What is subclavian steal syndrome
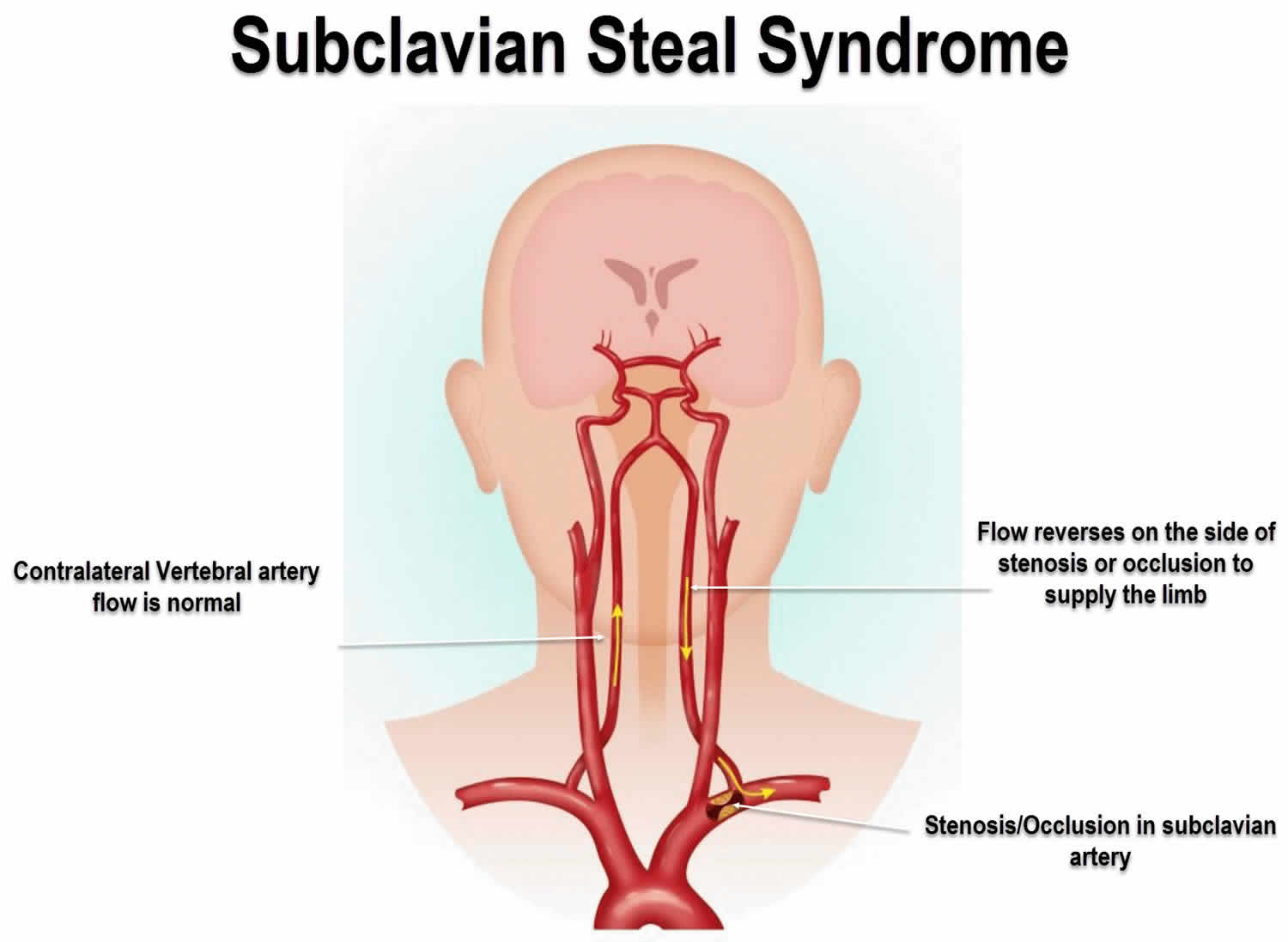
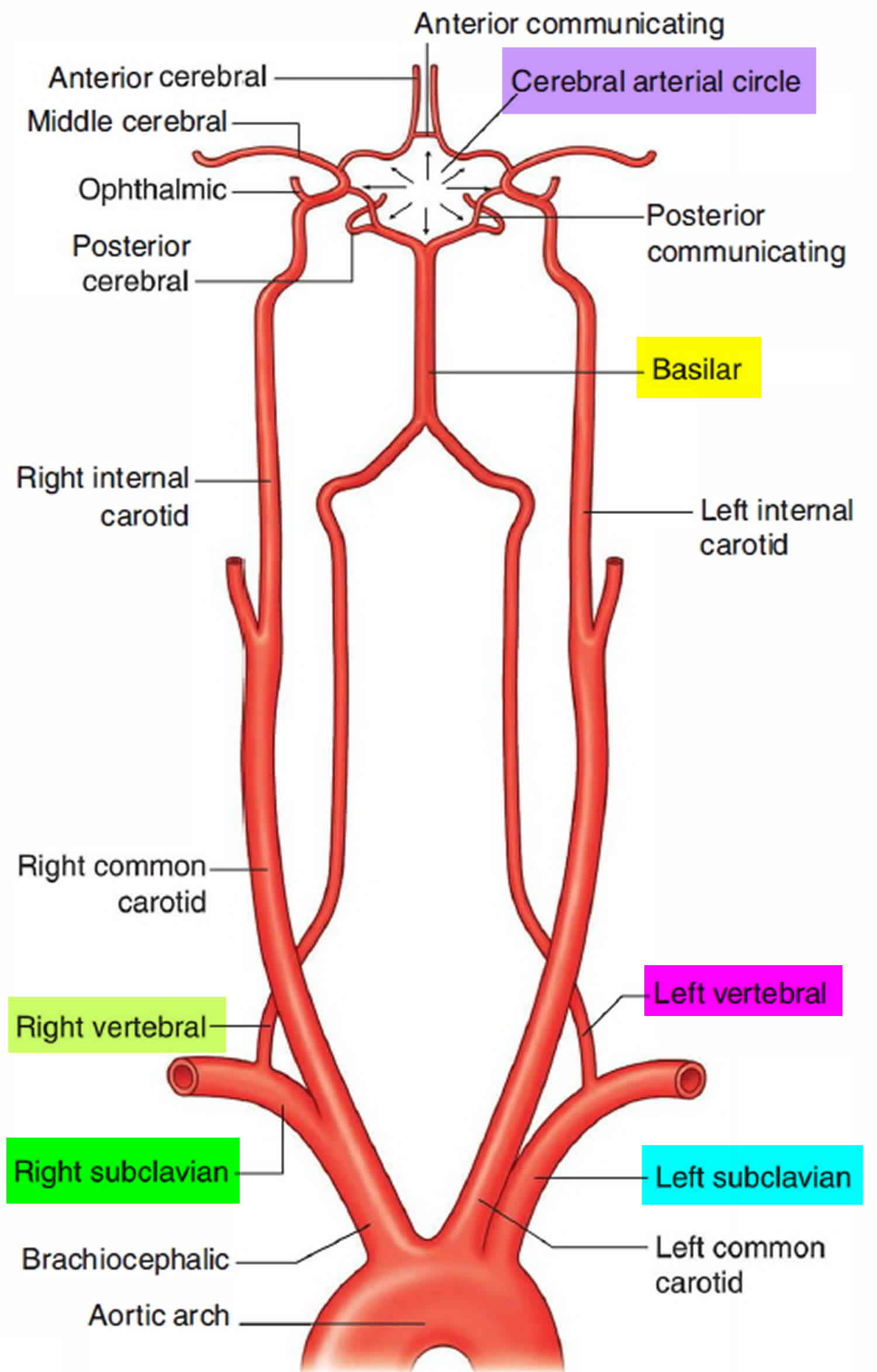
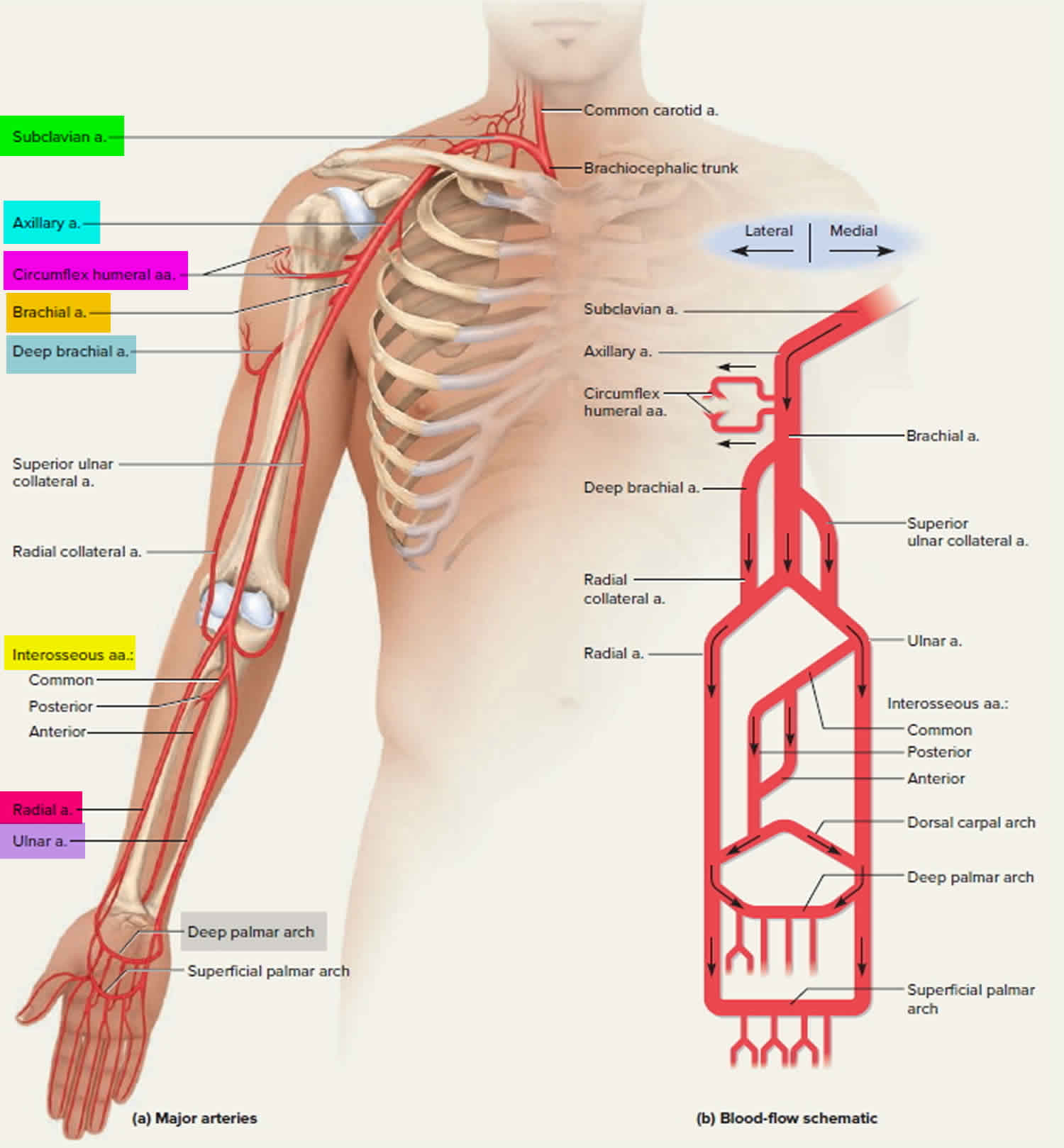
Subclavian steal syndrome is a vascular disorder in which occlusion or stenosis of the subclavian artery proximal to the vertebral artery origin (which is the subclavian artery) causes altered vascular haemodynamics that result in retrograde blood flow in the ipsilateral vertebral artery toward the upper arm, distal to the subclavian artery narrowing, where decreased blood pressure had been established and is associated with transient neurologic symptoms related to cerebral ischemia. Subclavian steal is a type of peripheral artery disease in which reduction or absence of flow in the proximal subclavian artery reverses the normal direction of blood flow in the vertebral artery, usually in the setting of subclavian artery occlusion or stenosis proximal to the origin of the vertebral artery 1. Blood is drawn from the contralateral vertebral, basilar, or carotid artery to provide flow in the affected subclavian artery distal to the stenosis 2. Alternatively, innominate artery disease has also been associated with retrograde flow in the ipsilateral vertebral artery, particularly where the subclavian artery origin is involved.
Subclavian steal is frequently asymptomatic because of the abundant collateral blood supply in the head, neck, and shoulder and may be discovered incidentally on ultrasonography or angiography done for other indications, or it may be prompted by a clinical examination finding of reduced unilateral upper-limb pulse or blood pressure 1. In some cases, patients may develop upper-limb ischemic symptoms due to reduced arterial flow in the setting of subclavian artery occlusion, or they may develop neurologic symptoms due to posterior circulation ischemia associated with exercise of the ipsilateral arm 3. Rarely, however, some patients may provoke the subclavian steal syndrome with exercise and present with transient ipsilateral arm claudication, ataxia, and/or angina.
Because most patients do not seek medical advice unless symptoms occur, the true prevalence of subclavian artery occlusive disease and subclavian steal syndrome is unknown 4.
Subclavian steal syndrome treatment has traditionally consisted of open subclavian artery revascularization, typically via carotid-subclavian bypass or subclavian artery transposition, which are generally durable procedures. Newer, less invasive options include endovascular intervention with recanalization as appropriate and angioplasty and stenting if required.
Figure 1. Subclavian artery and branches for the brain
Figure 2. Subclavian artery and branches for the arms
Subclavian steal syndrome causes
The underlying factor leading to subclavian steal syndrome is proximal subclavian artery occlusion or severe stenosis. In most cases, this is a result of atherosclerotic arterial disease, which has a preponderance for the left side. The left subclavian artery is the aortic arch branch vessel most commonly affected by atherosclerosis; therefore, it is not surprising that the left subclavian artery is involved with subclavian steal three times more frequently than the right subclavian artery is. On the right side, innominate artery disease or occlusion may result in occlusion of the subclavian artery origin.
Subclavian steal syndrome causes:
- Atherosclerosis: ~95%
- Vasculitides, e.g. Takayasu arteritis, radiation
- Thoracic aortic dissection
- Blalock-Taussig shunt
- Congenital
- interrupted aortic arch
- preductal aortic coarctation
- right aortic arch with isolated left subclavian
The risk factors for developing atherosclerotic plaques have been recognized for some time and are categorized as either nonmodifiable or modifiable.
Nonmodifiable risk factors include the following:
- Age
- Male sex
- Family history
Modifiable risk factors include the following:
- Cigarette smoking
- Hypercholesterolemia
- Diabetes mellitus
- Hypertension
- Hyperhomocysteinemia
Although retrograde blood flow in the vertebral artery is usually noted angiographically in association with proximal ipsilateral subclavian artery occlusion, subclavian steal may also occur with hemodynamically significant subclavian artery stenosis
Other, less common causes of subclavian occlusive disease include inflammatory arteriopathies such as Takayasu arteritis or giant cell arteritis. Congenital anomalies may also result in isolation of the subclavian artery and sacrifice of the proximal subclavian artery in aortic surgery (eg, a Blalock-Taussig procedure for tetralogy of Fallot or coverage of the left subclavian origin with a thoracic endovascular stent graft).
Thoracic outlet compression syndrome can cause subclavian artery occlusion, but this typically involves the subclavian artery beyond the vertebral artery origin.
Subclavian steal syndrome symptoms
Patients with subclavian steal syndrome are usually asymptomatic. In addition, with few exceptions, proximal subclavian stenosis or occlusion rarely causes symptoms of arm ischemia. Muscle cramping due to arm ischemia typically occurs in laborers performing vigorous work, often with arms elevated above the head. If the increased oxygen demand from arm exercise exceeds the ability of collateral vessels to provide sufficient blood flow, cerebral ischemia may occur as more blood is siphoned from the brain via the vertebrobasilar system.
Numerous symptoms are associated with posterior-circulation cerebral ischemia. Symptoms of dizziness or vertigo occur in more than 50% of patients, and syncope and dysarthria have been noted in 18% and 12.5%, respectively. Visual symptoms secondary to vestibular dysfunction or nystagmus include a sensation of objects moving and inability to focus, as well as monocular or binocular visual loss. Diplopia occurs in 19% of cases. Fortunately, these transient ischemic episodes seldom progress to cause cerebral infarction.
True subclavian steal syndrome cannot occur without retrograde blood flow in a vertebral artery associated with proximal ipsilateral subclavian artery stenosis or occlusion. In a healthy individual, blood pressures in both arms should be similar. Without a significant difference in blood pressure between the patient’s arms, proximal subclavian stenosis or occlusion cannot be present.
An invariable finding in patients with symptoms of subclavian steal syndrome is a difference in upper-extremity pulses and brachial systolic blood pressures between the patient’s arms. Therefore, with a simple physical examination, the clinician can effectively eliminate significant subclavian arterial lesions without the need for angiography or duplex ultrasonography.
Ipsilateral upper limb
- weak or absent pulse
- decreased systolic blood pressure in the affected side; systolic blood pressure difference between the brachial arteries are more than 20 mmHg 5
- arm claudication (rare due to collateral perfusion)
Neurological symptoms (exacerbated by arm exercise)
- dizziness/vertigo/syncope
- ataxia
- visual changes
- dysarthria
- weakness/sensory disturbances
The internal mammary artery (IMA) arises from the inferior aspect of the proximal subclavian artery, opposing the origin of the vertebral artery. Recurrent symptoms of angina pectoris after otherwise successful coronary revascularization with a left internal mammary artery (LIMA) graft may also indicate a hemodynamically significant proximal left subclavian stenosis.
Atherosclerotic lesions (stenosis or occlusion) of the proximal vertebral artery may produce similar symptoms. Occlusive disease of the vertebral artery should be considered if posterior circulation symptoms occur with normal blood pressures in the affected arm.
Subclavian steal syndrome diagnosis
After an adequate physical examination, routine laboratory studies should be ordered to address risk factors for atherosclerosis. These tests should include a fasting lipid profile and blood glucose.
Imaging studies that may be considered include duplex ultrasonography, computed tomography (CT) angiography (CTA), four-vessel cerebral arteriography, magnetic resonance angiography (MRA), and chest radiography 6. Electrocardiography (ECG) may also be considered.
Chest radiography is performed to look for unusual causes of subclavian artery obstruction (eg, cervical rib).
Because many of these patients have concomitant ischemic heart disease, ECG is advisable.
Ultrasonography
Color Doppler ultrasonography is the preferred examination for subclavian steal syndrome, but it is operator dependent. In addition, direct examination of the proximal subclavian artery is compromised by the overlying clavicle, ribs, and sternum.
Subclavian steal syndrome is now most commonly diagnosed during Doppler ultrasonography examination of the neck arteries 7. In most cases, because of anatomic constraints imposed by the chest wall, it is difficult to assess the proximal subclavian artery adequately by means of ultrasonography.
CT angiography and MR angiography are used to confirm any suspected subclavian steal cases found on ultrasound exams, because not all retrograde vertebral flow seen on ultrasound examinations constitute true subclavian steal. Some have been shown to stem from proximal vertebral artery stenosis or occlusion. These techniques can directly show the anatomic features of subclavian stenosis or occlusion, the presence of retrograde vertebral flow, and any associated extracranial and intracranial stenoses 8.
Angiography
Searching for significant lesions in the ipsilateral carotid artery is important. If brachial artery pressures are significantly decreased (>20%) in comparison with the contralateral side, arch aortography should be performed to further define the problem and plan for operative or interventional repair.
Although conventional angiography remains the gold standard investigation for the diagnosis of subclavian occlusive disease in most centers, CT angiography has replaced this modality as the first-line test. It has a high sensitivity and specificity and has the advantage of being able to identify other lesions in the arch vessels. No arterial puncture is required. Currently, CT angiography is regarded as excellent for planning and sizing in endovascular treatment, and only rarely is conventional four-vessel arteriography required.
Four-vessel cerebral arteriography can define the problem anatomically, demonstrating retrograde blood flow in the vertebral artery and associated proximal occlusive subclavian artery lesions. In addition, arteriography serves as a road map for possible repair (surgical or endovascular) of the subclavian artery.
MR angiography has become an alternative to conventional angiography for the assessment of subclavian steal syndrome, especially in patients with renal dysfunction. Unfortunately, however, MR angiography often overestimates the degree of arterial obstruction and is associated with a higher degree of false-positive results.
Subclavian steal syndrome treatment
Most commonly, subclavian artery steno-occlusive disease is not associated with symptoms and therefore can be managed conservatively with attention to diabetes and hyperlipidemia management, cessation of smoking, and antiplatelet therapy. When symptomatic, coincident significant carotid system stenoses should be excluded. Endovascular treatment is considered the first-line intervention in medically refractory patients with symptomatic subclavian steal syndrome. Surgical options, such as carotid-subclavian bypass, are generally reserved for patients in whom endovascular treatment has failed 2.
Patients with atherosclerotic occlusive plaques in the subclavian artery are usually asymptomatic and therefore require no treatment. However, if either vertebrobasilar symptoms or exercise-induced arm pain occurs, a search for subclavian artery occlusive disease should be undertaken.
No medical therapy is known to be capable of effectively treating subclavian steal syndrome. However, if the cause of subclavian steal syndrome is determined to be atherosclerotic stenosis or occlusion of the proximal subclavian artery, patients should be treated with lifelong antiplatelet therapy to reduce the risk of associated myocardial infarction, stroke, and other vascular causes of death.
If the ischemic symptoms are due to retrograde vertebral artery blood flow, surgical or interventional (ie, angioplasty or stenting) therapy is indicated. The goal is to restore antegrade blood flow in the vertebral artery, thereby alleviating symptoms. This goal can be achieved by restoring adequate perfusion pressure to the affected arm so that collateral blood flow from the head and neck is not required during arm exercise.
Surgical or interventional treatment should not be offered to treat subclavian artery stenosis or occlusion in the absence of symptoms related to either cerebral or ipsilateral arm ischemia. Symptoms (eg, ataxia, dysarthria, diplopia, and muscle cramping in the arm) must be associated with exercise and resolve quickly after cessation of exercise.
Endovascular treatment
Currently, endovascular (ie, catheter-based) treatment of the proximal subclavian artery is the most common approach to the management of proximal subclavian lesions. Although open bypass or transposition is the gold standard, retrospective analysis shows that in appropriately selected patients, endovascular treatment has equally good outcomes.
The technical success rate is 86-100%. In comparison with the open technique, complications with the endovascular technique are associated more with plaque emboli and bleeding from access sites than with local nerve injury. Moreover, most of these endovascular procedures can be performed successfully on an outpatient basis.
Although to date, there have been no double-blind randomized, controlled trials comparing balloon angioplasty alone with angioplasty and stenting for this condition, a systemic review of multiple retrospective observational studies concluded that stenting was superior to balloon angioplasty alone 9.
Endovascular recanalization and stenting improve perfusion to the arm and treat subclavian steal syndrome (see the image below). Because plaque in the proximal subclavian artery is actually part of the atherosclerotic lesion in the aortic arch, the stent must traverse the entire plaque and protrude slightly into the lumen of the aortic arch 10.
Endovascular treatment complications
Complications related to endovascular treatment can occur at the access site (femoral or brachial artery) or at the target vessel (subclavian or vertebral artery). Access site bleeding or hematoma is very uncommon but can occur. Target vessel thrombosis, dissection, or distal embolization have also been reported. These complications occur less than 4% of the time.
In a study comparing immediate and long-term results of endovascular treatment of steno-occlusive disease of subclavian arteries in 245 patients (125 with subclavian stenosis and 120 with subclavian occlusion), Karpenko et al 11 reported intraoperative transitory ischemic attacks in the vertebrobasilar system in one patient from group 1 and three from group 2. Nine patients from group 1 and 12 from group 2 had repeat interventions in the long term. Cumulative primary 4-year stent patency was 89.8% in group 1 and 87% in group 2. There was an increased risk of stent thrombosis or in-stent restenosis in patients with stents longer than 40 mm.
Proximal subclavian endarterectomy
Transthoracic approach to endarterectomy provided an excellent anatomic view for revascularizing the subclavian artery. Currently, direct surgical approaches to the proximal subclavian artery are of historical interest only, because endarterectomy has largely been replaced by less invasive extrathoracic bypass procedures; intraoperative mortality had ranged from 6% to 19%.
With endarterectomy, the artery is opened after vascular control is obtained, and the plaque, diseased intima, and internal elastic lamina of the vessel are removed, thus disobliterating the lumen.
Because the occlusive lesions in the proximal left subclavian artery develop as an extension of plaque from the aortic arch, partial occlusion of the arch must be performed to ensure that the entire lesion is effectively removed. On the left side, surgical exposure must be obtained through an anterolateral thoracotomy in the third intercostal space. On the right side, exposure can be accomplished through a transverse incision in the base of the neck without the need for thoracotomy.
Carotid intervention
In patients with severe concomitant carotid artery disease, this condition may contribute to cerebral hypoperfusion in the setting of subclavian steal. Carotid endarterectomy for carotid bifurcation disease may improve cerebral perfusion. Proximal common carotid artery disease may be best approached angiographically for angioplasty or stenting.
Surgical bypass or transposition
Extrathoracic carotid-subclavian bypass
Extrathoracic carotid-subclavian bypass using a prosthetic conduit has largely replaced subclavian endarterectomy; mortality is 0.5%. Surgical exposure is easily obtained through a transverse incision at the base of the neck that extends 5-7 cm laterally from the sternal notch parallel to the clavicle.
Conventionally, 6- to 8-mm Dacron or polytetrafluoroethylene (PTFE) prosthetic grafts are used; autogenous vein has poor 5-year patency rates 12. End-to-side (graft-to-artery) anastomoses can be performed without difficulty. The procedure is generally well tolerated.
Subclavian transposition
The subclavian artery can also be transposed to a new origin on the side of the common carotid artery. This operation is also performed through a transverse incision at the base of the neck and has the advantages of not requiring prosthetic material and of excluding the stenosis as a source of potential emboli. The dissection required is more extensive than that required for carotid-subclavian bypass, and care must be taken to avoid injury to the thoracic duct on the left side. An end-to-side subclavian-to-carotid anastomosis is performed.
Long-term results are similar to those of carotid-subclavian bypass. In patients who have an early origin of the vertebral artery or have had an internal thoracic artery harvested for coronary surgery, the bypass procedure is preferred.
Axillary-axillary bypass and variants
In settings where the ipsilateral carotid is unsuitable for carotid-subclavian bypass, the axillary artery may be revascularized via axillary-axillary bypass using a subcutaneously tunneled ring-reinforced prosthetic graft. Alternatively, axillofemoral bypass may be performed. These grafts are often superficial and are prone to infection. In severe innominate artery disease, antetracheal or sequential retroesophageal carotid-carotid and carotid-subclavian bypass can be performed.
Surgical treatment complications
Complications related to surgical treatment may be classified as either local or cerebral. Local complications are related to injury to adjacent structures that may be encountered during the course of the operation (eg, the thoracic duct injury or the phrenic nerve) and are quite uncommon.
Cerebral complications are related to brain ischemic symptoms and can be caused either by thrombosis of the repair or by embolism up the carotid or vertebral arteries during the course of the procedure. Cerebral ischemia during common carotid occlusion is most unusual; therefore, a shunt is not used for the procedure. Postoperative stroke rates are in the range of 1.5-2.1%.
Long-Term Monitoring
There are no standardized guidelines for follow-up after treatment. Patients are seen at 3- to 6-month intervals for the first year and annually thereafter. At every visit, blood pressures should be checked in both arms. A decline in pressure on the operated side may be the first sign that recurrent stenosis may be developing.
Follow-up duplex scans of the reconstruction should be obtained at 6-month and 1-year intervals. Patients who have had subclavian stents should be treated with both aspirin and clopidogrel for a period of 6-12 months. Thereafter, a single antiplatelet agent is appropriate.
Subclavian steal syndrome prognosis
Patients with asymptomatic subclavian steal syndrome have a benign natural history, and no specific treatment is required.
With proximal subclavian artery occlusive disease, patients may first seek medical treatment for symptoms of exercise-induced arm claudication rather than for neurologic symptoms associated with arm exercise. Furthermore, if a patient has undergone coronary revascularization with a left internal mammary artery (LIMA) graft, new-onset angina may herald proximal left subclavian stenosis. With subclavian steal syndrome, if neurologic symptoms do occur, they tend to be transient (eg, hypoperfusive transient ischemic attack) and seldom lead to stroke.
For patients in whom antegrade vertebral blood flow is reestablished by means of either surgical revascularization or endovascular stenting of the diseased subclavian artery, the prognosis is highly favorable. The stroke risk from the procedure is low, and the long-term durability is excellent.
Operative morbidity and mortality are substantially higher for transthoracic subclavian artery revascularization than for extrathoracic repair, mainly because of the morbidity associated with thoracotomy. Recognizing this problem, surgeons have virtually abandoned this approach in favor of extrathoracic revascularization in the form of either carotid-subclavian bypass or subclavian transposition. Operative mortality for either of these extrathoracic procedures approaches zero, and morbidity is very low.
The results of retrograde (brachial puncture) or antegrade (femoral puncture) percutaneous subclavian angioplasty or stent placement are also excellent 13. Most authors report initial success rates of 91-100%, and the complication rate is reasonably low (3-17%). After successful stenting of the subclavian artery, the restenosis rate is 0-16% after 12-48 months’ follow-up. The technical success rate of subclavian angioplasty ranges from 86% to 100%. The restenosis rate after subclavian angioplasty is 5-22% after 28-60 months’ follow-up.
References- Subclavian Steal Syndrome. https://emedicine.medscape.com/article/462036-overview
- Satti SR, Golwala SN, Vance AZ, Tuerff SN. Subclavian steal: Endovascular treatment of total occlusions of the subclavian artery using a retrograde transradial subintimal approach. Interv Neuroradiol. 2016 Jun. 22 (3):340-8
- Sharma VK, Chuah B, Teoh HL, Chan BP, Sinha AK, Robless PA. Chronic brainstem ischemia in subclavian steal syndrome. J Clin Neurosci. 2010 Oct. 17 (10):1339-41
- Labropoulos N, Nandivada P, Bekelis K. Prevalence and impact of the subclavian steal syndrome. Ann Surg. 2010 Jul. 252 (1):166-70
- Tan TY, Schminke U, Lien LM, Tegeler CH. Subclavian steal syndrome: can the blood pressure difference between arms predict the severity of steal?. (2002) Journal of neuroimaging : official journal of the American Society of Neuroimaging. 12 (2): 131-5.
- Potter BJ, Pinto DS. Subclavian steal syndrome. Circulation. 2014 Jun 3. 129 (22):2320-3
- Moghazy KM. Value of color Doppler sonography in the assessment of hemodialysis access dysfunction. Saudi J Kidney Dis Transpl. 2009 Jan. 20 (1):35-43.
- Toprak C, Yesin M, Mustafa Tabakci M, Demirel M, Avci A. Coronary Subclavian Steal Syndrome Evaluated with Multimodality Imaging. Intern Med. 2015. 54 (21):2717-20.
- Chatterjee S, Nerella N, Chakravarty S, Shani J. Angioplasty alone versus angioplasty and stenting for subclavian artery stenosis–a systematic review and meta-analysis. Am J Ther. 2013 Sep-Oct. 20 (5):520-3.
- Song L, Zhang J, Li J, Gu Y, Yu H, Chen B, et al. Endovascular stenting vs. extrathoracic surgical bypass for symptomatic subclavian steal syndrome. J Endovasc Ther. 2012 Feb. 19 (1):44-51
- Karpenko A, Starodubtsev V, Ignatenko P, Gostev A. Endovascular Treatment of the Subclavian Artery Steno-Occlusive Disease. J Stroke Cerebrovasc Dis. 2017 Jan. 26 (1):87-93.
- Ziomek S, Quiñones-Baldrich WJ, Busuttil RW, Baker JD, Machleder HI, Moore WS. The superiority of synthetic arterial grafts over autologous veins in carotid-subclavian bypass. J Vasc Surg. 1986 Jan. 3 (1):140-5
- Wrotniak L, Kabłak-Ziembicka A, Rosławiecka A, Musiałek P, Bogacki P, Trystuła M, et al. Resolution of ischemic symptoms after percutaneous angioplasty for a symptomatic subclavian artery stenosis. J Vasc Surg. 2016 Sep. 64 (3):684-91