Rhesus disease
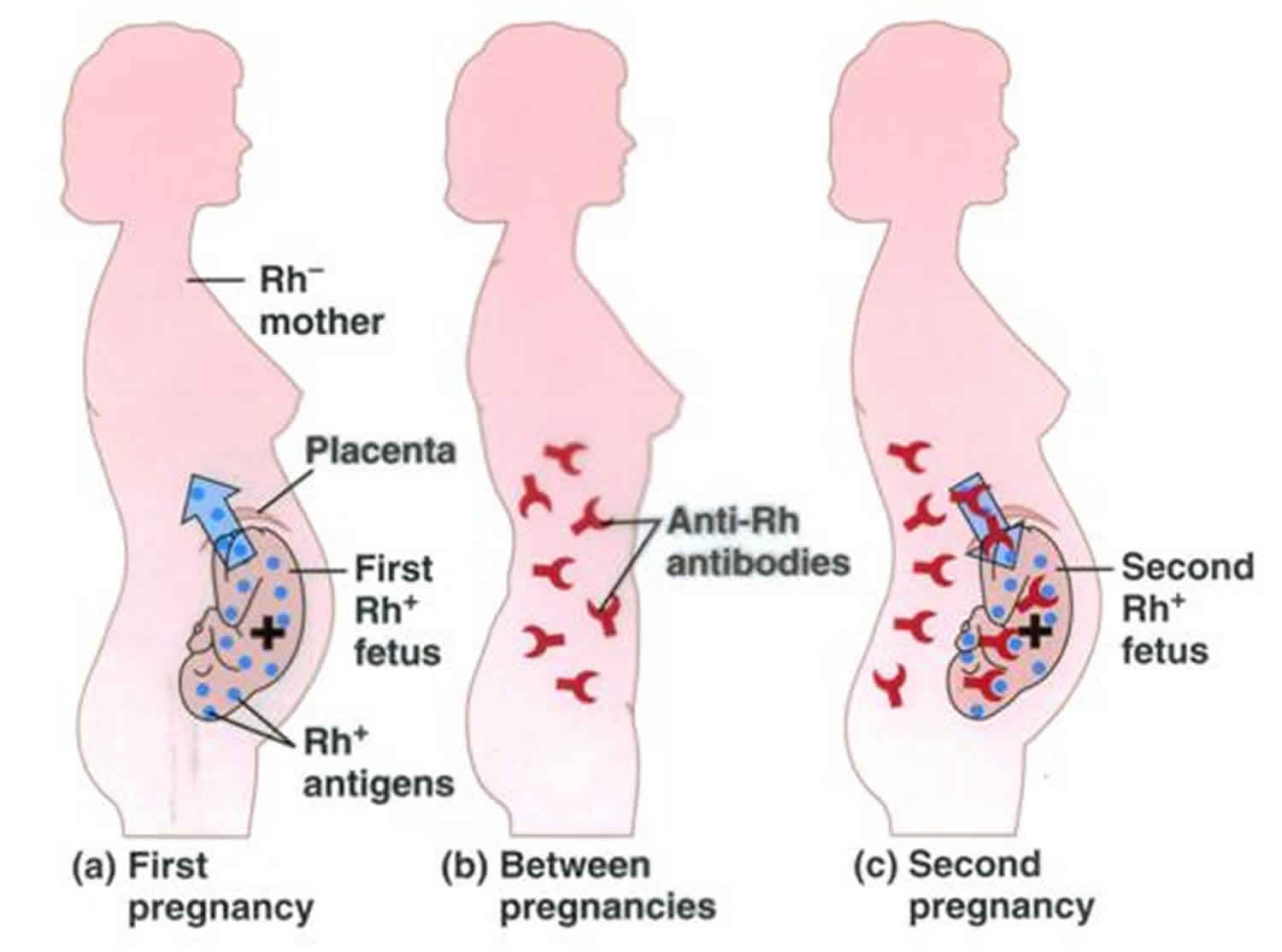
Rhesus disease also called Rh incompatibility or Rh disease, is a dangerous kind of anemia. Anemia is when a person doesn’t have enough healthy red blood cells to carry oxygen to the rest of your body. Rhesus disease happens when your blood is Rh-negative and your baby’s blood is Rh-positive. This means your blood and your baby’s blood are incompatible (Rh incompatibility), so it’s not safe for them to mix together. If they do mix, your body makes Rh antibodies that may go from your body through the placenta into your baby’s body, where they attack and destroy her/his red blood cells. The placenta grows in your uterus (womb) and supplies your baby with food and oxygen through the umbilical cord.
Even though you and your baby don’t share blood, a small amount of your baby’s blood can mix with yours during pregnancy. This can happen if:
- Your baby’s blood crosses into your blood through the placenta.
- You have an amniocentesis (also called amnio) or chorionic villus sampling (also called CVS). These are prenatal tests that your health care provider may recommend during pregnancy.
- You have bleeding during pregnancy.
- Your baby’s in a breech position (feet-down instead of head-down) before labor and your provider tries to rotate (move) him around so he’s head-down.
- You get hit in the belly during pregnancy.
- You have a miscarriage or an ectopic pregnancy. A miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. An ectopic pregnancy is when a fertilized egg implants itself outside of the uterus (womb) and begins to grow.
If you have Rh antibodies, you’re called Rh-sensitized.
What is Rh factor?
Rh factor also called Rhesus factor is a protein (a type of antigen) that’s found on some people’s red blood cells. The Rh blood group system also known as the Rhesus blood group system has over 50 Rh antigens; the 5 most significant Rh antigens are D, C, c, E, and e 1, 2, 3. Blood is either Rh-positive or Rh-negative. If your red blood cells have the Rhesus D protein (RhD antigen), you’re Rh-positive (Rh+). If your red blood cells don’t have the Rhesus D protein (RhD-), you’re Rh-negative (Rh-) 4, 5, 6. Being Rh-positive or Rh-negative doesn’t affect your health. But it can affect your baby during pregnancy if you’re Rh-negative and your baby is Rh-positive. In addition, Rh factor is also important when you have a blood transfusion. It is important to be given the right blood when you have a blood transfusion. Blood comes in 4 main blood types: A, B, AB, and O. These types refer to molecules called antigens on the surface of your red blood cells, where they serve as built-in protection devices for your blood supply. Antigens that reside on the surface of your red blood cells are designed to identify foreign cells and trigger immune responses that produce antibodies in the plasma to attack potential foreign invaders. Antigens are substances that can cause a person’s immune system to react.
The Rh blood group system was first described in 1939 by Levine and Stetson 7 who described a pregnant woman that had postpartum hemorrhage and the woman developed a severe transfusion reaction when she was transfused with blood from her husband following delivery of a stillborn child with erythroblastosis fetalis or immune hydrops fetalis (this occurs when the mother’s immune system attacks the blood cells of the baby). Even though she and her husband were ABO compatible, she developed pain and discolored urine after the blood transfusion. Agglutination occurred when her blood was remixed with her husband’s blood and from 80% of Caucasian ABO-compatible donors 8, 7. Levine and Stetson tested her blood with multiple ABO-matched donors and noted agglutination with 80% of the donor samples. The authors concluded that the patient had been isoimmunized with an unknown antigen from her fetus resulting in the incompatible blood transfusion 8, 7.
The following year, Landsteiner and Wiener found that sera from rabbits and later guinea pigs immunized with red blood cells from Macaca mulatta (Macacus rhesus in the original paper) agglutinated 85% of human red blood cell samples. Initially, it was thought that the animal and human antibodies identified a common factor, Rhesus (Rh) factor, on the surface of rhesus monkey and human red blood cells 9. Landsteiner and Wiener work would also describe the autosomal dominant inheritance pattern of the Rh factor 10. Later, it was discovered that humans and rhesus monkeys do not share the same red blood cell antigens, though the name persists 11. Therefore, the original terms Rh factor and anti-Rh coined by Landsteiner and Wiener, although being misnomers, have continued in common usage 2. The heteroantibody was renamed anti-LW (after Landsteiner and Wiener), and the human anti-Rh antibody was renamed anti-D 12
You can find out if you’re Rh-positive or Rh-negative with a blood test. Most people in the United States are Rh-positive. If you’re Rh-negative, your partner can get tested to find out his Rh type.
The Rh blood group is encoded by two tightly linked loci on chromosome 1p34-36 (short arm of chromosome 1) 4. The RHD gene encodes the RhD antigen, and the RHCE gene encodes RhCE antigens. SMP1, a sequence of unknown significance, separates RHD and RHCE 13. RHD and RHCE encode eight haplotypes of the Rh antigens in various combinations. The Rh proteins are hydrophobic transmembrane proteins embedded in the red blood cell phospholipid bilayer with an extracellular expression of the antigens. Interestingly, the RhD and RhCE proteins are very similar, with the first 41 amino acids identical 14.
Rh factor is inherited. This means Rh factor is passed from parents to children through genes. Genes are parts of your body’s cells that store instructions for the way your body grows and works. A baby may inherit the Rh-factor from either parent or a combination of both. Unlike antibodies to A and B antigens that determines the ABO blood type, antibodies to Rh factor are not produced naturally. Antibodies that are produced against the Rh factor can develop only if you lack the Rh factor on your red blood cells and then you are exposed to Rh-positive red blood cells. This can happen during pregnancy or birth when the mother is Rh-negative and the baby is Rh-positive, or sometimes when you are Rh-negative and are transfused with Rh-positive blood. In either case, the first exposure to the Rh antigen may not result in a strong response against the Rh-positive cells, but any subsequent exposure such as a second pregnancy may cause severe reactions. These antibodies can cross the placenta and destroy your baby’s red blood cells, resulting in hemolytic disease of the fetus and newborn (an immune-mediated red blood cell disorder in which maternal antibodies attack fetal or newborn red blood cells) 15. All newborn babies of Rh-negative mothers are typed for ABO and Rh soon after birth. This determines if the mother needs to receive Rh immune globulin, which prevents her from developing Rh antibodies against her fetus’ blood cells. If a Rh-negative mother has a negative red blood cell Rh antibody screen, then an Rh immune globulin injection is given within 72 hours to prevent Rh antibody production. If she has a positive test, then the antibody or antibodies present must be identified. If an antibody to the D antigen has been actively formed by the mother, then the Rh immune globulin injection is not useful. If she has a different antibody, then the Rh immune globulin injection can still be given to prevent her from producing antibodies to the D antigen.
Rh disease also called Rh incompatibility happens when your blood is Rh-negative and your baby’s blood is Rh-positive 16. This means your blood and your baby’s blood are incompatible, so it’s not safe for them to mix together. If they do mix, your body makes Rh antibodies that may go from your body through the placenta into your baby’s body, where they attack and destroy your baby’s red blood cells. The placenta grows in your uterus (womb) and supplies your baby with food and oxygen through the umbilical cord.
Rh disease can cause serious problems for your baby, including:
- Anemia
- Brain damage
- Heart failure
- Jaundice. Jaundice can make your baby’s eyes and skin look yellow. A baby has jaundice when his liver isn’t fully developed or isn’t working. If jaundice is severe and isn’t treated, a baby can develop a kind of brain damage called kernicterus.
- Stillbirth. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
- Death after birth
The presence or absence of antigens on your red blood cells and corresponding antibodies in your plasma defines your ABO blood group.
Each person’s blood is one of 8 specific types:
- A+ (A Rh-positive) means your blood has A antigens and B antibodies and Rh protein,
- A− (A Rh-negative) means your blood has A antigens and B antibodies and no Rh protein,
- B+ (B Rh-positive) means your blood has B antigens and A antibodies and Rh protein,
- B− (B Rh-negative) means your blood has B antigens and A antibodies and no Rh protein,
- AB+ (AB Rh-positive) means your blood has A antigen and B antigen and Rh protein and no A and B antibodies,
- AB− (AB Rh-negative) means your blood has A antigen and B antigen and no A and B antibodies and no Rh protein,
- O+ (O Rh-positive) means your blood has no A antigen and no B antigen, but it has both A and B antibodies and Rh protein,
- O− (O Rh-negative) means your blood has no A antigen and no B antigen and no Rh protein, but it has both A and B antibodies.
Note: Not everyone has one of the 8 common blood types, as there are over 600 other antigens can reside on red blood cells, leading to countless rare blood types 17. Since blood type is hereditary (passed from parents to children through genes), rare blood types typically exist in ethnic groups, but you won’t usually know this until you experience a medical emergency.
The following table indicates the type of antibodies you are expected to have based on your blood type.
Table 1. ABO Blood Group System
| Blood Type | Have Antibodies to |
|---|---|
| A | B antigen |
| B | A antigen |
| AB | No A and B antibodies |
| O | A and B antigens |
Blood is categorized in four primary types, or groups, based off of the ABO system. The four potential blood types are A, B, AB, and O. Antigens that are on the surface of red blood cells are either type A or they are type B. Their presence, or absence, determines whether blood is a type A or B. Blood groups are determined based on these antigens. Each blood type contains a delicate balance of antigens and antibodies, and not all blood types are compatible with one another. Since antibodies are designed to fight corresponding antigens, a transfusion that mixes two incompatible blood types could cause the antibodies in one to attack the antigens in another. These antibody attacks can lead to the creation of clumps of red blood cells also known as agglutination. Agglutination can create blood clots, stop circulation, and may cause red blood cells to split and leak, which triggers toxic reactions.
Since mixing incompatible types can be harmful or even fatal, understanding your blood type is critical, especially if you’re donating blood or receiving a transfusion from a donor. After all, some blood types can’t pair safely with others, while others are compatible with several other types.
People with O− (O Rh-negative) blood do not have A, B, or Rh proteins (antigens) on their blood cells. These people can donate blood to anyone, and are known as universal donors (universal red cell donor). This means that a person that is O negative can donate his blood to anyone regardless of that person’s blood type. In an emergency or if your life is in danger, medical personnel will most commonly administer O- (O Rh-negative) blood. However, despite type O- (O Rh-negative) blood reputation as a universal donor option, even O- (O Rh-negative) blood may have antibodies that react with other types. Since even O- (O Rh-negative) blood can cause complications that increase the risk of blood transfusion, medical personnel typically strive to use blood that precisely matches that of the patient.
People who are AB+ (AB Rh-positive) have all three antigens (A, B, and Rh factor) on their blood cells and can safely receive blood from anyone. Type AB+ (AB Rh-positive) is the universal plasma donor. This means that a person with AB+ (AB Rh-positive) blood type can donate plasma to anyone.
Other blood types can donate and give to only their matching blood types.
If a person receives the wrong type of blood, his or her immune system will react to it. This is a serious condition that can cause severe symptoms such as fever, muscles aches, and trouble breathing. It can sometimes be fatal.
The 8 standard blood groups can pair as follows:
- Type A+ (A Rh-positive): Can donate blood to types A+ and AB+. Can receive blood donations from types A+, A-, O+, and O-.
- Type A- (A Rh-negative): Can donate blood to types A+, A-, AB+, and AB-. Can receive blood donations from types A- and O-.
- Type B+ (B Rh-positive): Can donate blood to types B+ and AB+. Can receive blood donations from types B+, B-, O+, and O-.
- Type B− (B Rh-negative): Can donate blood to types B+, B-, AB+, and AB-. Can receive blood donations from types B- and O-.
- Type AB+ (AB Rh-positive): Can donate blood to type AB+. Can receive blood donations from all eight types.
- Type AB− (AB Rh-negative): Can donate blood to types AB+ and AB-. Can receive blood donations from types AB-, A-, B-, and O-.
- Type O+ (O Rh-positive): Can donate blood to types O+, A+, B+, and AB+. Can receive blood donations from types O+ and O-.
- Type O− (O Rh-negative): Can donate blood to all eight types. These people can donate blood to anyone, and are known as universal donors (universal red cell donor). But can receive blood donations only from type O-.
Overall, types O+ (O Rh-positive) with 37 percent of the population and A+ (A Rh-positive) 36 percent of the population are by far the most common blood types in the United States. Almost 9% of Americans have either type B+ (B Rh-positive) or O− (O Rh-negative) blood, while 6% have type A- (A Rh-negative), and 3% have type AB+ (AB Rh-positive) blood. Types B− (B Rh-negative) and AB− (AB Rh-negative) are the least common in the U.S., appearing in 2% and less than 1% of the population, respectively.
The following table shows what types of blood patients can safely receive, based on their individual blood types.
| Blood Group and Rh Type of Patient | Safe (Compatible) Blood Types for Red Blood Cell Transfusion* |
|---|---|
| A positive (A Rh-positive) | A positive, A negative, O positive, O negative |
| A negative (A Rh-negative) | A negative, O negative |
| B positive (B Rh-positive) | B positive, B negative, O positive, O negative |
| B negative (B Rh-negative) | B negative, O negative |
| AB positive (AB Rh-positive) | AB positive, AB negative, A positive, A negative, B positive, B negative, O positive, O negative |
| AB negative (AB Rh-negative) | AB negative, A negative, B negative, O negative |
| O positive (O Rh-positive) | O positive, O negative |
| O negative (O Rh-negative) | O negative |
Footnote: * These apply for red blood cell transfusions only; when transfusing plasma products and platelets, the compatible choices are different.
A blood transfusion is when blood is put into your body. Your blood has several parts. Plasma is the liquid part of your blood. It’s made of water, proteins, clotting factors, hormones, salts and other substances. Floating in the plasma are many red blood cells that transport oxygen, white blood cells that combat infections, and platelets that aid in clotting when you’re injured. Red blood cells contain hemoglobin (Hb) and hemoglobin (Hb) lets red blood cells carry oxygen from your lungs to the rest of your body. Your whole body needs oxygen, so it’s important to have enough red blood cells. Your blood also contains white blood cells. These help the body fight infection. And your blood contains smaller cells called platelets. These help the blood clot. Proteins called clotting factors also help your blood clot. Without these, your body can’t stop bleeding from even a tiny wound.
Whole blood refers to blood with all these parts. Most of the time, a blood transfusion is done with only part of the blood. You might be given one or more of these blood parts based on your needs.
Whether you receive O− (O Rh-negative) blood or your exact match, physicians generally begin the transfusion process by testing compatibility. Carefully cross-matching a small sample of your blood with the donor’s blood ensures that the two are compatible and won’t cause additional complications.
Who gets tested for Rh factor?
You, your partner and your baby can have tests to find out if you’re Rh-positive (Rh+) or Rh-negative (Rh-) and if your baby is at risk for Rh disease. If you and your baby have the same Rh factor, your blood types are considered compatible and won’t cause problems. However, if you are Rh-negative and your partner has Rh-positive, there’s a chance your baby has a negative Rh factor, which could lead to complications. While your blood won’t normally come into contact with your baby’s blood, the two could mix during delivery or if trauma occurs at any time during your pregnancy. Because Rh factor is an antigen, it can elicit an immune response and you could develop antibodies against the Rh antigen. These antibodies can cross the placenta and destroy your baby’s red blood cells, resulting in hemolytic disease of the fetus and newborn (an immune-mediated red blood cell disorder in which maternal antibodies attack fetal or newborn red blood cells) 15.
You should get a blood test at your first prenatal care visit to find out if you’re Rh-positive or Rh-negative. If you’re Rh-positive, there’s no risk of Rh disease in your baby.
If you’re Rh-negative:
- You get a test called an antibody screen to see if you have Rh antibodies in your blood.
- If you don’t have Rh antibodies, your partner gets tested to see if he’s Rh-positive or Rh-negative.
- If your partner is Rh-positive (Rh+) or you don’t know your partner’s Rh factor, your doctor may recommend an amniocentesis to check your baby’s Rh factor or his bilirubin level. Bilirubin is a yellow substance that can build up in your baby’s blood when his liver isn’t working right. You get a second antibody test at 28 weeks of pregnancy. If this second test shows that your baby has anemia, your doctor may do a Doppler ultrasound to check the flow of blood into your baby’s head.
- In the event that your blood do mix with your baby’s blood, your red blood cells could begin to produce Rh antibodies. While these antibodies aren’t likely to cause harm to you or your baby right away, they could affect your next pregnancy. During your next pregnancy, there’s a chance that the Rh antibodies could enter your baby’s blood supply. If you’re Rh-negative and your baby is Rh-positive, the antibodies could attack your baby’s red blood cells and cause anemia, a condition that could be fatal to your unborn child. To combat these potential complications, doctors often recommend that Rh-negative mothers have a blood test to screen for Rh antibodies during the first trimester and again at delivery. If you test positive for Rh antibodies at your 28th week of pregnancy, your obstetrician will generally monitor you and your baby carefully, providing a blood transfusion for the baby if necessary.
- If the Rh antibody test you take in your first trimester produces a negative result, you’ll typically receive an Rh immune globulin injection called Rho(D) immune globulin (brand name RhoGAM) to prevent your blood cells from generating any antibodies throughout your pregnancy. Rho(D) immune globulin consists of anti-Rh D antibodies that target Rh-positive red blood cells to prevent maternal sensitization. Rh immune globulin injection can prevent your body from producing Rh antibodies so your baby and future pregnancies won’t get Rh disease. Rh immune globulin injection doesn’t work if your body has already started making Rh antibodies in a previous pregnancy. This is why it’s really important to get prenatal care as early as possible in every pregnancy.
- You’ll undergo another blood test at delivery. If your baby is born Rh-positive (Rh+), you’ll typically need a second injection, but if your baby is born Rh-negative (Rh-), you won’t usually need additional treatment. In some cases, you’ll need additional injections to protect yourself and any future children. Prenatal tests like amniocentesis, chorionic villus sampling, or cordocentesis can all cause your baby’s blood to mix with yours and may require an injection. If you experience a miscarriage, an ectopic pregnancy, substantial bleeding, or an abortion, Rh immune globulin is typically necessary.
If I’m Rh-negative, can I protect my baby from Rh disease?
Rh disease can be prevented in your baby if you get treatment at the right times. If you haven’t developed Rh antibodies, your doctor can give you a shot of Rh immunoglobulin called Rho(D) immune globulin (RhoGAM). Rh immune globulin injection can prevent your body from producing Rh antibodies so your baby and future pregnancies won’t get Rh disease. Rh immune globulin injection doesn’t work if your body has already started making Rh antibodies in a previous pregnancy. This is why it’s really important to get prenatal care as early as possible in every pregnancy.
If you’re Rh-negative, you get Rh immune globulin injection:
- At about 28 weeks of pregnancy
- Within 72 hours after the birth if your baby is Rh-positive or if his Rh is unknown
- After any situation in which your blood and your baby’s blood may mix, like amniocentesis or chorionic villus sampling, miscarriage, ectopic pregnancy or a hit to your belly.
Your provider watches your baby closely during pregnancy to check his health and for signs of anemia. In your third trimester, your doctor may use amniocentesis or a special ultrasound called Doppler to check your baby. Ultrasound is a prenatal test that uses sound waves and a computer screen to show a picture of your baby inside the womb. A Doppler ultrasound helps a provider check your baby’s heartbeat and measure the blood flow in the umbilical cord and certain blood vessels.
If my baby has Rh disease, how she/he is treated?
If your baby has Rh disease, she can be treated to help prevent serious health problems.
If your baby has mild Rh disease, you may be able to have a full-term pregnancy. Full term means your baby is born between 39 weeks and 40 weeks, 6 days. After birth, your baby may need certain medicine, and she may need treatment for jaundice. Sometimes Rh disease is so mild that your baby doesn’t need any treatment. Most babies recover fully from mild Rh disease.
If your baby develops severe Rh disease and severe anemia before birth, you may have to give birth early, before her due date. She may need a blood transfusion with new blood to replace red blood cells that the Rh antibodies destroyed. Babies can get a blood transfusion in the womb as early as 18 weeks of pregnancy; they also can get a transfusion after birth.
If your baby is born with severe jaundice, she needs quick treatment to prevent more serious complications.
What happened before the Rh immune globulin injection was developed?
Prior to development of the Rh immune globulin injection, Rh-negative mothers would often become sensitized from the blood of their first Rh-positive baby and begin developing anti-Rh antibodies. Any subsequent Rh-positive babies would have some degree of Rh disease, due to the mother’s anti-Rh antibodies attacking the baby’s red blood cells. Miscarriages and stillborn babies were relatively common, and those babies who were born often needed immediate blood transfusions to survive. The Rh immune globulin injection has largely prevented these complications, although a small percent of women do still develop Rh antibodies.
What is hemolytic disease of the newborn?
Hemolytic disease of the newborn (HDN) also called immune erythroblastosis fetalis, ABO incompatibility HDN or Rh incompatibility HDN, is a potentially life-threatening condition that occurs when the blood types of a mother and baby are incompatible. Hemolytic disease of the newborn results from maternal antibodies attacking fetal red blood cells due to incompatibility of maternal and fetal blood based on the Rhesus (Rh) and ABO antigen systems where antibodies from a Rhesus negative (Rh-) pregnant mother attack a Rhesus positive (Rh+) fetus 18. Hemolytic disease of the newborn or erythroblastosis fetalis can destroy the newborn baby’s blood cells very quickly, which can cause symptoms during pregnancy or after the baby is born. The severity of hemolytic disease of the newborn can vary. Each child may experience different symptoms of hemolytic disease of the newborn (erythroblastosis fetalis). Some babies have no symptoms. In other cases, problems such as hydrops can cause the baby to die before, or shortly after, birth. Severe hemolytic disease of the newborn (erythroblastosis fetalis) may be treated before birth by intrauterine blood transfusions.
The most common symptoms of hemolytic disease of the newborn (erythroblastosis fetalis) are:
- pale skin
- yellowing of the amniotic fluid, umbilical cord, skin, and eyes (jaundice)
- enlarged liver or spleen
- severe swelling of the body (edema)
During pregnancy, symptoms of hemolytic disease of the newborn or immune erythroblastosis fetalis may include:
- Large amounts of amniotic fluid
- Thickened placenta
- Enlarged liver, spleen, or heart in the baby
- Fluid buildup in the baby’s abdomen
- Mild anemia: When the baby’s red blood cell count is deficient, his blood cannot carry enough oxygen from the lungs to all parts of his body, causing his organs and tissues to struggle.
- Hyperbilirubinemia and jaundice: The breakdown of red blood cells produces bilirubin, a brownish yellow substance that is difficult for a baby to discharge and can build up in his blood (hyperbilirubinemia) and make his skin appear yellow.
- Severe anemia with enlargement of the liver and spleen: The baby’s body tries to compensate for the breakdown of red blood cells by making more of them very quickly in the liver and spleen, which causes the organs to get bigger. These new red blood cells are often immature and unable to function completely, leading to severe anemia.
- Hydrops fetalis: When the baby’s body cannot cope with the anemia, his heart begins to fail and large amounts of fluid buildup in his tissues and organs. Hydrops (fluid throughout the body’s tissues, including in the spaces containing the lungs, heart, and abdominal organs), which can lead to heart failure or respiratory failure from too much fluid.
After birth, symptoms of hemolytic disease of the newborn or immune erythroblastosis fetalis may include:
- Pale coloring
- Severe swelling overall (edema), especially in the baby’s abdomen
- Enlarged liver and spleen
- Difficulty breathing
- Severe hyperbilirubinemia and newborn jaundice which occurs sooner and is more severe than normal. Excessive buildup of bilirubin in the baby’s blood causes his liver to become enlarged.
- Kernicterus: Buildup of bilirubin in the blood is so high that it spills over into the brain, which can lead to permanent brain damage.
Hemolytic disease of the newborn is currently estimated to affect 3 to 8 of every 100,000 pregnancies 19. The occurrence of hemolytic disease of the newborn is directly correlated with the inheritance pattern in females that results in the absence of the Rhesus (D) antigen; however, the incidence of hemolytic disease of the newborn is seen to vary with ethnicity 20. For instance, it has been found that whites have the highest prevalence of hemolytic disease of the newborn, and Asians and American Indians have the lowest, as illustrated in Table 3 below. Furthermore, among the Rh antigens in existence, the most immunogenic one is the D antigen. It is approximated that about 10% of pregnant white women are Rh incompatible 18.
Table 3. Prevalence of hemolytic disease of the newborn according to ethnic groups
| Ethnicity | Prevalence of hemolytic disease of the newborn by percentage |
|---|---|
| Africans | 4% |
| African-Americans | 8% |
| Whites | 15–16% |
| Eurasians | 2.4% |
| Asians | <1% |
| Basque (Spain/France) | 30–35% |
Hemolytic disease of the newborn is preventable. Before the onset of Rh immunoglobulin therapies, 1% of all pregnancies resulted in fetal death from hemolytic disease of the newborn. Today, nearly all women with Rh-negative blood are identified in early pregnancy through blood tests. If a mother is Rh-negative and has not been sensitized, she is usually given a drug called Rh immunoglobulin or RhoGAM. This specially developed blood product prevents an Rh-negative mother’s antibodies from reacting to her baby’s Rh-positive red blood cells. Mothers are typically given RhoGAM around the 28th week of pregnancy and again within 72 hours of giving birth.
Typically, it is the second Rh-positive fetus that is affected. When the first child inherits the father’s D antigen, whose inheritance has been shown to follow an autosomal dominant pattern, and maternal and fetal blood mixing occurs during the pregnancy. This mixing most commonly happens during labor and delivery but can theoretically occur at any time during the pregnancy. Once maternal and fetal blood mixing occurs during the pregnancy, pregnant mother begins producing anti-D antibodies. This constitutes alloimmunization, as the pregnant mother is D-negative 21.
The initial antibodies produced are IgM, which cannot cross the placental barrier. However, when isotype switching occurs, IgG antibodies are produced. IgG antibodies can cross the placental barrier, and they do so during the second and or subsequent pregnancies, attacking the fetal red blood cells and causing hemolysis and associated complications such as hydrops fetalis and jaundice 22. Although, the IgG antibodies can enter fetal circulation through fetomaternal hemorrhage as well.
The general absence of maternal and fetal blood mixing during the first pregnancy and the delay of IgG antibody production make it unlikely that the first D-negative pregnancy is affected. However, in the subsequent D-negative pregnancy, IgG antibodies cross the placenta and attack the D antigens on fetal red blood cells. This leads to hemolysis that may result in jaundice, anemia, kernicterus, and hydrops fetalis. Intrauterine death may occur without intrauterine blood transfusion, and any surviving fetus may have developmental delays, hearing loss, and hypotonia 18.
Hemolytic disease of the newborn can be diagnosed during pregnancy or after the baby is born. Tests conducted during pregnancy may include:
- complete blood count test for the mother
- ultrasound
- amniocentesis
- cordocentesis
After birth, tests may include:
- complete blood count test for the baby
- umbilical cord blood test
Hemolytic disease of the newborn can be treated during pregnancy or after the baby is born. Treatment during pregnancy may include:
- blood transfusion
- early delivery of the baby if severe complications arise and baby’s lungs are mature
After birth, treatment may include:
- Blood transfusion
- Intravenous fluids
- Oxygen or mechanical breathing machine
- Light therapy (phototherapy) using special blue lights to convert bilirubin into a form which is easier for the baby’s body to get rid of.
- Antibodies (intravenous immunoglobulin, or IVIG) to help protect the baby’s red cells from being destroyed.
- Feeding often and receiving extra fluids.
- Medicines to raise blood pressure if it drops too low.
- In severe cases, an exchange transfusion to replace the baby’s damaged blood with fresh blood may need to be performed. This involves removing a large amount of the baby’s blood, and thus the extra bilirubin and antibodies. Fresh donor blood is infused.
- Simple transfusion (without exchange). This may need to be repeated after the baby goes home from the hospital.
What influences my blood type?
Blood type is a hereditary trait, it is passed from parents to children through genes and is determined by two factors: the ABO grouping system and the Rh factor, such that your parents’ blood types determine your blood type. While children’s blood types aren’t necessarily an exact match for one of their parents, understanding parents’ blood types can help narrow down the potential types that children could have.
A single gene determines ABO blood type, and three versions of the gene exist: A, B, and O. Both A and B versions of the blood type gene are dominant, and the O version is recessive. Children inherit one version of the gene from each parent, resulting in six potential combinations of genes that place them in one of four ABO groups.
For example, a child who inherits an A version of the gene from one parent and a B version from the other will have blood type AB. Inheriting an A version and an O version of the gene will result in blood type A, while inheriting two O versions of the gene will result in blood type O.
A separate gene determines whether children have the Rh factor. Since Rh factor is either positive or negative, only two versions of this gene exist. In this case, the positive version is dominant, and the negative version is recessive. That means inheriting a positive version and a negative version of the gene will result in blood type Rh-positive (Rh+), while inheriting two negative versions will result in blood type Rh-negative (Rh-).
Although creating a hereditary chart can help in assessing potential blood type options for current and future generations, this method isn’t scientific. Only a reliable test can confirm your blood type.
I’m blood type O. Do I have a chance of having a baby with ABO hemolytic disease of the newborn?
Yes. Hemolytic disease of the newborn may occur when there is an ABO incompatibility between mother and baby, especially with mothers who are blood group O. However, the red blood cell antibody screen is not useful in this situation because our bodies naturally produce antibodies against the A and B antigens we do not have on our red blood cells. A mother who is blood type A will naturally have antibodies directed against the B surface antigens on red blood cells, and a mother who is type B will have anti-A antibodies, and so on. Generally, this is a mild form that is easily treatable.
Rh disease baby
Your baby is at risk for Rh disease only if you’re Rh-negative and your baby is Rh-positive. Your baby is Rh-positive depending on the blood of you and your baby’s father. Here’s how it works:
- If both you and your baby’s father are Rh-positive: Your baby’s blood is Rh-positive, and there’s no risk of Rh disease in your baby.
- If both you and your baby’s father are Rh-negative: Your baby’s blood is Rh-negative, and there’s no risk of Rh disease for your baby.
- If you’re Rh negative and your baby’s father is Rh-positive: Your baby’s blood may be Rh-positive. Your baby is at risk for Rh disease and needs to be checked closely.
Talk to your doctor about having your blood and your baby’s father’s blood tested to find out if your baby may be at risk.
If it’s your first pregnancy, your body usually doesn’t make enough Rh antibodies to harm your baby. But if you get pregnant again, your body produces more antibodies that can cause Rh disease in your baby.
Rh disease can cause serious problems for your baby, including:
- Anemia
- Brain damage
- Heart failure
- Jaundice. Jaundice can make your baby’s eyes and skin look yellow. A baby has jaundice when his liver isn’t fully developed or isn’t working. If jaundice is severe and isn’t treated, a baby can develop a kind of brain damage called kernicterus.
- Stillbirth. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
- Death after birth
If your baby has Rh disease, how is she treated?
If your baby has Rh disease, she can be treated to help prevent serious health problems.
If your baby has mild Rh disease, you may be able to have a full-term pregnancy. Full term means your baby is born between 39 weeks and 40 weeks, 6 days. After birth, your baby may need certain medicine, and she may need treatment for jaundice. Sometimes Rh disease is so mild that your baby doesn’t need any treatment. Most babies recover fully from mild Rh disease.
If your baby develops severe Rh disease and severe anemia before birth, you may have to give birth early, before her due date. She may need a blood transfusion with new blood to replace red blood cells that the Rh antibodies destroyed. Babies can get a blood transfusion in the womb as early as 18 weeks of pregnancy; they also can get a transfusion after birth.
If your baby is born with severe jaundice, she needs quick treatment to prevent more serious complications.
Rh disease causes
During pregnancy, red blood cells from the unborn baby can cross into the mother’s blood through the placenta.
If the mother is Rh-negative, her immune system treats Rh-positive fetal cells as if they were a foreign substance. The mother’s body makes antibodies against the fetal blood cells. These antibodies may cross back through the placenta into the developing baby. They destroy the baby’s circulating red blood cells.
When red blood cells are broken down, they make bilirubin. This causes an infant to become yellow (jaundiced). The level of bilirubin in the infant’s blood may range from mild to dangerously high.
Firstborn infants are often not affected unless the mother had past miscarriages or abortions. This would sensitize her immune system. This is because it takes time for the mother to develop antibodies. All children she has later who are also Rh-positive may be affected.
Rh incompatibility develops only when the mother is Rh-negative and the infant is Rh-positive. This problem has become less common in places that provide good prenatal care. This is because special Rho D immune globulin called RhoGAM are routinely used.
Rh disease symptoms
Rh incompatibility can cause symptoms ranging from very mild to deadly. In its mildest form, Rh incompatibility causes the destruction of red blood cells. There are no other effects.
After birth, the infant may have:
- Yellowing of the skin and whites of the eyes (jaundice)
- Low muscle tone (hypotonia) and lethargy
Before delivery, the mother may have more amniotic fluid around her unborn baby (polyhydramnios).
There may be:
- A positive direct Coombs test result
- Higher-than-normal levels of bilirubin in the baby’s umbilical cord blood
- Signs of red blood cell destruction in the infant’s blood
Rh disease prevention
Rh disease can be prevented in your baby if you get treatment at the right times. If you haven’t developed Rh antibodies, your doctor can give you a shot of Rh immunoglobulin called Rho D immune globulin (brand name RhoGAM®). RhoGAM can prevent your body from producing Rh antibodies so your baby and future pregnancies won’t get Rh disease. RhoGAM doesn’t work if your body has already started making Rh antibodies in a previous pregnancy. This is why it’s really important to get prenatal care as early as possible in every pregnancy.
If you’re RH-negative, you get Rho D immune globulin:
- At about 28 weeks of pregnancy
- Within 72 hours after the birth if your baby is Rh-positive or if his Rh is unknown
- After any situation in which your blood and your baby’s blood may mix, like amniocentesis or chorionic villus sampling, miscarriage, ectopic pregnancy or a hit to your belly.
Your provider watches your baby closely during pregnancy to check his health and for signs of anemia. In your third trimester, your provider may use amniocentesis or a special ultrasound called Doppler to check your baby. Ultrasound is a prenatal test that uses sound waves and a computer screen to show a picture of your baby inside the womb. A Doppler ultrasound helps a doctor check your baby’s heartbeat and measure the blood flow in the umbilical cord and certain blood vessels.
Rh disease treatment
Rh disease or Rh incompatibility can be prevented with the use of RhoGAM. Therefore, prevention remains the best treatment. Treatment of an infant who is already affected depends on the severity of the condition.
Infants with mild Rh incompatibility may be treated with phototherapy using bilirubin lights. IV immune globulin may also be used. For infants severely affected, an exchange transfusion of blood may be needed. This is to decrease the levels of bilirubin in the blood.
Rh disease prognosis
Full recovery is expected for mild Rh disease or Rh incompatibility.
Rh disease possible complications
Complications may include:
- Brain damage due to high levels of bilirubin (kernicterus)
- Fluid buildup and swelling in the baby (hydrops fetalis)
- Problems with mental function, movement, hearing, speech, and seizures
- Dacie and Lewis Practical Haematology Book. Twelfth Edition 2017. ISBN 978-0-7020-6696-2 https://www.sciencedirect.com/book/9780702066962/dacie-and-lewis-practical-haematology
- Avent ND, Reid ME. The Rh blood group system: a review. Blood. 2000 Jan 15;95(2):375-87. Erratum in: Blood 2000 Apr 1;95(7):2197. https://doi.org/10.1182/blood.V95.2.375
- Encyclopedia of Forensic and Legal Medicine (Second Edition) 2016, Pages 425-432. https://doi.org/10.1016/B978-0-12-800034-2.00054-9
- Rosenkrans D, Zubair M, Doyal A. Rh Blood Group System. [Updated 2023 Aug 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK594252
- Hyland CA, Gardener GJ, Davies H, Ahvenainen M, Flower RL, Irwin D, Morris JM, Ward CM, Hyett JA. Evaluation of non-invasive prenatal RHD genotyping of the fetus. Med J Aust. 2009 Jul 6;191(1):21-5. doi: 10.5694/j.1326-5377.2009.tb02668.x
- Ontario Health (Quality). Noninvasive Fetal RhD Blood Group Genotyping: A Health Technology Assessment. Ont Health Technol Assess Ser. 2020 Nov 2;20(15):1-160. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7670296
- P Levine, RE Stetson An unusual case of intragroup agglutination. JAMA. 1939;113(2):126–127. doi:10.1001/jama.1939.72800270002007a
- Levine P, Stetson RE. An Unusual Case of Intra-group Agglutination. JAMA. 1984;251(10):1316–1317. doi:10.1001/jama.1984.03340340056028
- Landsteiner K, Wiener AS. An Agglutinable Factor in Human Blood Recognized by Immune Sera for Rhesus Blood. Proceedings of the Society for Experimental Biology and Medicine. 1940;43(1):223-223. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2135190/pdf/309.pdf
- Landsteiner K, Wiener AS. STUDIES ON AN AGGLUTINOGEN (Rh) IN HUMAN BLOOD REACTING WITH ANTI-RHESUS SERA AND WITH HUMAN ISOANTIBODIES. J Exp Med. 1941 Sep 30;74(4):309-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2135190/pdf/309.pdf
- Roy T. Fisk, Alvin G. Foord, Observations on the Rh Agglutinogen of Human Blood, American Journal of Clinical Pathology, Volume 12, Issue 11, 1 November 1942, Pages 545–552, https://doi.org/10.1093/ajcp/12.11.545
- LEVINE, P., CELANO, M., WALLACE, J. et al. A Human ‘D-like’ Antibody. Nature 198, 596–597 (1963). https://doi.org/10.1038/198596a0
- Van Kim CL, Colin Y, Cartron JP. Rh proteins: key structural and functional components of the red cell membrane. Blood Rev. 2006 Mar;20(2):93-110. doi: 10.1016/j.blre.2005.04.002
- Avent ND, Ridgwell K, Tanner MJ, Anstee DJ. cDNA cloning of a 30 kDa erythrocyte membrane protein associated with Rh (Rhesus)-blood-group-antigen expression. Biochem J. 1990 Nov 1;271(3):821-5. doi: 10.1042/bj2710821
- Hall V, Avulakunta ID. Hemolytic Diseases of the Newborn. [Updated 2022 Nov 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557423
- Rh incompatibility. https://medlineplus.gov/ency/article/001600.htm
- 202 Table of blood group antigens within systems. https://www.isbtweb.org/resource/tableofbloodgroupantigenswithinsystems.html
- Myle AK, Al-Khattabi GH. Hemolytic Disease of the Newborn: A Review of Current Trends and Prospects. Pediatric Health Med Ther. 2021 Oct 7;12:491-498. doi: 10.2147/PHMT.S327032
- Routray SS, Behera R, Mallick B, Acharya D, Sahoo JP, Kanungo GN, Pati B. The Spectrum of Hemolytic Disease of the Newborn: Evaluating the Etiology of Unconjugated Hyperbilirubinemia Among Neonates Pertinent to Immunohematological Workup. Cureus. 2021 Aug 6;13(8):e16940. doi: 10.7759/cureus.16940
- Doll P. Hemolytic disease of newborn: symptom and causes. Pediatrics. 2021;132(3):e145–e232. doi: 10.2342/peds.114.2.e143
- Gupta GK, Balbuena-Merle R, Hendrickson JE, Tormey CA. Immunohematologic aspects of alloimmunization and alloantibody detection: A focus on pregnancy and hemolytic disease of the fetus and newborn. Transfus Apher Sci. 2020 Oct;59(5):102946. doi: 10.1016/j.transci.2020.102946
- Alaqeel AA. Hyporegenerative anemia and other complications of rhesus hemolytic disease: to treat or not to treat is the question. Pan Afr Med J. 2019 Mar 14;32:120. doi: 10.11604/pamj.2019.32.120.17757