Shortness of breath during pregnancy
Shortness of breath in pregnancy is a common complaint found in up to 70% of healthy women in the third trimester (weeks 27 to 40) 1 and is considered a normal physiologic response to pregnancy 2, although it may occasionally be a sign of underlying heart or lung disorders. Shortness of breath of pregnancy may also occur early in pregnancy. It often improves or stabilizes as term approaches 2 and it typically does not interfere with daily activities 3. Shortness of breath also called dyspnea, is when you feel like you can’t get enough air into your lungs when you breathe. You may feel like this later in pregnancy, when your womb and the position of your baby is pressing on your diaphragm (the muscle that helps you breathe) and making it difficult for your lungs to expand. The extra weight you are carrying may also make you feel short of breath. Even if you feel shortness of breath, your baby’s getting oxygen in the womb.
Usually it’s nothing to be concerned about, but it’s best to check with your doctor, since lots of things can cause shortness of breath.
As a normal part of pregnancy, your breathing may be affected by the increase in the hormone progesterone, which causes you to breathe in more deeply. This might make you feel as if you’re working harder to get air. Breathing may also become more difficult as your enlarging uterus takes up more space, resulting in pressure against your diaphragm (the muscle below your lungs).
As your baby “drops” lower into your pelvis as you near delivery, you should start to be able to breathe a little easier. In the meantime, try to:
- Maintain good posture when you’re sitting or standing (slouching doesn’t give your lungs enough room to expand when you breathe).
- Prop yourself up when sleeping by putting some pillows under the upper body in a semi-sitting position. It reduces the pressure that the uterus places on the lungs.
- Don’t overdo it, whether you’re exercising, just walking around, or doing housework. Take your time and respond to your body’s cues to slow down or stop altogether.
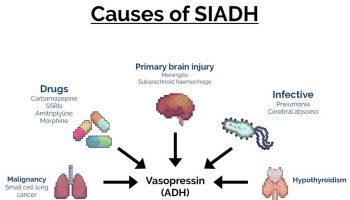
Other causes of shortness of breath during pregnancy include:
- Anemia: Anemia (being low in iron) can cause shortness of breath.
- Pre-eclampsia: This could be a cause especially if you have some of the other symptoms of pre-eclampsia.
- These are:
- a headache
- blurred vision
- upper tummy pain
- nausea
- vomiting
- swelling of your hands, feet, ankles, face and/or neck
- These are:
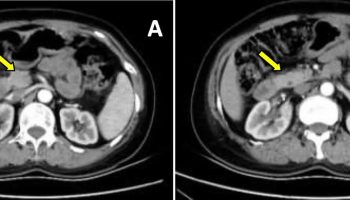
- Pulmonary embolism: This is a life-threatening condition. Pulmonary embolism happens when a deep vein thrombosis (DVT) or clot in a vein of your lower leg moves to your lungs. You may also have chest pain, particularly when you take a deep breath in or cough. You may also notice that your heart is beating faster than usual.
- Asthma: If you suffer from asthma, pregnancy may make your symptoms more severe. Talk to your GP urgently if you have a history of asthma and notice your shortness of breath is getting worse.
- Lung infections and pneumonia: If you have a cough that lasts more than 2 to 3 days always see your doctor. Simple infections make you sicker in pregnancy than they normally would. This is one of the reasons why it is recommended that you receive the flu vaccine during pregnancy.
Persistent and worsening shortness of breath requires thorough investigation, and physiologic shortness of breath should remain a diagnosis of exclusion. However, many pregnant women are admitted to hospital for severe shortness of breath and exercise intolerance. They undergo multiple tests to exclude significant cardiac or respiratory disorders, which, in most cases, are not found. There is no therapy for shortness of breath if no underlying treatable cause is identified 4.
If your shortness of breath has started suddenly, is severe, seems to be worsening, or is associated with pain, coughing, wheezing, or heart palpitations, let your doctor know. These may be signs that something other than pregnancy alone is causing your shortness of breath.
See your doctor or go to the emergency department immediately if:
- Your breathlessness is sudden or severe.
- There’s a big change in your breathing.
- You have a cough.
- You have breathlessness and pain in your chest, heart palpitations or dizziness.
Shortness of breath during pregnancy causes
The mechanism of shortness of breath of pregnancy is controversial. Various causes have been suggested, including an increased mechanical compression of the lungs, displacement of the diaphragm by the gravid uterus 5, a change in perception of normal respiration, hyperventilation in response to a reduced diffusion lung capacity 6, a higher sensitivity of the central chemo reflex response to carbon dioxide (CO2) 7 and an effect of gestational hormones (progesterone and estradiol) on the drive to breath 8. However, all of the above studies focused only on respiratory causes for shortness of breath and did not consider a possible role of subtle cardiac factors.
The physiologic changes in pregnancy include an increase in blood volume, a decrease in peripheral vascular resistance during the first weeks of pregnancy, and an increase in heart rate 9. These result in an increase in systolic function, notably an increase in cardiac output, a rise in preload, a decrease in afterload, and an increase in left ventricular (LV) mass. A slight increase in LV ejection fraction (LVEF) and LV cavity dimensions have been reported 9. Few data are available on cardiac diastolic function during normal pregnancy 10 and it is not considered to have an impact of clinical significance.
Two recent developments in echocardiography enable a more accurate assessment of diastolic function: a relatively preload‐insensitive estimation of left atrial pressure using tissue Doppler imaging in conjunction with standard Doppler 11 and a technique based on 2‐dimensional (2D) speckle tracking for quantification of myocardial strain, which provides data on longitudinal and circumferential myocardial function and rotation 12. These deformation indexes were reported to be very sensitive to assess early changes in LV function 13. Thus, recently, a small decrease in LV segmental longitudinal systolic strain in late pregnancy has been described 14.
Shortness of breath during pregnancy treatment
Shortness of breath during pregnancy treatment involves identifying and treating the underlying cause of your shortness of breath.
To help make your breathing easier:
- Don’t smoke. If you need help to quit smoking, tell your health care provider.
- Sit or stand up straight to give your lungs room to expand. Move slowly.
- Try to breathe clean air. Stay away from secondhand smoke (smoke from someone else’s tobacco) and other air pollutants.
- Reeder CF, Hambright AA, Fortner KB. Dyspnea in Pregnancy: A Case Report of a Third Trimester Mediastinal Mass in Pregnancy. Am J Case Rep. 2018;19:1536‐1540. Published 2018 Dec 28. doi:10.12659/AJCR.910725 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6322058
- Zeldis SM. Dyspnea during pregnancy: distinguishing cardiac from pulmonary causes. Clin Chest Med. 1992;13:567–585.
- Milne J, Howie AD, Pack AI. Dyspnea during normal pregnancy. Br J Obstet Gynaecol. 1978;85:260–263.
- Goland S, Perelman S, Asalih N, et al. Shortness of Breath During Pregnancy: Could a Cardiac Factor Be Involved?. Clin Cardiol. 2015;38(10):598‐603. doi:10.1002/clc.22452 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6490843
- Alaily AB, Carrol KB. Pulmonary ventilation in pregnancy. Br J Obstet Gynaecol. 1978;85:518–524.
- Knuttgen HG, Emmerson K Jr. Physiological response to pregnancy at rest and during exercise. J Appl Physiol. 1974;36:549–553.
- Jensen D, Wolfe LA, Slatkovska L, et al. Effects of human pregnancy on the ventilatory chemoreflex response to carbon dioxide. Am J Physiol Regul Integr Comp Physiol. 2005;288:R1369–R1375.
- García‐Rio F, Pino JM, Gómez L, et al. Regulation of breathing and perception of dyspnea in healthy pregnant women. Chest. 1996;110:446–453.
- Valensise H. Maternal diastolic dysfunction and left ventricular geometry in gestational hypertension. Hypertension. 2001;37:1209–1215.
- Mesa A, Jessurun C, Hernandez A, et al. Left ventricular diastolic function in normal human pregnancy. Circulation. 1999;99:511–517.
- Ommen SR, Nishimura RA, Appleton CP, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler‐catheterization study. Circulation. 2000;102:1788–1794.
- Reisner S, Lysyansky P, Agmon Y, et al. A Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr. 2004;17:630–633.
- VanWagner LB, Wilcox JE, Colangelo LA, et al. Association of nonalcoholic fatty liver disease with subclinical myocardial remodeling and dysfunction: a population‐based study. Hepatology. 2015;62:773–783.
- Savu O, Jurcuţ R, Giuşcă S, et al. Morphological and functional adaptation of the maternal heart during pregnancy. Circ Cardiovasc Imaging. 2012;5:289–297.