Nevus spilus
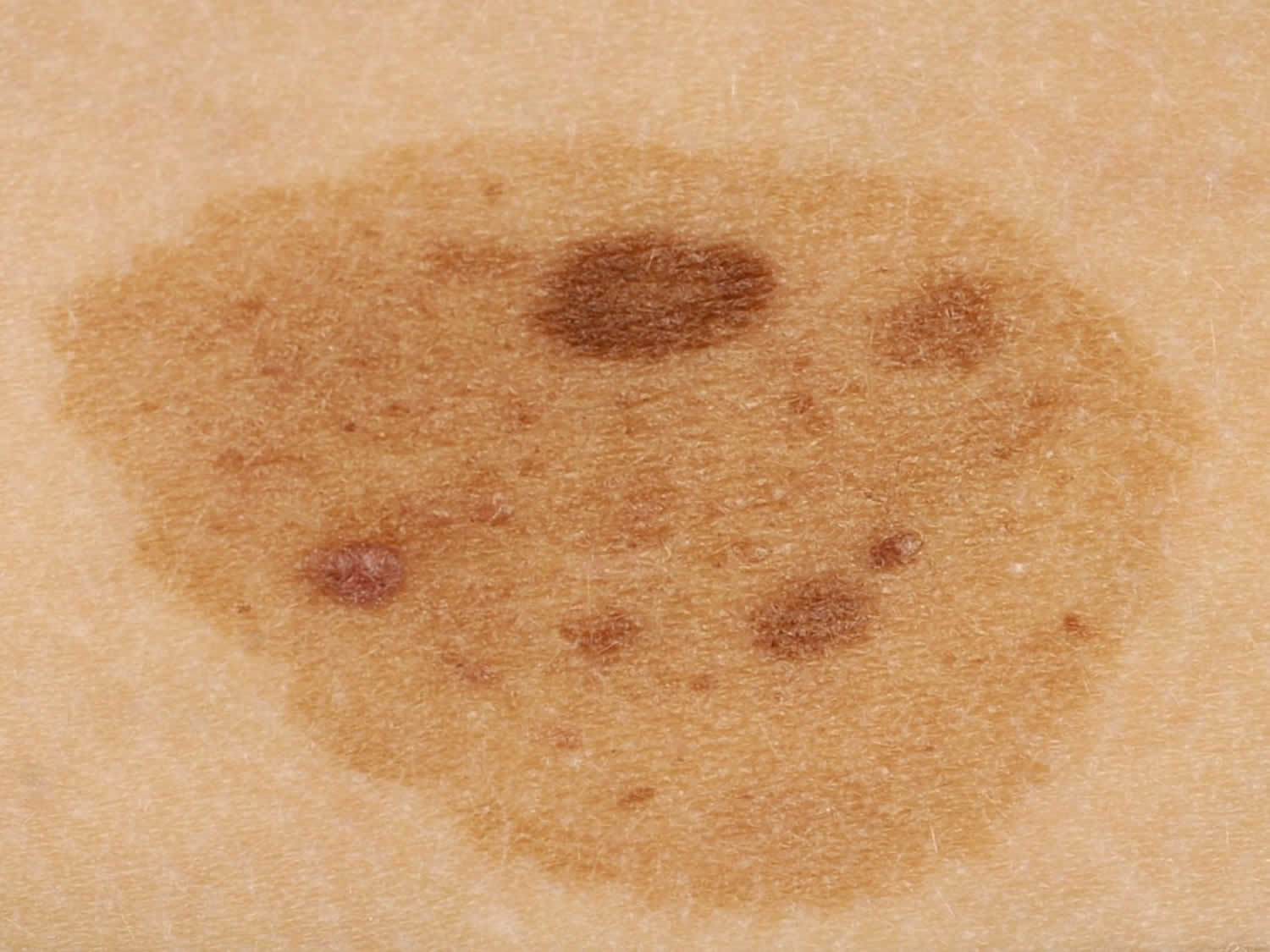
Nevus spilus also known as speckled lentiginous nevus or zosteriform lentiginous nevus, is a benign melanocytic cutaneous lesion consisting of a light brown background macule with numerous superimposed darker maculopapular speckles 1. Nevus spilus is characterized by tan macule containing darker macules or papules within its border 2. On histology, the background pigmented lesion of nevus spilus usually corresponds to a lentigo simplex or a cafe au lait macule, while the dark speckles show features of a variety of nevi: junctional, compound, intradermal, dysplastic, Spitz, blue, neurotized nevus, or ink spot lentigo 3.
Nevus spilus lesions range from small and isolated to giant or segmental, and may be associated with heritable syndromes 2. There are two clinically distinct variants. Nevus spilus maculosus is flat with evenly distributed macular hyperpigmentation likened to a polkadot pattern, and may be associated with phacomatosis pigmentovascularis. Nevus spilus papulosus is larger, with irregularly distributed larger papules in a “star map” pattern, and may be associated with phakomatosis pigmentokeratotica 4. Recent genetic studies have revealed two phenotypically and genetically distinct types of nevus spilus papulosus 5. Small, single lesions as well as large lesions associated with phakomatosis pigmentokeratotica have been shown to contain the activating HRAS G13R mutation 6. Agminated Spitz nevi arising in nevus spilus have recently been shown to have the same activating HRAS mutations as the nevus spilus, as well as additional amplification of HRAS, leading to hypothesize that they arise from the same postzygotic clone as the nevus spilus, but with the additional development of a second “hit” mutation 6. Larger, often segmental lesions containing large congenital-pattern nevi are referred to as nevus-spilus-type congenital melanocytic nevi. These have been shown to contain missense activating NRAS mutations involving Q61L, Q61H, and G13R 7. These discoveries indicate that nevus spilus is an expression of mosaicism through post-zygotic mutations in genes involved with the Ras pathway, and thus is an example of a mosaic RASopathy 8.
Nevus spilus is a relatively uncommon skin lesion found in 0.2%-2.3% of the general population. Nevus spilus lesions occur fairly equally in men and women and within different races; they may be present at birth (congenital) or have its onset in childhood, or even after the age of 20 years 9.
Despite the reports of melanoma arising within nevus spilus, the malignant potential of nevus spilus remains unclear 10. For a long time, nevus spilus was believed to be a harmless pigmented lesion. However, in 1957 Perkinson 11 reported a melanoma appearing on nevus spilus for the first time. Since then, less than 40 cases of melanoma developing within this entity have been published, sometimes with a fatal outcome 1. Reviewing the published literature, most cases of malignant transformation were found in Caucasian or black patients, more frequently on the trunk (64%) than the limbs (36%), with a female-male ratio of 56:44 and a mean age of 49 years 3. Melanoma on nevus spilus was usually one neoplasm, but multiple melanomas were observed within the same nevus spilus in three previous cases 12. The melanoma most found was superficial spreading melanoma (68%), followed by nodular (16%) and in situ melanoma (16%) 3. In 60% of cases, melanoma developed on small or medium-sized nevus spilus, 24% on zosteriform nevus spilus, and 16% on giant nevus spilus 3. In 52% of cases, nevus spilus was present at birth; in 33%, it was acquired during infancy; and in 14%, it appeared later 13.
The absolute risk for malignant transformation within nevus spilus remains unknown 14, but it is thought to vary from 0.13%-0.2% 3. An increased risk seems to exist when the nevus spilus is congenital or acquired in infancy, of macular type, and larger than 4 cm (especially giant and zosteriform variants) 3. Once a melanoma develops, it has a similar prognosis and management as compared with other melanomas 12. In summary. nevus spilus is an entity that requires further study, in order to clarify its biologic behavior and allow future development of standardized management guidelines.
Figure 1. Nevus spilus
Figure 2. Speckled lentiginous nevus
Nevus spilus symptoms
Clinically, nevus spilus generally consists of a single non-hairy lesion, with a medium size of 4.3 cm (± 3.5 cm) 14. Spotting within the lesion is more often macular than papular, sized 1-3 mm, and develop during a period of months to years 3. Nevus spilus can be divided into macular and papular variants, and further into three different size groups: small (<1.5 cm); medium (1.5-19.9 cm); and giant (>20 cm) 3. Less frequent segmental/zosteriform nevus spilus has also been described 3. Lesions can be found anywhere on the body, but involve especially the trunk and extremities 3.
Nevus spilus diagnosis
The diagnosis of a nevus spilus is usually based on the clinical appearance. If there is any doubt, examining the lesion with dermoscopy or taking a sample of the lesion for histology (biopsy) may show characteristic microscopic features.
Nevus spilus treatment
There is no standardized management approach for nevus spilus. Overall, patients should be advised to perform self-examination to monitor for any changes in their nevi and have a structured longterm follow-up with the help of sequential digital dermatoscopy and, if available, reflectance confocal microscopy 15. This strategy, coupled with judicious use of biopsy for suspicious areas, seems to assist in the early detection of melanoma 16. Prophylactic nevus spilus excision without pathologic confirmation of dysplasia or malignancy is not supported by the available literature 3. In the setting of dysplasia or malignant melanoma, complete nevus spilus excision is reasonable, size permitting, in order to eliminate the “faulty background” and to search for any multifocal melanomas 3.
References- Brito MH, Dionísio CS, Fernandes CM, Ferreira JC, Rosa MJ, Garcia MM. Synchronous melanomas arising within nevus spilus. An Bras Dermatol. 2017;92(1):107–109. doi:10.1590/abd1806-4841.20175230 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5312189
- Porubsky C, Teer JK, Zhang Y, Deschaine M, Sondak VK, Messina JL. Genomic analysis of a case of agminated Spitz nevi and congenital-pattern nevi arising in extensive nevus spilus. J Cutan Pathol. 2018;45(2):180–183. doi:10.1111/cup.13082 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768454
- Corradin MT, Giulioni E, Fiorentino R, Santeufemia DA, Re GL, Vettorello A. In situ malignant melanoma on nevus spilus in an elderly patient. Acta Dermatovenerol Alp Pannonica Adriat. 2014;23:17–19.
- Happle R. Speckled lentiginous naevus: which of the two disorders do you mean? Clinical and experimental dermatology. 2009;34(2):133–135.
- Krengel S, Widmer DS, Kerl K, Levesque MP, Schiestl C, Weibel L. Naevus spilus-type congenital melanocytic naevus associated with a novel NRAS codon 61 mutation. The British journal of dermatology. 2016;174(3):642–644.
- Sarin KY, McNiff JM, Kwok S, Kim J, Khavari PA. Activating HRAS mutation in nevus spilus. The Journal of investigative dermatology. 2014;134(6):1766–1768.
- Kinsler VA, Krengel S, Riviere JB, et al. Next-generation sequencing of nevus spilus-type congenital melanocytic nevus: exquisite genotype-phenotype correlation in mosaic RASopathies. The Journal of investigative dermatology. 2014;134(10):2658–2660.
- Lee SB, Hummel HM, Krengel S, Enk A, Haenssle HA. Mosaic RASopathies: phenotypic and genotypic differentiation of naevus spilus-type congenital melanocytic naevus and segmental naevus spilus. Journal of the European Academy of Dermatology and Venereology : JEADV. 2016;30(7):1244–1246.
- Manganoni AM, Pavoni L, Farisoglio C, Sereni E, Calzavara-Pinton P. Report of 27 cases of naevus spilus in 2134 patients with melanoma: is naevus spilus a risk marker of cutaneous melanoma? J Eur Acad Dermatol Venereol. 2012;26:129–130.
- Meguerditchian AN, Cheney RT, Kane 3rd JM. Nevus Spilus with Synchronous Melanomas: Case Report and Literature Review. J Cutan Med Surg. 2009;13:96–101.
- Perkinson NG. Melanoma arising in café au lait spot of neurofibromatosis. Am J Surg. 1957;93:1018–1020.
- Corradin MT, Zattra E, Fiorentino R, Alaibac M, Belloni-Fortina A. Nevus Spilus and Melanoma: Case Report and Review of the Literature. J Cutan Med Surg. 2010;14:85–89.
- Abecassis S, Spatz A, Cazeneuve C, Martin-Villepou A, Clerici T, Lacour JP, et al. Melanoma within naevus spilus: 5 cases. Ann Dermatol Venereol. 2006;133:323–328.
- Karam SL, Jackson SM. Malignant Melanoma Arising Within Nevus Spilus. Skinmed. 2012;10:100–102.
- Tavoloni Braga JC, Gomes E, Macedo MP, Pinto C, Duprat J, Begnami MD, et al. Early detection of melanoma arising within nevus spilus. J Am Acad Dermatol. 2014;70:e31–e32.
- Haenssle HA, Kaune KM, Buhl T, Thoms KM, Padeken M, Emmert S, et al. Melanoma arising in segmental nevus spilus: Detection by sequential digital dermatoscopy. J Am Acad Dermatol. 2009;61:337–341.