Stiff skin syndrome
Stiff skin syndrome is a rare kind of scleroderma that is a rare syndrome characterized by hard, thick skin, usually on the entire body. The thickening of the skin can limit joint mobility and causes joints to be stuck in a bent position (flexion contractures) 1. Stiff skin syndrome is divided into two categories: widespread stiff skin syndrome and segmental stiff skin syndrome 2. Widespread stiff skin syndrome is more severe, more common, has more limited joint range of motion and an earlier onset than segmental stiff skin syndrome. Segmental stiff skin syndrome is predominant in females, whereas widespread stiff skin syndrome does not seem to feature any sex preinclination 3. Segmental stiff skin syndrome has segmental distribution with unilateral predominance. Compared with widespread stiff skin syndrome, limited joint range of motion occurs less than half of patients in segmental stiff skin syndrome 2. Both widespread stiff skin syndrome and segmental stiff skin syndrome are reported to have early onset within the first six years of life 3.
Both categories of stiff skin syndrome may be genetically inherited (~20%). In many cases, chest expansion is decreased due to the decreased elasticity and increased thickening of the skin in the thoracic region, causing restrictive changes in the lungs 4. Stiff skin syndrome is not a progressive disorder 5; however, two cases reportedly progressed from segmental stiff skin syndrome to widespread stiff skin syndrome 6.
The onset of stiff skin syndrome signs and symptoms can range from presenting at birth through childhood 7. Other stiff skin syndrome signs and symptoms may include excessive hair growth (hypertrichosis), loss of body fat (lipodystrophy), scoliosis, muscle weakness, slow growth, and short stature. Weakness or paralysis of the eye muscles have also been reported 8.
Stiff skin syndrome diagnosis is based on a clinical evaluation that is consistent with stiff skin syndrome, and the diagnosis can be confirmed with genetic testing. Treatment is based on the symptoms of each individual and may include physical therapy to improve or maintain joint movement 9.
Therapeutic exercises and rehabilitation programs are suggested for preventing joint contractures. Corticosteroids and other immunosuppressants have proven ineffective 2. Only mycophenolate mofetil resolved skin lesions and improved joint range of motion in two cases 10. However, further knowledge and experience of stiff skin syndrome are required for a better treatment approach.
Is stiff skin syndrome an autoimmune disease?
Stiff skin syndrome is primarily considered to be a connective tissue disease, rather than an autoimmune disease. Connective tissue is the structural tissue that gives strength to joints, tendons, ligaments, and blood vessels.
In autoimmune diseases, inflammation and the immune response result in tissue damage which may affect various tissues and organs in the body 11. Autoimmune diseases affect a significant portion of the population and are typically thought to be multifactorial (caused by a combination of genetic and environmental factors). Autoimmune diseases due to mutations in single genes are rare 12. stiff skin syndrome is now known to be caused by mutations in the FBN1 gene (rather than a faulty immune response), which is responsible for a key component of connective tissue and is known to cause various other connective tissue disorders 13.
There are disorders that are considered both autoimmune diseases and connective tissue diseases. Sometimes they are referred to as autoimmune disorders of connective tissue, or as autoimmune rheumatic disorders. These conditions result from the immune system mistakenly attacking components of connective tissues.
Scleroderma is an example of an autoimmune disorder of connective tissue (of unknown cause) 13. stiff skin syndrome is sometimes described as an inherited, congenital form of scleroderma or a scleroderma-like disorder, because of overlapping features. It appears that in both conditions, the same process malfunctions and causes a similar end result of “stiff skin” or fibrosis 14. However, the triggers for this process appear to differ (an FBN1 gene mutation affecting skin development and maintenance, vs a faulty immune response). In this case, stiff skin syndrome is a connective tissue disorder that resembles scleroderma, which is autoimmune in nature 15.
Stiff skin syndrome causes
Stiff skin syndrome is a genetic syndrome caused by changes (mutations) in the FBN1 gene and is inherited in an autosomal dominant manner 9. The FBN1 gene gives the body instructions to make a large protein called fibrillin-1. This protein works in the spaces between the cells (the extracellular matrix) to help form elastic fibers which enable the skin, ligaments, and blood vessels to stretch. This protein is also important for providing support to bones and the tissues that support the nerves, muscles, and lenses of the eye 16.
Mutations in the FBN1 gene that cause stiff skin syndrome affect the fibrillin-1 protein, which is thought to cause abnormal associations between fibrillin and another protein called elastin. When these two proteins interact abnormally in the extracellular matrix, this leads to the development of features of stiff skin syndrome 8.
Mutations in the FBN1 gene are also associated with a different genetic syndrome called Marfan syndrome. The changes that cause stiff skin syndrome occur in a different part of a gene than the changes that cause Marfan syndrome 17. It is possible that some cases of stiff skin syndrome occur in people without mutations in FBN1. More research will be necessary to determine if all cases of stiff skin syndrome are due to mutations in FBN1 18.
Stiff skin syndrome inheritance pattern
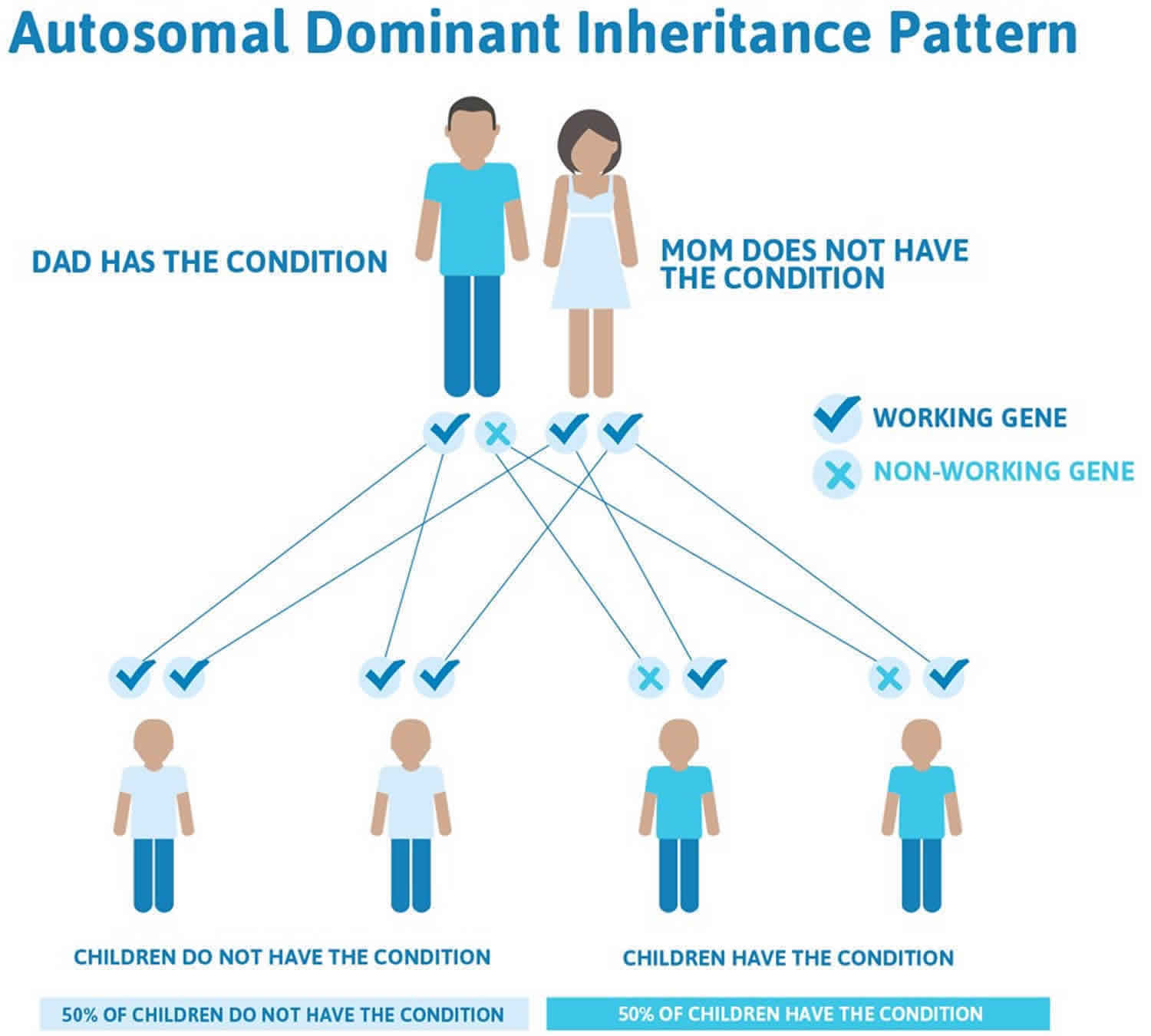
Stiff skin syndrome is inherited in an autosomal dominant manner 8. This means that having a change in only one copy of the FBN1 gene will cause symptoms of stiff skin syndrome. You inherit one copy of each of your genes from your mother and the other from your father.
Some people with stiff skin syndrome have a parent who has the syndrome as well. In this case, the affected individual inherited the syndrome from their affected parent. In other cases, a person with stiff skin syndrome is the first person in the family to have the syndrome, and neither parent is affected. In these cases, the mutation in FBN1 is new in the affected person, which is called a de novo mutation.
When a person with stiff skin syndrome has children, for each child there is a:
- 50% chance that the child will inherit the mutation in FBN1, which means they will have stiff skin syndrome
- 50% chance that the child will not inherit the mutation in FBN1, which means they will not have stiff skin syndrome.
Researchers have proposed that, in some cases, people with stiff skin syndrome may only have a mutation in FBN1 in some cells of the body. This could cause a less severe form of stiff skin syndrome that is called segmental stiff skin syndrome because it only affects certain parts of the body 18.
Figure 1 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 1. Stiff skin syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Stiff skin syndrome symptoms
The signs and symptoms associated with stiff skin syndrome include hard, thickened skin, especially affecting the buttocks, thighs, and shoulders. Other symptoms may include excessive hair growth (hypertrichosis), loss of body fat (lipodystrophy), scoliosis, muscle weakness, slow growth, and short stature 9. Some people with stiff skin syndrome may have restrictive pulmonary changes and a narrow chest cavity that cause trouble breathing. Many individuals with stiff skin syndrome walk on their tiptoes 19.
The thickening of the skin associated with stiff skin syndrome can result in difficulty moving joints, as they become stuck in the bent position (flexion contractures). This typically affects the larger joints, such as the shoulders, elbows, and knees. The ability to flex the joints of the fingers may also be affected, as individuals with this syndrome may develop nodules on the skin of the fingers. stiff skin syndrome is a slowly progressive syndrome, meaning that the signs and symptoms worsen as individuals get older 19.
Stiff skin syndrome diagnosis
A diagnosis of stiff skin syndrome can be made based on a clinical evaluation that is consistent with the signs and symptoms of the syndrome. Your child’s doctor may observe that your child has features of stiff skin syndrome. In some cases, biopsies of the skin can be used to determine if the skin has certain characteristics when viewed under a microscope 7. In some cases, genetic testing of the FBN1 gene may be used to confirm the diagnosis 19.
Stiff skin syndrome treatment
At this time, no specific therapies are available to reverse the symptoms of stiff skin syndrome. The recommended therapies aim to address issues moving the joints that may develop as a symptom of stiff skin syndrome. Regular physical therapy and exercise may be recommended to improve or maintain joint movement. A number of treatments have been tried in individual cases, including steroids, immunosuppressant drugs, psoralens (light-sensitizing medications), and light therapy. These treatments have not been helpful in slowing or stopping symptoms of stiff skin syndrome 7.
Some study findings on animal models have indicated potential future therapeutic options. In one study, mice with stiff skin syndrome were treated by blocking certain antibodies (integrin binding and TGF-beta antibodies). This prevented new skin lesions and reversed existing ones 20. You can read more about this discovery through the following link to the Scleroderma Research Society (https://srfcure.org/interrogation-of-the-pathogenesis-of-stiff-skin-syndrome-a-congenital-form-of-scleroderma).
Another recent paper discussed the possibility of using a medication that suppresses the immune system called mycophenolate mofetil in combination with physical therapy to treat individuals with stiff skin syndrome. Although this treatment has only been used for a couple of affected individuals, the doctors noted an improvement in symptoms. However, these individuals had the segmental form of stiff skin syndrome. It is not known whether this treatment would work for every person with the segmental form of stiff skin syndrome, and it is not known if it will work at all for people with the classic form of stiff skin syndrome 21.
Stiff skin syndrome prognosis
There is very limited information about how stiff skin syndrome affects a person during their teenage or adult years. Based upon case reports, it appears that stiff skin syndrome tends to slowly progress during childhood. It can involve joints, such as the knees and hips, which can limit movement and cause a deformity of the limbs. The loss of joint mobility may affect gait or posture. For this reason, some people with stiff skin syndrome walk on their tiptoes or have scoliosis. In severe cases, the syndrome may affect the chest and make breathing more difficult 7.
References- Chamney S, Cartmill B, Earley O, McConnell V, and Willoughby CE. The ocular phenotype of stiff-skin syndrome. Eye (Lond). January 2016; 30(1):156-159. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709530
- Myers KL, Mir A, Schaffer JV, Meehan SA, Orlow SJ, Brinster NK. Segmental stiff skin syndrome (SSS): A distinct clinical entity. J Am Acad Dermatol. 2016;75:163–168.
- Sari A, Çirakoglu D. Middle-Aged Female Diagnosed With Widespread Stiff Skin Syndrome. Arch Rheumatol. 2018;33(4):491–493. Published 2018 Mar 23. doi:10.5606/ArchRheumatol.2018.6805 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6409170
- Deng X, Chen F, Song Z, Yan H, You Y, Zhong B, et al. Four new cases of stiff skin syndrome with unusual presentations. J Eur Acad Dermatol Venereol. 2016;30:163–165.
- Jensen SA, Iqbal S, Bulsiewicz A, Handford PA. A microfibril assembly assay identifies different mechanisms of dominance underlying Marfan syndrome, stiff skin syndrome and acromelic dysplasias. Hum Mol Genet. 2015;24:4454–4463.
- Liu T, McCalmont TH, Frieden IJ, Williams ML, Connolly MK, Gilliam AE. The stiff skin syndrome: case series, differential diagnosis of the stiff skin phenotype, and review of the literature. Arch Dermatol. 2008;144:1351–1359.
- Amorim AG, Aide MK, Duraes SM, and Rochael MC. Stiff skin syndrome–case report. An Bras Dermatol. 2011 Jul-Aug; 86(4 Suppl 1):S178-81. https://doi.org/10.1590/S0365-05962011000700046
- STIFF SKIN SYNDROME; SSKS. https://omim.org/entry/184900
- Chamney S, Cartmill B, Earley O, McConnell V, Willoughby CE. The ocular phenotype of stiff-skin syndrome. Eye (Lond). 2016;30(1):156–159. doi:10.1038/eye.2015.183 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709530
- Kurtzman DJ, Wright NA, Patel M, Vleugels RA. Segmental stiff skin syndrome (SSS): Two additional cases with a positive response to mycophenolate mofetil and physical therapy. J Am Acad Dermatol. 2016;75:e237–e239.
- Overview of Autoimmune Disorders of Connective Tissue. https://www.merckmanuals.com/home/bone,-joint,-and-muscle-disorders/autoimmune-disorders-of-connective-tissue/overview-of-autoimmune-disorders-of-connective-tissue
- Maureen A. Su and Mark S. Anderson. Monogenic Autoimmune Diseases: Insights into Self-Tolerance. Pediatr Res. May, 2009; 65(5 Pt 2):20R-25R.
- Systemic Sclerosis. https://www.merckmanuals.com/home/bone,-joint,-and-muscle-disorders/autoimmune-disorders-of-connective-tissue/systemic-sclerosis
- Interrogation of the Pathogenesis of Stiff Skin Syndrome: A Congenital Form of Scleroderma https://srfcure.org/interrogation-of-the-pathogenesis-of-stiff-skin-syndrome-a-congenital-form-of-scleroderma
- E. V. Avvedimento and A. Gabrielli. Stiff and tight skin: A rear window into fibrosis without inflammation. Sci. Transl. Med. March 17, 2010; 2(23).
- FBN1 gene. https://ghr.nlm.nih.gov/gene/FBN1
- Eckes B, Wang F, Moinzadeh P, Hunzelmann N, Krieg T. Pathophysiological Mechanisms in Sclerosing Skin Diseases. Front Med (Lausanne). 2017;4:120. Published 2017 Aug 18. doi:10.3389/fmed.2017.00120 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5563304
- Myers KL, Mir A, Schaffer JV, Meehan SA, Orlow SJ, and Brinster NK. Segmental stiff skin syndrome (SSS): A distinct clinical entity. Journal of the American Academy of Dermatology. July 2016; 75(1):163-168. https://www.ncbi.nlm.nih.gov/pubmed/26944597
- Stiff skin syndrome. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=2833
- Gerber EE, Gallo EM, Fontana SC, Davis EC, Wigley FM, Huso DL, and Dietz HC. Integrin-modulating therapy prevents fibrosis and autoimmunity in mouse models of scleroderma. Nature. November 7, 2013; 503(7474):126-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3992987
- Kurtzman DJB, Wright NA, Patel M, and Vleugels RA. Segmental stiff skin syndrome (SSS): Two additional cases with a positive response to mycophenolate mofetil and physical therapy. Journal of the American Academy of Dermatology. December 2016; 75(6):237-239. https://www.ncbi.nlm.nih.gov/pubmed/27846975