What is telogen effluvium
Telogen effluvium is the name for temporary nonscarring hair loss on all parts of your body, but, generally, only loss of scalp hair is symptomatic due to shedding of resting or telogen hair after some shock to your system such as certain medications, trauma, fever, child-bearing, major surgery, weight loss, emotional and physiological stress 1. New hair continues to grow. Telogen effluvium is one of the most common causes of alopecia or hair loss 2. Telogen hair has a bulb or club-shaped tip. Telogen effluvium can occur in people of any age, any gender, and any racial background 3. Telogen effluvium should be distinguished from anagen effluvium, in which the hair shedding is due to interruption of active or anagen hair growth by drugs, toxins or inflammation (e.g. alopecia areata). Anagen hair has a pointed or tapered tip.
Telogen effluvium is divided into 2 stages depending on the duration of hair loss 2:
- Acute telogen effluvium: Acute telogen effluvium is defined as hair shedding lasting for less than six months. Acute telogen effluvium can affect people of all age groups and both sexes. Generally, hair loss occurs two to three months after the trigger exposure. In around 33% of the cases, the cause remains unknown 4. Acute telogen effluvium usually undergoes remission in around 95% of cases. On examination of those with resolved effluvium, there is an appearance of shorter, re-growing frontal hair. Such hair can be seen in a large quantity using videodermoscopy 1. A variant of acute telogen effluvium is telogen gravidarum, which is associated with pregnancy and usually occurs two to five months after childbirth 4.
- Chronic telogen effluvium: Chronic telogen effluvium is a condition lasting for more than six months. Chronic telogen effluvium with no clear precipitating cause tends to present in otherwise healthy women 30–60 years of age, having a prolonged fluctuating course. The examination of the scalp shows hair having normal thickness with signs of shorter re-growing hair in the frontal and bitemporal areas 1.
The five proposed mechanisms by which shedding of the hair may occur in telogen effluvium are as follows 4:
- Immediate anagen release: This is due to an underlying cause. Follicles leave the anagen phase and enter the telogen phase prematurely, leading to increased shedding two to three months later.
- Delayed anagen release: This is due to prolongation of the anagen phase resulting in heavy telogen shedding.
- Short anagen syndrome: This is due to idiopathic shortening of the anagen phase, leading to persistent telogen effluvium. The pathogenesis behind most of the cases of chronic telogen effluvium is considered to be the short anagen syndrome.
- Immediate telogen release: This is due to the shortening of the telogen phase, resulting in a massive release of club hair.
- Delayed telogen release: This is due to a prolonged telogen phase and a delayed transition to anagen phase 5.
It is normal to shed approximately 30-150 hairs from your scalp daily as part of our hair cycle, but this can vary depending on washing and brushing routines. Hair regrows automatically so that the total number of hairs on your head remains constant. Telogen effluvium occurs when there is a marked increase in hairs shed each day. An increased proportion of hairs shift from the growing phase (anagen) to the shedding phase (telogen). Anagen hair has a pointed or tapered tip. Normally only 10% of your scalp hair is in the telogen phase, but in telogen effluvium this increases to 30% or more. This usually happens suddenly and can occur approximately 3 months after a trigger.
In most people, 5-15% of the hair on the scalp is in telogen at any given time. Telogen effluvium is triggered when a physiologic stress or hormonal change causes a large number of hairs to enter telogen at one time. Shedding does not occur until the new anagen hairs begin to grow. The emerging hairs help to force the resting hairs out of the follicle. Evidence suggests that the mechanism of shedding of a telogen hair is an active process that may occur independent of the emerging anagen hair. The interval between the inciting event in telogen effluvium and the onset of shedding corresponds to the length of the telogen phase, between 1 and 6 months (average 3 months).
Common triggers of telogen effluvium include childbirth, severe trauma or illness, a stressful or major life event (such as losing a loved one), marked weight loss and extreme dieting, a severe skin problem affecting the scalp, a new medication or withdrawal of a hormone treatment. No cause is found in around a third of people diagnosed with telogen effluvium.
Hair shedding in telogen effluvium is usually from all over the scalp. Hair thickness decreases in the early stages resulting in thinness of hair volume.
Telogen effluvium is a form of nonscarring alopecia (hair loss) characterized by diffuse hair shedding, often with an acute onset 6. A chronic telogen effluvium with a more insidious onset and a longer duration also exists 7. Telogen effluvium is a reactive process caused by a metabolic or hormonal stress or by medications. Generally, recovery is spontaneous and occurs within 6 months, unless a background of pattern alopecia is present 8.
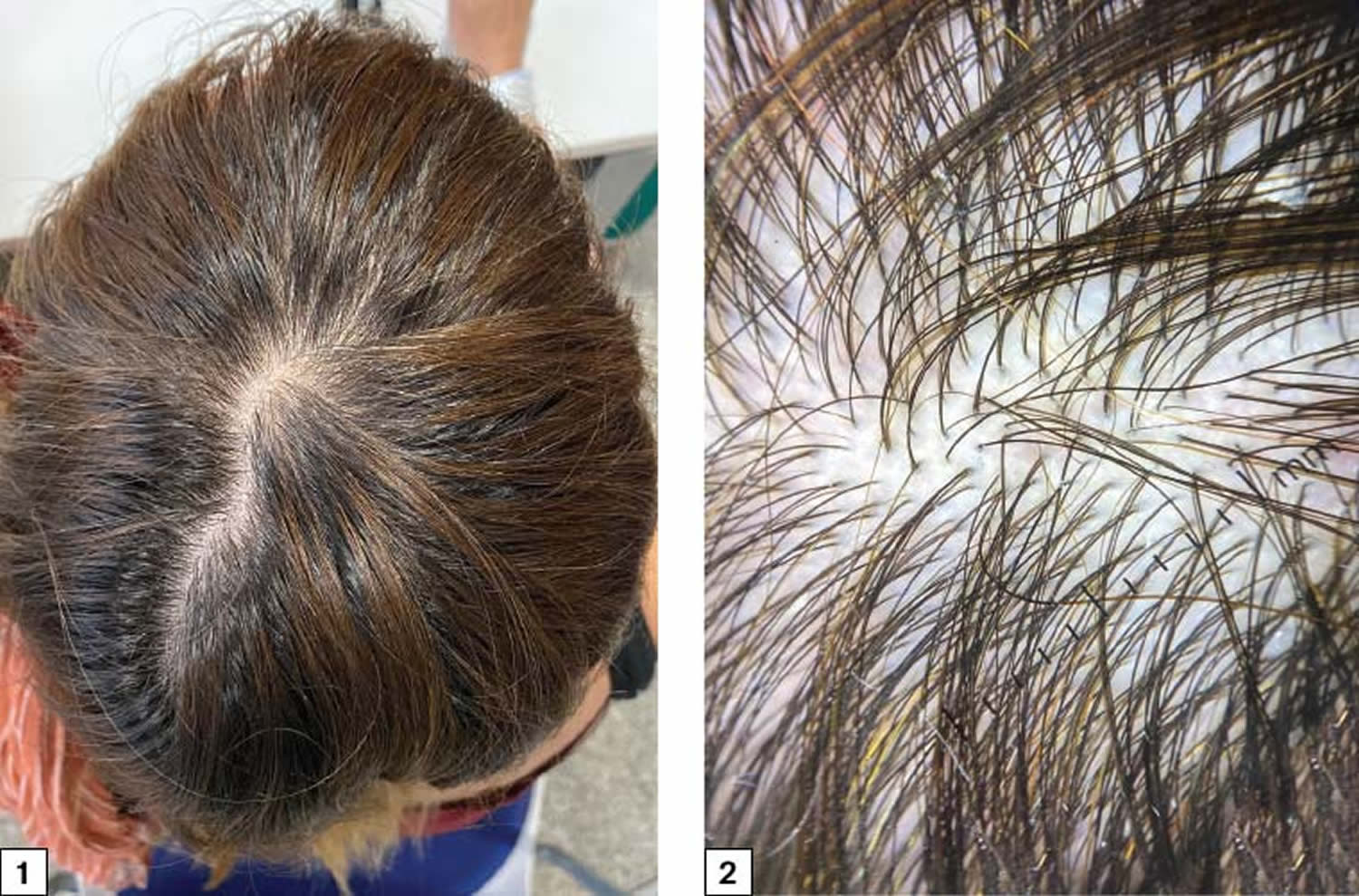
Figure 1. Telogen effluvium
Footnote: 1) Diffuse loss of hair volume without any defined alopecic patches. 2) Numerous follicular units of only one hair and without anisotrichosis (hair shafts with different diameters); no trichoscopic signs of alopecia areata or other kinds of alopecia
Telogen effluvium treatment tips
Telogen effluvium is self-correcting. It is really not influenced by any treatment that can be given. However, gentle handling of the hair, avoiding over-vigorous combing, brushing and any type of scalp massage are important.
You should also ensure a nutritious diet, with plenty of protein, fruit and vegetables.
The doctor may check your thyroid function, and levels of iron, vitamin B12 and folic acid, as any deficiency in these can slow hair growth.
You should also consider stopping smoking as heavy metals in cigarette smoke may worsen your hair loss.
What if the scalp starts to become visible because of thinning of the hair?
This can happen in severe cases of telogen effluvium, but various options for helping disguise the hair loss can be discussed with your doctor. It is very unusual for hair thinning in patients with telogen effluvium to be severe enough to require the use of a wig.
Hair Growth Cycle
Hair follicles extend deep into the dermis, often projecting into the underlying subcutaneous layer. The epithelium at the follicle base surrounds a small hair papilla, a peg of connective tissue containing capillaries and nerves. The hair bulb consists of epithelial cells that surround the papilla.
Hair production involves a specialized keratinization process. The hair matrix is the epithelial layer involved in hair production. When the superficial basal cells divide, they produce daughter cells that are pushed toward the surface as part of the developing hair. Most hairs have an inner medulla and an outer cortex. The medulla contains relatively soft and flexible soft keratin. Matrix cells closer to the edge of the developing hair form the relatively hard cortex. The cortex contains hard keratin, which gives hair its stiffness. A single layer of dead, keratinized cells at the outer surface of the hair overlap and form the cuticle that coats the hair.
The hair root anchors the hair into the skin. The root begins at the hair bulb and extends distally to the point where the internal organization of the hair is complete, about halfway to the skin surface. The hair shaft extends from this halfway point to the skin surface, where we see the exposed hair tip.
The size, shape, and color of the hair shaft are highly variable.
Growth and Replacement of Hair
A hair in the scalp grows for two to five years, at a rate of around 0.33 mm/day (about 1/64 inch). Variations in hair growth rate and the duration of the hair growth cycle account for individual differences in uncut hair length. A given hair goes through a hair cycle consisting of three developmental stages (see Figure 2):
- Anagen (growing phase). The anagen phase constitutes about 90% (1000 days or more) of the growth cycle 9. Anagen hairs are anchored deeply into the subcutaneous fat and cannot be pulled out easily.
- Catagen (involuting phase). The catagen phase is a much shorter phase, lasting three to six weeks. During this phase, the hair follicles go through a process of programmed cell death (apoptosis) 10.
- Telogen (resting phase). The telogen phase lasts for around three to five months, and 10% of the scalp hair are in this phase. During this phase, the hair shaft matures into a club hair, which is eventually shed from the follicle. If the percentage of scalp follicles present in the telogen phase increases, this results in excessive shedding of hair 9.
At any given time, about 90% of the scalp follicles are in the anagen stage. In this stage, stem cells from the bulge in the follicle multiply and travel downward, pushing the dermal papilla deeper into the skin and forming the epithelial root sheath. Root sheath cells directly above the papilla form the hair matrix. Here, sheath cells transform into hair cells, which synthesize keratin and then die as they are pushed upward away from the papilla. The new hair grows up the follicle, often alongside an old club hair left from the previous cycle.
The catagen phase (10 days) and telogen phase (100 days) constitute only 10% of the hair growth cycle. During the catagen and telogen phase of the hair growth cycle, as hairs are at the shedding and rest-from-growth period, no bald spots are shown as hairs are randomly distributed over the scalp.
In the catagen stage, mitosis in the hair matrix ceases and sheath cells below the bulge die. The follicle shrinks and the dermal papilla draws up toward the bulge. The base of the hair keratinizes into a hard club and the hair, now known as a club hair, loses its anchorage. Club hairs are easily pulled out by brushing the hair, and the hard club can be felt at the hair’s end. When the papilla reaches the bulge, the hair goes into a resting period called the telogen stage. Eventually, anagen begins anew and the cycle repeats itself. A club hair may fall out during catagen or telogen, or as it is pushed out by the new hair in the next anagen phase.
You lose about 50 to 100 scalp hairs daily. In a young adult, scalp follicles typically spend 6 to 8 years in anagen, 2 to 3 weeks in catagen, and 1 to 3 months in telogen. Scalp hairs grow at a rate of about 1 mm per 3 days (10–18 cm/yr) in the anagen phase.
Hair grows fastest from adolescence until the 40s. After that, an increasing percentage of follicles are in the catagen and telogen phases rather than the growing anagen phase. Hair follicles also shrink and begin producing wispy vellus hairs instead of thicker terminal hairs. Thinning of the hair, or baldness, is called alopecia. It occurs to some degree in both sexes and may be worsened by disease, poor nutrition, fever, emotional stress, radiation, or chemotherapy. In the great majority of cases, however, it is simply a matter of aging.
Pattern baldness (androgenic alopecia) is the condition in which hair is lost unevenly across the scalp rather than thinning uniformly. It results from a combination of genetic and hormonal influences. The relevant gene has two alleles: one for uniform hair growth and a baldness allele for patchy hair growth. The baldness allele is dominant in males and is expressed only in the presence of the high level of testosterone characteristic of men. In men who are either heterozygous or homozygous for the baldness allele, testosterone causes terminal hair to be replaced by vellus hair, beginning on top of the head and later the sides. In women, the baldness allele is recessive. Homozygous dominant and heterozygous women show normal hair distribution; only homozygous recessive women are at risk of pattern baldness. Even then, they exhibit the trait only if their testosterone levels are abnormally high for a woman (for example, because of a tumor of the adrenal gland, a woman’s principal source of testosterone). Such characteristics in which an allele is dominant in one sex and recessive in the other are called sex-influenced traits.
Excessive or undesirable hairiness in areas that are not usually hairy, especially in women and children, is called hirsutism. It tends to run in families and usually results from either masculinizing ovarian tumors or hypersecretion of testosterone by the adrenal cortex. It is often associated with menopause.
Contrary to popular misconceptions, hair and nails do not continue to grow after a person dies, cutting hair does not make it grow faster or thicker, and emotional stress cannot make the hair turn white overnight.
Figure 2. Hair growth cycle
How long does telogen effluvium last?
Generally, telogen effluvium recovery is spontaneous and occurs within 6 months, unless a background of pattern alopecia is present 8.
Can telogen effluvium be cured?
Telogen effluvium usually resolves completely without any intervention as the normal length of telogen is approximately 100 days (3 to 6 months) after which period the hair starts growing again (anagen phase). However, depending on the length of the hair, it may take many months for the overall hair volume to gradually return to normal. Telogen effluvium can return, especially if the underlying cause is not treated or recurs, and would be called chronic telogen effluvium if lasting more than 6 months.
Chronic telogen effluvium
In some patients, hair shedding continues to be intermittently or continuously greater than normal for long periods of time, sometimes for years. The hair cycle appears to be reset so that the anagen period is shortened.
Chronic telogen effluvium often presents in women that actually continue to have quite thick and moderately long hair – this is because they notice the shed hair more than those with finer or shorter hair. Telogen effluvium does not cause complete baldness, although it may unmask a genetic tendency to genetic balding i.e. female pattern hair loss , or in men, male pattern hair loss.
The mechanism of chronic telogen effluvium is not well understood. Middle-aged women with a long fluctuating course of telogen effluvium, producing widespread thinning lasting many years have normal hormonal studies.
Is telogen effluvium hereditary?
Telogen effluvium is not inherited, and it can affect all age groups and both genders equally.
Telogen effluvium causes
In a normal healthy person’s scalp about 85% of the hair follicles are actively growing hair (anagen hair) and 15% are resting hair (telogen hair). A hair follicle usually grows anagen hair for 4 years or so, then rests for about 4 months. The resting or telogen hair has a club or bulb at the tip. A new anagen hair begins to grow under the resting telogen hair and pushes it out.
Thus, it is normal to lose up to about 100 hairs a day on one’s comb, brush, in the basin or on the pillow, as a result of the normal scalp hair cycle.
If there is some shock to your system, as many as 70% of the anagen hairs can be precipitated into telogen, thus reversing the usual ratio. Typical triggering events include:
- Acute illness (physiological stress) such as febrile illness, severe infection, major surgery, chronic systemic illness, hemorrhage and severe trauma 11
- Chronic illness such as malignancy, particularly lymphoproliferative malignancy; and any chronic debilitating illness, such as systemic lupus erythematosus (SLE), systemic amyloidosis, inflammatory bowel disease, end-stage renal disease (chronic renal failure) or liver disease (liver failure) 11
- Medical conditions. Numerous medical disorders can lead to telogen effluvium. Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can cause telogen effluvium, and this is reversed once the normal thyroid state is achieved 12.
- Some autoimmune diseases including dermatomyositis, chronic infections such as HIV, and secondary syphilis.
- Inflammatory disorders such as psoriasis and seborrheic dermatitis can also lead to diffuse telogen hair loss 13.
- Surgical operation
- Accident
- Hormonal changes such as pregnancy and delivery (can affect both mother and child), hypothyroidism, and discontinuation of estrogen-containing medications 14
- Childbirth
- Nervous shock
- Weight loss or unusual diet. Changes in diet like crash dieting, anorexia, low protein intake, and chronic iron deficiency 15, 16: A study by Olsen et al. 17 sought to determine if iron deficiency played a role in female pattern hair loss. Results indicated that iron deficiency is common in women but is not significantly increased in patients with female patterns of hair loss or chronic telogen effluvium when compared with control subjects.
- Severe protein, fatty acid and zinc deficiency, chronic starvation, and caloric restriction can lead to telogen effluvium 13. Essential fatty acid deficiency leads to telogen effluvium, and this usually occurs two to four months after insufficient intake 13. Vitamin D is vital for cell growth and, hence, its deficiency could also be a possible cause of it. Another cause can be biotin deficiency but is reportedly very rarely 18.
- Heavy metals such as selenium, arsenic, and thallium
- Medications, of which the most frequency cited are beta-blockers, anticoagulants, oral contraceptive pills, androgens, retinoids (including excess vitamin A), propylthiouracil (induces hypothyroidism), anticoagulants (heparin), carbamazepine, ACE (angiotensin-converting enzyme) inhibitors, anticonvulsants, antidepressants, and immunizations 19, 20, 13
- Allergic contact dermatitis of the scalp 21
- Psychological stress 15
- Discontinuing the contraceptive pill
- Overseas travel resulting in jetlag
- Excessive sun exposure. Researchers found an increased frequency of telogen effluvium between July and October. They hypothesized that it could be actinic effluvium, a summer effect, induced by sunlight and ultraviolet (UV) light, manifesting in autumn 22. Electron microscopy of hair exposed to sunlight reveals alterations in the cellular components and damage to the hair cuticle and cortex. Both of these mechanisms can be attributed to increased shedding of hair in the telogen phase; however, it is not scientifically proven yet 1.
The association of telogen effluvium with age is unclear; however, elderly women are known to be more susceptible to acute telogen effluvium following fever, trauma, hemorrhage, or psychological stress 1. Studies have reported the incidence of telogen effluvium in children to be around 2.7% 23.
The resting scalp hairs, now in the form of club hairs, remain firmly attached to the hair follicles at first. It is only about 2 months after the shock that the new hairs coming up through the scalp push out the “dead” club hairs and increased hair fall is noticed.
Thus, paradoxically, with this type of hair loss, hair fall is a sign of hair regrowth. As the new hair first comes up through the scalp and pushes out the dead hair a fine fringe of new hair is often evident along the forehead hairline. At first the fall of club hairs is profuse and a general thinning of the scalp hair may become evident but after several months a peak is reached and hair fall begins to lessen, gradually tapering back to normal over 6-9 months. As the hair fall tapers off the scalp thickens back up to normal, but recovery may be incomplete in some cases.
Because nail and hair growth are under the same influences, an arrest in hair growth is often mirrored in the nails by a groove across them coinciding with the time of the shock to the system. This is called a Beau’s line. The time of the shock can be estimated from the fact that a finger nail takes 5 months to grow from the posterior nail fold to the free edge. So if the groove in the nail is half way down the nail then the shock must have been 2 1/2 months ago.
Telogen effluvium symptoms
Most people become aware of losing hair in increased amounts. This is most noticeable after washing or brushing with more hair being found in the plug hole or on the hair brush or comb. Some people will notice increased hair on the pillow in the morning or around the house. Usually there are no symptoms, but occasionally telogen effluvium can be accompanied by tenderness and altered sensations (pain, burning, itching & stinging) in the scalp known as trichodynia 24.
Acute telogen effluvium is defined as diffuse hair loss with no clinical or histological evidence of inflammation lasting less than 6 months. Patients with acute telogen effluvium usually complain of relatively sudden onset of hair loss and can affect up to 50% of the scalp hair. Careful questioning usually reveals a metabolic or physiologic stress 1-6 months before the start of the hair shedding. Physiologic stresses that can induce telogen effluvium include febrile illness, major injury, change in diet, pregnancy and delivery, and starting a new medication. Immunizations also have been reported to cause acute hair shedding. Papulosquamous diseases of the scalp, such as psoriasis and seborrheic dermatitis, can produce telogen effluvium. Because nail and hair growth are under the same influences, an arrest in hair growth is often mirrored in the nails by a groove across them coinciding with the time of the shock to the system — a Beau line (see Figure 2). The time of the shock can be estimated from the fact that a fingernail takes 5 months to grow from the posterior nail fold to the free edge. So if the groove in the nail is halfway down the nail, the shock must have been two and a half months ago.
Chronic telogen effluvium is hair shedding lasting longer than 6 months. The onset is often insidious, and it can be difficult to identify an inciting event. Because of the duration of the hair shedding, patients are more likely to complain of decreased scalp hair density, or they may note that their hair appears thin and lifeless. Visual analog scales can help patients to assess the severity of hair shedding 25.
Figure 2. Beau line (Beau line is a transverse depression affecting a nail, due to acute systemic illness stopping nail growth)
How is telogen effluvium diagnosed?
The diagnosis is usually based on appearance and the history of the hair shedding.
Telogen effluvium is usually diagnosed by its clinical features:
- Hair thinning involves the entire scalp +/- loss of other body hair.
- Examination shows diffuse thinning without focal areas of total alopecia and short hairs of normal thickness.
- A gentle hair pull test reveals an increased number of hairs; most are telogen with a typical epithelial sac.
- A trichogram can help confirm the diagnosis (see below)
The hair may be gently pulled to see if an increased quantity of hair is shed (although this test may be falsely negative if the hair has been washed within 48 hours beforehand) and occasionally hairs are plucked from the scalp so that they can be examined under the microscope. Very rarely a skin biopsy may be required.
If a biopsy is performed, some authors advocate taking three 4-mm punch biopsy specimens, all imbedded horizontally. This method provides a generous sample for determining anagen-to-telogen and terminal-to-vellus ratios and leads to greater diagnostic accuracy 26.
Chronic telogen effluvium may have a metabolic cause. Testing should be directed toward causes that are common and correctable. If any sign or symptom of hypothyroidism is present, a thyrotropin test is warranted. Iron deficiency is common in premenopausal women. Evaluation of complete blood count (CBC) count, serum iron, iron saturation, and ferritin may be warranted. Note that CBC count results may be completely normal in women with mild iron deficiency and hair loss, particularly in women older than 40 years. Blood is more essential than hair, and the body will shed hair before red cell indices become microcytic. Also, note that ferritin behaves as an acute phase reactant. Inflammation can produce normal ferritin levels in an individual who is iron deficient. Although a low ferritin is proof of iron deficiency, a normal ferritin level does not exclude iron deficiency. Some experts in the field regard iron saturation as the most sensitive indicator of iron deficiency.
Occasionally, screening for renal and hepatic enzymes may detect a systemic cause of hair shedding. If syphilis is considered as a cause of hair loss, a rapid plasma reagin or Venereal Disease Research Laboratory (VDRL) test should be preformed.
Other tests
If a patient is unwilling to undergo a scalp biopsy but would like confirmation of the diagnosis, serial hair collections may be obtained. This process can educate the patient in the normal hair cycle and can confirm the spontaneous resolution of the process.
The patient should be instructed to collect all hairs shed in a 24-hour period. The patient should not shampoo the hair during the day of collection. This process should be repeated every week or every other week, for a total of 3 or 4 collections.
Collections totaling 100 hairs or more in a given 24-hour period are indicative of ongoing telogen effluvium. If the collections are performed over several weeks while the telogen effluvium is resolving, the number of hairs collected each time should decrease. This finding can be very comforting to the patient.
An alternate method of hair collection has been proposed by Rebora et al. 27. According to this method, the patient collects hair during shampooing and the physician both counts and measures the length of these hairs. This method has the advantage of being able to detect and differentiate between telogen effluvium and androgenetic alopecia, even when the 2 conditions occur in the same individual. The disadvantage to this method is that it cannot be used in patients who have short hair (< 3 cm). Additionally, the counting and measuring procedure is very labor intensive, which limits its practicality in normal clinical practice.
Ross et al. 28 report on the successful use of videodermoscopy in the diagnosis of hair and scalp disorders. The color-transition sign has been used to differentiate alopecia areata from telogen effluvium 29.
Modified wash test and hair loss count
The modified wash test is an office procedure that permits to identify patients with telogen effluvium or androgenetic alopecia, and the severity of diseases. It is performed after five days of abstention from shampooing. The patients are asked to wash and rinse their hair in a sink covered by gauze, collect the hair, let them dry, and put them in an envelope. Afterward, the collected hair are counted along with the percentage of vellus hair 30. The results and possible diagnosis are as follows:
- Telogen effluvium: More than 100 shed hair, less than 10% vellus.
- Androgenetic alopecia: Less than 100 shed hair, more than 10% vellus.
- Association of telogen effluvium and androgenetic alopecia: More than 100 shed hair, more than 10% vellus.
- Normal or remitting telogen effluvium: Less than 100 shed hair, less than 10% vellus.
Trichogram
Trichogram is a plucking of hair in a defined area (40-60 hair). Cases of telogen effluvium show a significant reduction of the anagen:telogen ratio. More than 25% of hair are found to be in the telogen phase in the case of telogen effluvium 31.
Phototrichogram and TrichoScan
This technique involves trimming the hair of a 2 sq. cm area of scalp, pictures of the same area taken on different days, and then compared in hair density, hair growth, and rate of shedding. Since only anagen hair would elongate it helps in the assessment of the ratio of anagen:telogen hair. A TrichoScan is a fully computerized phototrichogram 32. A TrichoScan is a simpler, noninvasive, reproducible, and more sensitive than a classical trichogram and very useful in the diagnosis of hair loss 32.
Videodermoscopy
In the case of acute telogen effluvium, videodermoscopy will show numerous short re-growing hair with no variability of density 33.
Scalp biopsy
Scalp biopsy is recommended in cases where telogen loss lasts greater than six months. Performing multiple biopsies increases the diagnostic accuracy of telogen effluvium 34. In the case of acute telogen effluvium, there is a normal to supernormal anagen:telogen ratio 35. Follicular miniaturization and peribulbar infiltrate are not found. In chronic telogen effluvium, there are increased telogen hair, with an anagen:telogen ratio of 8:1 compared with 14:1 on normal scalp biopsies 33.
Telogen effluvium treatments
There is normally no treatment required for acute telogen effluvium as the hair will start growing back once the trigger is removed. Often, the knowledge that the hair loss will not progress to baldness is comforting to the patient. The patient should be encouraged to style the hair in a way that masks any perceived defects in hair density. Medication does not speed up this process, however, drugs suspected to cause telogen effluvium should be replaced or discontinued 36. Catagen-inducing drugs (e.g., beta-blockers, retinoids, anticoagulants, antithyroid drugs) should be avoided 1.
Your doctor may check your thyroid function for over- or underactive thyroid and levels of iron, vitamin B12 and folic acid, as any deficiency in these can slow hair growth.
Causative conditions such as scalp conditions (e.g., psoriasis, seborrheic dermatitis) should be treated 37.
While topical minoxidil is not proven to promote recovery of hair in telogen effluvium, this medication has a theoretical benefit and is well tolerated. Patients who are eager to play an active role in their treatment may choose to use minoxidil.
Topical corticosteroids are often employed by dermatologists in telogen effluvium treatment. If the patient reports decreasing trichodynia after the application of topical corticosteroids, it is a sign of the therapy being effective 38.
Chronic telogen effluvium is a primary idiopathic (unknown cause) and often self-limiting condition affecting middle-aged women. While chronic telogen effluvium is less likely to resolve rapidly, reassurance is appropriate for these patients.
In chronic telogen effluvium due to underlying systemic disorder like systemic lupus erythematosus (SLE), systemic corticosteroids can be given 39.
Recently, Davis et al. 40 reported a novel treatment named CNPDA (a combination of caffeine, niacinamide, panthenol, dimethicone, and an acrylate polymer) for thinning of hair. This new combination treatment leads to an increased cross-sectional area of individual terminal scalp hair by 10%.
Telogen effluvium diet
You should also ensure a nutritious diet, with plenty of protein, fruit and vegetables. Although the use of polyphenolic compounds such as those in green tea has been reported to improve hair loss in mice, no such controlled studies are available for humans 41.
Telogen effluvium prognosis
Telogen effluvium is a benign and spontaneously reversible condition. Regrowth usually occurs after removal of the trigger causing telogen effluvium. However, repeated episodes of acute telogen effluvium can sometimes evolve into female pattern hair loss. A good cosmetic outcome is also expected in chronic telogen effluvium, even if the hair shedding continues.
References- Grover C, Khurana A. Telogen effluvium. Indian J Dermatol Venereol Leprol. 2013 Sep-Oct;79(5):591-603. doi: 10.4103/0378-6323.116731
- Asghar, F., Shamim, N., Farooque, U., Sheikh, H., & Aqeel, R. (2020). Telogen Effluvium: A Review of the Literature. Cureus, 12(5), e8320. https://doi.org/10.7759/cureus.8320
- Hughes EC, Saleh D. Telogen Effluvium. [Updated 2021 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430848
- Headington JT. Telogen effluvium. New concepts and review. Arch Dermatol. 1993 Mar;129(3):356-63. doi: 10.1001/archderm.129.3.356
- Gilmore S, Sinclair R. Chronic telogen effluvium is due to a reduction in the variance of anagen duration. Australas J Dermatol. 2010 Aug;51(3):163-7. doi: 10.1111/j.1440-0960.2010.00654.x
- Poonia K, Thami GP, Bhalla M, Jaiswal S, Sandhu J. NonScarring Diffuse Hair Loss in Women: a Clinico-Etiological Study from tertiary care center in North-West India. J Cosmet Dermatol. 2018 May 17.
- Sinclair R. Chronic telogen effluvium: a study of 5 patients over 7 years. J Am Acad Dermatol. 2005 Feb. 52(2 Suppl 1):12-6.
- Perez-Mora N, Goren A, Velasco C, Bermudez F. Acute telogen effluvium onset event is associated with the presence of female androgenetic alopecia: potential therapeutic implications. Dermatol Ther. 2014 May-Jun. 27(3):159-62.
- Shapiro, J., Wiseman, M., & Lui, H. (2000). Practical management of hair loss. Canadian family physician Medecin de famille canadien, 46, 1469–1477. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2144852/pdf/canfamphys00029-0071.pdf
- Lindner, G., Botchkarev, V. A., Botchkareva, N. V., Ling, G., van der Veen, C., & Paus, R. (1997). Analysis of apoptosis during hair follicle regression (catagen). The American journal of pathology, 151(6), 1601–1617. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1858357/pdf/amjpathol00024-0099.pdf
- KLIGMAN AM. Pathologic dynamics of human hair loss. I. Telogen effuvium. Arch Dermatol. 1961 Feb;83:175-98. doi: 10.1001/archderm.1961.01580080005001
- Sperling LC. Hair and systemic disease. Dermatol Clin. 2001 Oct;19(4):711-26, ix. doi: 10.1016/s0733-8635(05)70310-7
- Harrison S, Bergfeld W. Diffuse hair loss: its triggers and management. Cleve Clin J Med. 2009 Jun;76(6):361-7. doi: 10.3949/ccjm.76a.08080
- Freinkel RK, Freinkel N. Hair growth and alopecia in hypothyroidism. Arch Dermatol. 1972 Sep. 106(3):349-52.
- Malkud S. A Hospital-based Study to Determine Causes of Diffuse Hair Loss in Women. J Clin Diagn Res. 2015 Aug. 9 (8):WC01-4.
- Moeinvaziri M, Mansoori P, Holakooee K, Safaee Naraghi Z, Abbasi A. Iron status in diffuse telogen hair loss among women. Acta Dermatovenerol Croat. 2009;17(4):279-84.
- Olsen EA, Reed KB, Cacchio PB, Caudill L. Iron deficiency in female pattern hair loss, chronic telogen effluvium, and control groups. J Am Acad Dermatol. 2010 Dec. 63(6):991-9.
- SULZBERGER MB, WITTEN VH, KOPF AW. Diffuse alopecia in women. Its unexplained apparent increase in incidence. Arch Dermatol. 1960 Apr;81:556-60. doi: 10.1001/archderm.1960.03730040060011
- Katz KA, Cotsarelis G, Gupta R, Seykora JT. Telogen effluvium associated with the dopamine agonist pramipexole in a 55-year-old woman with Parkinson’s disease. J Am Acad Dermatol. 2006 Nov. 55(5 Suppl):S103-4.
- Tosti A, Pazzaglia M. Drug reactions affecting hair: diagnosis. Dermatol Clin. 2007 Apr;25(2):223-31, vii. doi: 10.1016/j.det.2007.01.005
- Tosti A, Piraccini BM, van Neste DJ. Telogen effluvium after allergic contact dermatitis of the scalp. Arch Dermatol. 2001 Feb. 137(2):187-90.
- Piérard-Franchimont C, Peérard GE. L’effluvium télogène actinique: une facette de la chronobiologie humaine. Int J Cosmet Sci. 1999 Feb;21(1):15-21. doi: 10.1046/j.1467-2494.1999.181620.x
- Nnoruka EN, Obiagboso I, Maduechesi C. Hair loss in children in South-East Nigeria: common and uncommon cases. Int J Dermatol. 2007 Oct;46 Suppl 1:18-22. doi: 10.1111/j.1365-4632.2007.03457.x
- Grimalt R, Ferrando J, Grimalt F. Trichodynia. Dermatology. 1998;196(3):374.
- Martínez-Velasco MA, Vázquez-Herrera NE, Maddy AJ, Asz-Sigall D, Tosti A. The Hair Shedding Visual Scale: A Quick Tool to Assess Hair Loss in Women. Dermatol Ther (Heidelb). 2017 Mar. 7 (1):155-165.
- Sinclair R, Jolley D, Mallari R, Magee J. The reliability of horizontally sectioned scalp biopsies in the diagnosis of chronic diffuse telogen hair loss in women. J Am Acad Dermatol. 2004 Aug. 51(2):189-99.
- Rebora A, Guarrera M, Baldari M, Vecchio F. Distinguishing androgenetic alopecia from chronic telogen effluvium when associated in the same patient: a simple noninvasive method. Arch Dermatol. 2005 Oct. 141(10):1243-5.
- Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol. 2006 Nov. 55(5):799-806.
- Kinoshita-Ise M, Fukuyama M, Ohyama M. Color-transition sign: A useful trichoscopic finding for differentiating alopecia areata incognita from telogen effluvium. J Dermatol. 2018 Mar 6.
- Guarrera M, Fiorucci MC, Rebora A. Methods of hair loss evaluation: a comparison of TrichoScan(®) with the modified wash test. Exp Dermatol. 2013 Jul;22(7):482-4. doi: 10.1111/exd.12164
- The hair pull test and the hair pluck for analysis of hair abnormalities. Chong A, Wade M, Sinclair R. Modern Med Australia. 1999;42:105–110.
- Dhurat R. Phototrichogram. Indian J Dermatol Venereol Leprol. 2006 May-Jun;72(3):242-4. doi: 10.4103/0378-6323.25795
- Hoffmann R. TrichoScan: combining epiluminescence microscopy with digital image analysis for the measurement of hair growth in vivo. Eur J Dermatol. 2001 Jul-Aug;11(4):362-8.
- Sinclair R, Jolley D, Mallari R, Magee J. The reliability of horizontally sectioned scalp biopsies in the diagnosis of chronic diffuse telogen hair loss in women. J Am Acad Dermatol. 2004 Aug;51(2):189-99. doi: 10.1016/s0190-9622(03)00045-8
- Eudy G, Solomon AR. The histopathology of noncicatricial alopecia. Semin Cutan Med Surg. 2006 Mar;25(1):35-40. doi: 10.1016/j.sder.2006.01.005
- Harrison S, Sinclair R. Telogen effluvium. Clin Exp Dermatol. 2002 Jul;27(5):389-5. doi: 10.1046/j.1365-2230.2002.01080.x
- Bergfeld WF, Mulinari-Brenner F. Shedding: how to manage a common cause of hair loss. Cleve Clin J Med. 2001 Mar;68(3):256-61. doi: 10.3949/ccjm.68.3.256
- Rebora A. Trichodynia: a review of the literature. Int J Dermatol. 2016 Apr;55(4):382-4. doi: 10.1111/ijd.13204
- Rebora A. Telogen effluvium. Dermatology. 1997;195(3):209-12. doi: 10.1159/000245944
- Davis, M., Thomas, J., van de Velde, S., Boissy, Y., Dawson, T., Jr, Iveson, R. and Sutton, K. (2011), A novel cosmetic approach to treat thinning hair. British Journal of Dermatology, 165: 24-30. https://doi.org/10.1111/j.1365-2133.2011.10633.x
- Esfandiari, A., & Kelly, A. P. (2005). The effects of tea polyphenolic compounds on hair loss among rodents. Journal of the National Medical Association, 97(8), 1165–1169. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2576011/pdf/jnma00189-0119.pdf