Symmastia
Symmastia is a relatively rare implant displacement problem that occurs when the skin and muscle between the breasts over the sternum (breastbone) detaches and the two pockets of tissue that hold the breast implants come together to form one pocket 1. This allows the implants to come together in the middle, creating the appearance of a “uniboob” or “bread loafing” and sometimes causing discomfort or pain. Symmastia (Greek: syn, meaning “together” and mastos, meaning “breast”) is defined as a medial confluence of the breasts 2. Congenital symmastia is very rare 3 and very few cases of congenital symmastia were reported in the literature, with different techniques used for its correction, but there is no standard treatment for congenital symmastia 4.
The most common reason that symmastia develops in women who have had breast reconstruction is that during the mastectomy, the surgeon removed too much tissue too close to the sternum. Also, the implants that were inserted may have been too large. Larger implants require a bigger pocket and put more tension on the skin that has to attach to the sternum and hold the implant.
It’s often difficult to correct symmastia and it may require more than one surgery. In most cases, surgery will involve removing the implants and replacing them with new (usually smaller) implants. Also, your plastic surgeon will reattach the skin that has detached from the sternum using internal stitches and make adjustments to the pockets of tissue in the chest that hold the implants in place, often reinforcing their boundaries using a dermal matrix product (a skin substitute made mostly of collagen) or mesh.
Another option for correcting symmastia may be to have your plastic surgeon remove your implants and replace them with transplanted flaps of tissue from another place on your body. This is called “autologous reconstruction” or “flap reconstruction.”
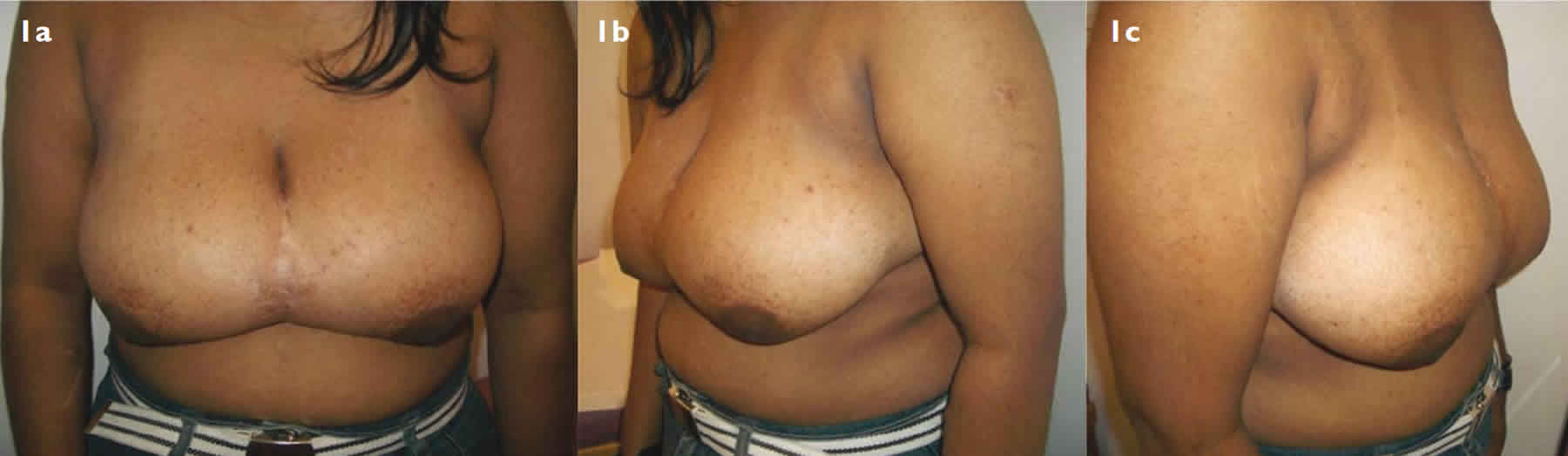
Figure 1. Congenital symmastia
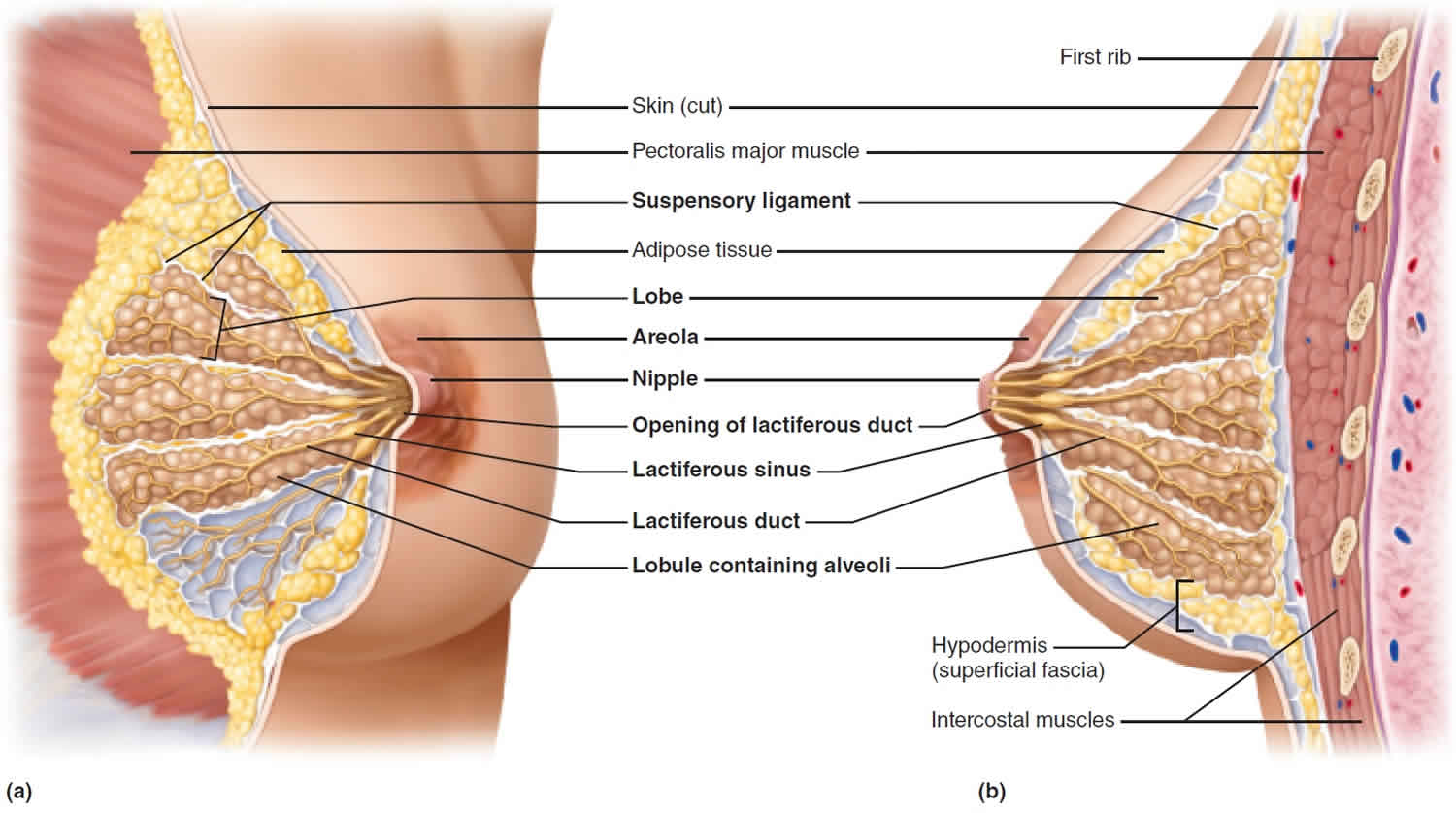
[Source 5 ]Figure 2. Breast anatomy
Symmastia causes
Commonly referred to as a “uniboob” or “bread loafing,” symmastia is a condition in which the breasts fuse into one breast instead of two separate breasts. This is usually the result of technical complications during breast implant surgery caused by over-dissection of the medial pocket over the sternum in the subglandular plane or by an over-division of the pectoralis muscle origin along the sternum in a submuscular plane 1. The most common reason that symmastia develops in women who have had breast reconstruction is that during the mastectomy, the surgeon removed too much tissue too close to the sternum. Also, the implants that were inserted may have been too large. Larger implants require a bigger pocket and put more tension on the skin that has to attach to the sternum and hold the implant.
If your breast implants were placed beneath the pectoral muscle, this could cause your skin and the pectoral muscle to pull away from the sternum. Some of the causes of symmastia may include:
- Breast implants are too large or wide for the patient’s body frame
- Implants are placed too close to the center line of the chest
- Improper placement of one or both implants
- Chest tissues, including glandular and connective tissues, or the pectoral muscles are pushing the implants closer together
Congenital symmastia
Congenital symmastia is a rare clinical anomaly, which represents webbing across the midline of the breasts that are usually symmetric 5. Like many anomalies of ectodermal origin, a broad spectrum of defects may be observed varying from an empty skin web to an apparent confluence of breast tissue across the midline 6. Few cases of congenital symmastia were reported in the literature, with different techniques used for its correction, but there is no standard treatment for congenital symmastia 4.
Congenital symmastia was reported for the first time by Spence et al 2 in 2 cases with successful treatment. Piza-Katzer et al 7 reported 2 cases of congenital symmastia in a mother and a daughter, and they found the abnormal arrangement of collagen fibers in the breast tissue (including Cooper’s ligament) in both cases, and so, they assumed that this condition may have a familial cause.
There is a broad spectrum of congenital symmastia varying from an empty skin web to an apparent confluence of breast tissue across the midline. So, if the deformity is minimal, the patient should be informed about the complications that could result from the operation to be weighed against the benefit that she can get from the operation. These complications include asymmetry, contour irregularities, and scarring.
Because the midline confluence of the breasts could contain fatty and glandular tissue, the degree of congenital symmastia could be affected by the fluctuations in body weight and by the breast maturity. So, the operation should be performed after breast maturity is complete, and the patient’s weight is stable.
Symmastia prevention
Choosing a highly skilled, board-certified surgeon can reduce or prevent symmastia from developing. Selecting the implant size and shape that is best suited to your unique anatomy can also decrease your risk of symmastia.
Symmastia symptoms
The typical symptoms of symmastia are pain, discomfort, and visible distortion of the breasts.
Symmastia treatment
While your surgeon can provide you with a separating bra to help with your symmastia, it does not offer a permanent fix. To permanently treat symmastia, you must undergo breast revision surgery. The type of revision procedure you need depends on the details of your previous breast augmentation procedure. Options may include a transaxillary or transareolar endoscopical approach, bilateral periareolar incisions with subcutaneous dissection, inframammary, subxiphoid or suprasternal approaches, or a combination of these. Other similar methods adopted in gynecomastia and breast-conserving surgery for cancer may also be considered 8. Although a sternal incision would allow direct access and exposure, a long marked surgical scar with a higher tendency for keloid formation would be a disadvantage. A periareolar approach requires a surgical wound on the breast and this may detract from its advantage. In practice, however, the current results show that the surgical wound around the nipple actually becomes inconspicuous after the surgery. An important point to note is to avoid injury and burns at the edge of the skin and especially at the nipple.
Submuscular revision
If symmastia occurs after submuscular breast augmentation (placement of the breast implant beneath the pectoral muscle), the breast pocket will need to be repaired to create a more natural-looking separation between the breasts.
Subglandular revision
When symmastia occurs in patients who have undergone subglandular breast augmentation (placement of the breast implants above the pectoral muscle), the implants may be removed during revision surgery and replaced under the muscle.
Implant replacement
In cases where symmastia has developed as a result of having oversized breast implants, the implants may be removed and replaced with more proportionally sized implants during a revision procedure.
Capsulorrhaphy and excess fat removal
Capsulorrhaphy, also known as the internal bra procedure, corrects symmastia with the placement of internal sutures to reposition the breast implants. Another option involves removing excess fat from the sternum area to separate the breasts.
Congenital symmastia treatment
The ideal technique for congenital symmastia correction should include 3 steps 5. First is the removal of the excess tissue between the 2 breasts. This is achieved either with surgical resection 9 or with liposuction 10. The use of liposuction only was reported to give successful result by 1 study 4, but in another study 9, the correction was insufficient, and a second procedure was performed with resection of the glandular-fatty tissue in the cleavage and suturing the skin to the chest wall.
Second is to fix the skin of the intermammary sulcus to the underlying periosteum with sutures either at the midline 10 or at the lateral sternal border 9. These sutures can be inserted through small inframammary fold incision 9, periareolar incision 11 or vertical scar mammoplasty incision 12. However, the inframammary incision gives superior cosmetic result as it is less visible. These sutures cause some dimpling, but it resolves with time 11.
The third step is the application of postoperative compression to the intermammary sulcus to facilitate the healing between the skin and the chest wall either with a bolster 10 or a sternal shaping bra 4.
References- Wong, M. T.; Cheong, E. C.; Lim, J.; Lim, T. C. (2007). “Creation of an intermammary sulcus in congenital synmastia”. Singapore Medical Journal. 48 (1): e29–e31. https://www.sma.org.sg/smj/4801/4801cr9.pdf
- Spence RJ, Feldman JJ, Ryan JJ. Symmastia: the problem of medial confluence of the breasts. Plast Reconstr Surg. 1984;73:261–269.
- Ankri A, Bureau H. [Third operation for breast hypertrophy]. Ann Chir Plast Esthet 1990; 35:324-6. French
- Karamese M, Hanci M, Abaci M, et al. An easy way for congenital symmastia correction. Aesthetic Plast Surg. 2014;38:369–372.
- Sadaka MS, Allam AA. Congenital Symmastia: A 3-Step Approach. Plast Reconstr Surg Glob Open. 2016;4(12):e1158. Published 2016 Dec 7. doi:10.1097/GOX.0000000000001158 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5222655
- Bland KI, Howard JH, Romrell LJ. Congenital and acquired disturbances of breast development and growth. In: Barsky SH, Gradishar WJ, Recht A, editors. In: The Breast: Comprehensive Management of Benign and Malignant Diseases. 4th ed. Philadelphia: Saunders Elsevier; 2009. pp. 189–207.
- Piza-Katzer H, Engelhardt TO, Steiner HJ, et al. Familial congenital symmastia: ultrastructurally abnormal breast tissue. Scand J Plast Reconstr Surg Hand Surg. 2009;43:339–342.
- Tamaki Y, Sakita I, Miyoshi Y, et al. Transareolar endoscopy-assisted partial mastectomy: a preliminary report of six cases. Surg Laparosc Endosc Percutan Tech 2001; 11:356-62. Comment in: Surg Laparosc Endosc Percutan Tech 2001; 11:363
- Sillesen NH, Hölmich LR, Siersen HE, et al. Congenital symmastia revisited. J Plast Reconstr Aesthet Surg. 2012;65:1607–1613.
- Fallon SC, Hatef DA, McKnight AJ, et al. Congenital synmastia with concurrent fibroadenomas in a pediatric patient. J Pediatr Surg. 2013;48:255–257.
- Salgado CJ, Mardini S. Periareolar approach for the correction of congenital symmastia. Plast Reconstr Surg. 2004;113:992–994.
- Wong MT, Cheong EC, Lim J, et al. Creation of an intermammary sulcus in congenital synmastia. Singapore Med J. 2007;48:e29–e31.