reflux (VUR) may be a familial disorder affecting 20% of infants who have a parent with a family history of vesicoureteral reflux, compared with a 1% to 2% frequency of vesicoureteral reflux in the general population 4. Hypertension occurs in 10% to 30% of children and young adults with reflux nephropathy 5. It is estimated that reflux nephropathy is responsible for 12% to 21% of all children with chronic renal failure 6. Reflux nephropathy is the second most common cause of chronic tubulointerstitial disease. Based on the North American Pediatric Renal Transplant Cooperative Study annual report for 2008, 3.5% of the 6,491 children on dialysis had reflux nephropathy 7. Reflux nephropathy is the fourth most common cause of end-stage renal disease in children after focal segmental glomerulosclerosis, renal aplasia, hypoplasia or dysplasia an, obstructive uropathy and is responsible for the end-stage renal disease in 7% to 17% of the children worldwide 1.
In pregnant females with vesicoureteral reflux, approximately 40% of the offspring will have the condition, and testing of offspring is highly recommended.
Vesicoureteral reflux causes no symptoms, but children with vesicoureteral reflux tend to have repeated urinary tract infections. Reflux nephropathy causes no symptoms. Occasionally, children with reflux nephropathy develop chronic kidney disease, sometimes during adolescence.
Doctors suspect vesicoureteral reflux in the following children:
- Those with a urinary tract infection at age 3 years or younger
- Those with urinary tract infection and fever at age 5 years or younger
- Those with repeated urinary tract infections
- Boys at any age with a urinary tract infection
Doctors sometimes also suspect vesicoureteral reflux in children with close relatives who have the disorder and in children or adults who have repeated urinary tract infections and in whom imaging tests show kidney scarring.
Doctors may suspect that a fetus has vesicoureteral reflux if routine prenatal ultrasonography shows a swollen kidney (called hydronephrosis).
When they suspect vesicoureteral reflux, doctors may do imaging tests to look for abnormalities of the kidneys and ureters that can cause vesicoureteral reflux as well as any kidney damage that may have resulted. These tests may include ultrasonography, voiding cystourethrography, and radionuclide cystourethrography. If vesicoureteral reflux has resolved but resulted in scarring, the scarring may be visible on the imaging tests.
Vesicoureteral reflux is separated into five different grades. Simple or mild reflux often falls into grade 1 or 2. The severity of the reflux and amount of damage to the kidney help determine treatment.
Simple, uncomplicated vesicoureteral reflux (called primary reflux) can be treated with:
- Antibiotics taken every day to prevent urinary tract infections
- Careful monitoring of kidney function
- Repeated urine cultures
- Yearly ultrasound of the kidneys
Controlling blood pressure is the most important way to slow kidney damage. The health care provider may prescribe medicines to control high blood pressure. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are often used.
Surgery is usually only used in children who have not responded to medical therapy.
More severe vesicoureteral reflux may need surgery, especially in children who do not respond to medical therapy. Surgery to place the ureter back into the bladder (ureteral reimplantation) can stop reflux nephropathy in some cases.
More severe reflux may need reconstructive surgery. This type of surgery may reduce the number and severity of urinary tract infections.
If needed, people will be treated for chronic kidney disease.
Reflux nephropathy key points
- Reflux nephropathy is a relatively common condition and is usually asymptomatic but often presents in early adulthood and women of childbearing age.
- Reflux nephropathy is a direct consequence of abnormal retrograde flow of urine from the bladder into one or both the ureters lead to vesicoureteral reflux (VUR).
- Reflux nephropathy is the second most common cause of chronic tubulointerstitial disease and fourth common cause of end-stage renal disease (ESRD) in children.
- Patients present with signs and symptoms of chronic kidney disease and hypertension.
- Pregnant females with reflux nephropathy may have accelerated hypertension, renal impairment and might lead to maternofetal comorbidities.
- Early diagnosis and appropriate management of reflux nephropathy are important for preserving the renal function.
- The mainstay of treatment is the prevention and management of hypertension and chronic kidney disease.
- Various modalities of renal replacement therapy can be used, but renal transplantation offers better long-term outcomes.
Reflux nephropathy in adults
The incidence of end-stage renal disease from reflux nephropathy is unknown in the worldwide adult population. About 12% of patients in Europe requiring treatment for end-stage renal disease may have reflux nephropathy. A study of 127 adults (mean age of 41 years) with a diagnosis of vesicoureteral reflux in childhood, 35% had unilateral renal scarring, 24% had bilateral renal scarring, 24% had albuminuria, and 11% had hypertension. In the patients with bilateral renal scars, 83% had reduced eGFR 8. In countries like Turkey, reflux nephropathy accounts for 18.5% of the causes of chronic kidney disease (CKD).
Reflux nephropathy causes
Urine flows from each kidney through tubes called ureters and into the bladder. When the bladder is full, it squeezes and sends the urine out through the urethra. No urine should flow back into the ureter when the bladder is squeezing. Each ureter has a one-way valve where it enters the bladder that prevents urine from flowing back up the ureter. But in some people, urine flows back up to the kidney, which is a direct consequence of incompetent and mislocated ureterovesical valves. The abnormal backward flow of urine from the bladder into one or both the ureters is called vesicoureteral reflux (VUR). Over time, the kidneys may be damaged or scarred by this reflux. Reflux nephropathy is a direct consequence of vesicoureteral reflux (VUR) or other urologic congenital anomalies stemming from chronic high-pressure sterile urine reflux and often leads to recurrent urinary tract infections (urinary tract infections) in the early childhood. It is important to understand that not all patients with urinary tract infections and vesicoureteral reflux develop reflux nephropathy.
Reflux can occur in people whose ureters do not attach properly to the bladder or whose valves do not work well. Children may be born with this problem or may have other birth defects of the urinary system that cause reflux nephropathy.
Reflux nephropathy can occur with other conditions that lead to a blockage of urine flow, including:
- Bladder outlet obstruction, such as an enlarged prostate in men
- Bladder stones
- Neurogenic bladder, which can occur in people with multiple sclerosis, spinal cord injury, diabetes, or other nervous system (neurological) conditions
Reflux nephropathy can also occur from swelling of the ureters after a kidney transplant or from injury to the ureter.
Risk factors for reflux nephropathy
Risk factors for reflux nephropathy include:
- Abnormalities of the urinary tract
- Personal or family history of vesicoureteral reflux
- The severity of vesicoureteral reflux
- Repeat urinary tract infections.
- Bladder-bowel dysfunction.
- Younger age
- Delay in the treatment of urinary tract infection.
Reflux nephropathy pathophysiology
Vesicoureteral reflux leads to high-pressure sterile urine reflux which stunts the normal growth of the kidneys and often exacerbated by the recurrent childhood infections. Not all urinary tract infections with vesicoureteral reflux lead to reflux nephropathy because of the architecture of the renal pyramids. Renal pyramids are of two types, simple and compound. Compound pyramids promote intrarenal reflux combined with vesicoureteral reflux which leads to reflux nephropathy, given transmission of high-pressure urine and infection to gain access to the renal parenchyma.
Vesicoureteral reflux ultimately results in the chronic interstitial nephritis, tubular atrophy, and renal scarring along with glomerular hypertrophy and secondary focal segmental glomerular sclerosis (FSGS).
Reflux nephropathy histopathology
Grossly the kidneys are small and irregularly contracted, with renal pelves and ureteral dilation with thickened walls. In the appropriate clinical setting, the following findings can be seen in the renal biopsy,
- Global glomerular hypertrophy and periglomerular fibrosis
- Chronic interstitial nephritis
- Patchy interstitial scarring
- Extensive tubular atrophy
- Secondary focal segmental glomerulosclerosis
Reflux nephropathy prevention
Quickly treating conditions that cause reflux of urine into the kidney may prevent reflux nephropathy.
Reflux nephropathy symptoms
Some people have no symptoms of reflux nephropathy. The problem may be found when kidney tests are done for other reasons.
If symptoms do occur, they might be similar to those of:
- Chronic kidney failure
- Nephrotic syndrome
- Urinary tract infection.
Children with vesicoureteral reflux and their parents should be aware of the symptoms of urinary tract infection, which can vary by age. They may include fever, vomiting, burning during urination, and inability to control the bladder.
Based on the age of presentation, the patients may have the following,
- History of recurrent childhood urinary tract infections
- Prolonged bedwetting
- Complicated urinary infection: Acute pyelonephritis in infants and children
- History of surgical reimplantation of the ureters into the bladder
- Hypertension on presentation 9
- Abnormal renal function with elevated serum creatinine and estimated glomerular filtration rate (eGFR)
- Episodes of fluctuating renal function
- Mild to moderate proteinuria
- Severe or nephrotic proteinuria may be from secondary focal segmental glomerulosclerosis, which can be confirmed by renal biopsy 10
- Urinary calculi
- Asymptomatic Bacteriuria in pregnancy 11
- In pregnancy: Urinary infection, hypertension, and preeclampsia 12
- Approximately 20% of women with reflux nephropathy will develop urinary tract infection in pregnancy, with around 6% of these from acute pyelonephritis
- Small kidneys with thinned cortices on renal ultrasound in asymptomatic young patients with hypertension
- Bilateral hydronephrosis on the renal ultrasonogram
- Urinary tract infections may be more common in adults who have had the surgical management of vesicoureteral reflux
Reflux nephropathy complications
The complications of reflux nephropathy are well known but poorly defined because of their insidious onset and slow progression 13.
Complications that may result from reflux nephropathy or its treatment include:
- Blockage of the ureter after surgery
- Chronic kidney disease
- Chronic or repeat urinary tract infections
- Chronic kidney failure if both kidneys are involved (can progress to end-stage kidney disease)
- Kidney infection
- High blood pressure
- Nephrotic syndrome
- Persistent reflux
- Scarring of the kidneys
- Early growth retardation is observed from recurrent cystitis and pyelonephritis in children affected with vesicoureteral reflux and later on with reflux nephropathy. Increased maternal complications are noted 14
- Suddenly-accelerated hypertension with associated renal impairment during pregnancy 15
- Fetal morbidity in women with reflux with renal scarring 16
Patients with reflux nephropathy will develop hypertension, proteinuria, urine concentration defects, hyperkalemia, acidosis (type 1 Renal tubular acidosis) and chronic kidney disease (CKD). Progressive chronic kidney disease can lead to end-stage renal failure. Chronic kidney disease from reflux nephropathy leads to increased cardiovascular mortality and morbidity.
Reflux nephropathy diagnosis
Reflux nephropathy is often found when a child is checked for repeated bladder infections. If vesicoureteral reflux is discovered, the child’s siblings may also be checked, because reflux can run in families.
Blood pressure may be high, and there may be signs and symptoms of long-term (chronic) kidney disease.
Blood and urine tests will be done, and may include:
- BUN (blood urea nitrogen)
- Creatinine — blood
- Creatinine clearance — urine and blood
- Urine protein to creatinine ratio
- Urinalysis or 24-hour urine studies
- Urine culture
Imaging tests that may be done include:
- Abdominal CT scan
- Bladder ultrasound
- Intravenous pyelogram (IVP)
- Kidney ultrasound
- Radionuclide cystogram (DMSA Scan)
- Retrograde pyelogram
- Voiding cystourethrogram (VCU)
Renal ultrasound is the most common and usually first evaluation of postnatal hydronephrosis and urinary tract infection in children. Renal renal ultrasound should be used for siblings of children with vesicoureteral reflux. renal ultrasound is less sensitive for diagnosis of acute pyelonephritis. Though helpful in renal abscess detection and perinephric space abnormalities, it is not diagnostic for vesicoureteral reflux and is not sensitive for renal scars diagnosis.
Diagnostic voiding cystourethrogram (VCU) is useful in patients with bilateral or unilateral hydronephrosis on the renal renal ultrasound in a patient with the appropriate clinical presentation. It is the primary diagnostic modality for identification of vesicoureteral reflux.
Nuclear cystography can be used to prevent radiation exposure in patients with post-surgical vesicoureteral reflux follow up. Sensitive than voiding cystourethrogram, but does not aid in the specific grading of vesicoureteral reflux or detection of other anatomic defects, for example, ureterocele and diverticulum
DMSA Scan (a radionuclide scan using dimercaptosuccinic acid) is highly sensitive and the gold standard for the diagnosis of acute pyelonephritis and renal scarring 17.
Magnetic resonance imaging (MRI), can be used to diagnose renal scarring as it differentiates swelling from scarring, unlike a DMSA scan. Not practical for use in infants and children, moreover cost is a hindrance.
Renal biopsy aids in both diagnosis and for prognostication.
Reflux nephropathy treatment
Low-grade vesicoureteral reflux typically resolves spontaneously over time, but in the meantime, it is very important to maintain sterile urine in affected individuals in childhood. In patients with symptomatic vesicoureteral reflux, two main treatment modalities include long-term antimicrobial prophylaxis, prompt treatment of urinary tract infections, and surgical correction.
Prophylactic antibiotics should be used depending on the frequency of urinary tract infections, the age of the child and the severity of the vesicoureteral reflux. Appropriate agents include trimethoprim-sulfamethoxazole, trimethoprim alone, nitrofurantoin, and cephalexin. It is crucial to pay attention to the management of bladder and bowel dysfunction, with the following:
- Laxatives and stool softeners
- Frequent and timed voiding (2 to 3 hours)
- Pelvic floor exercises
- Behavioral modification
- Anticholinergic medications as needed
In chronic and severe vesicoureteral reflux, surgical reimplantation of the ureters into the bladder to maintain the competency of the ureters is indicated. It is most beneficial in patients with failed medical management (antimicrobial prophylaxis) to prevent urinary tract infections. Surgery has no role in adolescents and adults with established renal scarring and markers of advanced chronic kidney disease.
Surgical indications include:
- Recurrent infections despite compliance with a prophylactic antibiotic regimen
- Worsening of renal scars on DMSA scan
- Non-adherence to the antibiotic prophylaxis
In patients with established reflux nephropathy, it is very important to prevent and aggressive management of hypertension. Appropriate use of Renin-angiotensin system (RAS) blockade in patients with glomerular hyperfiltration and patients with established proteinuria.
Various modalities of renal replacement therapies can be employed in patients who reach end-stage renal disease. Despite the higher incidence of urinary tract infection’s, there was no significant difference in posttransplantation complications or patient and graft survival rates between reflux nephropathy patients compared with the control group 18.
Reflux nephropathy prognosis
Outcome varies, depending on the severity of the reflux. Some people with reflux nephropathy will not lose kidney function over time, even though their kidneys are damaged. However, kidney damage may be permanent. If only one kidney is involved, the other kidney should keep working normally. Advanced age at presentation and bilateral vesicoureteral reflux decreases the probability of resolution.
High grade and severity of the vesicoureteral reflux have lesser chances of spontaneous resolution 19. Proteinuria predicts chronic kidney disease progression in patients with reflux nephropathy 20.
Reflux nephropathy may cause kidney failure in children and adults.
References- Hodson EM, Wheeler DM, Vimalchandra D, Smith GH, Craig JC. Interventions for primary vesicoureteric reflux. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD001532
- Aeddula NR, Baradhi KM. Reflux Nephropathy. [Updated 2019 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526055
- Zucchelli P, Gaggi R. Reflux nephropathy in adults. Nephron. 1991;57(1):2-9.
- Scott JE, Swallow V, Coulthard MG, Lambert HJ, Lee RE. Screening of newborn babies for familial ureteric reflux. Lancet. 1997 Aug 09;350(9075):396-400.
- Smellie JM, Prescod NP, Shaw PJ, Risdon RA, Bryant TN. Childhood reflux and urinary infection: a follow-up of 10-41 years in 226 adults. Pediatr. Nephrol. 1998 Nov;12(9):727-36.
- Deleau J, Andre JL, Briancon S, Musse JP. Chronic renal failure in children: an epidemiological survey in Lorraine (France) 1975-1990. Pediatr. Nephrol. 1994 Aug;8(4):472-6.
- Roihuvuo-Leskinen H, Lahdes-Vasama T, Niskanen K, Rönnholm K. The association of adult kidney size with childhood vesicoureteral reflux. Pediatr. Nephrol. 2013 Jan;28(1):77-82.
- Lahdes-Vasama T, Niskanen K, Rönnholm K. Outcome of kidneys in patients treated for vesicoureteral reflux (VUR) during childhood. Nephrol. Dial. Transplant. 2006 Sep;21(9):2491-7.
- Diamond DA, Mattoo TK. Endoscopic treatment of primary vesicoureteral reflux. N. Engl. J. Med. 2012 Mar 29;366(13):1218-26.
- Morita M, Yoshiara S, White RH, Raafat F. The glomerular changes in children with reflux nephropathy. J. Pathol. 1990 Nov;162(3):245-53.
- Mor Y, Leibovitch I, Zalts R, Lotan D, Jonas P, Ramon J. Analysis of the long-term outcome of surgically corrected vesico-ureteric reflux. BJU Int. 2003 Jul;92(1):97-100.
- Jungers P. Reflux nephropathy and pregnancy. Baillieres Clin Obstet Gynaecol. 1994 Jun;8(2):425-42.
- Mattoo TK. Vesicoureteral reflux and reflux nephropathy. Adv Chronic Kidney Dis. 2011 Sep;18(5):348-54.
- Köhler JR, Tencer J, Thysell H, Forsberg L, Hellström M. Long-term effects of reflux nephropathy on blood pressure and renal function in adults. Nephron Clin Pract. 2003 Jan;93(1):C35-46.
- Phelan ST. Renal disease in pregnancy ambulatory issues. Clin Obstet Gynecol. 2012 Sep;55(3):829-37.
- Hollowell JG. Outcome of pregnancy in women with a history of vesico-ureteric reflux. BJU Int. 2008 Sep;102(7):780-4.
- Lavocat MP, Granjon D, Allard D, Gay C, Freycon MT, Dubois F. Imaging of pyelonephritis. Pediatr Radiol. 1997 Feb;27(2):159-65.
- Yazici H, Caliskan Y, Ozturk S, Ozkan O, Turkmen A, Sever MS. Outcome of kidney transplantation following end-stage renal disease due to reflux nephropathy. Transplant. Proc. 2011 Jun;43(5):1566-9.
- Elder JS, Peters CA, Arant BS, Ewalt DH, Hawtrey CE, Hurwitz RS, Parrott TS, Snyder HM, Weiss RA, Woolf SH, Hasselblad V. Pediatric Vesicoureteral Reflux Guidelines Panel summary report on the management of primary vesicoureteral reflux in children. J. Urol. 1997 May;157(5):1846-51.
- Torres VE, Velosa JA, Holley KE, Kelalis PP, Stickler GB, Kurtz SB. The progression of vesicoureteral reflux nephropathy. Ann. Intern. Med. 1980 Jun;92(6):776-84.