What is Theophylline
Theophylline is a xanthine derivative bronchodilator that works by relaxing smooth muscles in your lungs making it easier for you to breathe by making your lungs less sensitive to allergens and other causes of bronchospasm. Theophylline is used to prevent and treat symptoms such as wheezing, shortness of breath, and chest tightness caused by asthma, chronic bronchitis, emphysema or chronic obstructive pulmonary disease (COPD) and other lung diseases.
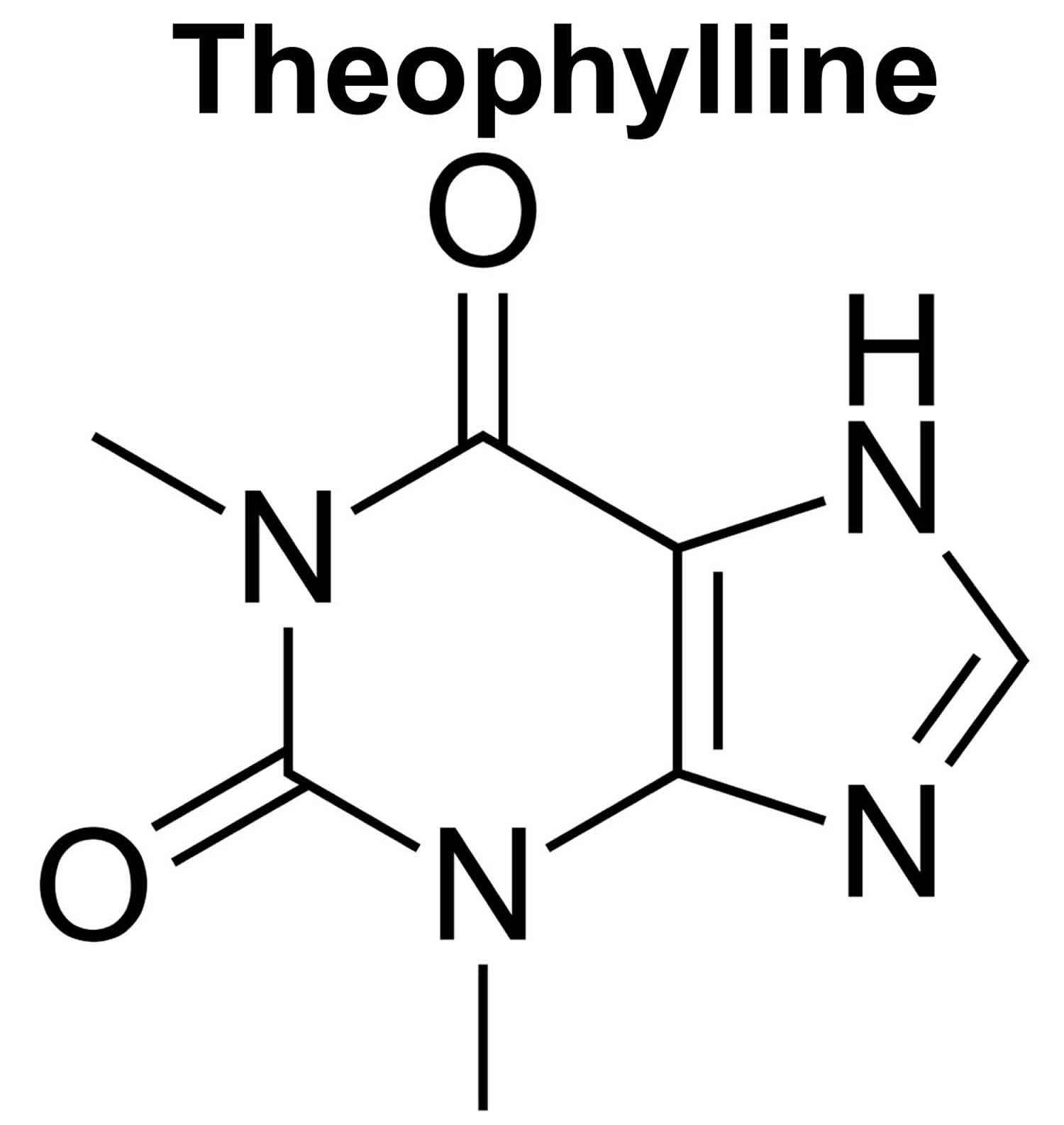
Theophylline is a drug derived from methylxanthine (a purine derivative) and has smooth muscle relaxant, bronchial dilation, diuretic, cardiac and central nervous system (CNS) stimulant activities 1. Naturally present in tea and cocoa beans in small amounts, it was initially extracted and synthesized in 1895, and used as a diuretic. Theophylline was approved for use in the United States in 1982 and is available in multiple generic forms for oral and intravenous use.
Theophylline comes as a tablet, capsule, solution, and syrup to take by mouth. Typical capsule or tablet sizes are 100, 200 and 300 mg. Typical dose regimens are 100 to 300 mg three to four times daily. Theophylline usually is taken every 6, 8, 12, or 24 hours. Syrups are available for use in children. Extended release formulations are also available in sizes of 100 to 600 mg which are typically given twice daily. Dosage is highly individualized. Intravenous formations are available for management of acute asthmatic attacks. Theophylline is marketed under multiple brand names including Asmalix, Elixophyllin, Quibron-T, Respbid, Theobid, Duracaps, and Uniphyl. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take theophylline exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Take this medication with a full glass of water on an empty stomach, at least 1 hour before or 2 hours after a meal. Do not chew or crush the extended-release (long-acting) tablets; swallow them whole. Extended-release capsules (e.g., Theo-Dur Sprinkles) may be swallowed whole or opened and the contents mixed with soft food and swallowed without chewing.
Theophylline controls symptoms of asthma and other lung diseases but does not cure them. Continue to take theophylline even if you feel well. Do not stop taking theophylline without talking to your doctor.
Common side effects of theophylline include dizziness, headache, insomnia, restlessness, tachycardia, palpitations, flushing, nausea, abdominal discomfort and diaphoresis, largely due to the effects of theophylline on the CNS, heart and muscle tissue.
Theophylline mechanism of action
Theophylline is a xanthine derivative that induces relaxation of smooth muscles in the bronchial tree causing bronchodilation. Theophylline also reduces the airway responsiveness to histamine, adenosine, methacholine, and allergens. Theophylline exerts these effects mainly through two distinct mechanisms 1:
- Theophylline acts as a competitive nonselective phosphodiesterase inhibitor (inhibiting type III and type IV phosphodiesterase), which increases the level of intracellular cAMP, activates protein kinase A, inhibits TNF-alpha and leukotriene synthesis, and also decreases inflammation and innate immunity.
- Theophylline is also a nonselective adenosine receptor antagonist. It acts on A1, A2, and A3 receptors with almost the same affinity and this possibly explains the cardiac effects of theophylline. Adenosine-mediated channels also increase the contraction force of diaphragmatic muscles through enhancing their calcium uptake 2.
Other proposed mechanisms of action of theophylline include 1:
- It inhibits nuclear factor-kappaB. This prevents the translocation of the pro-inflammatory transcription factor (nuclear factor-kappaB) to the nucleus, reducing the expression of known inflammatory genes in COPD and asthma).
- Increases interleukin-10 secretion; interleukin-10 has broad anti-inflammatory effects.
- Increases histone deacetylase 2 through inhibiting phosphoinositide 3-kinase-delta.
- Decreases Poly(ADP-ribose)polymerase-1 (PARP-1).
- Increases apoptosis of inflammatory cells (T cells, neutrophils)
Theophylline special precautions
Before taking theophylline:
- tell your doctor and pharmacist if you are allergic to theophylline or any other drugs.
- tell your doctor and pharmacist what prescription medications you are taking, especially allopurinol (Zyloprim), azithromycin (Zithromax), carbamazepine (Tegretol), cimetidine (Tagamet), ciprofloxacin (Cipro), clarithromycin (Biaxin), diuretics (‘water pills’), erythromycin, lithium (Eskalith, Lithobid), oral contraceptives, phenytoin (Dilantin), prednisone (Deltasone), propranolol (Inderal), rifampin (Rifadin), tetracycline (Sumycin), and other medications for infections or heart disease.
tell your doctor and pharmacist what nonprescription medications and vitamins you are taking, including ephedrine, epinephrine, phenylephrine, - phenylpropanolamine, or pseudoephedrine. Many nonprescription products contain these drugs (e.g., diet pills and medications for colds and asthma), so check labels carefully. Do not take these medications without talking to your doctor; they can increase the side effects of theophylline.
- tell your doctor if you have or have ever had seizures, ulcers, heart disease, an overactive or underactive thyroid gland, high blood pressure, or liver disease or if you have a history of alcohol abuse.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking theophylline, call your doctor.
- tell your doctor if you use tobacco products. Cigarette smoking may decrease the effectiveness of theophylline.
Precautions
- Patients with cardiovascular disease: Use cautiously in patients who have cardiac arrhythmias (excluding bradyarrhythmias); at it may exacerbate arrhythmias.
- Patients with cystic fibrosis: Use cautiously in patients with cystic fibrosis, as increased theophylline clearance may occur in these patients.
- Patients with hepatic impairment: Use cautiously in patients with hepatic impairment such as cirrhosis, cholestasis, acute hepatitis because there is an increased risk of severe and potentially fatal complications. This is because clearance decreases by 50% or more in these patients. Frequent monitoring and dose reduction of theophylline are required in these patients.
- Patients with hyperthyroidism: Use cautiously in patients with hyperthyroidism, as increased theophylline clearance may occur.
- Patients with peptic ulcer disease: Use cautiously in patients who have active peptic ulcer disease, as the use of theophylline may exacerbate peptic ulcer.
- Patients with seizure disorders: Use cautiously in patients who have seizure disorders, as use may exacerbate the seizure disorder.
Special Populations
- Elderly patients: Use with extreme caution in elderly patients as these patients are at an increased risk of serious theophylline toxicity.
- Pediatric patients: The dose must be selected with caution, and regular monitoring of concentrations should be performed (especially if the child is younger than 1 year of age) as the rate of clearance varies greatly in these patients.
Special dietary instructions
Drinking or eating foods high in caffeine, like coffee, tea, cocoa, and chocolate, may increase the side effects caused by theophylline. Avoid large amounts of these substances while you are taking theophylline.
Theophylline in Pregnancy
Theophylline is classified as a pregnancy category C drug. Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. Theophylline should only be used during pregnancy if the potential benefit to the mother outweighs the potential risk to the fetus 3.
Theophylline in Breastfeeding
The manufacturer makes no recommendation regarding use during lactation.
Excreted into human milk: Yes
Comments:
- Theophylline may cause irritability or other mild toxicities in nursing infants.
- The breastmilk theophylline concentration is about equal to the mother’s serum concentration.
- Serious adverse effects are unlikely unless maternal serum concentrations are toxic.
Theophylline contraindications
- Theophylline is contraindicated if the patient previously developed a hypersensitivity reaction to the drug or any component of its formulation (such as allergy to corn-related products (in injection use only).
- Other contraindications include hypersensitivity to xanthine derivatives and patients with coronary artery disease (where the cardiac stimulation effect of theophylline might prove harmful).
Theophylline uses
Theophylline is used to prevent and treat symptoms such as wheezing, shortness of breath, and chest tightness caused by asthma, chronic bronchitis, emphysema or chronic obstructive pulmonary disease (COPD) and other lung diseases. Theophylline is sometimes used to treat breathing problems in premature infants.
Theophylline has a very narrow therapeutic window, and its interaction with various other drugs has led to the limitation of its use. The serum theophylline levels must be monitored directly to avoid toxicity as the adverse effects of theophylline are related to its plasma concentration and have been observed when plasma levels exceed 20 mg/L. Some patients have also experienced adverse effects at low plasma concentrations. The dose is gradually increased until therapeutic plasma concentrations are achieved to reduce side effects.
Medical Uses
- Chronic obstructive pulmonary disease
- Asthma
- Infant Apnea
- Anosmia which is currently under investigation. A clinical study in 2008 reported that theophylline could potentially improve the sense of smell in those with anosmia.
Asthma Exacerbations
Treatment of asthma exacerbation with theophylline is not recommended by the current clinical practice guidelines (2018 GINA Report, Global Strategy for Asthma Management and Prevention; National asthma education and prevention program-NAEPP 2007) 1.
COPD Management
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) in 2018, the management of acute chronic obstructive pulmonary disease (COPD) with IV theophylline is not recommended by the current clinical practice guidelines due to its significant side effects 4.
Theophylline administration
Theophylline can be used as an oral agent (rapid or slow-release tablets, solution, syrup, or capsule) or in a more soluble form such as aminophylline (an ethylenediamine salt) that can be used orally or intravenously. Cautiously administer theophylline in a patient who has consumed large amounts of foods or drinks with high caffeine content as this could potentially increase the risk of side effects of theophylline.
Theophylline monitoring
Because of the small therapeutic window of theophylline and its many side effects, physicians should monitor the following in the patient:
- The heart rate of the patient
- CNS effects (headache, insomnia, irritability)
- The respiratory rate
- Patient’s arterial or capillary blood gases
- Patient’s electrolyte concentrations, fluid balance, and acid-base balance should be monitored during prolonged IV therapy.
Serum theophylline levels should be checked after the initiation of therapy, prior to increasing dose and if any signs or symptoms of toxicity are observed. Worsening of the current illness, an occurrence of a new illness, or any change in the patient’s treatment protocol that may alter theophylline clearance should also prompt the physician to check serum levels of theophylline. Attention should also be paid to the infusion site.
Oral Theophylline
For patients taking oral treatment, serum concentrations are monitored at 6-month intervals for rapidly developing children and at annual intervals for all others patients (if their symptoms are well controlled).
IV Theophylline
Loading dose: The serum concentration of theophylline should be checked 30 minutes after the completion of an intravenous loading dose in patients with no theophylline use in the last 24 hours to determine if additional loading may be required (if the serum concentration is less than 10 mcg/mL) or to delay initiating the constant IV infusion (if the serum concentration is greater than 20 mcg/mL).
Infusion: Serum concentration of theophylline should be measured to one expected half-life (approximately 4 hours in young children [ages 1 to 9 years], or around 8 hours in otherwise healthy adults, who do not smoke) after administering a continuous infusion, then checked every 12 to 24 hours to establish if any further adjustments are required, and then at 24 hour intervals for the remainder of the infusion.
Theophylline intravenous
Patients can be administered intravenous (IV) theophylline for acute bronchospasm. Those who are not currently taking theophylline should be given a loading dose of 5 to 7 mg/kg intravenously followed by a maintenance dose of 0.4 to 0.6 mg/kg per hour intravenously to maintain serum levels at 10 to 15 mg/L.
IV aminophylline had frequently been used in the management of acute exacerbations of COPD and asthma but is used much less frequently now as it is far less effective than nebulized beta2-agonists. The currently recommended loading dose is 6 to 7 mg/kg administered intravenously over 20 to 30 minutes. After this, a maintenance dose of 0.5 mg/kg per hour is administered. In patients already taking theophylline, or those who have any factors that decrease its clearance from the body, doses should be halved, and its plasma level checked more frequently. In patients with cardiac decompensation, cor pulmonale, older patients or those on medications that are known to decrease theophylline clearance, the infusion rate of theophylline should not be increased above 17 mg per hour unless the patient remains symptomatic, their steady-state serum concentrations are consistently below 10 mcg/mL, and their serum concentrations can be observed at 24-hour intervals. Administering solutions comprising dextrose concurrently through the same administration route as blood may result in hemolysis or pseudoagglutination, and should be avoided.
Theophylline oral
Theophylline tablets are rapidly absorbed, but plasma concentrations show wide fluctuations and are therefore not currently recommended. Several sustained-release preparations that are absorbed in a relatively constant rate provide steady plasma concentrations of the drug over a 12 to 24-hour period. It should be taken consistently with or without food (as this helps to maintain a more consistent serum drug level).
- The 12-hour formulation: This could be taken once every 24-hours in patients who are non-smokers (who have appropriate total body clearance of theophylline) and in patients who have low dosage requirements. Only after theophylline has titrated to therapeutic levels in the patient, can the 12-hour formulation be considered. The once-daily dosing should be based on the twice-daily dosing and initiated at the end of the every 12-hour dosing interval. Do not give the once-daily dosing to the patient at night (after the evening meal).
- The 24-hour formulation: Take each morning around the same time and avoid taking it at night (after the evening meal). In patients whom a higher dose is required (13 mg/kg or greater than or equal to 900 mg, whichever one is less), should take the medication less than 60 minutes before a high-fat meal (as a significant increase in the peak serum level and absorption could occur). Patients should consistently take theophylline either in a fasting state or with food (as this helps to maintain a more consistent serum drug level). The twice-daily dosing could be considered for those who metabolize theophylline quickly (for example, smokers, younger patients, and some nonsmoking adults) and those who still have symptoms at the end of the dosing interval. The first dose should be administered in the morning and the second one around 10 to 12 hours after the first dose (but before eating the evening meal). Administration at night should be avoided.
Other Routes
Administering by inhalation is both irritating and ineffective. Administration of theophylline through intramuscular injections is very painful and should never be given.
Dosing Considerations
- If aminophylline is being administered, the dose should be increased by 25% (as aminophylline is 79% to 86% theophylline).
- The ideal body weight should be used to calculate the dose.
- Aminophylline or immediate-release theophylline should be used for per-oral loading 5.
Theophylline therapeutic level
Therapeutic Levels for theophylline 1:
- For children: 5 to 15 mcg/mL
- For adults: 10 to 20 mcg/mL
- Toxic serum concentration: greater than 20 mcg/mL 6.
Toxic doses of theophylline can be as low as 7.5 mg/kg 7. When taken orally, 80% to 100% of theophylline is absorbed in the gastrointestinal tract. Peak serum levels can occur from 30 to 120 minutes for immediate release formulations. Sustained release formulations have peak levels between 6 and 10 hours. Intravenously, theophylline takes 30 minutes to reach peak levels. Therapeutic serum levels range from 10 to 20 mcg/mL. Toxic levels are considered to be 20 mcg/mL or higher. However, toxic effects can be seen within therapeutic levels as well. Cardiac dysrhythmias, seizures, and death can be seen with levels of 80 to 100 mcg/mL. Chronic toxicity can be seen at levels of 40 to 60 mcg/mL. Fifty percent to 65% of theophylline is protein-bound in the circulation. Volume distribution is small, at 0.45 L/kg. The half-life varies with age. A half-life of 4 to 8 hours is seen in young adults. A shorter half-life is seen in newborns. Theophylline is metabolized in the liver by the cytochrome P450 system and excreted by the kidneys. Therefore, any agents or pathology that alters the cytochrome P450 system or renal function can have a substantial effect on theophylline levels 8.
Theophylline dosage
The dose of theophylline will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of theophylline. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of theophylline that you take depends on the strength of the theophylline. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take theophylline depend on the medical problem for which you are using theophylline.
To treat symptoms of asthma, bronchitis, and emphysema (COPD):
For oral dosage form (elixir or tablets):
- Adults, teenagers, and children above 1 year of age weighing more than 45 kilograms (kg)—At first, 300 milligrams (mg) per day, divided and given every 6 to 8 hours. Your doctor may adjust your dose as needed. However, the total dose is usually not more than 600 mg per day.
- Older adults—The dose must be determined by your doctor. However, the total dose is usually not more than 400 milligrams per day, divided and given every 6 to 8 hours.
- Children and teenagers 1 to 15 years of age weighing less than 45 kilograms (kg)—Dose is based on body weight and must be determined by your doctor. At first, the dose is 12 to 14 milligrams (mg) per kg of body weight per day, divided and given every 4 to 6 hours. Your doctor may adjust your dose as needed. However, the total dose is usually not more than 20 mg per kg of body weight per day or 600 mg per day.
- Infants younger than 1 year of age—Dose is based on body weight and age and must be determined by your doctor.
For oral dosage form (extended-release capsules):
- Adults, teenagers, and children 12 years of age and older weighing more than 45 kilograms (kg)—At first, 300 to 400 milligrams (mg) as a single dose, usually in the morning, or divided and given two times per day. Your doctor may adjust your dose as needed. However, the total dose is usually not more than 600 mg per day.
- Older adults—The dose must be determined by your doctor. However, the total dose is usually not more than 400 milligrams per day as a single dose, usually in the morning, or divided and given two times per day.
- Children and teenagers 12 to 15 years of age weighing less than 45 kilograms (kg)—Dose is based on body weight and must be determined by your doctor. At first, the dose is 12 to 14 milligrams (mg) per kg of body weight per day as a single dose, usually in the morning, or divided and given two times per day. Your doctor may adjust your dose as needed. However, the total dose is usually not more than 20 mg per kg of body weight per day or 600 mg per day.
- Children younger than 12 years of age—Use and dose must be determined by your doctor.
For oral dosage form (extended-release tablets):
- Adults, teenagers, and children 6 years of age and older weighing more than 45 kilograms (kg)—At first, 300 milligrams (mg) per day, divided and given every 12 hours. Your doctor may adjust your dose as needed. However, the total dose is usually not more than 600 mg per day.
- Older adults—The dose must be determined by your doctor. However, the total dose is usually not more than 400 milligrams per day, divided and given every 12 hours.
- Children and teenagers 6 to 15 years of age weighing less than 45 kilograms (kg)—Dose is based on body weight and must be determined by your doctor. At first, the dose is 12 to 14 milligrams (mg) per kg of body weight per day, divided and given every 12 hours. Your doctor may adjust your dose as needed. However, the total dose is usually not more than 20 mg per kg of body weight per day or 600 mg per day.
- Children younger than 6 years of age—Use and dose must be determined by your doctor.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one. If you become severely short of breath, call your doctor.
Theophylline side effects
The most common theophylline side effects are nausea and vomiting, headache, increased stomach acid secretion, and gastroesophageal reflux, which could be due to phosphodiesterase inhibition. CNS (central nervous system) symptoms (irritability, lightheadedness, and dizziness) have also been observed in patients. In severe cases, seizures have also occurred. At high serum concentrations, adenosine A1A-receptor antagonism could lead to convulsions and cardiac arrhythmias 9.
Theophylline may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away.
- upset stomach
- stomach pain
- diarrhea
- headache
- restlessness
- insomnia
- irritability
If you experience any of the following symptoms, call your doctor immediately:
- vomiting
- increased or rapid heart rate
- irregular heartbeat
- seizures
- skin rash
Theophylline toxicity
Theophylline toxicity can lead to gastrointestinal distress, insomnia, and tremor. Severe nausea and vomiting, cardiac arrhythmias, hypotension, and convulsions have also been reported, more commonly in cases of overdosage. Very large overdoses, such as those during suicide attempts could potentially be lethal because of the development of arrhythmias and convulsions.
- Activated charcoal may prevent absorption by adsorbing the drug in the intestine.
- Beta-blockers could potentially be used for reversing the severe cardiovascular toxicity caused by theophylline.
- Intravenous benzodiazepines may abort seizures 3.
Theophylline has 2 primary mechanisms. One mechanism is that theophylline blocks adenosine receptors, which has both therapeutic and toxic effects such as bronchodilation, tachycardia, cardiac arrhythmias, seizures, and cerebral vasoconstriction. At larger doses, theophylline inhibits phosphodiesterase causing increased cyclic adenosine monophosphate resulting in increased levels of adrenergic activation and catecholamine release. In theophylline toxicity, epinephrine levels can be 4- to 8-times higher than normal, and norepinephrine concentrations can be 4- to 10-times higher than normal. Increased catecholamine concentrations have a variety of adverse effects such as cardiac arrhythmias, metabolic acidosis, hyperglycemia, and hypokalemia. Chronic theophylline toxicity can occur when there is an accumulation of the drug due to metabolism being overwhelmed or inhibited. It can also occur when clearance is decreased 10.
Theophylline toxicity symptoms
Depending on the dose, route of administration, and coingestants, there is a wide spectrum of clinical effects of theophylline toxicity, ranging from abdominal pain to cardiac arrhythmias to seizures.
- General: Agitation, irritability, restlessness
- Cardiovascular: Sinus tachycardia, ventricular tachycardia atrial fibrillation, supraventricular tachycardia, hypotension, cardiac arrest
- Respiratory: Tachypnea, acute lung injury, respiratory alkalosis
- Gastrointestinal (GI): Nausea, vomiting, abdominal pain
- Neurological: Tremors, hallucinations, seizures 11
Theophylline toxicity treatment
Most patients with theophylline toxicity are successfully managed with supportive care. Airway, breathing, circulation, and hemodynamic monitoring are essential to the care of patients with theophylline toxicity. Intubation with ventilator support may be required for airway protection.
Gastrointestinal (GI) decontamination: Activated charcoal (1 g/kg) by mouth or nasogastric tube is recommended in patients that present to the emergency department within if there are no contraindications to activated charcoal. Gastric lavage or induced emesis is not recommended in theophylline toxicity. Whole bowel irrigation is controversial as animal models do not demonstrate that it is a beneficial therapy. Multiple-dose activated charcoal is recommended for acute theophylline toxicity if there are no contraindications.
Hypotension-isotonic saline (20 mL/kg): Hypotension refractory to IV fluid administration, an alpha agonist such as phenylephrine is recommended. Primarily alpha agonists such as norepinephrine can be used as well. Treatment of hypotension with a beta antagonist should only be used in consultation with a toxicologist.
Nausea and vomiting: Ondansetron is recommended. Metoclopramide can be used in cases that are refractory to ondansetron.
Cardiac arrhythmias: Treatment of cardiac arrhythmias should be managed according to advanced cardiac life support and pediatric advanced life support protocols.
Seizures: In adults benzodiazepines (lorazepam, midazolam, diazepam) are the first-line treatment for theophylline-induced seizures. Phenobarbital and continuous infusion of propofol or midazolam can be used for seizures refractory to benzodiazepines. In pediatrics, benzodiazepines are the first-line treatment for seizures. Phenobarbital or continuous infusion of midazolam or pentobarbital or propofol can be used refractory seizures.
Hemodialysis: In acute overdose, hemodialysis is indicated for life-threatening arrhythmias and seizures, theophylline levels greater than 100 mcg/mL, clinical instability, or increased theophylline levels despite appropriate care. In chronic theophylline toxicity, hemodialysis is indicated with severe symptoms, such as life-threatening arrhythmias, seizures, and theophylline levels greater than 60 mcg/mL in patients between the ages of 6 months to 60 years, or levels greater than 50 mcg/mL in patients of age less than 6 months or greater than 60 years. Hemodialysis is preferred as opposed to hemoperfusion. However, if hemodialysis is not available, hemoperfusion may be used instead. Decisions to initiate hemodialysis or hemoperfusion should always be made in consultation with a medical toxicologist.
Hypokalemia: Potassium supplementation Is recommended for patients with ventricular arrhythmias or potassium levels less than 3 mEq/L 12.
References- Jilani TN, Preuss CV, Sharma S. Theophylline. [Updated 2019 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519024
- Essayan DM. Cyclic nucleotide phosphodiesterases. J. Allergy Clin. Immunol. 2001 Nov;108(5):671-80
- Hansel TT, Tennant RC, Tan AJ, Higgins LA, Neighbour H, Erin EM, Barnes PJ. Theophylline: mechanism of action and use in asthma and chronic obstructive pulmonary disease. Drugs Today. 2004 Jan;40(1):55-69
- Pacifici GM. Clinical pharmacology of theophylline in preterm infants: effects, metabolism and pharmacokinetics. Curr Pediatr Rev. 2014;10(4):297-303
- Cova D, Cuglituri G, Rossini L, Bonfardeci G. Comparative dose study of a theophylline sustained-release tablet formulation after repeated administrations. Int J Clin Pharmacol Ther Toxicol. 1989 Jun;27(6):273-5
- Sohn JA, Kim HS, Oh J, Cho JY, Yu KS, Lee J, Shin SH, Lee JA, Choi CW, Kim EK, Kim BI, Park EA. Prediction of serum theophylline concentrations and cytochrome P450 1A2 activity by analyzing urinary metabolites in preterm infants. Br J Clin Pharmacol. 2017 Jun;83(6):1279-1286
- Journey JD, Bentley TP. Theophylline Toxicity. [Updated 2018 Dec 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532962
- Monteiro J, Alves MG, Oliveira PF, Silva BM. Pharmacological potential of methylxanthines: Retrospective analysis and future expectations. Crit Rev Food Sci Nutr. 2018 Apr 06;:1-29
- Lal D, Manocha S, Ray A, Vijayan VK, Kumar R. Comparative study of the efficacy and safety of theophylline and doxofylline in patients with bronchial asthma and chronic obstructive pulmonary disease. J Basic Clin Physiol Pharmacol. 2015 Sep;26(5):443-51
- Greene SC, Halmer T, Carey JM, Rissmiller BJ, Musick MA. Theophylline toxicity: An old poisoning for a new generation of physicians. Turk J Emerg Med. 2018 Mar;18(1):37-39
- Aggelopoulou E, Tzortzis S, Tsiourantani F, Agrios I, Lazaridis K. Atrial Fibrillation and Shock: Unmasking Theophylline Toxicity. Med Princ Pract. 2018;27(4):387-391
- Greene SC, Halmer T, Carey JM, Rissmiller BJ, Musick MA. Theophylline toxicity: An old poisoning for a new generation of physicians. Turk J Emerg Med. 2018 Mar;18(1):37-39.