Snapping hip
Snapping hip also known as snapping hip syndrome, coxa saltans or dancer’s hip, is a condition in which you feel a snapping sensation or hear a popping sound in your hip when you walk, get up from a chair, or swing your leg around 1. Snapping hip syndrome can be caused by structures inside the joint or structures outside the hip joint. The snapping sensation occurs when a muscle or tendon (the strong tissue that connects muscle to bone) moves over a bony protrusion in your hip. People who suffer snapping hips are typically young and athletic, with dancers being particularly affected. Although snapping hip syndrome is usually painless and harmless, the sensation can be annoying. In some cases, snapping hip leads to bursitis, a painful swelling of the fluid-filled sacs that cushion the hip joint.
In snapping hip syndrome, slightly different biomechanics are involved with the iliotibial band than with the iliopsoas musculotendinous unit 2. Snapping hip syndrome may develop as the result of an acute injury leading to subsequent bursitis, tendinitis, or biomechanical changes. More commonly, snapping hip syndrome is the result of repetitive overuse.
Snapping hip can occur in different areas of the hip where tendons and muscles slide over knobs in the hip bones.
- Outside of the hip. The most common site of snapping hip is at the outer side where the iliotibial band passes over the portion of the thighbone known as the greater trochanter. When the hip is straight, the iliotibial band is behind the trochanter. When the hip bends, the band moves over the trochanter so that it is in front of it. The iliotibial band is always tight, like a stretched rubber band. Because the trochanter juts out slightly, the movement of the band across it creates the snap you hear. Eventually, snapping hip may lead to hip bursitis. Bursitis is thickening and inflammation of the bursa, a fluid-filled sac that allows the muscle to move smoothly over bone.
- Front of the hip. Another tendon that could cause a snapping hip runs from the front of the thigh up to the pelvis (rectus femoris tendon). Snapping of the rectus femoris tendon is felt in the front of the hip. As you bend the hip, the tendon shifts across the head of the thighbone, and when you straighten the hip, the tendon moves back to the side of the thighbone. This back-and-forth motion across the head of the thighbone causes the snapping. In addition to the rectus femoris tendon at the front of the hip, the iliopsoas tendon can catch on bony prominences at the front of the pelvis bone.
- Back of the hip. Snapping in the back of the hip can involve the hamstring tendon. This tendon attaches to the sitting bone, called the ischial tuberosity. When it moves across the ischial tuberosity, the tendon may catch, causing a snapping sensation in the buttock region.
- Cartilage problems. The labrum that lines the socket of the hip can tear and cause a snapping sensation. Damaged cartilage can loosen and float in the joint causing the hip to catch or “lock up.” This type of snapping hip usually causes pain and may be disabling.
External snapping hip syndrome most commonly is caused by the iliotibial band snapping over the greater trochanter of the femoral head during movements such as flexion, extension, and external or internal rotation.
Internal snapping hip is most commonly caused by the iliopsoas tendon snapping over underlying bony prominences, such as the iliopectinal eminence or the anterior aspect of the femoral head.
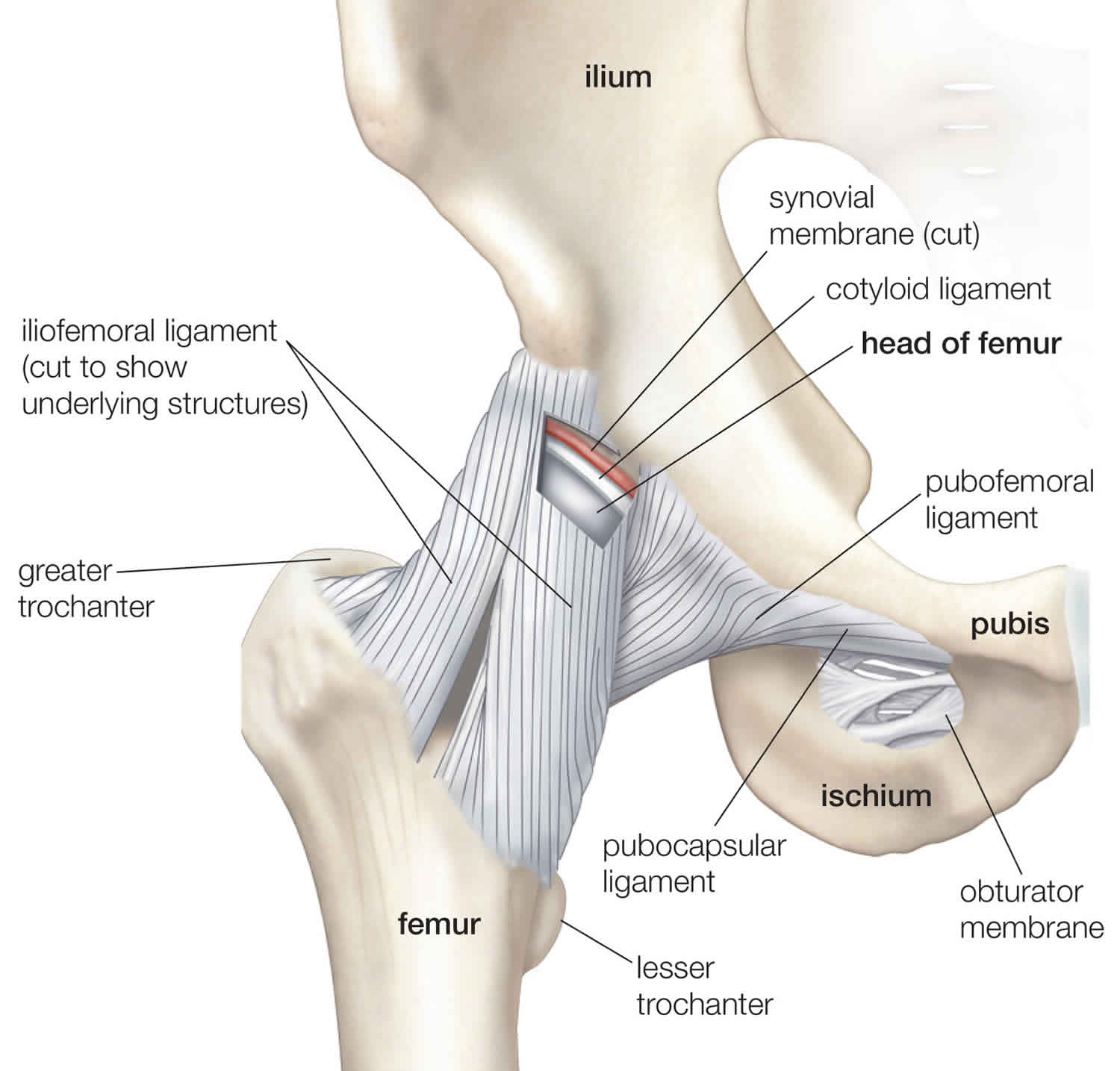
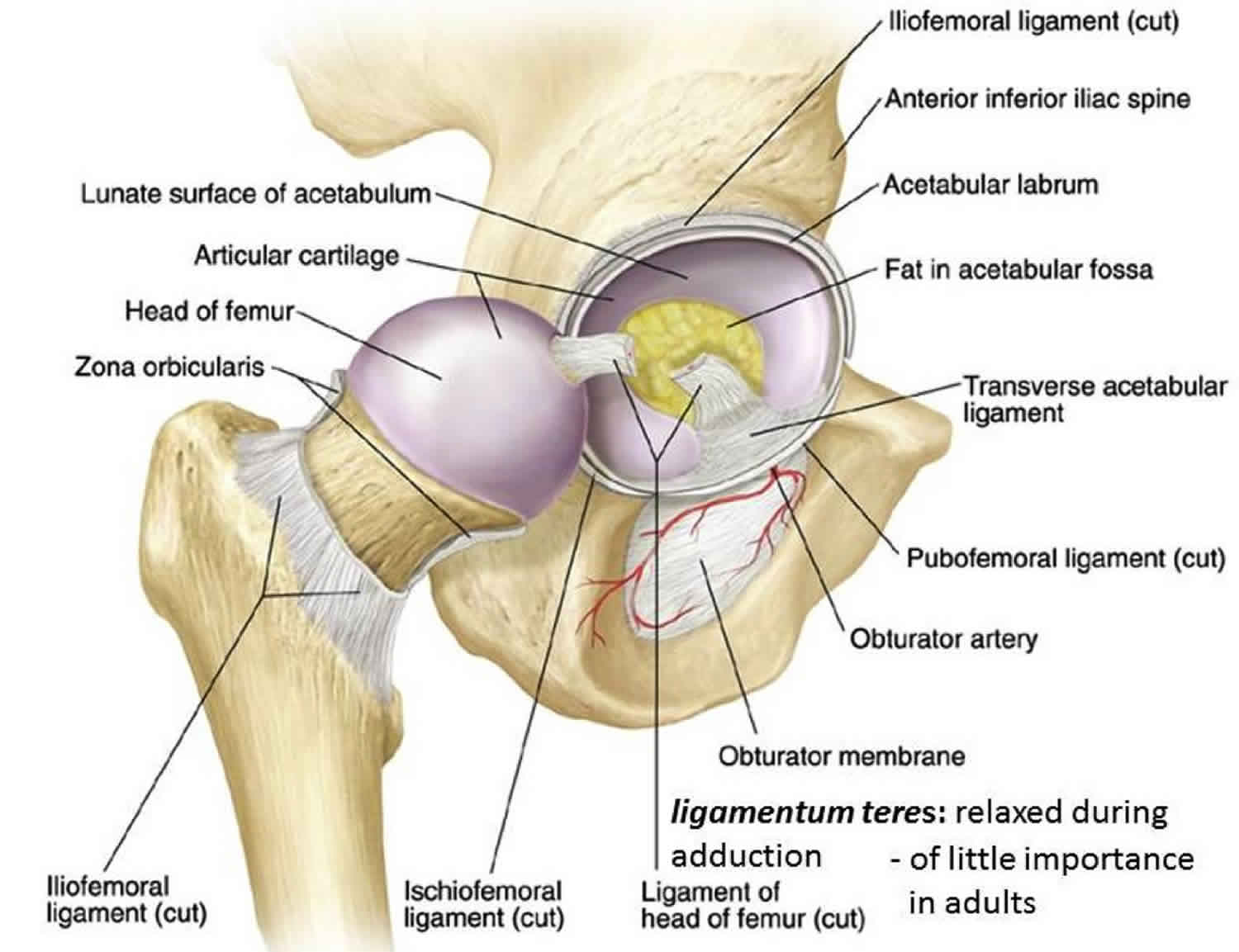
Figure 1. Hip joint anatomy (in a healthy hip, the head of the femur stays firmly within the acetabulum)
Internal snapping hip syndrome
Internal snapping hip most commonly occurs as the iliopsoas tendon snaps over underlying bony prominences, such as the iliopectinal eminence or the anterior aspect of the femoral head 1. As an overuse phenomenon, this condition may occur in any activity resulting in repeated hip flexion or external rotation of the femur. Activities that may predispose to iliopsoas tendinitis include dancing, ballet, resistance training (eg. squats), rowing, running (particularly uphill), track and field, soccer, and gymnastics.
During the adolescent growth spurt, a tendency exists for the hip flexors to become relatively inflexible. For younger athletes, this can lead to problems as increased stress is placed on the iliopsoas musculotendinous unit and general biomechanics are altered. Tightness of the iliopsoas, tensor fascia lata, or rectus femoris can lead to inhibition of the gluteus maximus, allowing for an anterior pelvic tilt, which can lead to adverse affects on the kinetic chain.
Excessive anterior tilt due to a tight iliopsoas muscle, tight hip adductors, and a relatively weak rectus abdominis can lead to increased lumbar lordosis with subsequent increased stress on the lower lumbar disks, facet joints, and sacroiliac joints. This also may result in increased knee flexion during gait at the heel-strike and midstance phases. The increase in eccentric load across the knee extensor mechanism may result in patellar tendon injuries (eg. patellar tendinitis, Osgood-Schlatter disease). With increased knee flexion, compressive forces at the patellofemoral articulation increase and may predispose to patellofemoral problems.
Other causes include paralabral cysts and partial or complete bifurcation of the iliopsoas tendon. The snapping sensation can closely mimic intra-articular pathology, since they both originate from the anterior hip area. Close physical exam and imaging can differentiate the two. It should be noted, however, that in approximately 50% of internal snapping hip cases, an additional intra-articular hip pathology is identified.
External snapping hip syndrome
External snapping hip syndrome may be caused by either the iliotibial band or gluteus maximus snapping over the greater trochanter. External snapping hip is most commonly attributed to the iliotibial band moving over the greater trochanter of the femoral head during hip movements in flexion, extension, and external or internal rotation. Subluxation of the iliotibial band over the greater trochanter may occur while the hip extends from a flexed position (in which the iliotibial band moves from a position anterior to the greater trochanter to a position posterior to the greater trochanter) 3. This action is most pronounced with sudden loading of the hip joint into a flexed position, such as occurs when landing a jump (eg. dismounting from an apparatus in gymnastics, rebounding in basketball, long jumping in track-and-field competitions).
The gluteus maximus is a powerful extensor of the thigh and trunk when the lower extremities are fixed. However, it is posturally unimportant, relaxed with standing, and used little in walking. The gluteus maximus is used in activities such as running, climbing, and rising from a seated or stooped position. It also regulates flexion at the hip (a paradoxical action) 2.
Other causes include the proximal hamstring tendon rolling over the ischial tuberosity, either the fascia lata or the anterior aspect of the gluteus maximus rolling over the greater trochanter, and the psoas tendon rolling over the medial fibers of the iliacus muscle. A combination of defects is also possible; for example, thickening of both the posterior iliotibial band and anterior gluteus maximus, which snap over the greater trochanter at the same time 4.
Snapping hip syndrome causes
Snapping hip syndrome can be caused by structures inside the joint (internal causes) or structures outside the joint (external causes).
Snapping hip is most often the result of tightness in the muscles and tendons surrounding the hip. People who are involved in sports and activities that require repeated bending at the hip are more likely to experience snapping hip. Dancers are especially vulnerable.
Young athletes are also more likely to have snapping hip. This is because tightness in the muscle structures of the hip is common during adolescent growth spurts.
External causes
- The most common cause of snapping hip syndrome is excessive movement of the tough band of tissue that runs down the outer side of the leg (iliotibial band) over the boney point of the hip joint (greater trochanter of the femur). If this is the tendon causing the problem, then the pain will be felt on the outer aspect of the hip.
- The hip flexor (psoas muscle): this muscle runs down the front of the hip and helps to lift or flex the hip bone. If this is the muscle causing the problem, then the pain will often be felt in the groin.
- The tough ligaments that surround the hip joint (the iliofemoral ligaments) can also be a cause of snapping hip syndrome but this is a rarer cause.
Internal causes
- Internal causes of snapping hip syndrome include mechanical catching from cartilage tears (labral tears) or loose bodies.
Risk factors for snapping hip syndrome
- Snapping hip syndrome due to external causes is most commonly seen in young athletes and dancers. The large range of movement required of athletes and especially dancers, may lead to a tendon near the hip moving excessively.
- Risk factors for snapping hip syndrome caused by internal structures include osteoarthritis, femoroacetabular impingement and loose bodies.
Snapping hip syndrome prevention
The primary goal for prevention of snapping hip syndrome is maintenance of good flexibility and strength in the hip and pelvis 5.
Snapping hip syndrome symptoms
People with snapping hip syndrome usually have a snap or click in the hip which may be loud enough to be heard by an observer. The snapping sensation may be either painless or painful.
The location of the pain may be in the outer aspect of the hip, the groin or in rare cases the pain may refer to the knee.
Occasionally, the sensation of the hip ‘popping out’ is described and is associated with the tough band of tissue that runs down the outer side of the leg (iliotibial band) flicking over the hip bone.
The pain and snapping will usually subside with rest.
Snapping hip syndrome complications
Snapping hip syndrome can cause irritation to the structure causing the snapping, or irritation to the structure over which the snapping occurs. It can lead to:
- hip bursitis
- hip muscle strains
- hip muscle tendonitis
Snapping hip syndrome diagnosis
Your doctor will first determine the exact cause of the snapping by discussing you medical history and symptoms, and conducting a physical examination. He or she may ask you where it hurts, what kinds of activities bring on the snapping, whether you can demonstrate the snapping, or whether you have experienced any injury to the hip area.
You may also be asked to stand and move your hip in various directions to reproduce the snapping. Your doctor may even be able to feel the tendon moving as you bend or extend your hip.
Imaging tests
X-rays provide clear pictures of dense structures, such as bone. Although x-rays of people with snapping hip do not typically show anything abnormal, your doctor may order x-rays or other tests to rule out any problems with the bones or joint.
Ultrasound is a useful, noninvasive diagnostic tool because it may demonstrate changes in the muscles and tendons around the hip.
An MRI scan is usually not needed in this condition but may be reserved for cases that remain undiagnosed following the above investigations.
Snapping hip test
A positive response to anesthetic joint injection in the affected area can help distinguish between external and internal snapping hip syndrome 6.
Clinically visible external snapping hip syndrome can be confirmed on T1 weighted axial MRI as a thickened iliotibial band or thickened anterior edge of the gluteus maximus muscle. If the snapping is not visible on physical exam, dynamic ultrasonography can be used to demonstrate the snapping of the iliotibial band over the greater trochanter. Dynamic ultrasonography also can reveal associated tendonitis, iliopsoas bursitis, or muscle tears.
A diagnosis of internal snapping hip syndrome can be confirmed using iliopsoas bursography combined with fluoroscopy, dynamic ultrasonography, magnetic resonance imaging, or magnetic resonance arthrography. Magnetic resonance arthrography is preferred because it also can detect intra-articular hip pathology, which commonly accompanies internal snapping hip syndrome.
Snapping hip syndrome treatment
Most people do not see a doctor for snapping hip unless they experience some pain. If the snapping hip bothers you — but not to the point of seeing a doctor — try the following conservative home treatment options:
- Reduce your activity levels and apply ice to the affected area.
- Use nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen, to reduce discomfort.
- Modify your sport or exercise activities to avoid repetitive movement of the hip. For example, reduce time spent on a bicycle, and swim using your arms only.
If you are still experiencing discomfort after trying these conservative methods, consult your doctor for professional treatment.
Snapping hip syndrome stretches
Your doctor may prescribe exercises to stretch and strengthen the musculature surrounding the hip. Guidance from a physical therapist may also be recommended.
Iliotibial band stretch
- Stand next to a wall for support
- Cross the leg that is closest to the wall behind your other leg.
- Lean your hip toward the wall until you feel a stretch at the outside of your hip. Hold the stretch for 30 seconds.
- Repeat on the opposite side.
- Perform 2 to 3 sets of 4 repetitions each side.
Figure 2. Iliotibial band stretch
Piriformis stretch
- Lie on your back with bent knees and feet flat on the floor.
- Cross the foot of the affected hip over the opposite knee and clasp your hands behind your thigh.
- Pull your thigh toward you until you feel the stretch in your hip and buttocks. Hold the stretch for 30 seconds.
- Repeat on the opposite side.
- Perform 2 to 3 sets of 4 repetitions each side.
Figure 3. Piriformis stretch
Corticosteroid injection
If you have hip bursitis, your doctor may recommend an injection of a corticosteroid into the bursa to reduce painful inflammation.
Surgical treatment
In the rare instances that snapping hip does not respond to conservative treatment, your doctor may recommend surgery. The type of surgery will depend on the cause of the snapping hip.
Hip arthroscopy
During hip arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your hip joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments.
Because the arthroscope and surgical instruments are thin, the surgeon can use very small incisions (cuts), rather than the larger incision needed for standard, open surgery.
Hip arthroscopy is most often used to remove or repair fragments of a torn labrum.
Open procedure
A traditional open surgical incision (several centimeters long) may be required to address the cause of the snapping hip. An open incision can help your surgeon to better see and gain access to the problem in the hip.
Your orthopaedic surgeon will discuss with you the best procedure to meet your individual health needs.
For external snapping hip syndrome, loosening of the iliotibial band is usually the goal and can be accomplished with either open or arthroscopic procedures. The iliotibial tendon is lengthened or completely released using various procedures including formal Z-lengthening, a cross-shaped release, a Z-shaped release or a gluteus maximus release. Weakness in abduction may be a complication if the release is excessive or there is damage to the surrounding area 7.
For internal snapping hip syndrome, open or arthroscopic procedures also are available to lengthen or release the iliopsoas tendon. Arthroscopic methods are preferred to avoid complications of open surgery. The most common adverse effect of iliopsoas release is hip flexor weakness, which may occur if there is excessive release or there is damage to the surrounding area. Corrective surgeries for either internal or external snapping hip can result in other complications including infection, heterotopic ossification, muscle atrophy, continued symptoms, or nerve damage.
Return to play
Patients may return to activities as tolerated. The return to sports activities is safe once the patient is free from pain and is capable of demonstrating sports-specific activities. This generally requires full flexibility at the involved hip, and recovery of at least 90% of the strength of the involved lower extremity as compared to the uninvolved lower extremity.
For individuals who present with internal snapping hip in the absence of any pain or limitation, activity is generally not restricted; however, the authors find it prudent to fully assess the iliopsoas complex and implement an appropriate course of flexibility training and strengthening of the hip stabilizers (with attention to the iliopsoas and hip flexors) in order to prevent further problems.
References- Musick SR, Varacallo M. Snapping Hip Syndrome. [Updated 2019 Apr 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448200
- Hruska R. Pelvic stability: influences of lower-extremity kinematics. Biomechanics. June 1998. 6:23-9.
- Choi YS, Lee SM, Song BY, Paik SH, Yoon YK. Dynamic sonography of external snapping hip syndrome. J Ultrasound Med. 2002 Jul. 21(7):753-8.
- Badowski E. Snapping Hip Syndrome. Orthop Nurs. 2018 Nov/Dec;37(6):357-360.
- Reid DC. Prevention of hip and knee injuries in ballet dancers. Sports Med. 1988 Nov. 6(5):295-307.
- Nolton EC, Ambegaonkar JP. Recognizing and Managing Snapping Hip Syndrome in Dancers. Med Probl Perform Art. 2018 Dec;33(4):286-291.
- Ilizaliturri VM, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc Rev. 2010 Jun;18(2):120-7.