What is tinea versicolor
Tinea versicolor also known as Pityriasis versicolor, is a common long-term (chronic) fungal infection of the skin. Tinea versicolor is a superficial infection of the stratum corneum (the top layer of your skin) by the lipophilic fungus known as Malassezia furfur, formerly known as Pityrosporum, that interferes with the normal pigmentation of your skin, resulting in small, discolored patches. People with tinea versicolor develop white, yellow, red, pink or brown spots that can be mildly itchy. These patches may be lighter or darker in color than the surrounding skin and most commonly affect your shoulders, back and upper chest. The most common predisposing factor is excessive sweating but others include application of oils and systemic steroids. Hot weather, humidity and sun exposure can make tinea versicolor worse 1.
Tinea versicolor (pityriasis versicolor) is a skin reaction to overgrowth of normally occurring yeast organisms Malassezia furfur living on the skin 2. About 90% of healthy people have these yeast organisms growing on their skin but they grow in larger numbers with sweating and humidity and where the sebaceous (oil) glands in the skin are very active. Some people may have an inherited predisposition to overgrowth of these organisms. The Malassezia furfur yeast produces chemicals which may affect the normal pigment production in the skin.
Tinea versicolor is more common in warm humid environments and may be seasonal. Tinea versicolor affects about 1% of people who live in mild or moderate climates. Tinea versicolor affects up to 40% of people who live in tropical, humid climates.
Tinea versicolor occurs most frequently in teens and young adults. Sun exposure may make tinea versicolor more apparent.
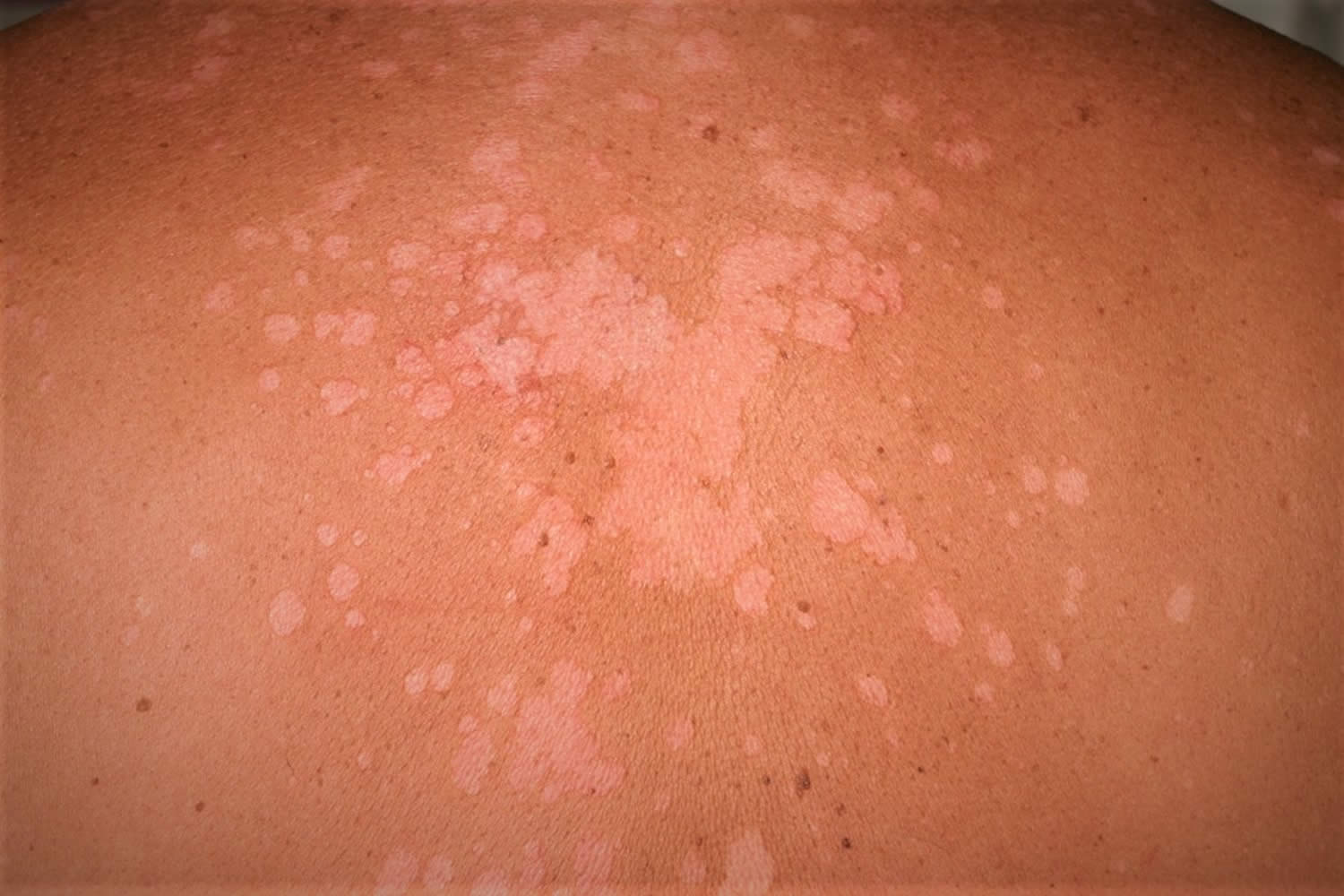
Tinea versicolor is characterized by mildly scaly lighter (hypopigmented) or darker (hyperpigmented) round or oval shaped patches, most commonly affecting areas of skin that are rich in sebum production such as the trunk (especially the upper part), neck, shoulders and upper arms 3, 4, 5, 6, 7.
Facial involvement is less common in adults. On the other hand, facial involvement is common in children and may be the only site involved 3, 8. The forehead is the usual site of facial involvement 9, 10. Other sites of involvement, such as forearms and thighs, are less common 11. Unusual sites of involvement include the scalp, eyelid, armpit, areola, periareolar area, antecubital fossae(anterior surface of the elbow), popliteal fossa (behind the knee), pubis, groin, perineum, penile shaft and vulva 12, 11, 13, 14, 15, 16.
Most people with tinea versicolor or Pityriasis versicolor are concerned about the appearance of the rash. Sometimes it may cause minor symptoms such as scaling, itch or irritation. Tinea versicolor can be much more widespread if there is a problem with your immune system. This may happen if you take medications like corticosteroids or have medical conditions like diabetes. People who are pregnant are more susceptible to tinea versicolor because of hormonal changes.
Antifungal creams, lotions or shampoos can help treat tinea versicolor. But even after successful treatment, skin color may remain uneven for several weeks or months. Tinea versicolor often recurs, especially in warm, humid weather.
What does tinea versicolor look like?
The typical appearance of the rash is of a discolored round or oval shaped eruption most commonly affecting areas of skin that are rich in sebum production such as the upper trunk region, sometimes extending to the neck, shoulders and upper arms 3, 4, 5, 6, 7. Occasionally, the rash may affect other areas of your body. The color of the eruption may appear lighter (hypopigmented) or darker (hyperpigmented) than the surrounding normal skin, hence the name “versicolor”. It’s more common for your skin to get lighter. The rash itself may be slightly raised with a fine scale. The spots can appear white, pink, red, brown, light tan or yellow.
On darker skin, tinea versicolor appears white or light tan. On lighter or paler skin, tinea versicolor looks light red or pink.
Some patches or spots can become scaly and dry. Over time, the patches get larger and start to connect, covering larger areas of your skin.
The patches might be more noticeable after sun exposure because the rest of your skin tans (or gets darker) but the infected area won’t. This makes them stand out a little more.
Figure 1. Tinea versicolor on face
Figure 2. Tinea versicolor upper back
Figure 3. Tinea versicolor
Figure 4. Tinea versicolor
Is tinea versicolor contagious?
Tinea versicolor, which is also called pityriasis versicolor, is not painful or contagious. But it can lead to emotional distress or self-consciousness.
Tinea versicolor is caused by a type of yeast called Malassezia furfur. This yeast is found on the skin of more than 90% of adults, where it normally lives without causing any problems. But tinea versicolor can develop if this yeast starts to multiply more than usual. It’s not clear exactly why this happens in some people and not in others.
Who gets tinea versicolor?
Tinea versicolor affects many people worldwide. It’s unclear why the Malassezia furfur yeast overgrows on some people’s skin and not others. People living in tropical or subtropical regions are most at risk for tinea versicolor 17, 18, 19. Tinea versicolor occurs most frequently in teens and young adults presumably because of increased skin oil production 20, 21, 22, 23. It’s common during the summer months in temperate climates and around puberty when your skin’s oil glands are more active.
Tinea versicolor is slightly more common in men than in women presumably due to increased sebaceous (oil gland) activity in men 24, 25. A positive family history of tinea versicolor is present in approximately 17% of affected individuals 26, 27. The incidence of tinea versicolor appears to be the same in all races, though the change in skin pigmentation is more visually apparent in dark-skinned individuals 25.
You may be at higher risk if you have a weak immune system. This may happen if you take medications like corticosteroids or have medical conditions like diabetes. People who are pregnant are more susceptible to tinea versicolor because of hormonal changes.
What happens if tinea versicolor is left untreated?
Tinea versicolor tends to persist for years if left untreated 28, 29, 30. Tinea versicolor doesn’t typically cause any serious side effects. If left untreated, you may experience worsening symptoms like increased discoloration or itching.
How long does tinea versicolor take to go away?
Tinea versicolor is generally easy to treat. Your skin may stay lighter or darker for several weeks or months, but it should return to its usual color eventually. Mild cases of tinea versicolor respond well to over-the-counter treatments such as using a dandruff shampoo containing selenium. Apply the shampoo to your skin in the shower and let it sit for 10 minutes before rinsing. But some people need stronger medication from their doctor. Your doctor may recommend a topical antifungal medication such as:
- Ketoconazole (Nizoral® or Extina®).
- Ciclopirox (Loprox® or Penlac®).
If your symptoms are severe, your docto may also prescribe oral antifungals such as:
- Fluconazole (Diflucan®).
- Itraconazole (Onmel® or Sporanox®).
Tinea versicolor can return, especially in the summer months. Some people may need to use medication several times a year to manage skin discoloration.
Can tinea versicolor come back?
Tinea versicolor isn’t a harmful infection and only affects the top layer of your skin. People often have more than one episode of tinea versicolor. Because the yeast grows naturally on your skin, it can recur (come back). When the air outdoors is warm and humid, the yeast can quickly grow out of control. Using medicated soap a couple of times each week or month can reduce recurrences of tinea versicolor.
Tinea versicolor outlook (prognosis)
Tinea versicolor prognosis is good. Tinea versicolor is easy to treat. Mycological cure is usually achieved soon after antifungal treatment 31. Changes in skin color may last for months. The condition may come back during warm weather, especially in patients with a positive family history of tinea versicolor 32, 33. Framil et al. 33 followed 102 patients with clinical and laboratory diagnosis of tinea versicolor for one year. After appropriate treatment, 33 (33.35%) patients did not have any relapsing episodes, 54 (52.94%) patients had one to four relapsing episodes and 15 (14.7%) patients had more than four relapsing episodes. Patients with a positive family history of tinea versicolor also have a longer duration of the disease 34. Relapse rates as high as 80% following treatment have been reported 35.
Several factors can increase your risk of developing tinea versicolor, including:
- living or staying in a warm, moist environment, in the summer
- sweating excessively (hyperhidrosis)
- having naturally oily skin
- being a teenager or in your early 20s
Tinea versicolor isn’t related to poor hygiene. The condition can’t be spread from person to person because most people already have the Malassezia yeast on their skin.
Tinea versicolor causes
Tinea versicolor is caused by dimorphic lipophilic and lipid-dependent fungus in the genus Malassezia (formerly known as Pityrosporum) species, notably Malassezia furfur, Malassezia globosa and Malassezia sympodialis 31. Other Malassezia species that have been implicated include Malassezia restricta, Malassezia obtuse, Malassezia slooffiae, Malassezia pachydermatis and Malassezia japonica 36, 37, 38, 39. These fungi are normal inhabitants on the skin surface 17, 40. Skin colonization increases with age; 25% of children and almost 100% of adults are affected 3.
Tinea versicolor occurs when the saprophytic yeast or budding form of the organism converts to the pathogenic hyphal or mycelial form. The fungal infection is localized to the stratum corneum.
A number of factors may trigger this conversion, including 31 , 41, 4, 5, 42, 43, 44:
- Hot, humid weather
- Oily skin
- Application of oily lotion or cream to the skin
- Hormonal changes
- Weakened immune system
- Hyperhidrosis (excessive sweating)
- Wearing of masks
- Excessive lipid-containing sebaceous secretions
- Malnutrition
- Poor general health
- Use of oral contraceptives
- Pregnancy
- Diabetes mellitus
- Use of topical or systemic corticosteroids
- Cushing disease
- Helicobacter pylori infection
- Immunodeficiency
- Genetic predisposition .
A recent study showed oxidative stress has no role in the pathogenesis of tinea versicolor 42.
Hypopigmented lesions (more commonly noted in darker skin tones) seen in tinea versicolor are thought to result from damage to melanocytes (skin cells that produce the skin pigment melanin) and inhibition of tyrosinase by azelaic acid (a dicarboxylic acid) produced by the Malassezia species, small melanosomes and accumulation of lipid-like material in the stratum corneum blocking ultraviolet light 45, 46, 47, 48. On the other hand, hyperpigmented lesions (more commonly noted in lighter skin tones) may result from a hyperemic inflammatory response elicited by Malassezia species, more tonofilaments in the granulosum, a thicker stratum corneum and abnormally large melanosomes 25, 46, 49, 50. Keratinase, produced by the Malassezia fungi, causes loosening of the stratum corneum with subsequent scale formation 51, 52.
Tinea versicolor prevention
To help prevent tinea versicolor from returning, your doctor can prescribe a skin or oral treatment that you use once or twice a month. You may need to use these just during warm and humid months. Preventive treatments include 53:
- Selenium sulfide (Selsun) 2.5 percent lotion or shampoo
- Ketoconazole (Ketoconazole, Nizoral, others) cream, gel, shampoo
- Itraconazole (Onmel, Sporanox) tablets, capsules or oral solution
- Fluconazole (Diflucan) tablets or oral solution.
The Malassezia furfur yeast that causes tinea versicolor occurs naturally on your skin. Doctors aren’t sure why some people develop tinea versicolor and others don’t.
If you have a history of tinea versicolor, your doctor may recommend you use soap containing zinc pyrithione (like Vanicream™ Z-Bar or DermaZinc™ Zinc Therapy Soap), ketoconazole (Nizoral®) or selenium sulfide (Selsun Blue®). This type of soap may help prevent future infections and yeast overgrowth. Your doctor may also recommend using prescriptions medications during summer months when tinea versicolor is more likely to return.
Some other things you can do to lower your risk for repeat tinea versicolor infections are:
- Avoid excessive sweating, exposure to sunlight and heat.
- Wear sunscreen or avoid sun exposure.
- Wear loose-fitting, cotton clothing to reduce sweating.
Tinea versicolor symptoms
The main symptom of tinea versicolor is patches of discolored skin that:
- Have sharp borders (edges) and fine scales
- Tinea versicolor skin spots may be lighter (or darker) than your surrounding skin. The color of the spots can be white, pink, salmon, red, tan, or brown.
- Are often dark reddish to tan in color
- Are found on your back, underarms, upper arms, chest, and neck (can appear anywhere on the body).
- Do not darken in the sun so may appear lighter than the surrounding healthy skin. The yeast prevents the skin from tanning.
- Grow together, forming patches of lighter (or darker) skin.
- Grow slowly.
- Disappear when the temperature drops and return in the spring or summer when the air turns warm and humid.
Sometimes the spots are so faint that people do not realize they have tinea versicolor. If tinea versicolor causes light spots on the skin, it can be mistaken for vitiligo. Vitiligo is a skin disease that causes the skin to lose its natural color.
But there are many ways to tell the difference:
- Vitiligo often develops symmetrically (on both sides of your body at the same time), whereas tinea versicolor may not.
- Skin affected by vitiligo usually has a normal texture, whereas areas affected by tinea versicolor are usually slightly scaly or flaky.
- Vitiligo is more common around the mouth, eyes, fingers, wrists, armpits and groin, whereas tinea versicolor tends to develop on the chest, tummy, back and upper arms.
African Americans may have a loss of skin color or an increase in skin color.
Other symptoms include:
- Increased sweating
- Cause the affected skin to itch.
Tinea versicolor complications
For some people, tinea versicolor causes skin discoloration that lasts for months to years. In most cases, this discoloration fades away gradually after treatment is complete. A preliminary study showed that topical application of cycloserine, a transaminase 1 inhibitor, to the hyperpigmented lesions of tinea versicolor twice a day for 5 days resulted in complete clearing of the hyperpigmentation 54. Well-designed, large-scale, multicenter, randomized, placebo-controlled trials are needed to confirm this finding.
Hair thinning and/or hair loss within the tinea versicolor lesions has been reported 55. In a study of 39 patients with tinea versicolor, hair thinning and/or hair loss within the tinea versicolor lesions occurred in 24 (61.5%) patients 55. Hair thinning and/or hair loss occurred most commonly on the forearms, abdomen, neck and, in men, the beard area 55.
Tinea versicolor diagnosis
The diagnosis of tinea versicolor (pityriasis versicolor) is based on a clinical examination and the typical appearance of the eruption. Your doctor can diagnose tinea versicolor by looking at it. The affected skin may show yellowish fluorescence under long wave ultraviolet light (Wood’s lamp) examination. If there’s any doubt, he or she may take skin scrapings from the infected area and view them under a microscope. In rare cases, a skin biopsy taken under local anesthetic may be required for examination under a microscope.
Tinea versicolor treatment
Treatment may be required if the rash is causing concern. Treatment is directed towards reducing the number of yeast organisms living in the skin of the affected areas, using an anti-fungal preparation applied directly to the skin.
Treatment options for tinea versicolor 31:
- Topical antifungals
- Azoles (for example, ketoconazole, econazole, eberconazole, efinaconazole, bifonazole, luliconazole, clotrimazole, miconazole, sertaconazole, sulconazole, oxiconazole, fenticonazole, tioconazole, fluconazole and dapaconazole)
- Terbinafine
- Naftifine
- Butenafine
- Ciclopirox olamine
- Non-specific topical antifungal agents (for example, selenium sulfide, zinc pyrithione, propylene glycol, Whitfield ointment, sulfur plus salicylic acid and benzoyl peroxide)
- Oral antifungals
- Itraconazole
- Fluconazole
- Laser and photodynamic therapies
- Alternative therapies
Tinea versicolor treatment over the counter
Examples include imidazole lotions or creams (such as ketoconazole, clotrimazole, econazole, miconazole) and anti-dandruff shampoos (such as ketoconazole, zinc pyrithione, selenium sulphide, ciclopirox olamine). With regard to topical therapy, ketaconazole is the most studied and seemingly the most effective. Topical antifungal, e.g., clotrimazole cream daily twice daily for 10 days is an alternative.
For smaller areas, one of the imidazole creams or lotions may be suitable and may be applied once or twice daily for 1 to 4 weeks.
For larger areas, one of the above anti-dandruff shampoos may be used as a body wash. The shampoo is applied to the whole affected area (after wetting the skin) and left on for 10 minutes before washing off. This is to allow time for the active ingredient to penetrate into the skin and hair follicles to reduce the number of yeast organisms. The treatment is performed daily for 2 to 4 weeks and subsequent maintenance therapy once or twice a week may be required to prevent recurrence. The effectiveness is generally improved with a longer course of treatment and a higher concentration of the active ingredient. If skin irritation occurs, treatment should be stopped and medical advice obtained.
Tinea versicolor home remedies
For a mild case of tinea versicolor, you can apply an over-the-counter antifungal lotion, cream, ointment or shampoo. Most fungal infections respond well to these topical agents, which include:
- Clotrimazole (Lotrimin AF) cream or lotion
- Miconazole (Micaderm) cream
- Selenium sulfide (Selsun Blue) 1 percent lotion. Apply the shampoo to your skin in the shower and let it sit for 10 minutes before rinsing.
- Terbinafine (Lamisil AT) cream or gel
- Zinc pyrithione soap
When using creams, ointments or lotions, wash and dry the affected area. Then apply a thin layer of the product once or twice a day for at least two weeks. If you’re using shampoo, rinse it off after waiting five to 10 minutes. If you don’t see an improvement after four weeks, see your doctor. You may need a stronger medication.
It also helps to protect your skin from the sun and artificial sources of UV light. Usually, the skin tone evens out eventually.
Some people need stronger medicine, so they see a doctor. Whether you decide to self-treat or see a doctor, these tips can help you get better results:
- Stop using skin care products that are oily. Use products that are oil-free. The label may also read “non-comedogenic.”
- Wear loose clothes. Nothing should feel tight.
- Protect your skin from the sun. A tan makes tinea versicolor easier to see.
- Do not use a tanning bed or sun lamp. Again, a tan makes tinea versicolor easier to see.
How to protect your skin from the sun
To get the best results, you need to protect your skin from the sun. To do this, you should apply sunscreen every day. Be sure to apply the sunscreen 20 minutes before you go outside. And apply it to all skin that will not be covered by clothing. Make sure to use a sunscreen that offers:
- UVA and UVB protection (label may say broad-spectrum).
- Sun Protection Factor (SPF) of 30+ or higher.
- Non-greasy formula (label may read “oil-free” or “non-comedogenic”).
Tinea versicolor natural treatment
A wide variety of alternative medicines have been shown to have some therapeutic effects on tinea versicolor. However, none of these treatments have yet been subjected to rigorous studies nor randomized clinical trials 31.
Tinea versicolor natural treatments include:
- topical application of beeswax and honey 56,
- essential oils of Cymbopogon citratus 57,
- quince seed mucilage hydrogel decorated with essential oils of Nigella sativa, Citrus sinensis and Cinnamon verum 58,
- polyherbal Unani formulation 59,
- Pentas longiflora leaf extract 60,
- Acalypha wilkesiana leaf extract 61,
- Artemisia sieberi shrub extract 62,
- nitric oxide-liberating cream 63,
- irradiated human amniotic membrane in combination with tea tree oil 64.
Prescription-strength medication
If tinea versicolor is severe or doesn’t respond to over-the-counter antifungal medicine, you may need a prescription-strength medication. Some of these medications are topical preparations that you rub on your skin. Others are drugs that you swallow. Examples include:
- Ciclopirox (Loprox, Penlac) cream, gel or shampoo
- Fluconazole (Diflucan) tablets or oral solution. Fluconazole 300 mg once and repeat in one week.
- Itraconazole (Onmel, Sporanox) tablets, capsules or oral solution. Itraconazole 200 mg/day for 5-7 days.
- Pramiconazole 200 mg/day for 2 days.
- Ketoconazole (Ketoconazole, Nizoral, others) cream, gel or shampoo. Ketoconazole 2% shampoo, lather scalp and trunk for 10 minutes daily for 7 days.
- Selenium sulfide (Selsun) 2.5 percent lotion or shampoo
Oral anti-fungal treatment may be considered in unusually severe or resistant cases but there is a risk of side effects and drug interactions occurring with these oral medications. Your doctor will discuss these issues.
Side effects of these tablets are uncommon, although some people experience problems such as rashes, feeling sick and abdominal (tummy) pain while taking them.
With regard to oral anti fungal agents, itraconazole and fluconazole seem equally effective for the treatment of tinea versicolor. For simplicity, fluconazole 300 mg orally once and repeat in one week is recommended.
The discoloration of the skin may take several weeks, or even months to return to normal, even after successful treatment.
Also, the infection may return in hot, humid weather. In persistent cases, you may need to take a medication once or twice a month to prevent the infection from recurring.
Tinea versicolor recurrences
It’s common for tinea versicolor to come back after treatment, particularly during the summer or during holidays to warm and humid countries.
But you can reduce this likelihood by regularly using the antifungal shampoos mentioned above.
For example, continuing to use the shampoo once every 2 to 4 weeks after the initial treatment, or once a day for a few days before going on holiday, can help prevent tinea versicolor recurring.
As these shampoos are available to buy from pharmacies, you don’t need to see your doctor for a prescription if you run out.
If you develop tinea versicolor again after treatment, you can try treating it yourself with antifungal shampoo, or see your doctor for advice and alternative treatments.
If you have frequent and severe episodes of tinea versicolor, your doctor may consider prescribing antifungal tablets to take a few times a month to prevent the condition recurring.
References- Renati S, Cukras A, Bigby M. Pityriasis versicolor. BMJ. 2015;350:h1394. doi: 10.1136/bmj.h1394
- Gupta AK, Foley KA. Antifungal treatment for pityriasis versicolor. J Fungi (Basel) 2015;1(1):13–29. doi: 10.3390/jof1010013
- Leung AKC. Pityriasis versicolor. In: Lang F, editor. The Encyclopedia of Molecular Mechanisms of Disease. Berlin: Springer-Verlag; 2009. pp. 1652–1654.
- Alam HS, Ward JM, Davis LS. Generalized tinea versicolor following initiation of ixekizumab therapy. JAAD Case Rep. 2021;18:54–56. doi: 10.1016/j.jdcr.2021.10.008
- Brandi N, Starace M, Alessandrini A, Piraccini BM. Tinea versicolor of the neck as side effect of topical steroids for alopecia areata. J Dermatolog Treat. 2019;30(8):757–759. doi: 10.1080/09546634.2019.1573308
- Cohen L, Seminario-Vidal L, Lockey RF. Dermatologic problems commonly seen by the allergist/immunologist. J Allergy Clin Immunol Pract. 2020;8(1):102–112. doi: 10.1016/j.jaip.2019.07.019
- Tan C, Zhu WY, Min ZS. Blaschkoid pityriasis versicolor. Mycoses. 2010;53(4):366–368. doi: 10.1111/j.1439-0507.2009.01721.x
- Terragni L, Lasagni A, Oriani A, Gelmetti C. Pityriasis versicolor in the pediatric age. Pediatr Dermatol. 1991;8(1):9–12. doi: 10.1111/j.1525-1470.1991.tb00831.x
- Sandhu K, Kanwar AJ. Extensive pityriasis versicolor of the face. J Dermatol. 2004;31(3):258–259. doi: 10.1111/j.1346-8138.2004.tb00670.x
- Terragni L, Lasagni A, Oriani A. Pityriasis versicolor of the face. Mycoses. 1991;34(7–8):345–347. doi: 10.1111/j.1439-0507.1991.tb00674.x
- Romano C, Feci L, Mancianti F, Fimiani M. Perineal and genital pityriasis versicolor due to Malassezia globosa. J Eur Acad Dermatol Venereol. 2015;29(9):1857–1858. doi: 10.1111/jdv.12547
- Greco V, Megna M, Luciano MA, Fabbrocini G. Pityriasis versicolor with uncommon localizations. G Ital Dermatol Venereol. 2020;155(6):786–787. doi: 10.23736/S0392-0488.18.06120-5
- Cinelli E, Vastarella M, Fabbrocini G, Gallo L. Erythrasmoid pityriasis versicolor with exclusive involvement of the pubis and inguinal region. Ital J Dermatol Venerol. 2021;156(Suppl 1 to 6):11–12. doi: 10.23736/S2784-8671.18.06208-9
- Nevas J. Tinea versicolor: understanding effective treatment options. Nurse Pract. 2012;37(1):11–13. doi: 10.1097/01.NPR.0000409912.87769.f0
- Huang WW, Tharp MD. A case of tinea versicolor of the eyelids. Pediatr Dermatol. 2013;30(6):e242–e243. doi: 10.1111/j.1525-1470.2012.01753.x
- Khaddar RK, Cherif F, Ben Hadid R, Mokni M, Ben Osman A. Penile shaft involvement in pityriasis versicolor. Acta Dermatovenerol Alp Pannonica Adriat. 2008 Jun;17(2):86-9. https://s3-eu-west-1.amazonaws.com/thejournalhub/10.15570/archive/acta-apa-08-2/9.pdf
- Gupta AK, Bluhm R, Summerbell R. Pityriasis versicolor. J Eur Acad Dermatol Venereol. 2002;16(1):19–33. doi: 10.1046/j.1468-3083.2002.00378.x
- Gupta AK, Batra R, Bluhm R, Faergemann J. Pityriasis versicolor. Dermatol Clin. 2003;21(3):413–429. v–vi. doi: 10.1016/s0733-8635(03)00039-1
- Hellgren L, Vincent J. The incidence of tinea versicolor in central Sweden. J Med Microbiol. 1983;16(4):501–502. doi: 10.1099/00222615-16-4-501
- Ghosh SK, Dey SK, Saha I, Barbhuiya JN, Ghosh A, Roy AK. Pityriasis versicolor: a clinicomycological and epidemiological study from a tertiary care hospital. Indian J Dermatol. 2008;53(4):182–185. doi: 10.4103/0019-5154.44791
- Karakaş M, Turaç-Biçer A, Ilkit M, Durdu M, Seydaoğlu G. Epidemiology of pityriasis versicolor in Adana, Turkey. J Dermatol. 2009;36(7):377–382. doi: 10.1111/j.1346-8138.2009.00663.x
- Leung AKC, Barankin B. Tinea versicolor in a 69-year-old man: an uncommon finding. Sch J Med Case Rep. 2015;3(10A):993–994.
- Rao GS, Kuruvilla M, Kumar P, Vinod V. Clinico-epidermiological studies on tinea versicolor. Indian J Dermatol Venereol Leprol. 2002 Jul-Aug;68(4):208-9.
- Bélec L, Testa J, Bouree P. Pityriasis versicolor in the Central African Republic: a randomized study of 144 cases. J Med Vet Mycol. 1991;29(5):323–329. doi: 10.1080/02681219180000491
- Kallini JR, Riaz F, Khachemoune A. Tinea versicolor in dark-skinned individuals. Int J Dermatol. 2014;53(2):137–141. doi: 10.1111/ijd.12345
- Burke RC. Tinea versicolor: susceptibility factors and experimental infection in human beings. J Invest Dermatol. 1961;36:389–402. doi: 10.1038/jid.1961.60
- Gupta AK, Kogan N, Batra R. Pityriasis versicolor: a review of pharmacological treatment options. Expert Opin Pharmacother. 2005;6(2):165–178. doi: 10.1517/14656566.6.2.165
- Gupta AK, Lyons DC. Pityriasis versicolor: an update on pharmacological treatment options. Expert Opin Pharmacother. 2014;15(12):1707–1713. doi: 10.1517/14656566.2014.931373
- Gupta AK, Lane D, Paquet M. Systematic review of systemic treatments for tinea versicolor and evidence-based dosing regimen recommendations. J Cutan Med Surg. 2014;18(2):79–90. doi: 10.2310/7750.2013.13062
- Pantazidou A, Tebruegge M. Recurrent tinea versicolor: treatment with itraconazole or fluconazole? Arch Dis Child. 2007;92(11):1040–1042. doi: 10.1136/adc.2007.124958
- Leung AK, Barankin B, Lam JM, Leong KF, Hon KL. Tinea versicolor: an updated review. Drugs Context. 2022 Nov 14;11:2022-9-2. doi: 10.7573/dic.2022-9-2
- Dyląg M, Leniak E, Gnat S, Szepietowski JC, Kozubowski L. A case of anti-pityriasis versicolor therapy that preserves healthy mycobiome. BMC Dermatol. 2020;20:9. doi: 10.1186/s12895-020-00106-x
- Framil VM, Melhem MS, Szeszs MW, Zaitz C. New aspects in the clinical course of pityriasis versicolor. An Bras Dermatol. 2011;86(6):1135–1140. doi: 10.1590/s0365-05962011000600011
- Jena DK, Sengupta S, Dwari BC, Ram MK. Pityriasis versicolor in the pediatric age group. Indian J Dermatol Venereol Leprol. 2005;71(4):259–261. doi: 10.4103/0378-6323.16618
- Faergemann J. Pityrosporum species as a cause of allergy and infection. Allergy. 1999;54(5):413–419. doi: 10.1034/j.1398-9995.1999.00089.x
- Duy Nguyen B, Thi Thanh Vo H, Dinh Thi Thanh M, et al. Epidemiological characterization of pityriasis versicolor and distribution of Malassezia species among students in Hai Phong city, Vietnam. Curr Med Mycol. 2020;6(2):11–17. doi: 10.18502/CMM.6.2.2838
- Ogunbiyi AO, George AO. Pityriasis versicolor: Current concepts in Aetiology and Management. Niger Postgrad Med J. 2005 Sep;12(3):183-8.
- Petry V, Tanhausen F, Weiss L, Milan T, Mezzari A, Weber MB. Identification of Malassezia yeast species isolated from patients with pityriasis versicolor. An Bras Dermatol. 2011;86(4):803–806. doi: 10.1590/s0365-05962011000400032
- Romero-Sandoval K, Costa AA, Teixeira Sousa MG, et al. Recurrent and disseminated pityriasis versicolor: a novel clinical form consequent to Malassezia-host interaction? Med Hypotheses. 2017;109:139–144. doi: 10.1016/j.mehy.2017.10.013
- Kurniadi I, Hendra Wijaya W, Timotius KH. Malassezia virulence factors and their role in dermatological disorders. Acta Dermatovenerol Alp Pannonica Adriat. 2022 Jun;31(2):65-70. https://acta-apa.mf.uni-lj.si/journals/acta-dermatovenerol-apa/papers/10.15570/actaapa.2022.8/actaapa.2022.8.pdf
- Aghaei Gharehbolagh S, Kordbacheh P, Hashemi SJ, et al. MGL_3741 gene contributes to pathogenicity of Malassezia globosa in pityriasis versicolor. Mycoses. 2018;61(12):938–944. doi: 10.1111/myc.12840
- Kilinc F, Akbas A, Sener S, Ergin M, Baran P, Metin A. The effect of tinea versicolor on thiol/disulphide homeostasis. Postepy Dermatol Alergol. 2018;35(3):299–303. doi: 10.5114/ada.2018.76227
- Kutlu Ö, Doğan Z, Ekşioğlu HM, Kekilli M. Relationship between helicobacter pylori infection and pityriasis versicolor: can helicobacter pylori infection be a new etiologic factor for pityriasis versicolor? Turk J Med Sci. 2020;50(4):771–775. doi: 10.3906/sag-1910-48
- Miotto IZ, De Oliveira WRP. Epidermodysplasia verruciformis: report of two patients with autosomal dominant inheritance. Dermatol Online J. 2021;27(2) 13030/qt53t469nn
- Charles CR, Sire DJ, Johnson BL, Beidler JG. Hypopigmentation in tinea versicolor: a histochemical and electronmicroscopic study. Int J Dermatol. 1973;12(1):48–58. doi: 10.1111/j.1365-4362.1973.tb00212.x
- Galadari I, el Komy M, Mousa A, Hashimoto K, Mehregan AH. Tinea versicolor: histologic and ultrastructural investigation of pigmentary changes. Int J Dermatol. 1992;31(4):253–256. doi: 10.1111/j.1365-4362.1992.tb03565.x
- Karaoui R, Bou-Resli M, Al-Zaid NS, Mousa A. Tinea versicolor: ultrastructural studies on hypopigmented and hyperpigmented skin. Dermatologica. 1981;162(2):69–85. doi: 10.1159/000250253
- Nazzaro-Porro M, Passi S. Identification of tyrosinase inhibitors in cultures of Pityrosporum. J Invest Dermatol. 1978;71(3):205–208. doi: 10.1111/1523-1747.ep12547184
- Aljabre SH, Alzayir AA, Abdulghani M, Osman OO. Pigmentary changes of tinea versicolor in dark-skinned patients. Int J Dermatol. 2001;40(4):273–275. doi: 10.1046/j.1365-4362.2001.01201.x
- Dotz WI, Henrikson DM, Yu GS, Galey CI. Tinea versicolor: a light and electron microscopic study of hyperpigmented skin. J Am Acad Dermatol. 1985;12(1 Pt 1):37–44. doi: 10.1016/s0190-9622(85)70006-0
- Han A, Calcara DA, Stoecker WV, Daly J, Siegel DM, Shell A. Evoked scale sign of tinea versicolor. Arch Dermatol. 2009;145(9):1078. doi: 10.1001/archdermatol.2009.203
- Rivard SC. Pityriasis versicolor: avoiding pitfalls in disease diagnosis and therapy. Mil Med. 2013;178(8):904–906. doi: 10.7205/MILMED-D-13-00057
- Choi FD, Juhasz MLW, Atanaskova Mesinkovska N. Topical ketoconazole: a systematic review of current dermatological applications and future developments. J Dermatolog Treat. 2019;30(8):760–771. doi: 10.1080/09546634.2019.1573309
- Mayser P, Rieche I. Rapid reversal of hyperpigmentation in pityriasis versicolor upon short-term topical cycloserine application. Mycoses. 2009;52(6):541–543. doi: 10.1111/j.1439-0507.2009.01784.x
- Mostafa WZ, Assaf MI, Ameen IA, El Safoury OS, Al Sulh SA. Hair loss in pityriasis versicolor lesions: a descriptive clinicopathological study. J Am Acad Dermatol. 2013;69(1):e19–e23. doi: 10.1016/j.jaad.2012.03.004
- Cherniack EP. Bugs as drugs, Part 1: Insects: the “new” alternative medicine for the 21st century? Altern Med Rev. 2010 Jul;15(2):124-35.
- Carmo ES, Pereira Fde O, Cavalcante NM, Gayoso CW, Lima Ede O. Treatment of pityriasis versicolor with topical application of essential oil of Cymbopogon citratus (DC) Stapf – therapeutic pilot study. An Bras Dermatol. 2013;88(3):381–385. doi: 10.1590/abd1806-4841.20131800
- Mirzaii M, Yaeghoobi M, Afzali M, Amirkhalili N, Mahmoodi M, Sajirani EB. Antifungal activities of quince seed mucilage hydrogel decorated with essential oils of Nigella sativa, Citrus sinensis and Cinnamon verum. Iran J Microbiol. 2021;13(3):352–359. doi: 10.18502/ijm.v13i3.6398
- Lone AH, Ahmad T, Anwar M, Sofi G. Clinical efficacy and safety of a pharmacopial polyherbal Unani formulation in pityriasis versicolor: a comparative randomized single-blind study. J Altern Complement Med. 2012;18(10):978–982. doi: 10.1089/acm.2011.0520
- Kagisha V, Djang’eing’a RM, Muganga R, et al. Pentas longiflora Oliv. (Rubiaceae), a plant used in the treatment of pityriasis versicolor in Rwanda: chemical composition and standardization of leaves and roots. Fitoterapia. 2021;153:104974. doi: 10.1016/j.fitote.2021.104974
- Sherifat KO, Itohan AM, Adeola SO, Adeola KM, Aderemi OL. Antifungal activity of Acalypha wilkesiana: a preliminary study of fungal isolates of clinical significance. Afr J Infect Dis. 2021;16(1):21–30. doi: 10.21010/Ajid.v16i1.4
- Rad F, Aala F, Reshadmanesh N, Yaghmaie R. Randomized comparative clinical trial of Artemisia sieberi 5% lotion and clotrimazole 1% lotion for the treatment of pityriasis versicolor. Indian J Dermatol. 2008;53(3):115–118. doi: 10.4103/0019-5154.43209
- Jowkar F, Jamshidzadeh A, Pakniyat S, Namazi MR. Efficacy of nitric oxide-liberating cream on pityriasis versicolor. J Dermatolog Treat. 2010;21(2):93–96. doi: 10.3109/09546630902887229
- Nashwa RK, Ahmed EB, Nemr WA. Comparative study between topically applied irradiated human amniotic membrane in combination with tea tree oil versus topical tioconazole in pityraisis versicolor treatment. Cell Tissue Bank. 2020;21(2):313–320. doi: 10.1007/s10561-020-09824-5