What is vasa previa
Vasa previa is a rare but clinically important obstetrical complication in which fetal blood vessels run in close proximity to the inner cervical os below the presenting part, without the support of placental tissue or umbilical cord 1. These fetal blood vessels course within the membranes (unsupported by the umbilical cord or placental tissue) and are at risk of rupture when the supporting membranes rupture. Vasa previa can be associated with a low-lying placenta or placenta previa 2. Rupture of these fetal blood vessels at the time of spontaneous or artificial rupture of the membranes not infrequently results in fetal exsanguination and death 3. When the diagnosis is not made prenatally, over half of fetuses die, and median Apgar scores in survivors are low (median, 1 at 1 min and 4 at 5 min) 4. In addition, over half of these survivors require neonatal blood transfusions 4. A good outcome depends primarily on prenatal diagnosis by ultrasound and elective delivery before the membranes rupture 5.
The estimated incidence of vasa previa is approximately 1 in 2500 deliveries, but it is much higher (1 in 700) among patients who conceive through assisted reproductive technologies 2. About 10% of vasa previa occur in twins 6.
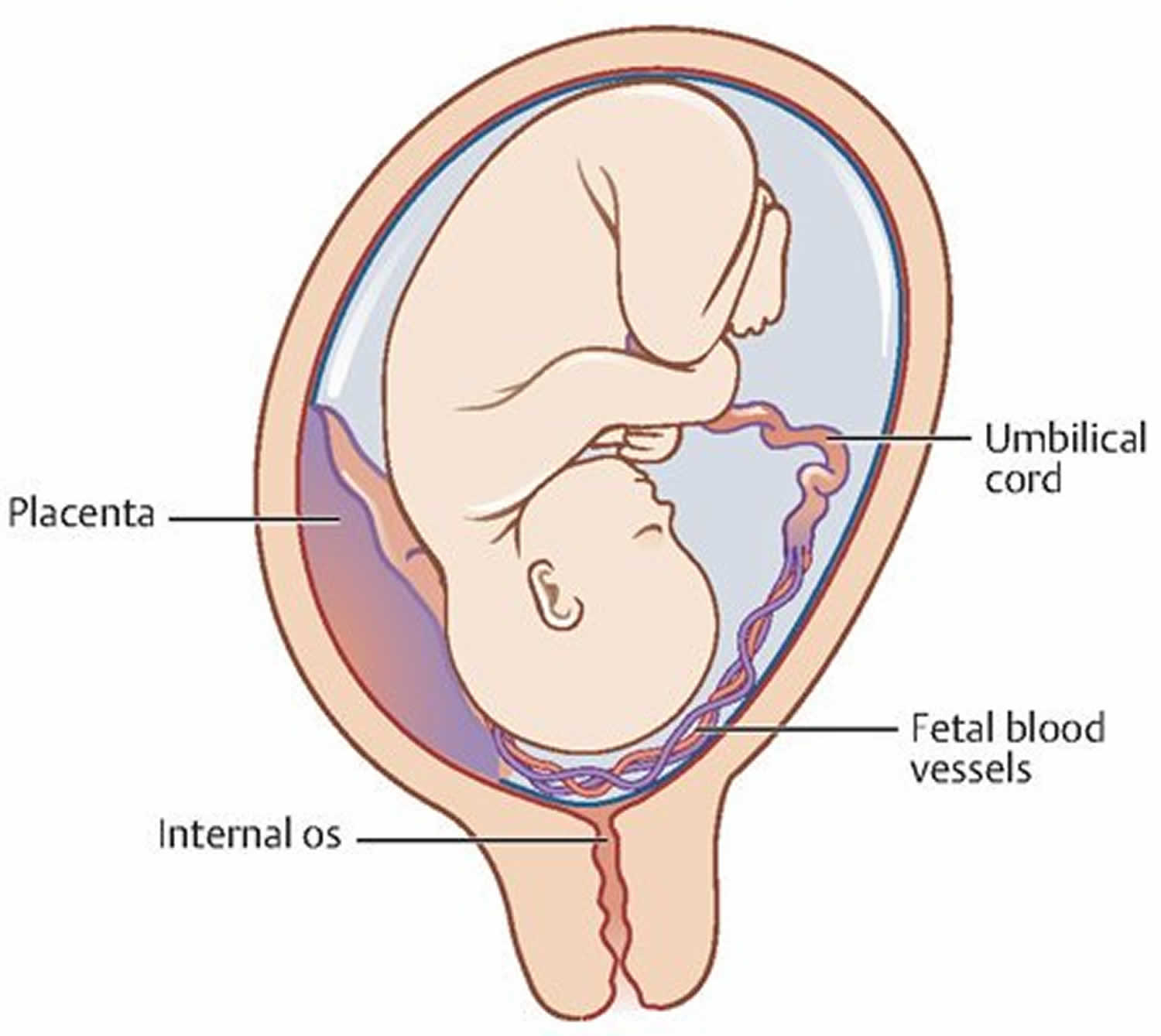
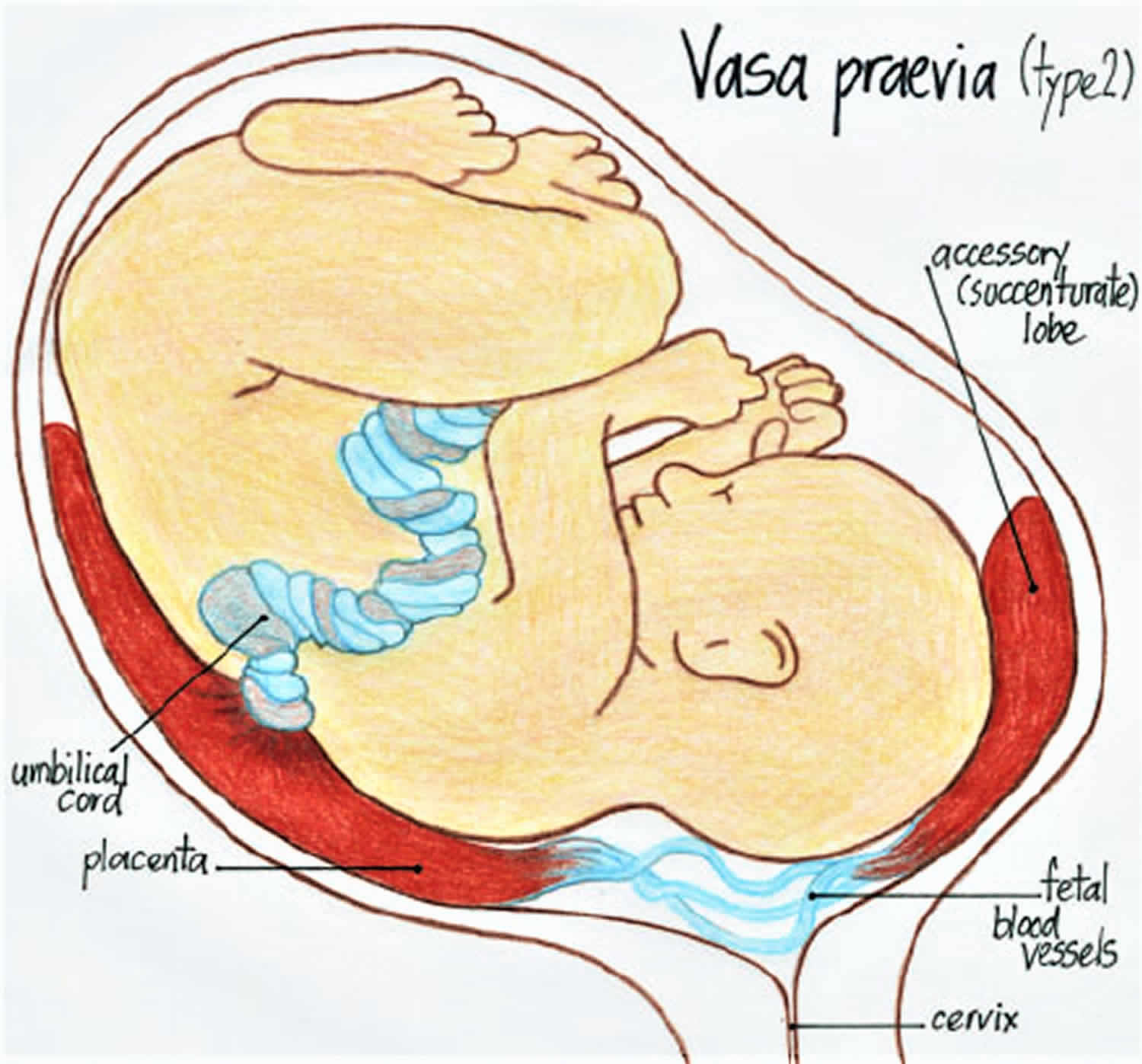
Two variants of vasa previa have been described: Type 1 results from velamentous insertion of the cord (see Figure 1) and Type 2 from vessels running between two lobes of a bilobed or succenturiate placenta (Figure 2) 7. Pregnancies with second‐trimester low‐lying placentae, placentae with accessory lobes, multiple pregnancies, and those resulting from in‐vitro fertilization (IVF) have previously been described as being at risk for vasa previa. Women with such conditions may benefit from routine prenatal determination of the placental cord insertion site 8.
Fortunately, vasa previa can often be diagnosed prenatally by ultrasound examination. The importance and clinical impact of an antenatal diagnosis of vasa previa is very significant because of the likelihood of adverse fetal outcomes 9. Because the blood vessels are attached to the chorion, rupture of fetal membranes can result in fetal bleeding and death within minutes. When vasa previa is not diagnosed antenatally, the perinatal mortality rate is reported to be approximately 44%, whereas 97% of fetuses survive when an antenatal diagnosis is made, indicating significantly different outcomes 10. Furthermore, a low-lying placenta is reportedly a risk factor for vasa previa because it occurs in 5% of patients 6. Accurate diagnosis of vasa previa is therefore crucial.
Figure 1. Vasa previa type 1
[Source 11 ]Figure 2. Vasa previa type 2
[Source 11 ]Vasa previa causes
The 2 main causes of vasa previa are velamentous insertions (where the cord inserts directly into the membranes, leaving unprotected vessels running to the placenta) (25–62%) and vessels crossing between lobes of the placenta such as in succenturiate or bilobate placentas (33–75%) 10. Less commonly, a vessel that courses over the edge of a marginal placenta or a placenta previa may become a vasa previa after extension of the placenta over better vascularized area (trophotropism) 12 and involution of the cotyledons that were previa 13.
Risk factors for vasa previa
Conditions associated with vessels that run close to the cervix, such as low-lying placenta 14, placenta previa 15, multiple pregnancies 16, and of course multilobate placentas and velamentous insertion about 1% of singleton pregnancy 17 and 10% in multifetal pregnancies 18. About 2% of velamentous insertions are associated with a vasa previa 19.
Placenta membranacea 20 is also a risk factor. It is less clear why, but in-vitro fertilization increases the risk of vasa previa 21, about 1:300 pregnancies 22. Many of these conditions present with vaginal bleeding which should be considered a possible alert symptom for vasa previa.
Vasa previa symptoms
Vasa previa is asymptomatic. Therefore the identification and exclusion of vasa previa using trans-vaginal ultrasound are essential to ensure appropriate and timely treatment.
Previously, vasa previa was usually detected by digital palpation of the fetal vessels within the membranes during labor or on the basis of acute-onset vaginal bleeding and subsequent fetal bradycardia and/or death after membrane rupture.
Vasa previa diagnosis
The primary methods of vasa previa diagnosis are trans-vaginal ultrasonography and real-time color Doppler ultrasonography, and most cases are diagnosed antenatally.
Previously, vasa previa was usually detected by digital palpation of the fetal vessels within the membranes during labor or on the basis of acute-onset vaginal bleeding and subsequent fetal bradycardia and/or death after membrane rupture.
Alternative methods of diagnosis of a vasa previa include amnioscopy, Apt, Ogita alkaline denaturation test that may help to rapidly identify the presence of fetal hemoglobin 23 or similar fetal blood detection tests 24, have mostly a historical significance. MRI has been suggested too 25. All these methods require a greater expertise then color Doppler ultrasound.
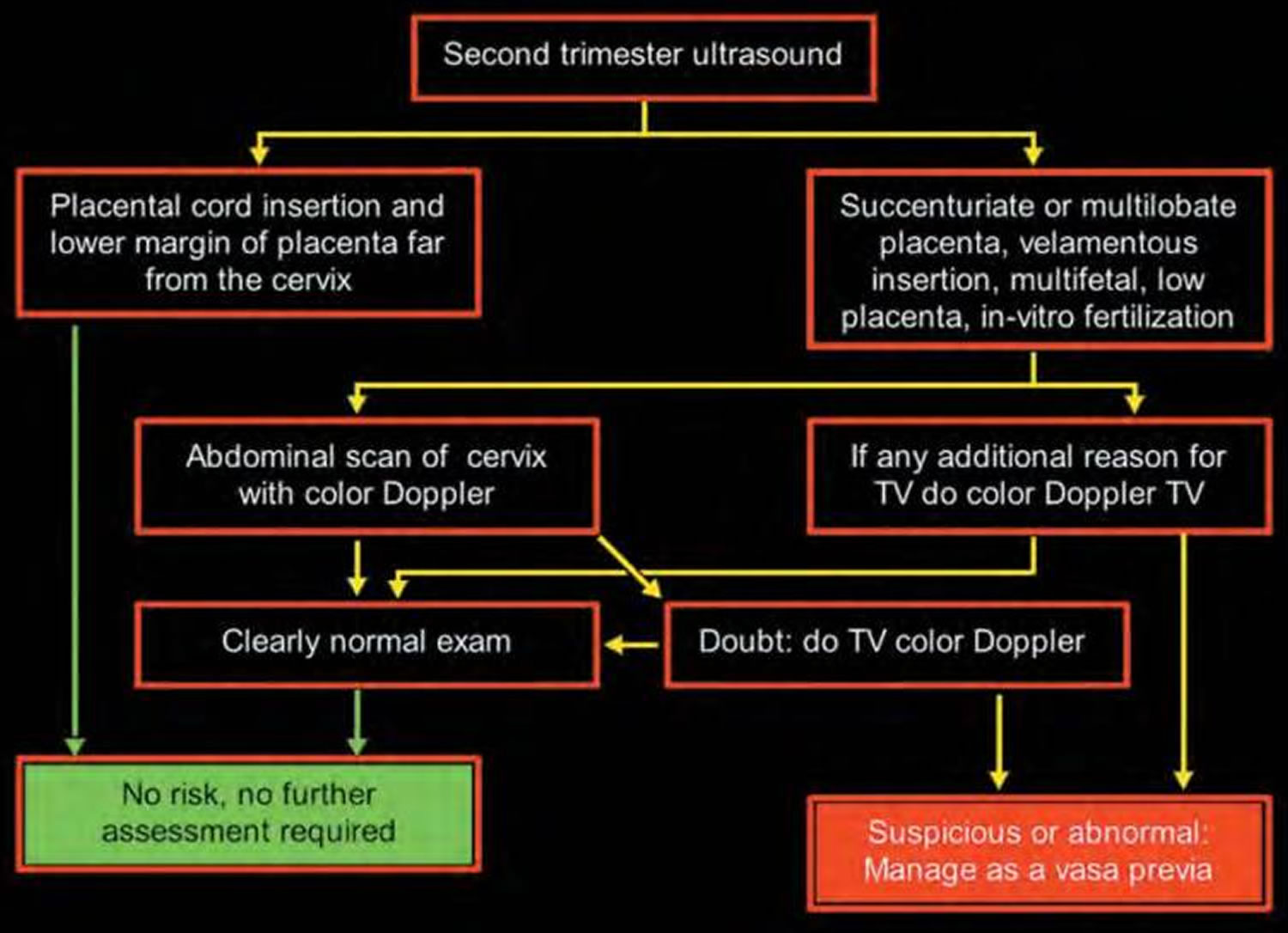
Although vasa previa can be recognized in grey-scale as linear structures in front of the inner os 26, the diagnosis is considerably simpler by putting a flash of color Doppler (color or power) 27, over the cervix. Arterial flow but also venous flow can be recognized. Although some have obtained the diagnosis by perineal scan 28, a transvaginal image is clearly superior to an abdominal scan. Some have also advocated the use of 3D sonography 29. 3D sonography has an important role in the evaluation of vasa previa and other placental abnormalities, especially when the diagnosis is uncertain following 2D ultrasound. Some experts recommend that the use of 3D ultrasound be considered whenever a diagnosis of vasa previa is suspected on 2D sonography. In particular, 3D ultrasound may play a crucial role in mapping out the relationship of the placenta, vessels and internal cervical os, to obtain the best possible outcome at the time of Cesarean delivery.
Figure 3. Proposed diagnostic algorithm for the second-trimester detection of the vasa previa
Figure 4. Vasa previa ultrasound
Footnote: Multiplanar three‐dimensional (3D) transvaginal sonogram with color Doppler. (a) The sagittal view shows the vessels running in an anterior–superior sagittal plane over the cervix. The cervical canal is clearly demonstrated. The reference dot lies within the cervical canal. (b) Transverse cross‐section through the cervix, which in this view is a circular structure with the cervical canal in the center (arrows). The cervical glands are clearly demonstrated. The reference point can be seen within the cervical canal. (c) In a coronal view of the vasa previa and the cervix, the cervical canal can be seen as a straight line (arrows), and the vessel is seen as a large dot at the internal os. (d) 3D reconstruction of the cervix and vasa previa.
[Source 30 ]Vasa previa management
The outcome is markedly improved (97% survival versus 44%) when a prenatal diagnosis is followed by elective C-section is performed at 35 weeks or earlier if signs of labor or membrane rupture occurs 31. Some have advocate hospitalization from 30–32 weeks with corticosteroids to assist in promoting lung maturity when the cervix is not demonstrated to be long and closed 32. When time permits, an amniocentesis to assess lung maturity is justified 33.
Vasa previa prognosis
The major complication from vasa previa is the rupture of the vessels carrying fetal blood. This occurs at or near delivery if the condition is undetected. These results in a perinatal mortality of 56% 31 in undiagnosed cases, and 3% in those diagnosed prenatally 31. The median Apgar score (1 and 5 min) is 8 and 9 when detected prenatally versus only 1 and 4 for survivors of undetected cases 31. Further, transfusion is required in 58% of newborn without prenatal diagnosis, versus only 3% of those diagnosed prenatally 31. A less well quantified complication is the compression of the vasa previa by the presenting part resulting in decreased flow to the fetus and possibly hypoxia 34. Postnatal complications are related to either prematurity (due to early C-section with no confirmation of lung maturity) and include hyaline membrane disease, bronchopulmonary dysplasia, transient tachypnea, respiratory distress syndrome, or to partial exsanguination and complications related to anemia, hypovolemic shock 26 or complications of transfusions 35.
References- Derbala Y, Grochal F, Jeanty P. Vasa previa. J Prenat Med. 2007;1(1):2–13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309346
- Saghir S, Kouach J, Agadr A. A case report of vasa previa incidentally discovered. Pan Afr Med J. 2015;21:34. Published 2015 May 18. doi:10.11604/pamj.2015.21.34.6697 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4564431
- Oyelese KO, Turner MJ, Lees CC, Campbell S. Vasa previa: An avoidable obstetric tragedy. Obstet Gynecol Surv 1999; 54: 138–145.
- Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, Tovbin Y, Goldstein V, Smulian JC. Vasa previa: the impact of prenatal diagnosis on outcomes. Obstet Gynecol 2004; 103: 937–942.
- Lee W, Kirk JS, Comstock CH, Romero R. Vasa previa: prenatal detection by three‐dimensional ultrasonography. Ultrasound Obstet Gynecol 2000; 16: 384–387.
- Poor perinatal outcome associated with vasa previa: is it preventable? A report of three cases and review of the literature. Fung TY, Lau TK. Ultrasound Obstet Gynecol. 1998 Dec; 12(6):430-3.
- Catanzarite V, Maida C, Thomas W, Mendoza A, Stanco L, Piacquadio KM. Prenatal sonographic diagnosis of vasa previa: ultrasound findings and obstetric outcome in ten cases. Ultrasound Obstet Gynecol 2001; 17: 109–115
- Sepulveda W, Rojas I, Robert JA, Schnapp C, Alcalde JL. Prenatal detection of velamentous insertion of the umbilical cord: a prospective color Doppler ultrasound study. Ultrasound Obstet Gynecol 2003; 21: 564–569.
- Guidelines for the management of vasa previa. Gagnon R, DIAGNOSTIC IMAGING COMMITTEE., MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Aug; 31(8):748-753.
- Vasa previa: the impact of prenatal diagnosis on outcomes. Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, Tovbin Y, Goldstein V, Smulian JC. Obstet Gynecol. 2004 May; 103(5 Pt 1):937-42.
- Daly-Jones, Elizabeth & John, Ann & Leahy, Alison & Mckenna, Ciara & Sepulveda, Waldo. (2008). Vasa Praevia; a Preventable Tragedy. Ultrasound. 16. 10.1179/174313408X259508.
- Strassmann P. Placenta previa. Arch Gynecol. 1902;67:112.
- Three-dimensional sonographic diagnosis of vasa previa. Oyelese Y, Chavez MR, Yeo L, Giannina G, Kontopoulos EV, Smulian JC, Scorza WE. Ultrasound Obstet Gynecol. 2004 Aug; 24(2):211-5.
- Lee W, Kirk JS, Comstock CH, Romero R. Vasa previa: prenatal detection by three-dimensional ultrasonography. Ultrasound Obstet Gynecol. 2000 Sep;16(4):384–7
- Francois K, Mayer S, Harris C, Perlow JH. Association of vasa previa at delivery with a history of second-trimester placenta previa. J Reprod Med. 2003 Oct;48(10):771–4
- Raga F, Ballester MJ, Osborne NG, Bonilla-Musoles F. Role of color flow Doppler ultrasonography in diagnosing velamentous insertion of the umbilical cord and vasa previa. A report of two cases. J Reprod Med. 1995 Nov;40( 11):804–8
- Sepulveda W, Rojas I, Robert JA, Schnapp C, Alcalde JL. Prenatal detection of velamentous insertion of the umbilical cord: a prospective color Doppler ultrasound study. Ultrasound Obstet Gynecol. 2003 Jun;21(6):564–9
- Bernirschke K, Kaufmann P. Pathology of the human placenta. New York, NY: Springer-Verlag; 2000. pp. 353–359
- Toivonen S, Heinonen S, Anttila M, Kosma VM, Saarikoski S. Reproductive risk factors, Doppler findings, and outcome of affected births in placental abruption: a population-based analysis. Am J Perinatol. 2002 Nov;19(8):451–60
- Sauerbrei EE, Davies GL. Diagnosis of vasa previa with endovaginal color Doppler and power Doppler sonography: report of two cases. J Ultrasound Med. 1998 Jun;17( 6):393–8.
- Spellacy WN. Vasa previa, multiple pregnancies, and in vitro fertilization clarification. Fertil Steril. 2003 May;79( 5):1254–5
- Schachter M, Tovbin Y, Arieli S, Friedler S, Ron-El R, Sherman D. In vitro fertilization is a risk factor for vasa previa. Fertil Steril. 2002 Sep;78(3):642–3
- Odunsi K, Bullough CH, Henzel J, Polanska A. Evaluation of chemical tests for fetal bleeding from vasa previa. Int J Gynaecol Obstet. 1996 Dec;55(3):207–12
- Lindqvist PG, Gren P. An easy-to-use method for detecting fetal hemoglobin-A test to identify bleeding from vasa previa. Eur J Obstet Gynecol Reprod Biol. 2006;22
- Oyelese Y, Jha RC, Moxley MD, Collea JV, Queenan JT. Magnetic resonance imaging of vasa praevia. BJOG. 2003 Dec;110(12):1127–8
- Lee W, Lee VL, Kirk JS, Sloan CT, Smith RS, Comstock CH. Vasa previa: prenatal diagnosis, natural evolution, and clinical outcome. Obstet Gynecol. 2000 Apr;95(4):572–6
- Clerici G, Burnelli L, Lauro V, Pilu GL, Di Renzo GC. Prenatal diagnosis of vasa previa presenting as amniotic band. ’A not so innocent amniotic band’ Ultrasound Obstet Gynecol. 1996 Jan;7(1):61–3.
- Hertzberg BS, Kliewer MA. Vasa previa: prenatal diagnosis by transperineal sonography with Doppler evaluation. J Clin Ultrasound. 1998 Oct;26(8):405–8
- Araujo Junior E, Filho HA, Pires CR, Zanforlin Filho SM, Moron AF. Prenatal diagnosis of vasa previa through color Doppler and three-dimensional power Doppler ultrasonography. A case report. Clin Exp Obstet Gynecol. 2006;33( 2):122–4
- Oyelese, Y. , Chavez, M. R., Yeo, L. , Giannina, G. , Kontopoulos, E. V., Smulian, J. C. and Scorza, W. E. (2004), Three‐dimensional sonographic diagnosis of vasa previa. Ultrasound Obstet Gynecol, 24: 211-215. doi:10.1002/uog.1097
- Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, Tovbin Y, Goldstein V, Smulian JC. Vasa previa: the impact of prenatal diagnosis on outcomes. Obstet Gynecol. 2004 May;103(5 Pt 1):937–42
- Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol. 2006 Apr;107(4):927–41
- Canterino JC, Mondestin-Sorrentino M, Muench MV, Feld S, Baum JD, Fernandez CO. Vasa previa: prenatal diagnosis and evaluation with 3-dimensional sonography and power angiography. J Ultrasound Med. 2005 May;24(5):721–4
- Harding JA, Lewis DF, Major CA, Crade M, Patel J, Nageotte MP. Color flow Doppler–a useful instrument in the diagnosis of vasa previa. Am J Obstet Gynecol. 1990 Nov;163(5 Pt 1):1566–8
- Fung TY, Lau TK. Poor perinatal outcome associated with vasa previa: is it preventable? A report of three cases and review of the literature. Ultrasound Obstet Gynecol. 1998 Dec;12(6):430–3