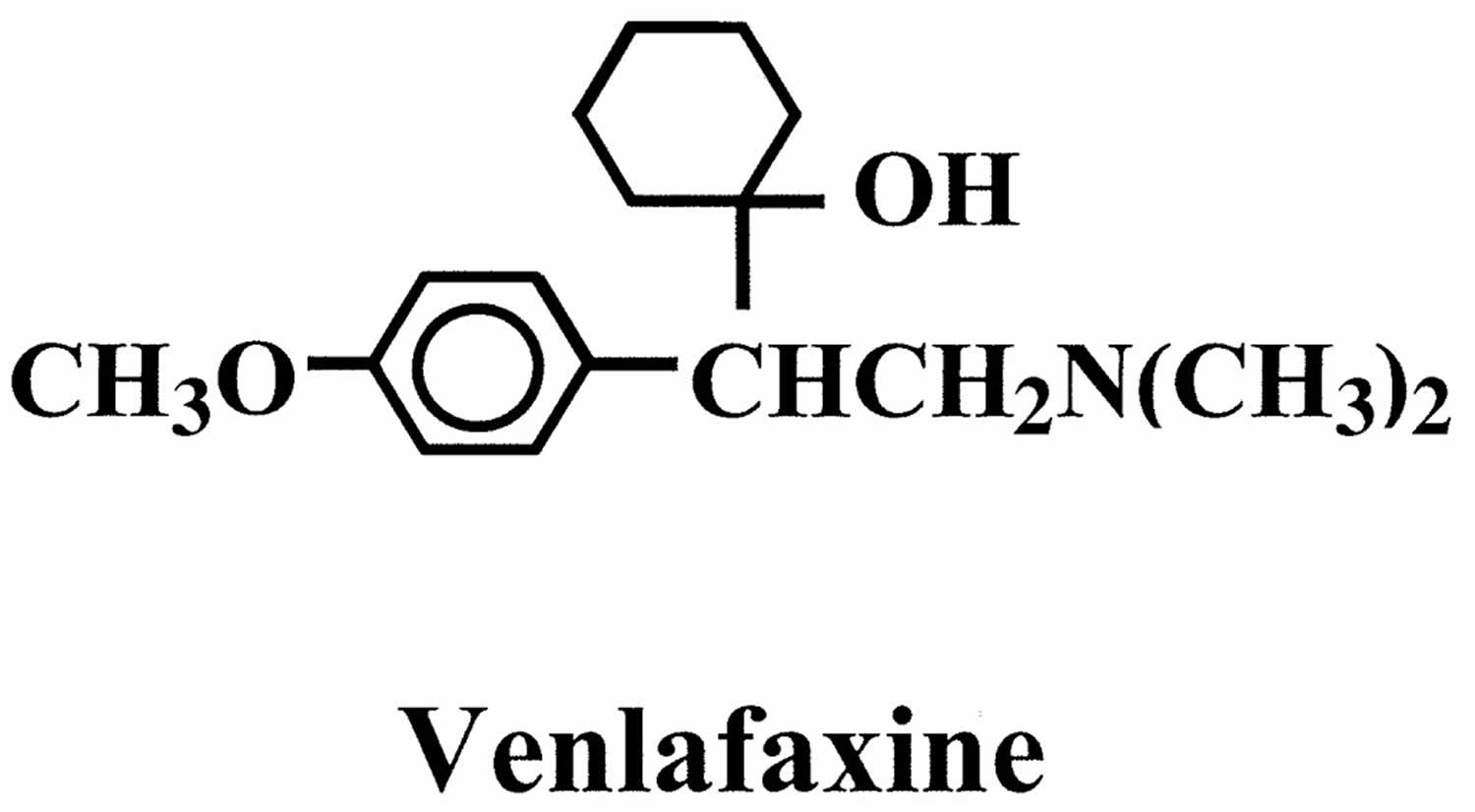
What is venlafaxine
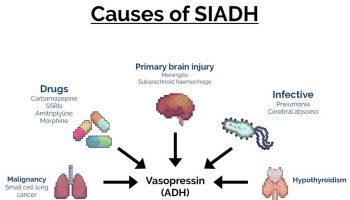
Venlafaxine is an antidepressant often used to treat depression, anxiety and panic attacks. Venlafaxine is in a class of medications called selective serotonin and norepinephrine reuptake inhibitors (SNRIs). Venlafaxine works by increasing the amounts of serotonin and norepinephrine, natural substances in the brain that help maintain mental balance.
Venlafaxine helps many people recover from depression, and has fewer unwanted effects than older antidepressants.
Venlafaxine comes as tablets and capsules which are available only on prescription.
The mechanism of the antidepressant action of venlafaxine in humans is believed to be associated with its potentiation of neurotransmitter activity in the CNS (central nervous system). Preclinical studies have shown that venlafaxine and its active metabolite, O-desmethylvenlafaxine, are potent inhibitors of neuronal serotonin and norepinephrine reuptake and weak inhibitors of dopamine reuptake. Venlafaxine and O-desmethylvenlafaxine have no significant affinity for muscarinic, histaminergic, or adrenergic receptors in vitro. Pharmacologic activity at these receptors is hypothesized to be associated with the various anticholinergic, sedative, and cardiovascular effects seen with other psychotropic drugs.
Key facts
- It usually takes 4 to 6 weeks for venlafaxine to work.
- Side effects such as feeling sick, headaches, sweating, and dry mouth are common. They are usually mild and go away after a couple of weeks.
- Venlafaxine can cause withdrawal symptoms. Don’t stop taking it without talking to your doctor.
- Venlafaxine has lots of different brand names including Effexor, Effexor XR and Efexor XL.
How and when to take venlafaxine
- Take venlafaxine once or twice a day as recommended by your doctor. It’s best to take venlafaxine with food so it doesn’t make you feel sick.
Suicidality and Antidepressant Drugs
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of Major Depressive Disorder and other psychiatric disorders. Anyone considering the use of Venlafaxine tablets or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Venlafaxine tablets are not approved for use in pediatric patients.
A small number of children, teenagers, and young adults (up to 24 years of age) who took antidepressants (‘mood elevators’) such as venlafaxine during clinical studies became suicidal (thinking about harming or killing oneself or planning or trying to do so). Children, teenagers, and young adults who take antidepressants to treat depression or other mental illnesses may be more likely to become suicidal than children, teenagers, and young adults who do not take antidepressants to treat these conditions. However, experts are not sure about how great this risk is and how much it should be considered in deciding whether a child or teenager should take an antidepressant. Children younger than 18 years of age should not normally take venlafaxine, but in some cases, a doctor may decide that venlafaxine is the best medication to treat a child’s condition.
You should know that your mental health may change in unexpected ways when you take venlafaxine or other antidepressants even if you are an adult over 24 years of age. You may become suicidal, especially at the beginning of your treatment and any time that your dose is increased or decreased. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: new or worsening depression; thinking about harming or killing yourself, or planning or trying to do so; extreme worry; agitation; panic attacks; difficulty falling asleep or staying asleep; aggressive behavior; irritability; acting without thinking; severe restlessness; and frenzied abnormal excitement. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Your healthcare provider will want to see you often while you are taking venlafaxine, especially at the beginning of your treatment. Be sure to keep all appointments for office visits with your doctor.
The doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with venlafaxine. Read the information carefully and ask your doctor or pharmacist if you have any questions. You also can obtain the Medication Guide from the FDA website: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm.
No matter your age, before you take an antidepressant, you, your parent, or your caregiver should talk to your doctor about the risks and benefits of treating your condition with an antidepressant or with other treatments. You should also talk about the risks and benefits of not treating your condition. You should know that having depression or another mental illness greatly increases the risk that you will become suicidal. This risk is higher if you or anyone in your family has or has ever had bipolar disorder (mood that changes from depressed to abnormally excited) or mania (frenzied, abnormally excited mood) or has thought about or attempted suicide. Talk to your doctor about your condition, symptoms, and personal and family medical history. You and your doctor will decide what type of treatment is right for you.
How does venlafaxine work?
Venlafaxine is one of a group of antidepressants called serotonin and noradrenaline reuptake inhibitors, or SNRIs. These medicines are thought to work by increasing the levels of mood-enhancing chemicals called serotonin and noradrenaline in the brain.
Is venlafaxine better than other antidepressants?
Venlafaxine isn’t any better or worse than other antidepressants. However, sometimes people respond better to one antidepressant than to another. If you aren’t feeling any better after 6 weeks, talk to your doctor.
Are there other treatments that will help?
Antidepressants, including venlafaxine, are just one of several approaches to treating depression. Other potential treatments include:
- talking therapy (such as cognitive behavioral therapy or CBT)
- exercise programmes
- help to get a good night’s sleep
Choosing a treatment that’s most suitable for you depends on how long you have had depression, your symptoms, whether you have had any previous bouts of depression, whether previous treatment has worked, how likely you are to stick with your treatment, the potential side effects and your preferences and priorities.
When will I feel better?
You may see an improvement in your symptoms after a week although it usually takes between 4 and 6 weeks before you feel the full benefits. That’s because it takes around a week for venlafaxine levels to build up in your body, and then a few weeks longer for your body to adapt and get used to it.
Don’t stop taking venlafaxine just because you feel it is not helping your symptoms. Give venlafaxine at least 6 weeks to work.
How will venlafaxine make me feel?
Antidepressants like venlafaxine help to jump start your mood so you feel better. You may notice that you sleep better and get on with people more easily because you’re less anxious. You will hopefully take in your stride little things that used to worry you.
Venlafaxine won’t change your personality or make you feel really happy. It will simply help you feel like yourself again.
Don’t expect to feel better overnight, though. Some people feel worse during the first few weeks of treatment before they begin to feel better.
Will I gain or lose weight?
Venlafaxine can make you feel less hungry than usual, so you may lose weight when you start taking it. Some people might find they gain weight.
If you start to have problems with your weight while taking venlafaxine, talk to your doctor or pharmacist.
How long will I take venlafaxine for?
Once you’re feeling better it’s likely that you will continue to take venlafaxine for several more months. Most doctors recommend that you take antidepressants for 6 months to 1 year after you no longer feel depressed. Stopping before that time can make depression come back.
Is it safe to take venlafaxine for a long time?
Venlafaxine is safe to take for a long time. There don’t seem to be any lasting harmful effects from taking it for many months and years.
However, taking venlafaxine for more than a year has been linked to a small increased risk of getting diabetes. But you will be regularly checked for this.
What will happen when I come off venlafaxine?
If you stop taking venlafaxine suddenly you may get unpleasant withdrawal symptoms. These include:
- dizziness
- feeling sick
- numbness or tingling in the hands or feet
- trouble sleeping
- feeling agitated or anxious
- headaches
- shaking
Withdrawal symptoms are usually harmless and over within a few days but it’s possible to prevent them by reducing the dose gradually when you stop taking this medicine.
Don’t stop taking venlafaxine unless your doctor tells you to.
Will venlafaxine affect my sex life?
The good effects of venlafaxine may, after a while, improve your sex life as your mood lifts and you become interested in life and relationships again.
Some of the possible negative effects include:
- men might have problems with getting an erection, or with ejaculating
- women might have some vaginal bleeding
- both men and women might find they don’t reach orgasm the same way as before
- you may have a lower sex drive
Any mild sexual side effects might pass after the first couple of weeks. If they don’t, and this a problem for you, go back to your doctor to see if there’s an alternative antidepressant for you to try.
Will venlafaxine affect my contraception?
For women, venlafaxine will not affect contraceptive pills or the morning after pill.
Is there any food or drink I need to avoid?
You can eat and drink normally while taking venlafaxine.
Can I drink alcohol with venlafaxine?
You can drink alcohol while taking venlafaxine but it may make you feel sleepy. It might be best to stop drinking alcohol during the first few days of treatment until you see how this medicine affects you.
Can I drive or ride a bike?
Some people can’t concentrate properly while they’re taking venlafaxine. It might be best to stop driving and cycling for the first few days of treatment until you know how this medicine makes you feel.
Will recreational drugs affect venlafaxine?
The sleep-inducing effects of cannabis can add to those of venlafaxine, especially in people who have just started taking it. Cannabis and venlafaxine can also give you a fast heartbeat.
Methadone can make sleepiness worse with venlafaxine.
It can be potentially dangerous to take venlafaxine with:
- stimulants like MDMA (ecstasy) or cocaine
- hallucinogens like LSD
- novel psychoactive substances (which used to be known as legal highs) like mephedrone
Venlafaxine has not been properly tested with recreational drugs. Talk to your doctor if you think you might take any while taking venlafaxine.
How should venlafaxine be used?
Venlafaxine comes as a tablet or extended-release capsule to take by mouth. The tablet is usually taken two or three times a day with food. The extended-release capsule is usually taken once daily in the morning or evening with food. Take venlafaxine at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take venlafaxine exactly as directed. Do not take more or less of it or take it more often or for a longer period of time than prescribed by your doctor.
Swallow the extended-release capsule whole; do not split, chew, or crush it, or place it in water. If you cannot swallow the extended-release capsule, you may carefully open the capsule and sprinkle the entire contents on a spoonful of applesauce. Swallow (without chewing) this mixture immediately after preparation and then drink a glass of water to make sure that you have swallowed all of the medication.
Your doctor will probably start you on a low dose of venlafaxine and gradually increase your dose, not more often than once every 4 to 7 days. Tell your doctor how you are feeling during your treatment so that your doctor can adjust your dose properly.
Venlafaxine controls depression but does not cure it. It may take 6 to 8 weeks or longer for you to feel the full benefit of this medication. Continue to take venlafaxine even if you feel well. Do not stop taking venlafaxine without talking to your doctor. Your doctor will probably decrease your dose gradually. If you suddenly stop taking venlafaxine, you may experience withdrawal symptoms such as agitation; anxiety; confusion; sad mood; irritability; frenzied or abnormal excitement; lack of coordination; trouble falling asleep or staying asleep; nightmares; nausea; vomiting; loss of appetite; diarrhea; dry mouth; sweating; ringing in the ears; seizures; or burning, tingling, numbness, or electric shock-like feelings in any part of the body. Tell your doctor if you experience any of these symptoms while you are decreasing your dose of venlafaxine or soon after you stop taking venlafaxine.
Who can and can’t take venlafaxine
Venlafaxine can be taken by adults for depression, anxiety and panic attacks.
Check with your doctor before starting to take venlafaxine if you:
- have had an allergic reaction to venlafaxine or any other medicines in the past
- have a heart problem – as venlafaxine can speed up or change your heartbeat
- are trying to become pregnant, are already pregnant or you are breastfeeding
- have an eye problem called glaucoma because venlafaxine can increase the pressure in your eye
If you have diabetes, venlafaxine can make it more difficult to keep your blood sugar stable. Monitor your blood sugar more often for the first few weeks of treatment with venlafaxine and adjust your diabetes treatment if necessary.
Pregnancy and breastfeeding
It’s important for you and your baby that you stay well during your pregnancy. If you become pregnant while taking venlafaxine speak to your doctor. Do not stop taking your medicine unless your doctor tells you to.
Venlafaxine has been linked to a very small increased risk of problems for your unborn baby. However if your depression is not treated during pregnancy this can also increase the chance of problems.
You may need to take venlafaxine during pregnancy if you need it to remain well. Your doctor can explain the risks and the benefits, and will help you decide which treatment is best for you and your baby.
Can taking venlafaxine during my pregnancy cause birth defects in my baby?
Studies have looked at nearly 700 babies born to women who took venlafaxine during early pregnancy or throughout the first trimester. These studies suggest that using venlafaxine during pregnancy is unlikely to increase the chance of birth defects above the 3-5% background population risk.
Should I stop taking venlafaxine during the pregnancy or wean off it before the third trimester?
It is important to talk about the risks and benefits of taking venlafaxine during pregnancy with your healthcare providers. Studies have shown that when depression is left untreated during pregnancy, there may be increased risks for miscarriage, preeclampsia (dangerous rise in maternal blood pressure), preterm delivery, low birth weight, postpartum mood disorders and other harmful effects. For some women the effects of stopping venlafaxine may be more harmful than the possible risks to the baby from staying on venlafaxine. If you’re thinking about stopping venlafaxine before or during pregnancy, you should wean off slowly over time with the help of your healthcare provider.
Does taking venlafaxine during my pregnancy increase my chance of premature birth?
One study found that women taking venlafaxine were more likely to deliver prematurely, but other studies have not found venlafaxine to increase the chance for prematurity. Depression itself may increase the chance for preterm birth, which makes it difficult to find out whether the medications used to treat depression can also cause prematurity.
I am taking venlafaxine, but would like to stop using it before becoming pregnant. How long does venlafaxine stay in my body?
Individuals break down medicines at different rates. On average, it is thought to take around two days for most of venlafaxine to be gone from the body. You should always speak with your healthcare provider before making any changes in your medication.
Women who suddenly stop taking their antidepressants are at risk for withdrawal. Symptoms include dizziness, stomach upset, and nervousness or anxiety. If a woman plans to stop taking her venlafaxine, it is recommended that this be done slowly over time.
Can taking venlafaxine during my pregnancy increase the chance for miscarriage?
One study found that women taking venlafaxine were more likely to miscarry, but other studies have not found venlafaxine to increase the chance for miscarriage. Depression itself may increase the chance for miscarriage, which makes it difficult to find out whether the medications used to treat depression can also cause miscarriage.
I need to take venlafaxine throughout my entire pregnancy. Will it cause withdrawal symptoms in my baby?
Possibly. If you are taking venlafaxine at the time of delivery, your baby may have jitteriness, increased muscle tone, irritability, changes in sleep patterns, tremors (seizure like activity), difficulty eating and some problems with breathing. Symptoms usually start by day 4. Some babies may need to stay in the hospital for several days. However, most of the time these effects are mild and go away on their own. They usually go away within 2 to 21 days. A small number of follow-up data have not found that babies with these symptoms will have ongoing health problems. Not all babies exposed to venlafaxine will have these symptoms.
Will taking venlafaxine during my pregnancy have any long-term effect on my baby’s behavior and development?
Right now there is no evidence that taking venlafaxine during pregnancy causes changes in the baby’s behavior or intellect. Several studies found no difference in IQ scores between children whose mothers took venlafaxine when compared to mothers taking other antidepressants or who had maternal depression. No meaningful difference in children’s IQ was seen in mothers who took venlafaxine when compared to mothers without depression. More longterm studies are needed to determine if venlafaxine has any effects on a child’s learning or behavior.
Venlafaxine and breastfeeding
If your doctor or health visitor says your baby is healthy, venlafaxine can be used during breastfeeding. It has been used by many breastfeeding mothers usually without any problems.
Venlafaxine and its breakdown products pass into breast milk in small amounts. It has been linked with side effects in very few breastfed babies.
Most of the reports about taking venlafaxine when breastfeeding have not found harmful effects in the infants. Long term studies on children older than two years have not been done. Because the amount of medication in the breast milk can vary, infants can be watched for unusual sleepiness and monitored for good weight gain. If there is a concern, infant blood levels can be taken. Be sure to talk to your healthcare provider about all of your breastfeeding questions.
It’s important to continue taking venlafaxine to keep you well. Breastfeeding will also benefit both you and your baby.
If you notice that your baby isn’t feeding as well as usual, or seems unusually sleepy, or if you have any other concerns about your baby, then talk to your health visitor or doctor.
Venlafaxine special precautions
Before taking venlafaxine:
- tell your doctor and pharmacist if you are allergic to venlafaxine, any other medications, or any of the ingredients in venlafaxine tablets or extended-release capsules. Ask your pharmacist for a list of the ingredients.
- tell your doctor if you are taking a monoamine oxidase (MAO) inhibitor, such as isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate), or if you have stopped taking one of these medications within the past 14 days. Your doctor will probably tell you that you should not take venlafaxine. If you stop taking venlafaxine, your doctor will tell you that you should wait at least 7 days before you start to take an MAO inhibitor.
- tell your doctor and pharmacist what other prescription and nonprescription medications, and vitamins you are taking or plan to take. Be sure to mention any of the following: anticoagulants (‘blood thinners’) such as warfarin (Coumadin); amiodarone (Cordarone, Pacerone); other antidepressants; cimetidine (Tagamet); clozapine (Clozaril); diuretics (‘water pills’); duloxetine (Cymbalta); haloperidol (Haldol); imipramine (Tofranil); indinavir (Crixivan); ketoconazole (Nizoral); linezolid (Zyvox); lithium; medications for anxiety, mental illness, pain, seizures, or weight loss; medications for migraine such as almotriptan (Axert), eletriptan (Relpax), frovatriptan (Frova), naratriptan (Amerge), rizatriptan (Maxalt), sumatriptan (Imitrex), and zolmitriptan (Zomig); methadone (Dolophine); methylene blue; phentermine (Adipex P, Ionamin); ritonavir (Norvir); sedatives; selective serotonin reuptake inhibitors (SSRIs) such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft); sibutramine (Meridia); sleeping pills; tramadol (Ultram); and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what nutritional supplements and herbal products you are taking, especially St. John’s wort and tryptophan.
- tell your doctor if you have ever used illegal drugs or overused prescription medications. Also tell your doctor if you have recently had a heart attack and if you have or have ever had high blood pressure, high blood cholesterol seizures, or heart, kidney, liver, or thyroid disease.
- tell your doctor if you are pregnant, especially if you are in the last few months of your pregnancy, or if you plan to become pregnant or are breast-feeding. If you become pregnant while taking venlafaxine, call your doctor. Venlafaxine may cause problems in newborns following delivery if it is taken during the last months of pregnancy.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking venlafaxine.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by this medication.
- you should know that venlafaxine may cause angle-closure glaucoma (a condition where the fluid is suddenly blocked and unable to flow out of the eye causing a quick, severe increase in eye pressure which may lead to a loss of vision). Talk to your doctor about having an eye examination before you start taking this medication. If you have nausea, eye pain, changes in vision, such as seeing colored rings around lights, and swelling or redness in or around the eye, call your doctor or get emergency medical treatment right away.
Cautions with other medicines
Some medicines and venlafaxine can interfere with each other and increase the chances of you having side effects.
Tell your doctor if you’re taking these medicines before you start venlafaxine:
- any medicines that affect your heartbeat – as venlafaxine can speed up or change your heartbeat
- any other medicines for depression. Some rarely used antidepressants can interact with venlafaxine to cause very high blood pressure even when they have been stopped for a few weeks.
Mixing venlafaxine with herbal remedies and supplements
Don’t take the herbal remedy for depression, St John’s wort, while you are being treated with venlafaxine as it will increase your risk of side effects.
Tell your doctor or pharmacist if you are taking any other medicines, including herbal remedies, vitamins or supplements.
What is venlafaxine used for?
Venlafaxine is used to treat depression and it is also sometimes used to treat anxiety and panic attacks. Venlafaxine extended-release (long-acting) capsules are also used to treat generalized anxiety disorder (GAD; excessive worrying that is difficult to control), social anxiety disorder (extreme fear of interacting with others or performing in front of others that interferes with normal life), and panic disorder (sudden, unexpected attacks of extreme fear and worry about these attacks).
Venlafaxine is also sometimes used to treat hot flashes (hot flushes; sudden strong feelings of heat and sweating) in women who have experienced menopause (‘change of life’; the end of monthly menstrual periods) or who are taking medication to treat breast cancer. Talk to your doctor or pharmacist about the risks of using venlafaxine to treat your condition.
Venlafaxine has also been used for ADHD, binge eating disorder, bipolar disorder, diabetic neuropathy, obsessive-compulsive disorder, posttraumatic stress disorder (PTSD), premenstrual dysphoric disorder, and tension-type headaches.
This medication is sometimes prescribed for other uses; ask your doctor or pharmacist for more information.
Venlafaxine dosage
The usual starting dose of venlafaxine is 75mg a day. This might be gradually increased to a maximum dose of 375mg.
If you have problems with your liver or kidneys your doctor might prescribe a lower dose.
Venlafaxine tablets and capsules can be either immediate release or extended release. How you take them depends on the type you’ve been prescribed.
Immediate release tablets release the venlafaxine into your system as soon as you swallow them. You will usually take 37.5mg immediate release tablets twice a day, once in the morning and once in the evening.
Extended release tablets and capsules are released into your system gradually. You will usually take 75mg extended release tablets or capsules once a day. You can choose to take them at any time as long as you stick to the same time every day. If you have trouble sleeping, it’s best to take it in the morning.
Dose adjustments for discontinuation: A gradual reduction in the dose is recommended whenever possible. In clinical studies, tapering was achieved by reducing the daily dose by 75 mg at one-week intervals.
Adult Dose for Depression
Use: Treatment of major depressive disorder
Immediate release:
- Initial dose: 37.5 mg orally twice a day or 25 mg orally 3 times a day
- Maintenance dose: May increase in daily increments of up to 75 mg orally at intervals of no less than 4 days
- Maximum dose: (moderately depressed outpatients): 225 mg orally per day
- Maximum dose (severely depressed inpatients): 375 mg orally per day
Comments:
- Daily dosage may be divided in 2 or 3 doses/day
Extended release:
- Initial dose: 75 mg orally once a day
- Maintenance dose: May increase in daily increments of up to 75 mg orally at intervals of no less than 4 days
- Maximum dose (moderately depressed outpatients): 225 mg orally per day
- Maximum dose (severely depressed inpatients): 375 mg orally per day
Adult Dose for Anxiety
Uses:
- Treatment of Generalized Anxiety Disorder (GAD)
- Treatment of Social Anxiety Disorder
Extended release:
- Initial dose: 75 mg orally once a day
- Maintenance dose: May increase in daily increments of 75 mg orally at intervals of no less than 4 days
- Maximum dose: 225 mg orally per day
Adult Dose for Panic Disorder
Use: Treatment of Panic Disorder, with or without agoraphobia
Extended release:
- Initial dose: 37.5 mg orally once a day
- Maintenance dose: May increase dose in daily increments of 75 mg orally at intervals of no less than 7 days
- Maximum dose: 225 mg orally per day
Renal Dose Adjustments
- Mild to moderate renal impairment (creatinine clearance 30 to 89 mL/min): Dosage should be reduced by 25% to 50%
Liver Dose Adjustments
- Mild to moderate hepatic impairment: Dosage should be reduced 50%.
- Cirrhosis: Dosage should be reduced by at least 50%.
What should I do if I forget a dose?
If you occasionally forget to take a dose, don’t worry. Take your next dose at the usual time. Never take 2 doses at the same time to make up for a forgotten one.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
Ask your doctor for advice straight away. An overdose can lead to potentially serious symptoms such as:
- feeling sleepy
- vomiting
- a racing heart
- seizures
Venlafaxine side effects
Like all medicines, venlafaxine can cause side effects in some people, but many people have no side effects or only minor ones. Some of the common side effects of venlafaxine will gradually improve as your body gets used to it.
Common side effects
These side effects happen in more than 1 in 100 people. Keep taking the medicine, but tell your doctor or pharmacist if these side effects bother you or don’t go away:
- feeling sick
- headaches
- sweating
- dry mouth
- trouble sleeping
- dizziness
- feeling sleepy
- constipation
Call your doctor if any of the following symptoms are severe or do not go away:
- drowsiness
- weakness or tiredness
- dizziness
- headache
- nightmares
- nausea
- vomiting
- stomach pain
- constipation
- diarrhea
- gas
- heartburn
- burping
- dry mouth
- change in ability to taste food
- loss of appetite
- weight loss
- uncontrollable shaking of a part of the body
- pain, burning, numbness, or tingling in part of the body
- muscle tightness
- twitching
- yawning
- sweating
- hot flashes or flushing
- frequent urination
- difficulty urinating
- sore throat, chills, or other signs of infection
- ringing in the ears
- changes in sexual desire or ability
- enlarged pupils (black circles in the middle of the eyes)
Some side effects can be serious.
Serious side effects happen uncommonly (in less than 1 in 100 people), but some people may have serious side effects when taking venlafaxine.
Tell a doctor straight away if you develop:
- headaches, trouble focusing, memory problems, not thinking clearly, weakness, seizures, or losing your balance – these can be signs of low sodium levels
- thoughts about harming yourself or ending your life
- chest pain or pressure, shortness of breath, or a fast or irregular heart beat
- severe dizziness or passing out
- feelings of euphoria, excessive enthusiasm or excitement, or a feeling of restlessness that means you can’t sit or stand still
- unexplained muscle pain or weakness
- yellow skin or eyes – this can be a sign of liver problems
- any changes in your eyesight, like blurred vision or dilated pupils
- putting on or losing weight without trying to
- changes in your periods such as heavy bleeding, spotting, or bleeding between periods
Or, if you get any signs of abnormal bleeding including:
- vomiting blood or dark vomit, coughing up blood, blood in your pee, black or red poo – these can be signs of bleeding from the gut
- bleeding from the gums or bruises that appear without a reason or that get bigger
- any bleeding that is very bad or that you cannot stop
Serious allergic reaction
In rare cases, it’s possible to have a serious allergic reaction to venlafaxine. A serious allergic reaction is an emergency. Contact a doctor straight away if you think you or someone around you is having a serious allergic reaction.
The warning signs of a serious allergic reaction are:
- getting a skin rash that may include itchy, red, swollen, blistered or peeling skin
- wheezing
- tightness in the chest or throat
- having trouble breathing or talking
- swelling of the mouth, face, lips, tongue, or throat
If you experience any of the following symptoms or those listed in the IMPORTANT WARNING or SPECIAL PRECAUTIONS sections, call your doctor immediately:
- rash
- hives
- itching
- difficulty breathing or swallowing
- chest pain
- fast, pounding, or irregular heartbeat
- seizures
- unusual bruising or bleeding
- small purple spots on the skin
- eye pain or redness
- fever, sweating, confusion, fast or irregular heartbeat, and severe muscle stiffness
- fever
- problems with coordination
- hallucinations (seeing things or hearing voices that do not exist)
- coma (loss of consciousness for a period of time)
Venlafaxine may slow growth and weight gain in children. If your child is taking venlafaxine, your child’s doctor will watch your child’s growth carefully. Talk to your child’s doctor about the risks of giving venlafaxine to your child.
These are not all the side effects of venlafaxine. For a full list see the leaflet inside your medicines packet. Call your doctor if you have any unusual problems while you are taking venlafaxine.
How to cope with side effects
What to do about:
- feeling sick – try taking venlafaxine with or after food. It may also help if you avoid rich or spicy food.
- headaches – make sure you rest and drink plenty of fluids. Don’t drink too much alcohol. Ask your pharmacist to recommend a painkiller. Headaches should usually go away after the first week of taking venlafaxine. Talk to your doctor if they last longer than a week or are severe.
- a dry mouth – chew sugar-free gum or sugar-free sweets
- dizziness – if venlafaxine makes you feel dizzy, stop what you’re doing and sit or lie down until you feel better
- feeling sleepy – cut down the amount of alcohol you drink
- being unable to sleep – take venlafaxine first thing in the morning
- constipation – eat more high-fibre foods such as fresh fruit and vegetables and cereals, and drink plenty of water. Try to exercise more regularly, for example, by going for a daily walk or run. If this doesn’t help, talk to your pharmacist or doctor.
You can reduce the chance of having a side effect that bothers you if you take venlafaxine in the evening. That way you’re asleep when the level of medicine in your body is highest.
Venlafaxine withdrawal
Dizziness (33.3%), vivid dreams (26.4%), fatigue (22.2%), vertigo (5.6%), rapid changing mood (6.9%), and tachycardia (4.2%) were the most frequently reported symptoms 1. Tint et al. 2 randomized 28 patients treated with different selective serotonin reuptake inhibitor (SSRI) or venlafaxine to a short (3 days) or long (14 days) taper. Results showed that 46% of subjects reported discontinuation symptoms and that the incidence was similar in both conditions (47 vs. 46% in the short vs. long taper groups). When escitalopram was compared to venlafaxine XR in major depressive disorder patients, significantly more venlafaxine-treated patients than escitalopram-treated ones reported a Discontinuation Emergent Signs and Symptoms score >4 in a 1-week runout period 3. Increased dreaming, trouble sleeping, nervousness or anxiety, irritability, and sudden worsening of mood occurred with an incidence >10% in the escitalopram group.
The pathophysiological mechanisms of withdrawal phenomena are still hypothetical and in need of proper neurobiological investigations 4. A number of mechanisms have been suggested: a decrease in serotonin availability when treatment ends 5, a behavioral stress response that is associated with increased hippocampal N-methyl-D-aspartate (NMDA) receptor density 6, and genetic vulnerabilities 7. Animal studies concerned with the long-term use of antidepressant drug have limited implications, since clear discontinuation-like behaviors in animal models are not available 8. Fava and Offidani 9 have interpreted the withdrawal phenomena according to the oppositional model of tolerance. Continued drug treatment may recruit processes that oppose the initial acute effects of a drug and may lead to a loss of efficacy and/or to a treatment-unresponsive course. When drug treatment ends, oppositional processes may operate for some time, resulting in the appearance of withdrawal symptoms and/or an increased vulnerability to relapse and/or resistance to treatment (if it is reinstituted) and/or switching to a bipolar course 9. The appearance of withdrawal symptoms after SSRI discontinuation may thus be potentially related to a number of important clinical phenomena 10.
Venlafaxine overdose
There were 14 reports of acute overdose with Venlafaxine tablets, either alone or in combination with other drugs and/or alcohol, among the patients included in the premarketing evaluation. The majority of the reports involved ingestions in which the total dose of Venlafaxine tablets taken was estimated to be no more than several-fold higher than the usual therapeutic dose. The 3 patients who took the highest doses were estimated to have ingested approximately 6.75 g, 2.75 g, and 2.5 g. The resultant peak plasma levels of Venlafaxine for the latter 2 patients were 6.24 and 2.35 ⛤g/mL, respectively, and the peak plasma levels of O-desmethylVenlafaxine were 3.37 and 1.30 ⛤g/mL, respectively. Plasma Venlafaxine levels were not obtained for the patient who ingested 6.75 g of Venlafaxine. All 14 patients recovered without sequelae. Most patients reported no symptoms. Among the remaining patients, somnolence was the most commonly reported symptom. The patient who ingested 2.75 g of Venlafaxine was observed to have 2 generalized convulsions and a prolongation of QTc to 500 msec, compared with 405 msec at baseline. Mild sinus tachycardia was reported in 2 of the other patients.
Symptoms of overdose may include:
- dizziness
- nausea
- vomiting
- burning, tingling, or numbness of the hands and feet
- increased size of the pupil (black center of the eye)
- muscle pain
- hot and cold spells
- sleepiness
- seizures
- fast, slow, or irregular heartbeat
- coma (loss of consciousness for a period of time).
In postmarketing experience, overdose with Venlafaxine has occurred predominantly in combination with alcohol and/or other drugs. The most commonly reported events in over dosage include tachycardia, changes in level of consciousness (ranging from somnolence to coma), mydriasis, seizures, and vomiting. Electrocardiogram changes (eg, prolongation of QT interval, bundle branch block, QRS prolongation), ventricular tachycardia, bradycardia, hypotension, rhabdomyolysis, vertigo, liver necrosis, serotonin syndrome, and death have been reported.
Published retrospective studies report that Venlafaxine overdosage may be associated with an increased risk of fatal outcomes compared to that observed with SSRI antidepressant products, but lower than that for tricyclic antidepressants. Epidemiological studies have shown that Venlafaxine-treated patients have a higher pre-existing burden of suicide risk factors than SSRI-treated patients. The extent to which the finding of an increased risk of fatal outcomes can be attributed to the toxicity of Venlafaxine in over dosage as opposed to some characteristic(s) of Venlafaxine-treated patients is not clear. Prescriptions for Venlafaxine tablets should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Management of venlafaxine overdosage
Treatment should consist of those general measures employed in the management of over dosage with any antidepressant.
Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. General supportive and symptomatic measures are also recommended. Induction of emesis is not recommended. Gastric lavage with a large-bore orogastric tube with appropriate airway protection, if needed, may be indicated if performed soon after ingestion or in symptomatic patients. Activated charcoal should be administered. Due to the large volume of distribution of this drug, forced diuresis, dialysis, hemoperfusion and exchange transfusion are unlikely to be of benefit. No specific antidotes for Venlafaxine are known.
In managing overdosage, consider the possibility of multiple drug involvement. The physician should consider contacting a poison control center for additional information on the treatment of any overdose.
- Sir A, D’Souza RF, Uguz S, George T, Vahip S, Hopwood M, Martin AJ, Lam W, Burt T: Randomized trial of sertraline versus venlafaxine XR in major depression: efficacy and discontinuation symptoms. J Clin Psychiatry 2005;66:1312-1320.[↩]
- Tint A, Haddad P, Anderson I: The effect of rate of antidepressant tapering on the incidence of discontinuation symptoms: a randomized study. J Psychopharmacol 2008;22:330-332.[↩]
- Montgomery S, Huusom A, Bothmer J: A randomised study comparing escitalopram with venlafaxine XR patients in primary care with major depressive disorder. Neuropsychobiology 2004;50:57-64.[↩]
- Withdrawal Symptoms after Selective Serotonin Reuptake Inhibitor Discontinuation: A Systematic Review. Psychother Psychosom 2015;84:72-81 https://doi.org/10.1159/000370338[↩]
- Blier P, Tremblay P: Physiologic mechanisms underlying the antidepressant discontinuation syndrome. J Clin Psychiatry 2006;67:8-13.[↩]
- Harvey BH, McEwen BS, Stein DJ: Neurobiology of antidepressant withdrawal: implications for longitudinal outcome of depression. Biol Psychiatry 2003;54:1105-1117.[↩]
- Murata Y, Kobayashi D, Imuta N, Haraguchi K, Ieiri I, Nishimura R, Koyama S, Mine K: Effects of serotonin 1A, 2A, 2C, 3A and 3B and serotonin transporter gene polymorphisms on the occurrence of paroxetine discontinuation syndrome. J Clin Psychopharmacol 2010;30:11-17.[↩]
- Renoir T: Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Front Pharmacol 2013;4:1-10.[↩]
- Fava GA, Offidani E: The mechanisms of tolerance in antidepressant action. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:1593-1602.[↩][↩]
- Fava GA: Rational use of antidepressant drugs. Psychother Psychosom 2014;83:197-204.[↩]