What is tick paralysis
Tick paralysis is a loss of muscle function that results from a tick bite. Tick paralysis is caused by over 40 species of ticks worldwide (five in North America, including the deer tick) and can occur in almost any region where ticks are found. Hard-bodied and soft-bodied female ticks are believed to make a poison that can cause paralysis. A salivary neurotoxin only produced by an engorged female tick during feeding induces paralysis. Clinical presentation varies depending on the species of tick 1. Ticks attach to the skin to feed on blood. The poison enters the bloodstream during this feeding process. The paralysis is ascending. That means it starts in the lower body and moves up. Tick paralysis has killed thousands of animals, mainly cows and sheep, in other parts of the world. Although tick paralysis is of concern in domestic animals and livestock in the United States as well, human cases are rare and usually occur in children under the age of 10.
Tick paralysis occurs when an engorged and gravid (egg-laden) female tick produces a neurotoxin in its salivary glands and transmits it to its host during feeding. Experiments have indicated that the greatest amount of toxin is produced between the fifth and seventh day of attachment (often initiating or increasing the severity of symptoms), although the timing may vary depending on the species of tick.
Tick paralysis was first described in Australia in the 19th century, but clusters of cases have been described in Argentina, Canada, and in several regions of the United States. It has been reported in both humans and domesticated animals. Like most tick-borne illnesses, the peak incidence is in the spring and early summer. Tick paralysis is reported more commonly in children, perhaps accounting for greater toxin effects given smaller body mass. It appears to be more common in females, possibly because long hair makes an engorged tick more likely to escape early detection. Reporting is not universally required, and reliable data on incidence and distribution do not exist.
Unlike Lyme disease, ehrlichiosis, and babesiosis, which are caused by the systemic proliferation and expansion of parasites in their hosts long after the offending tick is gone, tick paralysis is chemically induced by the tick and can therefore continue only in its presence. Once the tick is removed, symptoms usually diminish rapidly. However, in some cases, profound paralysis can develop and even become fatal before anyone becomes aware of a tick’s presence.
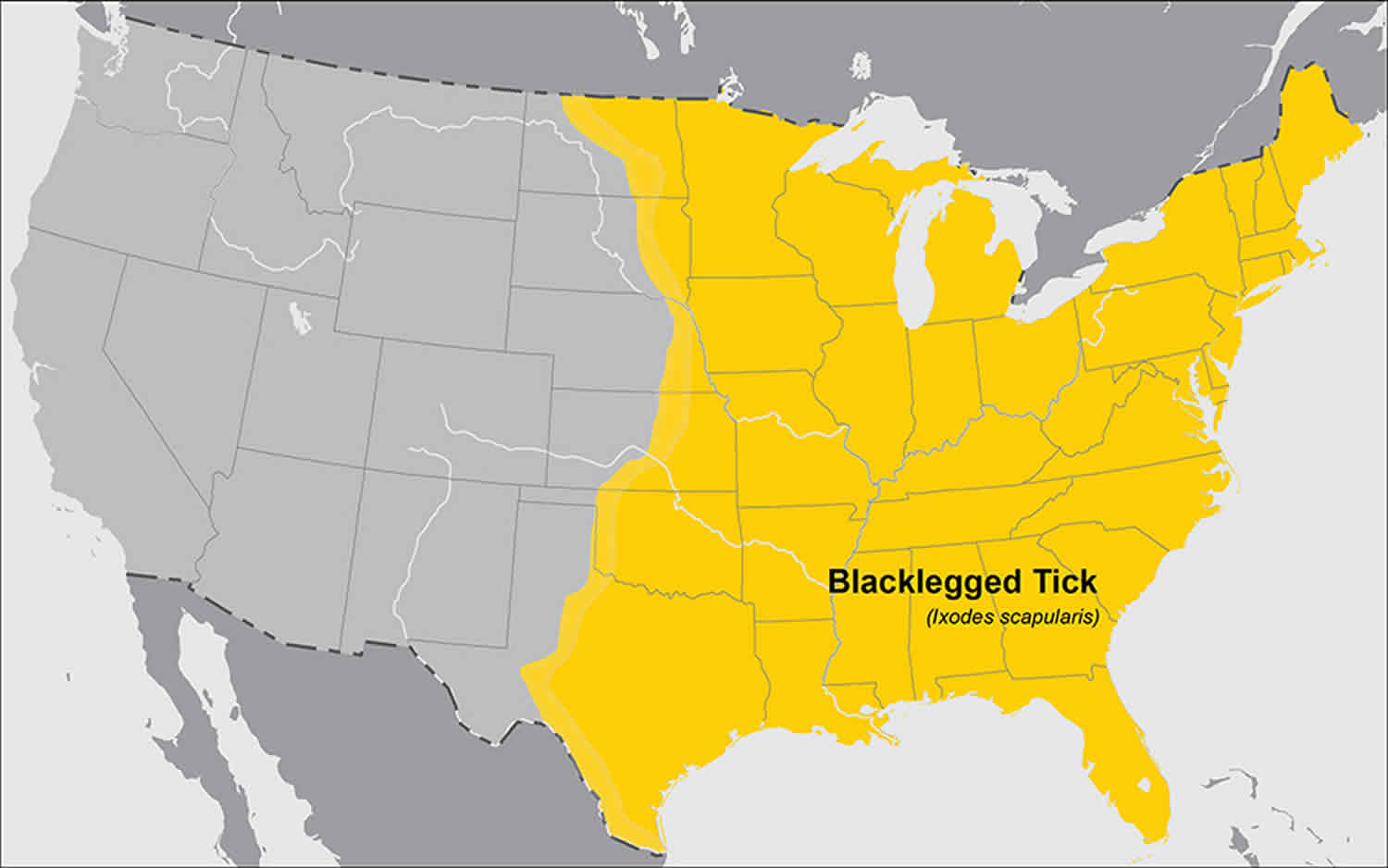
Ticks that cause tick paralysis are found in almost every region of the world. In the United States, most reported cases have occurred in the Rocky Mountain states, the Pacific Northwest and parts of the South. The five North American species of ticks thought to cause tick paralysis are widely distributed throughout the United States; therefore, the potential for contact with such ticks exists in every state.
Patients may have more than one tick-borne illness at the same time, so tick-borne infections like Lyme disease, ehrlichiosis, and Rocky Mountain Spotted fever may also occur. Many of the ticks implicated in tick paralysis are also vectors for infectious disease. Associated fever or rash is rarely reported with tick paralysis alone and should raise suspicion for infection.
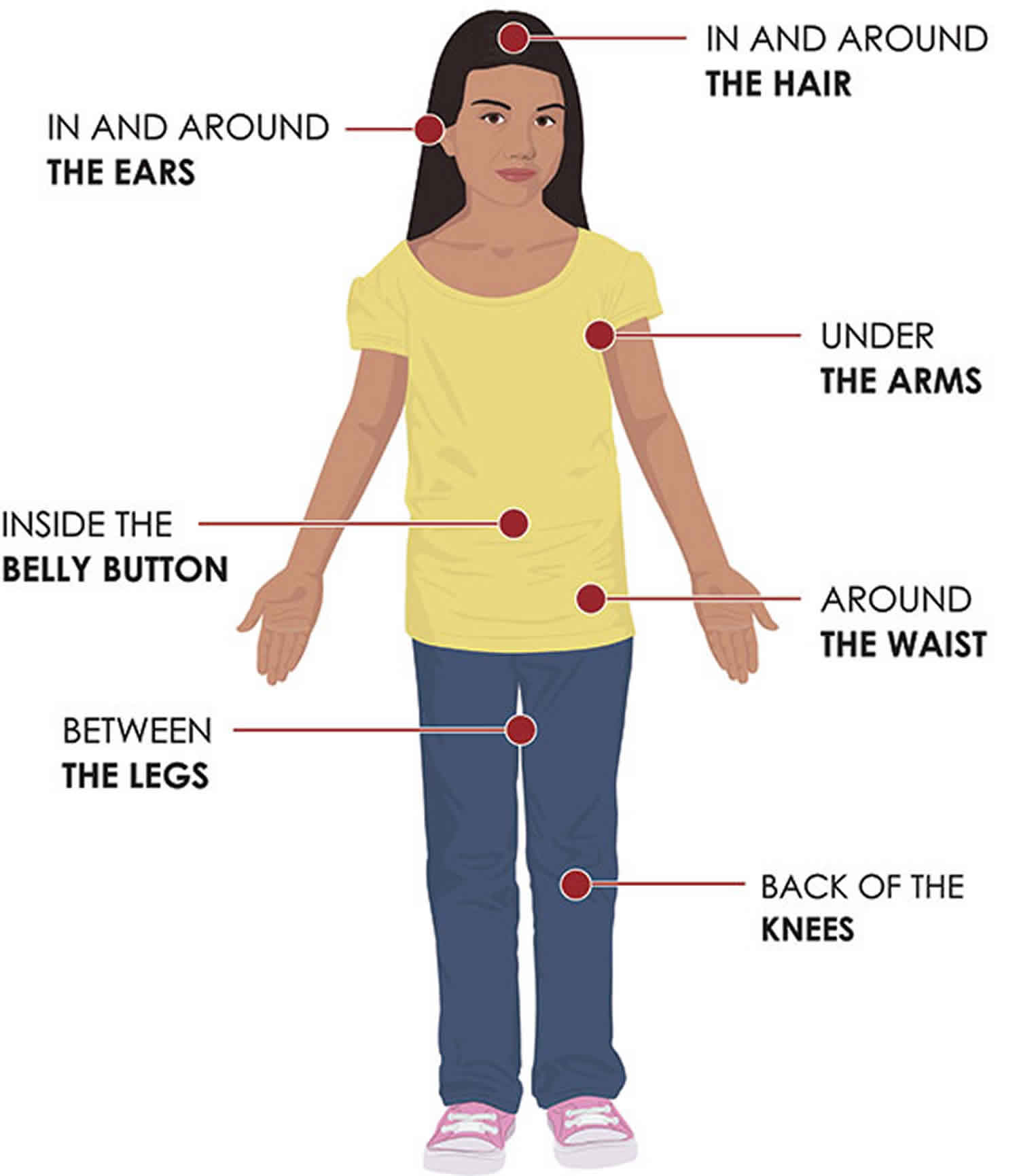
The most common site for tick attachment in the scalp behind the ears.
Ophthalmoplegia is almost universally present in Australian tick paralysis. It may be present in North American cases but is less common.
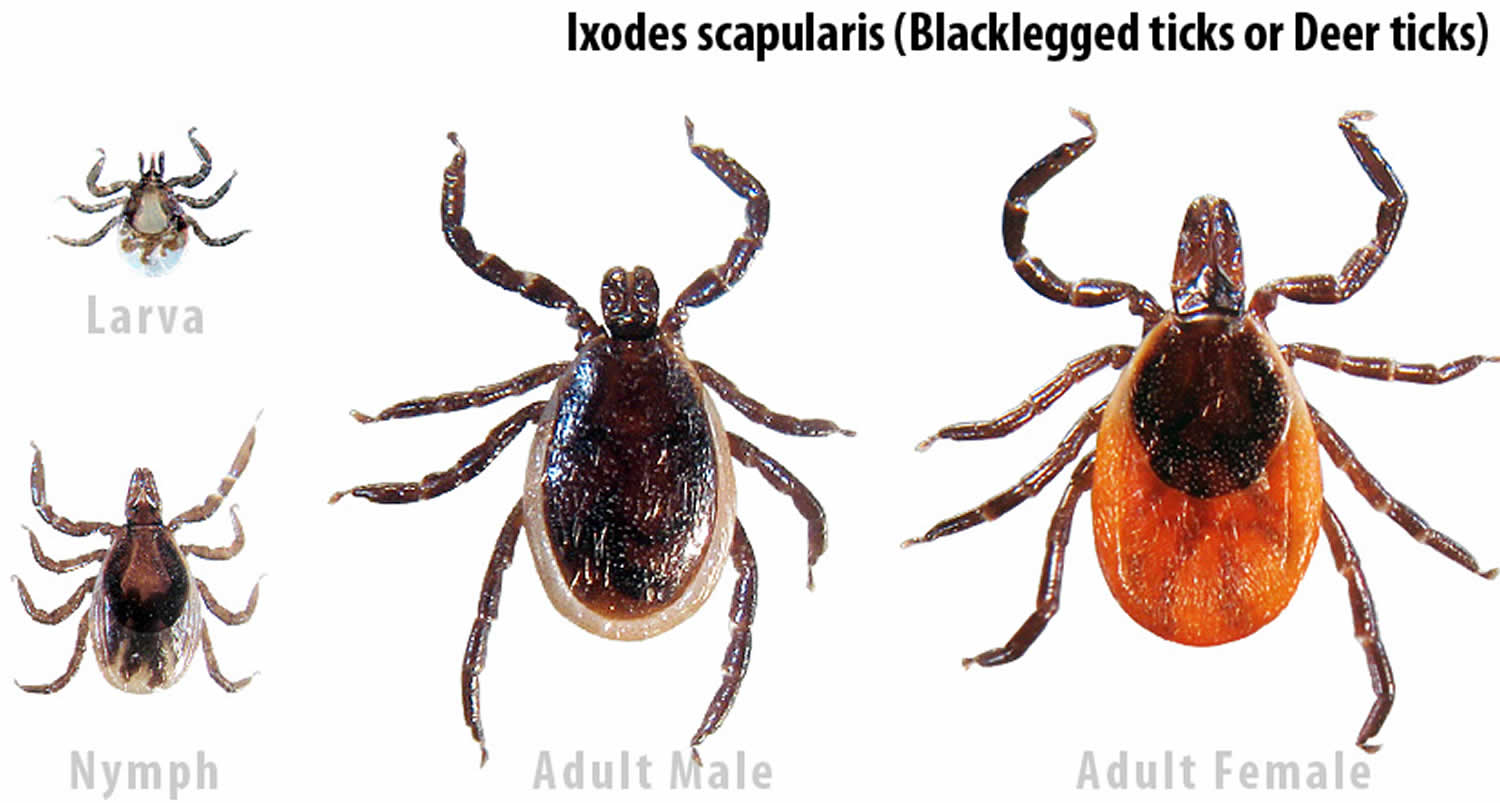
Figure 1. Deer ticks
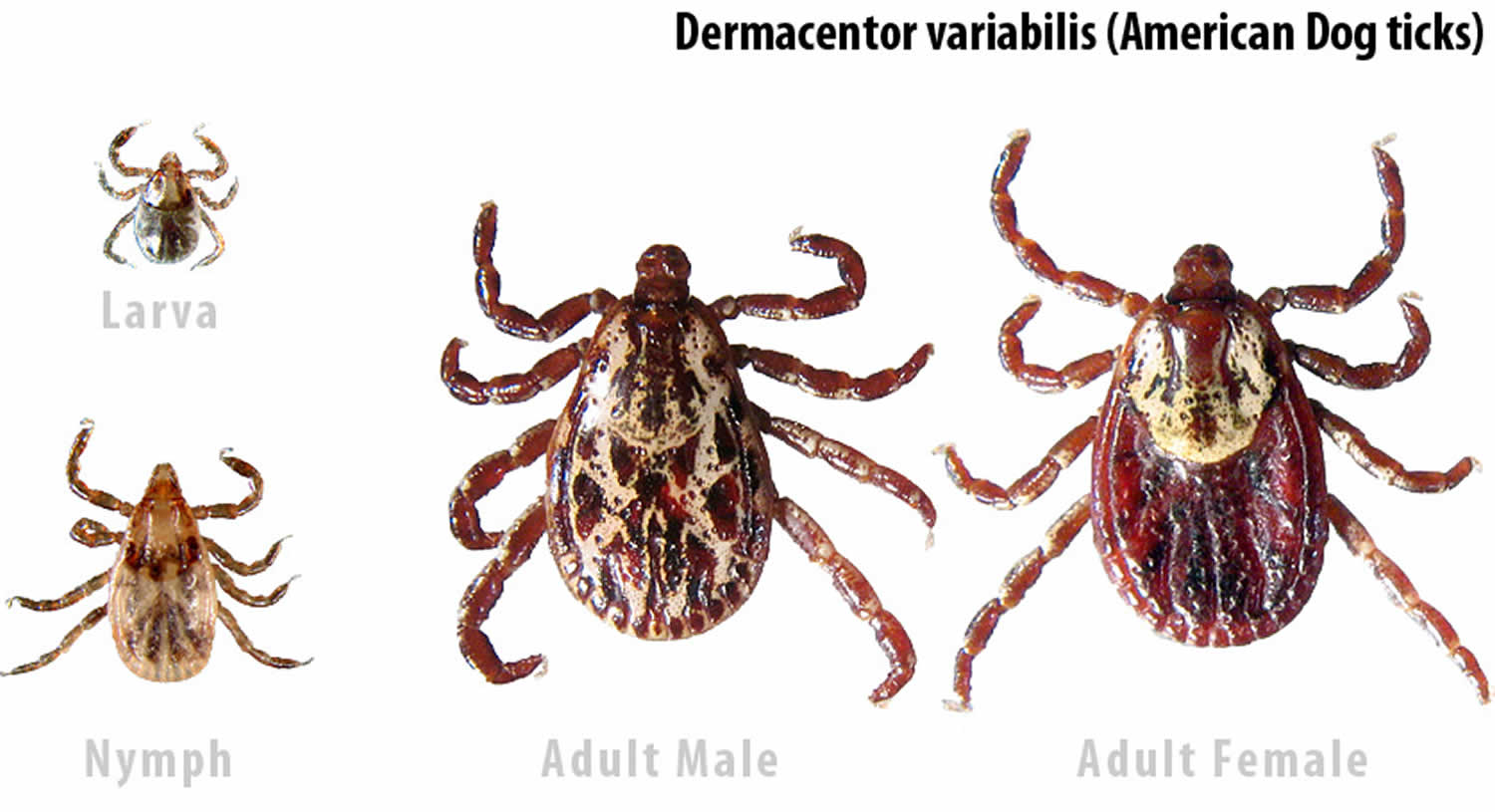
Figure 2. Dog ticks
Is tick paralysis curable?
Yes. Tick paralysis is chemically induced by the tick and can therefore continue only in its presence. Once the tick is removed, symptoms usually diminish rapidly. Full recovery is expected following the removal of the tick. However, in some cases, profound paralysis can develop and even become fatal before anyone becomes aware of a tick’s presence.
Tick paralysis causes
Over 40 species of ticks have been associated with tick paralysis. In North America, most cases of tick paralysis are associated with Dermacentor species. Dermacentor variabilis, the American dog tick, and Dermacentor andersoni, the Rocky Mountain wood tick, are the most common species associated with tick paralysis 2. Other ticks such as Amblyomma americanum, the Lone Star tick, and Ixodes scapularis, the black-legged tick, are also associated with tick paralysis. In Australia, Ixodes holocyclus, the scrub tick, is most commonly implicated.
Tick paralysis primarily affects motor pathways. Symptoms typically develop after the tick has been attached for 3 to 7 days and may vary depending on the species of tick. The precise mechanism is not fully understood, but with Dermacentor species, it most likely involves interruption of sodium flux across axonal membranes resulting in weakness due to impairment in transmission to motor nerve terminals. The neurotoxins produced by Ixodes holocyclus act on presynaptic motor neuron terminals to inhibit the release of acetylcholine and may produce clinical findings similar to botulism. Onset is typically slower than other forms of tick paralysis and may be associated with ophthalmoplegia 3.
Tick paralysis prevention
Prevention is the best way to avoid tick-borne illness. Except for tick-borne encephalitis, there is no vaccine available to prevent tick-borne disease. Protective clothing, such as long pants, long sleeves, and closed shoes should be worn in tick-infested areas, particularly in the late spring in summer when most cases occur. Pant legs should be tucked into socks when walking through high grass and brush. Permethrin, which is an insecticide, may be applied to clothing and is quite effective in repelling ticks. Other tick repellents such as diethyl-m-toluamide (DEET) may be applied to skin or clothing, with variable effectiveness. DEET can be quite toxic, with effects ranging from local skin irritation to seizures. DEET should be avoided in infants.
Use insect repellents and protective clothing when in tick-infested areas. Tuck pant legs into socks. Carefully check the skin and hair after being outside and remove any ticks you find.
If you find a tick on your child, write the information down and keep it for several months. Many tick-borne diseases do not show symptoms right away, and you may forget the incident by the time your child becomes sick with a tick-borne disease.
Before you go outdoors
- Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside walking your dog, camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
- Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
- Use Environmental Protection Agency (EPA)-registered insect repellents containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone (https://www.epa.gov/insect-repellents). EPA’s helpful search tool (https://www.epa.gov/insect-repellents/find-repellent-right-you) can help you find the product that best suits your needs. Always follow product instructions.
- DO NOT use insect repellent on babies younger than 2 months old.
- DO NOT use products containing OLE or PMD on children under 3 years old.
Avoid contact with ticks
- Avoid wooded and brushy areas with high grass and leaf litter.
- Walk in the center of trails.
After you come indoors
Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. Tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
Examine gear and pets. Ticks can ride into the home on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.
Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting Lyme disease and may be effective in reducing the risk of other tickborne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
Check your body for ticks after being outdoors. Conduct a full body check upon return from potentially tick-infested areas, including your own backyard. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body and your child’s body for ticks:
- Under the arms
- In and around the ears
- Inside belly button
- Back of the knees
- In and around the hair
- Between the legs
- Around the waist
Figure 3. Check your body for ticks
Preventing tick bites
Tick exposure can occur year-round, but ticks are most active during warmer months (April-September). Know which ticks are most common in your area (see geographic distribution of ticks that bite humans below).
When spending time outdoors, make these easy precautions part of your routine:
- Wear enclosed shoes and light-colored clothing with a tight weave to spot ticks easily
- Scan clothes and any exposed skin frequently for ticks while outdoors
- Stay on cleared, well-traveled trails
- Use insect repellant containing DEET (Diethyl-meta-toluamide) on skin or clothes if you intend to go off-trail or into overgrown areas
- Avoid sitting directly on the ground or on stone walls (havens for ticks and their hosts)
- Keep long hair tied back, especially when gardening
- Do a final, full-body tick-check at the end of the day (also check children and pets)
When taking the above precautions, consider these important facts:
- If you tuck long pants into socks and shirts into pants, be aware that ticks that contact your clothes will climb upward in search of exposed skin. This means they may climb to hidden areas of the head and neck if not intercepted first; spot-check clothes frequently.
- Clothes can be sprayed with either DEET or Permethrin. Only DEET can be used on exposed skin, but never in high concentrations; follow the manufacturer’s directions.
- Upon returning home, clothes can be spun in the dryer for 20 minutes to kill any unseen ticks
- A shower and shampoo may help to remove crawling ticks, but will not remove attached ticks. Inspect yourself and your children carefully after a shower. Keep in mind that nymphal deer ticks are the size of poppy seeds; adult deer ticks are the size of apple seeds.
Any contact with vegetation, even playing in the yard, can result in exposure to ticks, so careful daily self-inspection is necessary whenever you engage in outdoor activities and the temperature exceeds 45° F (the temperature above which deer ticks are active). Frequent tick checks should be followed by a systematic, whole-body examination each night before going to bed. Performed consistently, this ritual is perhaps the single most effective current method for prevention of Lyme disease.
Finally, prevention is not limited to personal precautions. Those who enjoy spending time in their yards can reduce the tick population around the home by:
- keeping lawns mowed and edges trimmed
- clearing brush, leaf litter and tall grass around houses and at the edges of gardens and open stone walls
- stacking woodpiles neatly in a dry location and preferably off the ground
- clearing all leaf litter (including the remains of perennials) out of the garden in the fall
- having a licensed professional spray the residential environment (only the areas frequented by humans) with an insecticide in late May (to control nymphs) and optionally in September (to control adults).
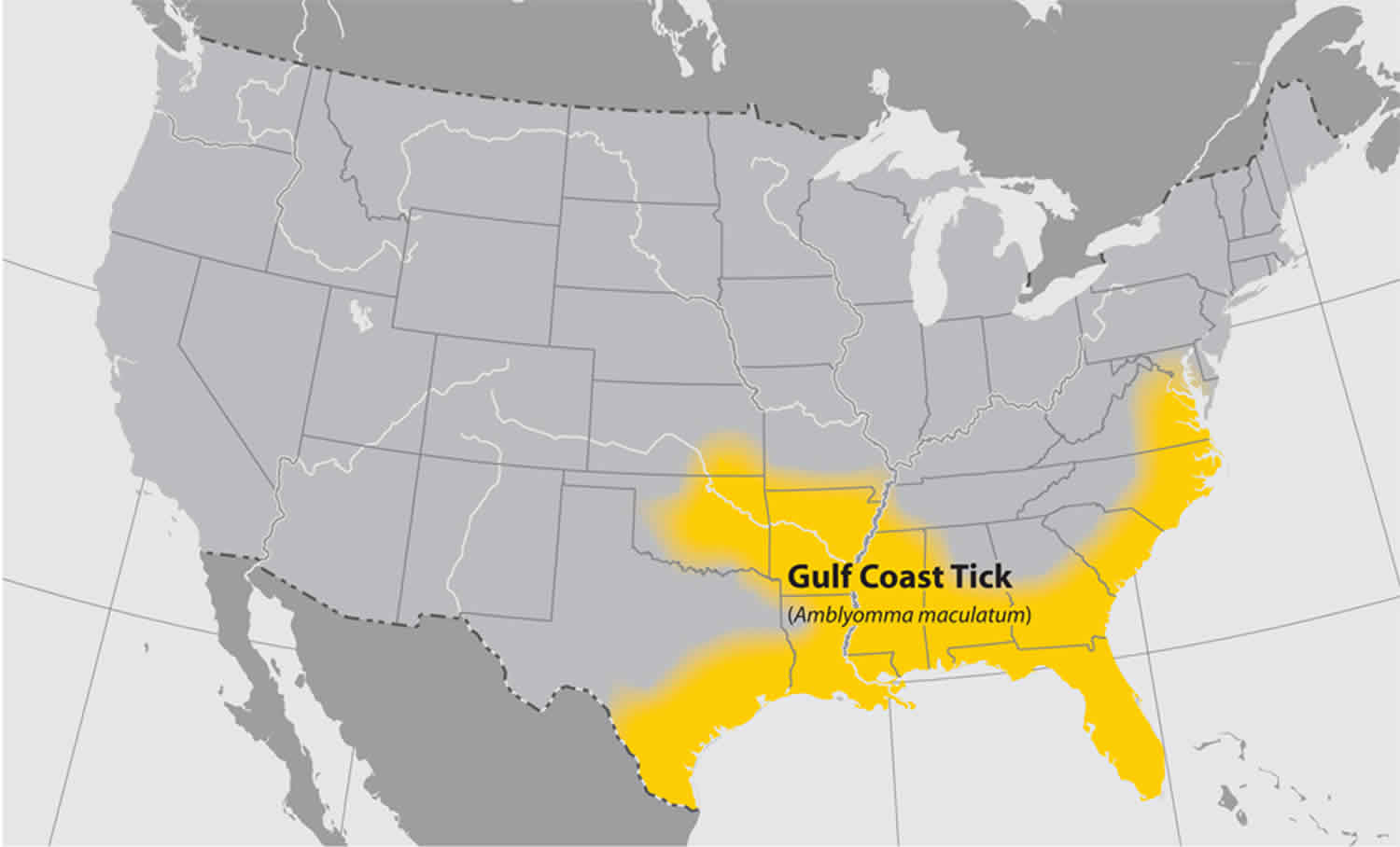
Geographic distribution of ticks that bite humans
Figure 4. Geographic distribution of American dog ticks that bite humans
Figure 5. Geographic distribution of blacklegged ticks that bite humans
Figure 6. Geographic distribution of brown dog ticks that bite humans
Figure 7. Geographic distribution of Gulf Coast ticks that bite humans
Figure 8. Geographic distribution of Lone Star ticks that bite humans
Figure 9. Geographic distribution of Rocky Mountain wood ticks that bite humans
Figure 10. Geographic distribution of Western blacklegged ticks that bite humans
Paralysis tick symptoms
Symptoms of tick paralysis generally begin from five to seven days after a tick becomes attached (usually on the scalp), beginning with fatigue, numbness of the legs, muscle pains and weakness which progress to ataxia and then ascending paralysis. Paralysis rapidly develops from the lower to the upper extremities and, if the tick is not removed, is followed by tongue and facial paralysis. The most severe complications may include convulsions, respiratory failure and, in up to 12% of untreated cases, death. Most patients present with fatigue and weakness which progress to ataxia and then ascending paralysis 2.
Children with tick paralysis develop an unsteady gait followed several days later by weakness in the lower legs. This weakness gradually moves up to involve the upper limbs.
Tick paralysis may cause breathing difficulties, which may require the use of a breathing machine.
The child may also have mild, flu-like symptoms (muscle aches, tiredness).
Some also report irritability, muscle pain or paresthesias or other subjective sensory complaints as early symptoms. Fever is absent, and there is no associated rash, headache or change in mental status. Sensory exam, despite paresthesias, is usually normal. Weakness starts in the legs and ascends and progresses rapidly. Deep tendon reflexes are absent. Muscles innervated by cranial nerves may be involved and may occasionally include pupillary dilatation. Involvement of respiratory muscles may lead to respiratory failure or death. Patients rarely present with a history of tick bites, and a thorough physical exam with careful attention to the scalp, axilla, interdigital spaces and perineum is critical in making the diagnosis. Providers frequently miss ticks, and they are often found by caregivers or other members of the healthcare team. Patients may have more than one tick attached. Guillain-Barre syndrome is the most common misdiagnosis, and a thorough search for a tick in any patient where this diagnosis is considered is critical to avoid unnecessary testing and expensive therapies such as plasmapheresis or immune globulin, which are not helpful in this setting. Tick paralysis usually progresses more rapidly than Guillain-Barre or Miller-Fisher syndrome.
Tick paralysis possible complications
Breathing difficulties can cause respiratory failure. When this happens, the body’s organs do not have enough oxygen to work well.
Tick paralysis diagnosis
People can be exposed to ticks in many ways. For example, they may have gone on a camping trip, live in a tick-infested area, or have dogs or other animals that can pick up ticks. Often, the tick is found only after thoroughly searching a person’s hair.
Finding a tick embedded in the skin and having the above symptoms confirms the diagnosis. No other testing is required.
Because of the inability of laboratory tests to indicate tick paralysis, diagnosis is based on symptoms and the rapid improvement of the patient once the engorged tick is removed.
Tick paralysis treatment
Treatment involves simply removing the feeding tick(s). Removing the tick removes the source of the poison. Recovery is rapid after the tick is removed. It is important to remove all the mouth-parts, since they contain the salivary glands which may continue to infect the patient even after the body of the tick has been removed.
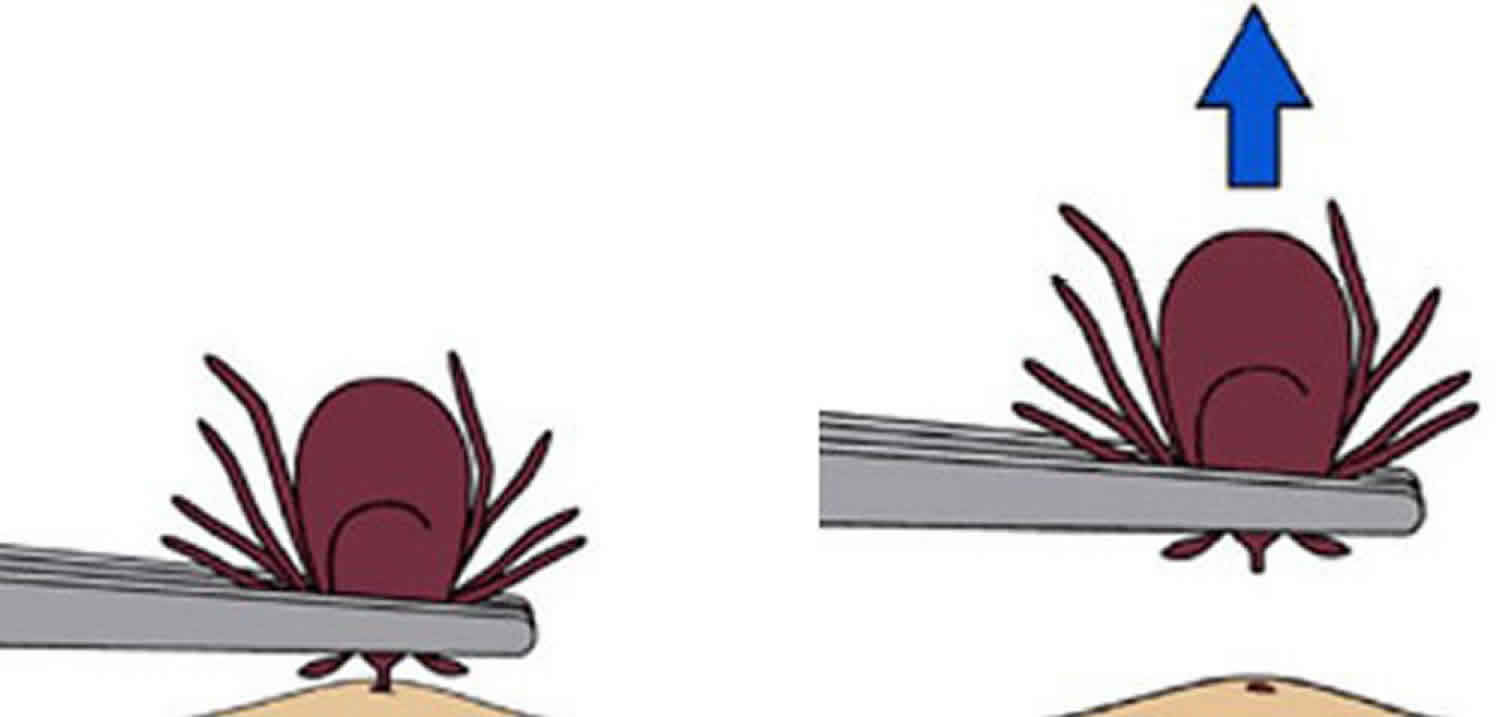
How to remove a tick
If you find a tick attached to your skin, there’s no need to panic—the key is to remove the tick as soon as possible. There are several tick removal devices on the market, but a plain set of fine-tipped tweezers work very well.
To remove a tick, follow these steps:
- Using a pair of fine-tipped or pointy tweezers, grasp the tick by the head or mouth-parts right where they enter the skin. DO NOT grasp the tick by the body.
- Without jerking, pull firmly and steadily directly outward. DO NOT twist the tick out or apply petroleum jelly, a hot match, alcohol, nail polish or any other irritant to the tick in an attempt to get it to back out. Your goal is to remove the tick as quickly as possible–not waiting for it to detach. If the mouth-parts to break off and remain in the skin, remove the mouth-parts with tweezers. If you are unable to remove the mouth easily with clean tweezers, leave it alone and let the skin heal.
- Never crush a tick with your fingers. Dispose of a live tick by putting it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet.
- Clean the bite wound with with rubbing alcohol or soap and water. Keep in mind that certain types of fine-pointed tweezers, especially those that are etched, or rasped, at the tips, may not be effective in removing nymphal deer ticks. Choose unrasped fine-pointed tweezers whose tips align tightly when pressed firmly together.
Then, monitor the site of the bite for the appearance of a rash beginning 3 to 30 days after the bite. At the same time, learn about the other early symptoms of Lyme disease and watch to see if they appear in about the same timeframe. If a rash or other early symptoms develop, see a physician immediately. Be sure to tell the doctor about your recent tick bite, when the bite occurred, and where you most likely acquired the tick.
Figure 11. How to remove a tick
Testing for ticks
People who have removed a tick sometimes wonder if they should have it tested for evidence of infection. Although some commercial groups offer testing, in general this is not recommended because:
- Laboratories that conduct tick testing are not required to have the high standards of quality control used by clinical diagnostic laboratories. Results of tick testing should not be used for treatment decisions.
- Positive results showing that the tick contains a disease-causing organism do not necessarily mean that you have been infected.
- Negative results can lead to false assurance. You may have been unknowingly bitten by a different tick that was infected.
- If you have been infected, you will probably develop symptoms before results of the tick test are available. If you do become ill, you should not wait for tick testing results before beginning appropriate treatment.
Tick paralysis prognosis
Most patients with tick paralysis will fully recover with supportive care and removal of the tick. While tick paralysis has no long-term sequelae when identified and treated, mortality may be as high as 12% in untreated or misdiagnosed cases.
Most patients with paralysis caused by Dermacentor species will fully recover within hours of tick removal. However, in cases caused by the Australian Ixodes holocyclus tick, weakness and paralysis may initially worsen in the first 24 to 48 hours after the tick is removed necessitating inpatient observation for respiratory compromise.
References- Kularatne SAM, Fernando R, Selvaratnam S, Narampanawa C, Weerakoon K, Wickramasinghe S, Pathirage M, Weerasinghe V, Bandara A, Rajapakse J. Intra-aural tick bite causing unilateral facial nerve palsy in 29 cases over 16 years in Kandy, Sri Lanka: is rickettsial aetiology possible? BMC Infect. Dis. 2018 Aug 22;18(1):418
- Simon LV, McKinney WP. Tick Paralysis. [Updated 2019 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470478
- Borawski K, Pancewicz S, Czupryna P, Zajkowska J, Moniuszko-Malinowska A. Tick paralysis. Przegl Epidemiol. 2018;72(1):17-24.