Steatorrhea
Steatorrhea or steatorrhoea, is fatty stools or an increase in fat excretion in the stools 1. An increase in the fat content of stools results in the production of pale, large volume, malodorous, loose stools. Patients with steatorrhea present with bulky, pale, foul-smelling oily stools. These fatty stools tend to float in the toilet bowl and often challenging to flush as well. Steatorrhea is one of the clinical features of fat malabsorption and noted in many conditions such as exocrine pancreatic insufficiency, celiac disease, and tropical sprue 1. Screening for steatorrhea may be carried out by examining stool samples for the presence of fat by Sudan III staining. However, quantitative fecal fat estimation is required to confirm the diagnosis.
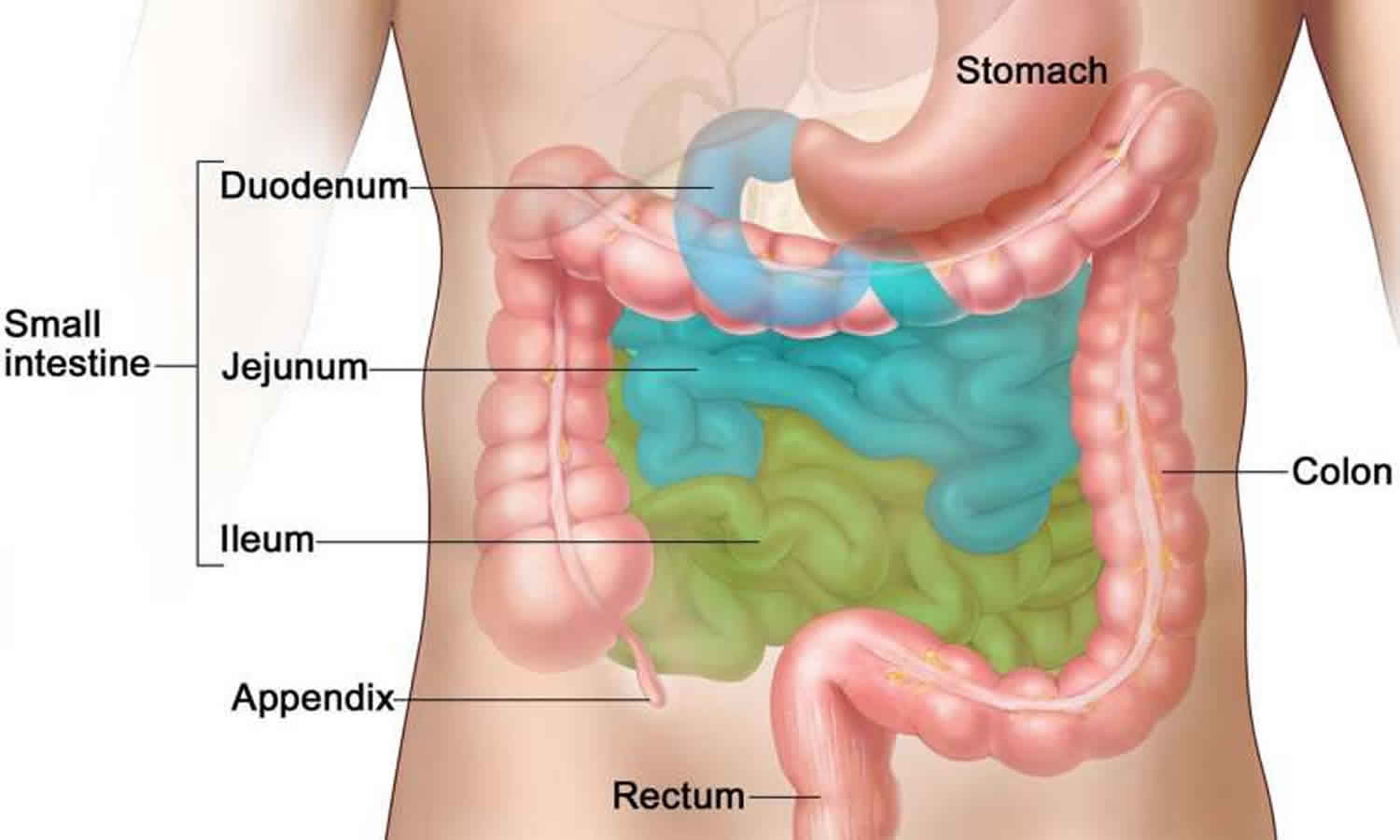
Among the macronutrients, digestion and absorption of fat involve a complex mechanism. Fat absorption requires bile acids, digestive enzymes, and a normally functioning small intestinal mucosa. Dietary lipids, mostly as triacylglycerols, are initially emulsified by bile acids and then hydrolyzed by the pancreatic lipases and colipases into free fatty acids and monoglycerides. In the proximal small bowel, these hydrolyzed lipids form micelles by the action of bile acids. The micelles are then absorbed across the intestinal villi and transported as chylomicrons via the intestinal lymphatics. Therefore, any defects in the availability or function of bile acids, pancreatic digestive enzymes or absorptive villi will lead to steatorrhea 2.
In the early stages, steatorrhea may be unrecognized by many patients due to minimal or nonspecific presenting symptoms. Therefore, the exact prevalence and incidence of steatorrhea are challenging to estimate and often go underreported 1.
In adults, chronic pancreatitis is the most common cause of exocrine pancreatic insufficiency. Chronic pancreatitis has an annual incidence of approximately 4 per 100,000 persons and a prevalence of about 42 per 100,000 individuals in the U.S. 3. In children, cystic fibrosis accounts for most cases of exocrine pancreatic insufficiency. cystic fibrosis is the most common lethal autosomal recessive condition affecting the White population 4. The approximate prevalence of cystic fibrosis is 1 in 3000 births. About 85% of cystic fibrosis patients have pancreatic insufficiency 4.
The prevalence of the celiac disease is on the rise, and a recent study reported a global seroprevalence of 1.4% 5. Also, there are differences in the prevalence depending on geographical location. Reports of a biopsy-proven celiac disease show lower prevalence rates in South America and Africa and higher rates in Europe and Oceania 5. For example, in Europe, Germany has a lower prevalence of celiac disease, and the highest prevalence was in Sweden and Finland 5. Celiac disease has a higher prevalence in certain high-risk groups such as type 1 diabetes mellitus, Down syndrome, Turner syndrome, IgA deficiency, William’s syndrome, and in first-degree relatives of celiac disease 6.
Based on a study from the Netherlands, primary biliary cholangitis had an incidence of 1.1 per 100,000 (male to female ratio was 1 to 6.3), and the point prevalence was 13.2 per 100,000 individuals in 2008 7. Another study from the U.S. reported an overall incidence of primary biliary cholangitis as 2.7 per 100,000 person-years and age and sex-adjusted prevalence of 40 per 100,000 with a similar female predilection 8. primary sclerosing cholangitis has a prevalence rate depending on the geographical location. A systematic review reported the incidence and prevalence rates of primary sclerosing cholangitis ranging from 0 to 1.3 per 100000 people per year and 0 to 16 per 100000 people, respectively 9. As there is no consensus on the definition of SIBO (small intestinal bacterial overgrowth), its exact prevalence is unknown 10.
Steatorrhea causes
The causes of steatorrhea are numerous and subclassify under three broad categories:
- Conditions leading to exocrine pancreatic insufficiency,
- Bile acid deficiency states, and
- Diseases affecting the small intestine.
Most notable disorders in each category are given below 11:
- Exocrine pancreatic insufficiency due to chronic pancreatitis, cystic fibrosis (CF), and conditions resulting in pancreatic duct obstruction or resection of the pancreas (e.g., pancreatic tumors)
- Bile acid deficiency either due to cholestasis (e.g. primary biliary cirrhosis, currently referred as primary biliary cholangitis, primary sclerosing cholangitis) or inability to absorb bile acids in the distal ileum resulting in diminished bile acid pool (e.g. ileal resection or Crohn disease of the ileum) or deconjugation of bile acids (e.g., small intestinal bacterial overgrowth [SIBO])
- Diseases affecting proximal small intestines such as celiac disease, tropical sprue, giardiasis, Whipple disease, lymphoma, amyloidosis, SIBO (small intestinal bacterial overgrowth), and HIV enteropathy
Other rare causes of steatorrhea include lipase inhibitors such as orlistat, Zollinger-Ellison syndrome (increased production of gastric acid inactivates the pH-sensitive pancreatic lipases), and graft-versus-host disease 12.
Steatorrhea pathophysiology
- Exocrine pancreatic insufficiency: Chronic exposure to alcohol is the most common etiological factor for chronic pancreatitis. The other notable risk factors for chronic pancreatitis include predisposing genetic mutations (PRSS-1, SPINK-1, CFTR, CTRC), autoimmune pancreatitis, pancreatic duct obstruction, and chronic nicotine exposure 13. The exact pathophysiological pathways underlying chronic pancreatitis are unclear but may include mechanisms such as chronic ongoing parenchymal inflammation with acinar cell destruction, and ductal dysfunction, etc. 13. The histopathological changes include pancreatic atrophy with fibrous scarring, which may be focal or diffuse 14.
- Cystic fibrosis: Cystic fibrosis is a multisystem disease as a result of mutations in the gene which encodes the cystic fibrosis transmembrane conductance regulator (CFTR) 4. In the pancreas, CFTR dysfunction results in thick viscous secretions along with defective bicarbonate flow resulting in exocrine pancreatic insufficiency.
- Cholestatic diseases: The mechanisms underlying the development of chronic cholestatic liver diseases, including primary biliary cholangitis and primary sclerosing cholangitis, are not entirely understood. Both these disorders are characterized by portal inflammation and progressive fibrosis and eventually resulting in end-stage liver disease. Here, the reduction in bile flow results in the accumulation of toxic bile products, which leads to biliary epithelial damage 15. This decrease in bile reaching the small bowel interferes with fat absorption and causes steatorrhea in these patients.
- Celiac disease: It is a chronic autoimmune-mediated enteropathy related to exposure to dietary gluten in genetically susceptible individuals. The genes which encode for major histocompatibility complex (MHC) class II proteins HLA-DQ2 and HLA-DQ8 are prerequisites for this disease. Ingestion of gluten (specifically the gliadin peptides from wheat, rye, and barely) by susceptible individuals, along with some unknown trigger factors, leads to pathogenesis 6. Gliadin polypeptides are resistant to degradation in the gastrointestinal tract and can cross the small intestinal epithelial barrier. In the lamina propria, these peptides get deamidated by local extracellular tissue transglutaminase 6. This deamidation increases the affinity of gliadin binding to the antigen-binding groove of HLA DQ2 or HLA DQ8 on antigen-presenting cells. Upon presentation to CD4+ T lymphocytes, the gliadin peptides trigger an immune response causing local inflammation, which results in the destruction of villi. In addition to adaptive immune dysfunction, patients with celiac disease also have defects in innate intestinal immunity. The histopathological changes include increased intraepithelial lymphocytes, intestinal villous atrophy (blunting or flattening of the villi), and crypt hyperplasia (elongation of the crypts) 16. These changes lead to malabsorption of fats and fat-soluble vitamins.
- SIBO: Under physiological conditions, several defense mechanisms regulate the microbiota in the gastrointestinal tract and prevent small intestine bacterial overgrowth. The significant factors in SIBO prevention include immunoglobin A, gastric acidity, bile, and defensins 17. The aboral peristalsis with migratory motor complexes and an intact ileocaecal valve also play a vital role in preventing SIBO 17. Any disturbances in these mechanisms could result in bacterial overgrowth 17. Deconjugation of bile acids causes fat malabsorption along with other factors such as ongoing inflammation, increased intestinal permeability 17.
Steatorrhea symptoms
Patients with steatorrhea present with bulky, pale, foul-smelling oily stools. These fatty stools tend to float in the toilet bowl and often challenging to flush as well. In the early stages, steatorrhea may be asymptomatic and go unnoticed. Patients also have other nonspecific manifestations of fat malabsorption such as chronic diarrhea, abdominal discomfort, bloating sensation, and weight loss. Children may present with growth failure and delayed puberty. In severe cases, loss of subcutaneous fat and muscle wasting may be evident. Manifestations of fat-soluble vitamin (A, D, E, and K) deficiencies can accompany fat malabsorption. Celiac patients can present with a variety of extraintestinal signs such as anemia, oral ulcers, and dermatitis herpetiformis rash. Abdominal pain is a predominant symptom in patients with chronic pancreatitis but also reported in other conditions such as SIBO (small intestinal bacterial overgrowth), inflammatory bowel disease, and celiac disease. CF patients have sinopulmonary manifestations. Jaundice, fatigue, and pruritis are suggestive of cholestatic liver diseases such as primary biliary cholangitis or primary sclerosing cholangitis. Signs for end-stage liver disease such as splenomegaly, ascites can be noted in primary biliary cholangitis or primary sclerosing cholangitis.
Steatorrhea complications
Steatorrhea complications include:
- Weight loss in adults and other consequences of malnutrition such as increased susceptibility to infections, and increased morbidity and mortality from various disease states. Additionally, in children, malnutrition results in growth failure and poor neurological development
- Deficiencies of fat-soluble vitamins (A, D, E, and K)
- Poor bone health resulting in osteopenia, osteoporosis, and fractures (cystic fibrosis, celiac disease)
- Iron deficiency anemia, zinc deficiency (celiac disease)
- Dermatitis herpetiformis, non-Hodgkin lymphoma, adenocarcinoma of the upper gastrointestinal tract (celiac disease)
- Megaloblastic anemia due to B12 deficiency (in terminal ileum disease and SIBO)
- Pancreatic pseudocyst, ascites, splenic vein thrombosis, diabetes, pancreatic cancer (chronic pancreatitis)
- Seizure, osteopenia, ataxia, early bruising, headache, hyposplenism, and tetany (celiac disease)
- Cirrhosis, end-stage liver disease (primary biliary cholangitis, primary sclerosing cholangitis), malignancies such as cholangiocarcinoma, colon cancer in primary sclerosing cholangitis
Steatorrhea diagnosis
The diagnosis of steatorrhea is based on clinical findings, laboratory tests, and radiological images. Endoscopy with small intestinal biopsy, liver biopsy, and other specialized investigations may be needed to detect the exact cause of steatorrhea.
- Quantitative estimation of fecal fat (exceeding 7 g per 24 hours) is an essential first step for the diagnosis of steatorrhea. The standard method of fecal fat quantification is by calculating the coefficient of fat absorption (CFA).[24] With a standard quantity of fat ingestion, coefficient of fat absorption (CFA) is the percentage of dietary fat that is absorbed 18. Patients should follow a strict diet for five days containing 100 g of fats daily 18. Stools are collected in the last 72-hour for fecal fat estimation. Coefficient of fat absorption (CFA) over 92% is considered normal 18. Even though accurate, this method is cumbersome and unpleasant for most patients. For evaluation of exocrine pancreatic insufficiency, fecal elastase may be utilized instead of the 72-hour fecal fat testing. A value of more than 200 mcg/g of stool is considered normal; 100 to 200 mcg/g as indeterminate, and less than 100 mcg/g is abnormal and indicative of exocrine pancreatic insufficiency. Here the advantage is the requirement of a single stool sample. However, in the early stages of exocrine pancreatic insufficiency, this test has a lower sensitivity. Also, a formed stool is necessary for testing. Otherwise, the fecal elastase could be falsely low due to dilution.
- For evaluation of chronic pancreatitis (1) A plain abdominal radiograph may show pancreatic calcification, (2) Abdominal CT or MRI scans may reveal calcifications of chronic pancreatitis and ductal dilatation, (3) Magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP) can offer more detailed evaluation of pancreatic parenchymal and ductal changes in chronic pancreatitis 19. Similarly, MRCP, ERCP, and endoscopic ultrasound (EUS) are indispensable in the evaluation of pancreatic tumors.
- For evaluation of celiac disease: (1) Estimation of serum tissue transglutaminase IgA antibodies (TTG-IgA) with total serum IgA is the recommended screening test 6. IgA endomysial antibodies (EMA-IgA) has the highest specificity and is an option if transglutaminase IgA antibodies is weakly positive 6. In patients with IgA deficiency, both TTG-IgA and EMA-IgA may be falsely low. In this population, TTG-IgG and deamidated gliadin peptide IgG (DGP-IgG) are the recommendations for screening 6. Patients with positive serological tests should be followed up with duodenal biopsies for confirmation 6.
- In patients suspected to have chronic liver disease: (1) serum liver tests may reflect a cholestatic pattern, (2) elevation of alkaline phosphatase and gamma-glutamyl transferase are frequent findings in both primary biliary cholangitis and PSC (3) AST, ALT, and bilirubin may be normal or elevated (4) Anti-mitochondrial antibodies are noted in 90 to 95% of patients with primary biliary cholangitis 20. Liver biopsy is not routinely needed for the diagnosis of primary biliary cholangitis. If done, a liver biopsy may show the destruction of interlobular bile ducts and cirrhotic changes in the later stages.
- In primary sclerosing cholangitis, magnetic resonance cholangiography (MRC) is the preferred modality and may show a multifocal narrowing of both intrahepatic and extrahepatic biliary ductal strictures. These strictures may be seen alternating with dilation, which is referred to as the “beaded” appearance 21. ERCP or percutaneous transhepatic cholangiography is also helpful to delineate the biliary anatomy in primary sclerosing cholangitis but not routinely utilized for the diagnosis due to their invasiveness 21. In primary sclerosing cholangitis, a liver biopsy is not a routine test, and when done, may demonstrate periductular fibrosis (onion skin fibrosis) 21. Even though specific, this finding is infrequent 21. In primary sclerosing cholangitis, a liver biopsy may be helpful in a few particular circumstances, such as for the evaluation of small duct primary sclerosing cholangitis and also to exclude coexistent autoimmune hepatitis, which is referred to as overlap syndrome 21. About 80% of patients with primary sclerosing cholangitis have inflammatory bowel disease (IBD). Due to this strong association, if previously undiagnosed, a workup for IBD is recommended at the time of diagnosis of primary sclerosing cholangitis.
- Endoscopy with direct aspiration and culture of the small intestinal contents was traditionally the gold standard test for SIBO 10. However, due to its invasive nature and lack of consensus on the definition regarding SIBO, this method is less preferred 10. Breath tests utilizing either glucose or lactulose are commonly used in clinical practice 10.
Steatorrhea treatment
Treatment of steatorrhea depends on the underlying conditions which cause steatorrhea.
- In patients with exocrine pancreatic insufficiency, a pancreatic enzyme replacement therapy (PERT) is the cornerstone of treatment 22. Along with pancreatic enzyme replacement therapy , patients with exocrine pancreatic insufficiency should receive normal to a high-fat diet and fat-soluble vitamin supplementation 12. Fat restriction may improve the symptoms associated with steatorrhea but will worsen the nutritional status and is no longer a recommendation.
- In patients with SIBO (small intestinal bacterial overgrowth), an empiric trial of antibiotics is recommended. In many institutions, rifaximin is preferable to other antibiotics such as ciprofloxacin, metronidazole, norfloxacin, doxycycline, and amoxicillin-clavulanic acid 17.
- In patients with celiac disease, diet-centered recommendations include a strict life-long gluten-free diet, education about the disease, management of nutritional deficiencies, access to an advocacy group, and consultation with a skilled dietitian 16.
- Ursodeoxycholic acid is the first-line treatment of choice for primary biliary cholangitis 23. About 40% of patients may not respond to ursodeoxycholic acid and may eventually need a liver transplant 23.
- Even though ursodeoxycholic acid is often used in primary sclerosing cholangitis, medical therapy is not effective in curtailing the disease progression. ERCP with stent dilatation is useful for symptomatic improvement in biliary ductal strictures in large intrahepatic or extrahepatic ducts 21. Liver transplantation is the definitive treatment for primary sclerosing cholangitis and, post-transplant recurrence is not uncommon.
- Azer SA, Sankararaman S. Steatorrhea. [Updated 2020 Jan 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541055
- Di Sabatino A, Lenti MV, Corazza GR. Malabsorption and malabsorption tests: do they still matter? Dig Liver Dis. 2014 May;46(5):389-90.
- Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am. J. Gastroenterol. 2011 Dec;106(12):2192-9.
- Paranjape SM, Mogayzel PJ. Cystic fibrosis. Pediatr Rev. 2014 May;35(5):194-205.
- Singh P, Arora A, Strand TA, Leffler DA, Catassi C, Green PH, Kelly CP, Ahuja V, Makharia GK. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2018 Jun;16(6):823-836.e2
- Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet. 2018 Jan 06;391(10115):70-81.
- Boonstra K, Kunst AE, Stadhouders PH, Tuynman HA, Poen AC, van Nieuwkerk KM, Witteman EM, Hamann D, Witteman BJ, Beuers U, Ponsioen CY., Epi PSC PBC study group. Rising incidence and prevalence of primary biliary cirrhosis: a large population-based study. Liver Int. 2014 Jul;34(6):e31-8
- Kim WR, Lindor KD, Locke GR, Therneau TM, Homburger HA, Batts KP, Yawn BP, Petz JL, Melton LJ, Dickson ER. Epidemiology and natural history of primary biliary cirrhosis in a US community. Gastroenterology. 2000 Dec;119(6):1631-6.
- Boonstra K, Beuers U, Ponsioen CY. Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review. J. Hepatol. 2012 May;56(5):1181-8.
- Grace E, Shaw C, Whelan K, Andreyev HJ. Review article: small intestinal bacterial overgrowth–prevalence, clinical features, current and developing diagnostic tests, and treatment. Aliment. Pharmacol. Ther. 2013 Oct;38(7):674-88.
- Sharma P, Baloda V, Gahlot GP, Singh A, Mehta R, Vishnubathla S, Kapoor K, Ahuja V, Gupta SD, Makharia GK, Das P. Clinical, endoscopic, and histological differentiation between celiac disease and tropical sprue: A systematic review. J. Gastroenterol. Hepatol. 2019 Jan;34(1):74-83.
- Shandro BM, Nagarajah R, Poullis A. Challenges in the management of pancreatic exocrine insufficiency. World J Gastrointest Pharmacol Ther. 2018 Oct 25;9(5):39-46.
- Kleeff J, Whitcomb DC, Shimosegawa T, Esposito I, Lerch MM, Gress T, Mayerle J, Drewes AM, Rebours V, Akisik F, Muñoz JED, Neoptolemos JP. Chronic pancreatitis. Nat Rev Dis Primers. 2017 Sep 07;3:17060.
- Conwell DL, Lee LS, Yadav D, Longnecker DS, Miller FH, Mortele KJ, Levy MJ, Kwon R, Lieb JG, Stevens T, Toskes PP, Gardner TB, Gelrud A, Wu BU, Forsmark CE, Vege SS. American Pancreatic Association Practice Guidelines in Chronic Pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014 Nov;43(8):1143-62.
- Mattner J. Impact of Microbes on the Pathogenesis of Primary Biliary Cirrhosis (PBC) and Primary Sclerosing Cholangitis (PSC). Int J Mol Sci. 2016 Nov 09;17(11).
- Lindfors K, Ciacci C, Kurppa K, Lundin KEA, Makharia GK, Mearin ML, Murray JA, Verdu EF, Kaukinen K. Coeliac disease. Nat Rev Dis Primers. 2019 Jan 10;5(1):3.
- Ghoshal UC, Ghoshal U. Small Intestinal Bacterial Overgrowth and Other Intestinal Disorders. Gastroenterol. Clin. North Am. 2017 Mar;46(1):103-120.
- Lindkvist B, Phillips ME, Domínguez-Muñoz JE. Clinical, anthropometric and laboratory nutritional markers of pancreatic exocrine insufficiency: Prevalence and diagnostic use. Pancreatology. 2015 Nov-Dec;15(6):589-97.
- Durie P, Baillargeon JD, Bouchard S, Donnellan F, Zepeda-Gomez S, Teshima C. Diagnosis and management of pancreatic exocrine insufficiency (PEI) in primary care: consensus guidance of a Canadian expert panel. Curr Med Res Opin. 2018 Jan;34(1):25-33.
- Bader TR, Beavers KL, Semelka RC. MR imaging features of primary sclerosing cholangitis: patterns of cirrhosis in relationship to clinical severity of disease. Radiology. 2003 Mar;226(3):675-85.
- Fricker ZP, Lichtenstein DR. Primary Sclerosing Cholangitis: A Concise Review of Diagnosis and Management. Dig. Dis. Sci. 2019 Mar;64(3):632-642.
- Clark R, Johnson R. Malabsorption Syndromes. Nurs. Clin. North Am. 2018 Sep;53(3):361-374.
- Santiago P, Scheinberg AR, Levy C. Cholestatic liver diseases: new targets, new therapies. Therap Adv Gastroenterol. 2018;11:1756284818787400