von Gierke disease
von Gierke disease also known as glycogen storage disease type 1 or glucose-6-phosphate deficiency, is an inherited disorder caused by the buildup of a complex sugar called glycogen in the body’s cells. The accumulation of glycogen in certain organs and tissues, especially the liver, kidneys, and small intestines, impairs their ability to function normally.
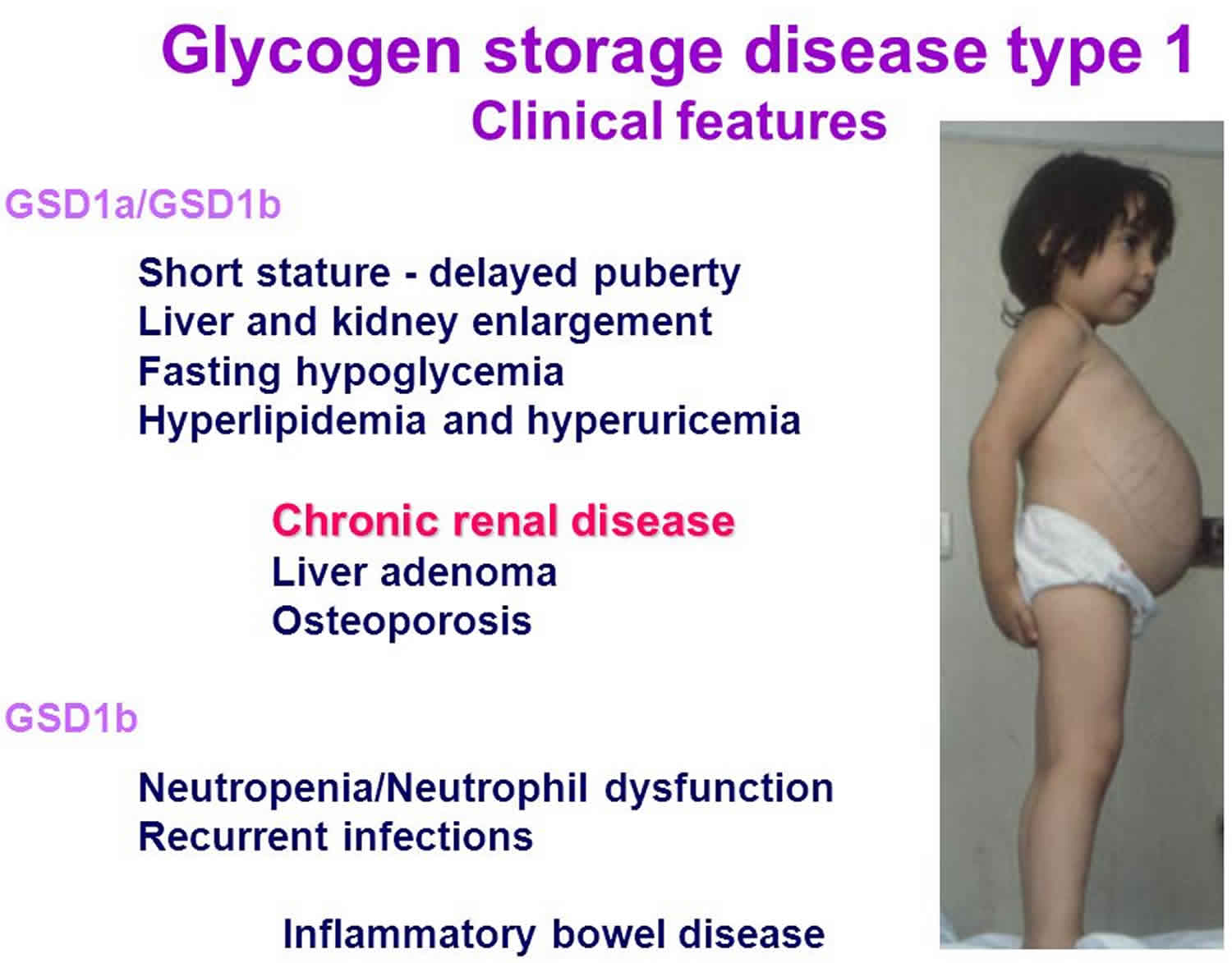
Signs and symptoms of von Gierke disease typically appear around the age of 3 or 4 months, when babies start to sleep through the night and do not eat as frequently as newborns. Affected infants may have low blood sugar (hypoglycemia), which can lead to seizures. They can also have a buildup of lactic acid in the body (lactic acidosis), high blood levels of a waste product called uric acid (hyperuricemia), and excess amounts of fats in the blood (hyperlipidemia). As they get older, children with von Gierke disease have thin arms and legs and short stature. An enlarged liver may give the appearance of a protruding abdomen. The kidneys may also be enlarged. Affected individuals may also have diarrhea and deposits of cholesterol in the skin (xanthomas).
People with von Gierke disease may experience delayed puberty. Beginning in young to mid-adulthood, affected individuals may have thinning of the bones (osteoporosis), a form of arthritis resulting from uric acid crystals in the joints (gout), kidney disease, and high blood pressure in the blood vessels that supply the lungs (pulmonary hypertension). Females with this condition may also have abnormal development of the ovaries (polycystic ovaries). In affected teens and adults, tumors called adenomas may form in the liver. Adenomas are usually noncancerous (benign), but occasionally these tumors can become cancerous (malignant).
Researchers have described two types of von Gierke disease, which differ in their signs and symptoms and genetic cause. These types are known as glycogen storage disease type 1a (GSD1a) and glycogen storage disease type 1b (GSD1b). Two other forms of von Gierke disease have been described, and they were originally named types 1c and 1d. However, these types are now known to be variations of glycogen storage disease type 1b (GSD1b); for this reason, GSD1b is sometimes called GSD type 1 non-a.
he two major subtypes of glycogen storage disease type 1 are:
- Glycogen storage disease type 1a (GSD1a), caused by the deficiency of glucose-6-phosphatase (G6Pase) catalytic activity;
- Glycogen storage disease type 1b (GSD1b), caused by a defect in glucose-6-phosphate exchanger SLC37A4 (transporter).
Many people with glycogen storage disease type1b (GSD1b) have a shortage of white blood cells (neutropenia), which can make them prone to recurrent bacterial infections. Neutropenia is usually apparent by age 1. Many affected individuals also have inflammation of the intestinal walls (inflammatory bowel disease). People with glycogen storage disease type 1b may have oral problems including cavities, inflammation of the gums (gingivitis), chronic gum (periodontal) disease, abnormal tooth development, and open sores (ulcers) in the mouth. The neutropenia and oral problems are specific to people with glycogen storage disease type 1b and are typically not seen in people with glycogen storage disease type 1a.
The overall incidence of von Gierke disease is 1 in 100,000 individuals 1. The prevalence of von Gierke disease in Ashkenazi Jews is approximately 1 in 20,000. This condition affects males and females in equal numbers in any given population group. Glycogen storage disease type1a is more common than glycogen storage disease type1b, accounting for 80 percent of all von Gierke disease cases.
The goal of treatment is to avoid low blood sugar. Eat frequently during the day, especially foods that contain carbohydrates (starches). Older children and adults may take cornstarch by mouth to increase their carbohydrate intake.
In some children, a feeding tube is placed through their nose into the stomach throughout the night to provide sugars or uncooked cornstarch. The tube can be taken out each morning. Alternatively, a gastrostomy tube (G-tube) can be placed to deliver food directly to the stomach overnight.
A medicine to lower uric acid in the blood and decrease the risk for gout may be prescribed. Your doctor may also prescribe medicines to treat kidney disease, high lipids, and to increase the cells that fight infection.
People with von Gierke disease cannot properly break down fruit or milk sugar. It is best to avoid these products.
von Gierke disease cause
Mutations in two genes, G6PC and SLC37A4, cause von Gierke disease. G6PC gene mutations cause glycogen storage disease type 1a, and SLC37A4 gene mutations cause glycogen storage disease type 1b.
The proteins produced from the G6PC and SLC37A4 genes work together to break down a type of sugar molecule called glucose 6-phosphate. The breakdown of this molecule produces the simple sugar glucose, which is the primary energy source for most cells in the body.
Mutations in the G6PC and SLC37A4 genes prevent the effective breakdown of glucose 6-phosphate. Glucose 6-phosphate that is not broken down to glucose is converted to glycogen and fat so it can be stored within cells. Too much glycogen and fat stored within a cell can be toxic. This buildup damages organs and tissues throughout the body, particularly the liver and kidneys, leading to the signs and symptoms of von Gierke disease.
von Gierke disease inheritance pattern
von Gierke disease is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 1 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 1. von Gierke disease autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
von Gierke disease symptoms
The primary symptom of von Gierke disease in infancy is a low blood sugar level (hypoglycemia). Symptoms of von Gierke disease usually begin at three to four months of age and include enlargement of the liver (hepatomegaly), kidney (nephromegaly), elevated levels of lactate, uric acid and lipids (both total lipids and triglycerides), and possible seizures caused due to repeated episodes of hypoglycemia. Continued low blood sugar can lead to delayed growth and development and muscle weakness. Affected children typically have doll-like faces with fat cheeks, relatively thin extremities, short stature, and protuberant abdomen.
High lipid levels can lead to the formation of fatty skin growths called xanthomas. Other conditions that can be associated with untreated GSD1 include; osteoporosis, delayed puberty, gout (arthritis caused by accumulation of uric acid), kidney disease, pulmonary hypertension (high blood pressure in the arteries that supply the lungs), hepatic adenoma (benign liver tumors), polycystic ovaries in females, an inflammation of the pancreas (pancreatitis), diarrhea and changes in brain function due to repeated episodes of hypoglycemia.
Impaired platelet function can lead to a bleeding tendency with frequent nose bleeds (epistaxis). In general glycogen storage disease type1b patients have similar clinical manifestations as type Ia patients, but in addition to the above mentioned manifestations, glycogen storage disease type1b is also associated with impaired neutrophil and monocyte function as well as chronic neutropenia after the first few years of life, all of which result in recurrent bacterial infections and oral and intestinal mucosal ulcers.
Early diagnosis and effective treatment can result in normal growth and puberty and many affected individuals live into adulthood and enjoy normal life activities. Many female patients have had successful pregnancies and childbirth.
von Gierke disease complications
These complications can occur in patients with von Gierke disease:
- Frequent infection
- Gout
- Kidney failure
- Liver tumors
- Osteoporosis (thinning bones)
- Seizures, lethargy, confusion due to low blood sugar
- Short height
- Underdeveloped secondary sexual characteristics (breasts, pubic hair)
- Ulcers of the mouth or bowel
Long-term complications of untreated von Gierke disease include the following:
- Short stature. Children with von Gierke disease have poor growth and short stature in adulthood; however, with strict dietary regimens and control, growth and final adult stature have improved 2.
- Osteoporosis. Frequent fractures and radiographic evidence of osteopenia are common. Bone mineral content can be significantly reduced even in prepubertal children 3.
- Delayed puberty. Untreated affected individuals historically showed delayed onset of puberty; however, with adherence to a strict dietary regimen, age of onset of puberty can be normal 4.
- Gout. Although hyperuricemia is present in young affected children, gout rarely develops in untreated children before puberty 5.
- Renal disease. Proteinuria, hypertension, renal stones, nephrocalcinosis, and altered creatinine clearance may occur in younger affected individuals. With disease progression, interstitial fibrosis becomes evident. Some individuals progress to end-stage renal disease (ESRD) and may require a renal transplant 6.
- Systemic hypertension does not usually develop until the second decade or later and is often found in those individuals with von Gierke disease who also have renal disease 7.
- Pulmonary hypertension. Overt pulmonary hypertension as a long-term complication of von Gierke disease has been reported 8. Those at highest risk typically have a coexisting condition that also predisposes them to developing pulmonary hypertension 2.
- Hepatic adenomas with potential for malignant transformation. By the second or third decade of life, most affected individuals exhibit hepatic adenomas, a complication of which is intrahepatic hemorrhage. In some, the adenomas may undergo malignant transformation into hepatocellular carcinoma 9. Evidence for a relationship between poor metabolic control and the development of adenomas is conflicting 10. While it has been reported, the pathogenesis is likely to be multifactorial 11.
- Pancreatitis, a secondary complication of hypertriglyceridemia, is seen in some affected individuals, particularly those in poor dietary compliance.
- Neurocognitive effects. Changes in IQ, MRI findings, and EEG were found to correlate with the frequency of hypoglycemic episodes, particularly in those in poor dietary compliance 12.
- Anemia is a common problem in individuals with von Gierke disease 7, although the pathophysiology appears to differ in individuals with glycogen storage disease type 1a and those with glycogen storage disease type 1b 13: those with glycogen storage disease type 1a and severe anemia are likely to have hepatic adenomas, while those with glycogen storage disease type 1b and severe anemia may have enterocolitis 13.
- Vitamin D deficiency. In one study, 16/26 affected individuals had suboptimal levels of vitamin D suggesting that 25(OH)-vitamin D levels should be measured on a routine basis 14.
- Polycystic ovaries. Virtually all affected females have ultrasound findings consistent with polycystic ovaries. While this may affect ovulation and fertility in some females, in general fertility does not appear to be reduced 4.
- Irregular menstrual cycles. About half of women with von Gierke disease were found to have irregular menstrual cycles 4.
- Bleeding disorder. Some individuals have features suggestive of a von Willebrand disease-like defect with reduced von Willebrand factor antigen and/or dysfunctional von Willebrand factor. Manifestations include epistaxis, easy bruising, menorrhagia, and bleeding during surgical procedures. Menorrhagia appears to be a problem for reproductive-age females with von Gierke disease 15. This issue should be addressed when reviewing the clinical history of reproductive-age females with von Gierke disease. Referral to a gynecologist for management should be made when appropriate.
In addition, individuals with glycogen storage disease type 1b may develop the following:
- Neutropenia and impaired neutrophil function. Neutropenia and recurrent infections are common in individuals with glycogen storage disease type 1b and can also occur in a small subset of individuals with glycogen storage disease type 1a 16. Evidence suggests that the neutropenia in those with glycogen storage disease type 1b may be caused by increased apoptosis and migration of the neutrophils to inflamed tissues rather than by impairment in maturation 2.
- Inflammatory bowel disease or enterocolitis is common in individuals with glycogen storage disease type 1b 17.
- Thyroid autoimmunity. The prevalence of thyroid autoimmunity and hypothyroidism has been found to be increased in individuals with glycogen storage disease type 1b 18.
In the past, many individuals with von Gierke disease who were untreated died at a young age and the prognosis was guarded in survivors. However, early diagnosis and treatment have improved prognosis. Normal growth and puberty may be expected in treated children, and most affected individuals live into adulthood. However, it is not known if all long-term secondary complications can be avoided by good metabolic control. Some individuals treated early develop hepatic adenoma and proteinuria in adulthood.
von Gierke disease diagnosis
von Gierke disease is diagnosed by laboratory tests that indicate abnormal levels of glucose, lactate, uric acid, triglycerides and cholesterol. Molecular genetic testing for the G6PC and SLC37A4 genes is available to confirm a diagnosis. Molecular genetic testing can also be used for carrier testing and prenatal diagnosis. Liver biopsy can also be used to prove specific enzyme deficiency for glycogen storage disease type1a.
von Gierke disease should be suspected in individuals with the following clinical, laboratory, and histopathologic features.
Clinical findings: Signs of hypoglycemia, hepatomegaly, and growth failure
Laboratory findings
- Hypoglycemia. Fasting blood glucose concentration <60 mg/dL (reference range: 70-120 mg/dL)
- Lactic acidosis. Blood lactate >2.5 mmol/L (reference range: 0.5-2.2 mmol/L)
- Hyperuricemia. Blood uric acid >5.0 mg/dL (reference range: 2.0-5.0 mg/dL)
- Hyperlipidemia
- Triglycerides >250 mg/dL (reference range: 150-200 mg/dL); hypertriglyceridemia causes the plasma to appear “milky.”
- Cholesterol >200 mg/dL (reference range: 100-200 mg/dL)
- Glucagon or epinephrine challenge test. Administration of glucagon or epinephrine causes little or no increase in blood glucose concentration, but both increase serum lactate concentrations significantly.
Histopathologic liver findings
Distention of the liver cells by glycogen and fat; PAS positive and diastase sensitive glycogen that is uniformly distributed within the cytoplasm; normal or only modestly increased glycogen as compared with that seen in other liver glycogen storage diseases (especially glycogen storage disease type 3 and glycogen storage disease type 9); and large and numerous lipid vacuoles. Fibrosis and cirrhosis do not occur in von Gierke disease.
Note: As liver biopsy is invasive, it should only be done when a diagnosis cannot be made using molecular genetic testing (see Establishing the Diagnosis). Liver tissue may be obtained at the same time as another surgery (e.g., G-tube placement) as a snap-frozen liver sample and diagnosis can be made by measuring G6Pase enzyme activity; however, G6Pase enzyme activity on a piece of snap-frozen liver biopsy tissue will not detect glycogen storage disease type 1b.
von Gierke disease treatment
von Gierke disease is treated with a special diet in order to maintain normal glucose levels, prevent hypoglycemia and maximize growth and development. Frequent small servings of carbohydrates must be maintained during the day and night throughout the life. Calcium, vitamin D and iron supplements maybe recommended to avoid deficits. Frequent feedings of uncooked cornstarch are used to maintain and improve blood levels of glucose. Allopurinol, a drug capable of reducing the level of uric acid in the blood, may be useful to control the symptoms of gout-like arthritis during the adolescent years. Medications maybe prescribed to lower lipid levels and prevent and/or treat kidney disease. Human granulocyte colony stimulating factor (GCSF) may be used to treat recurrent infections in glycogen storage disease type1b patients. Liver tumors (adenomas) can be treated with minor surgery or a procedure in which adenomas are ablated using heat and current (radiofrequency ablation). Kidney and/or liver transplantation are sometimes considered if other therapies are unsuccessful or where liver adenomas keep growing.
Individuals with von Gierke disease should be monitored at least annually with kidney and liver ultrasound and routine blood work specifically used for monitoring glycogen storage disease patients.
Genetic counseling is recommended for affected individuals and their families.
Uncooked cornstarch orally can be started during infancy 19. Cornstarch should be given between meals or before bedtime so as not to interfere with appetite at meal time.
- Argo® is the preferred brand in the United States in terms of both taste and sustainability. Other brands should be used with caution, and randomly switching between brands is not recommended. A modified cornstarch, waxy maize extended-release cornstarch, Glycosade®, is available in Europe and the United States for overnight treatment 20.
- There is no consensus on the age at which cornstarch therapy should be initiated but a trial is often introduced between ages six months and one year. Amylase is required to digest cornstarch and may not be present until age two years.
- The severity and recurrence of hypoglycemic episodes determines the timing of cornstarch therapy initiation via nasogastric tube or gastrostomy tube in infancy and childhood and oral ingestion in teenagers and adults.
- Note: Recommendations for uncooked cornstarch dosing are: 1.6 g/kg body weight every four hours for infants, 1.7-2.5 g/kg body weight every six hours for young children through puberty, and 1.7-2.5 g/kg body weight given before bed time for adults. Dosing for modified cornstarch should be decided under the guidance of a metabolic treatment team using frequent glucose monitoring.
Optimal nutrition for growth and development:
- Complex carbohydrates (60%-70% of recommended total energy intake) including cornstarch and starches from whole-grain bread, rice, and potatoes for children and adolescents and rice cereals for infants
- Note: (1) Intake of sucrose and fructose should be restricted for infants and older children. Avoid sugar, fruits, fruit juice, high-fructose corn syrup, sorbitol, cane juice, and other foods that cannot be broken down into glucose. (2) Intake of lactose and galactose should be limited. One serving per day for an older child usually entails 1.5 ounces of cheese OR 1 cup of yogurt OR 1 cup of skim milk. (3) Blood glucose monitoring for hypoglycemia is important so that overtreatment with cornstarch may be avoided. If excess weight gain occurs, consider decreasing the amount of cornstarch gradually over time and mixing cornstarch in water instead of Prosobee® or Tolerex®.
- Protein (10%-15% of recommended total energy intake) of high quality, high biologic value (e.g., protein low in fat). Soy formula (Prosobee®) and soy milk (lactose/galactose free) can be used both in infancy and childhood for carbohydrate and protein needs.
- Note: (1) Avoid soy milks that are sweetened with sucrose; the ones with rice syrup or brown rice syrup can be taken. (2) Soy milk mixed with cane sugar should be avoided.
- Fat (10%-15% of recommended total energy intake) as part of a low-fat diet that includes heart-healthy fats such as canola oil and olive oil. Note: Families need explicit guidelines on fat intake as part of monitoring total energy intake and avoiding excessive weight gain.
- Calcium and vitamin D supplements to support bone growth and mineralization. If the individual is not on calcium-fortified soy milk, calcium citrate or calcium carbonate with vitamin D is recommended to meet RDA for age needs and to prevent nutritional deficiencies.
- Iron supplements in complete multivitamins with minerals (100% RDA iron and zinc) to avoid anemia and iron deficiency
Treatment of other manifestations
Allopurinol, a xanthine oxidase inhibitor, is used to prevent gout when dietary therapy fails to completely normalize blood uric acid concentration, especially after puberty.
Lipid-lowering medications, such as HMG-CoA reductase inhibitors and fibrate (e.g., Lipitor®, gemfibrozil), are used when lipid levels remain elevated despite good metabolic control, especially after puberty.
Citrate supplementation may help prevent or ameliorate nephrocalcinosis and the development of urinary calculi.
- In young children, an initial dose of 1 mEq/kg/day in liquid form divided into three doses should be instituted. The dose should be increased based on urinary citrate excretion.
- In older children and adults, potassium citrate tablets can be started at a dose of 10 mEq/3x/day. Citrate use should be monitored as it can cause hypertension and life-threatening hyperkalemia in affected individuals with renal impairment. Sodium levels should also be monitored.
Angiotensin-converting enzyme (ACE) inhibitors such as captopril are used to treat microalbuminuria, an early indicator of renal dysfunction.
Kidney transplantation can be performed for end-stage renal disease (ESRD).
Hepatic adenomas can be treated with surgery or other interventions including percutaneous ethanol injections and radiofrequency ablation.
Liver transplantation can be considered when other interventions have failed.
Human granulocyte colony-stimulating factor (G-CSF) can be used to treat recurrent infections:
- G-CSF may increase the number and improve the function of circulating neutrophils.
- G-CSF may improve the symptoms of Crohn’s-like inflammatory bowel disease in individuals with GSDIb.
- G-CSF should be administered subcutaneously starting at 1.0 μg/kg given daily or every other day. The G-CSF dose should be increased stepwise at approximately two-week intervals until the target absolute neutrophil count (ANC) of greater than 500 to up to 1.0 x 109/L is reached.
Standard management of individuals with platelet dysfunction/von Willebrand disease include antifibrinolytics and deamino-8-d-arginine vasopressin (DDAVP), which acts by stimulating factor VIII from endothelial cells and improving von Willebrand factor activity and the platelet release reaction. However, DDAVP should be used with caution due to the risk for fluid overload and hyponatremia.
Surveillance
Annual ultrasound examination of the kidneys after the first decade of life; liver ultrasound every 12 to 24 months until age 16 years; in individuals age 16 years and older, liver CT or MRI with contrast every six to 12 months to monitor for hepatic adenomas; liver ultrasound or MRI examinations (depending on age) every three to six months if hepatic adenoma is detected; hepatic profile (AST, ALT, albumin, bilirubin, PT/INR, aPTT) and serum creatinine every six to 12 months; complete blood count every three months for those on G-CSF; imaging with measurement of the spleen for those on G-CSF; systemic blood pressure at every clinic visit beginning in infancy; echocardiography every three years beginning at age ten years (or earlier if symptoms are present) to screen for pulmonary hypertension; routine monitoring of vitamin D levels.
When hepatic adenoma is detected. Abdominal CT/MRI with contrast should be performed in older individuals or individuals within the pediatric age group once adenomas are detected on ultrasound. Imaging should be repeated every six to 12 months or more often depending on laboratory and clinical findings. Liver imaging studies (MRI/CT scan) should evaluate liver size, adenomas, evidence of portal hypertension, or features suggestive of liver carcinoma (nodules, heterogeneous echogenic shadows) 9.
Note: Serum AFP and CEA levels are not reliable markers of hepatocellular carcinoma 21.
For those individuals treated with G-CSF serial blood counts should be performed approximately every three months to assess response to treatment and, although the risk of acute myeloid leukemia (AML) is low, to evaluate for the presence of myeloblasts in the blood. Any imaging performed for liver surveillance (e.g., ultrasound, CT, or MRI) should include measurements of the spleen to identify and monitor splenomegaly.
Cardiovascular surveillance
- Systemic blood pressure measurements should be obtained at all clinic visits beginning in infancy.
- Screening for pulmonary hypertension by echocardiography every three years beginning at age ten years (or earlier if symptoms are present) is appropriate.
25(OH)-vitamin D levels should be monitored routinely and treated as needed.
Agents and circumstances to avoid
Diet should be low in fructose and sucrose; galactose and lactose intake should be limited to one serving per day; combined oral contraception should be avoided in women, particularly those with adenomas.
Pregnancy management
Although successful pregnancies have been reported in women with von Gierke disease, certain precautions should be taken:
- Pre-pregnancy counseling regarding diet to avoid low blood glucose and to stress the importance of blood glucose monitoring prior to and during pregnancy
- Baseline ultrasound of liver and kidneys prior to pregnancy
- Consideration of referral to high-risk obstetrician
- Review of medications prior to conception to weigh risks and benefits:
- Exposure to ACE inhibitors in the second and third trimesters of pregnancy can cause fetal damage and death.
- No data on the use of allopurinol during pregnancy in humans exist; however, high doses have been shown to interfere with embryo development in animal models.
- Lipid-lowering drugs may also lead to adverse fetal effects and should be avoided during pregnancy.
Metabolic control should be followed closely throughout the pregnancy. Because carbohydrate requirements may increase with pregnancy, glucose levels should be monitored closely and treated accordingly 22.
Abdominal ultrasound should be performed every six to 12 weeks. Sechi et al 4 reported an increase in the size of pre-existent adenomas and the development of new adenomas during pregnancy and recommended monitoring by imaging before, during, and after pregnancy. Resection of large (≥5 cm) or growing adenomas before pregnancy has been recommended 23.
Renal function should be followed closely, as this may worsen during pregnancy 24. Development of renal calculi has been reported in pregnant women with glycogen storage disease type 1b 25.
Glucose infusion during labor has been used 22.
Platelet count, hemoglobin, and clotting studies should be performed because of the potential for increased bleeding at delivery 26.
von Gierke disease prognosis
With treatment, growth, puberty, and quality of life have improved for people with von Gierke disease. Those who are identified and carefully treated at a young age can live into adulthood.
Early treatment also decreases the rate of severe problems such as:
- Gout
- Kidney failure
- Life-threatening low blood sugar
- Liver tumors.
- Glycogen storage disease type I. https://ghr.nlm.nih.gov/condition/glycogen-storage-disease-type
- Kishnani PS, Austin SL, Abdenur JE, Arn P, Bali DS, Boney A, Chung WK, Dagli AI, Dale D, Koeberl D, Somers MJ, Wechsler SB, Weinstein DA, Wolfsdorf JI, Watson MS. Diagnosis and management of glycogen storage disease type I: a practice guideline of the American College of Medical Genetics and Genomics. Genet Med. 2014;16:e1
- Cabrera-Abreu J, Crabtree NJ, Elias E, Fraser W, Cramb R, Alger S. Bone mineral density and markers of bone turnover in patients with glycogen storage disease types I, III and IX. J Inherit Metab Dis. 2004;27:1–9.
- Sechi A, Deroma L, Lapolla A, Paci S, Melis D, Burlina A, Carubbi F, Rigoldi M, Di Rocco M. Fertility and pregnancy in women affected by glycogen storage disease type I, results of a multicenter Italian study. J Inherit Metab Dis. 2013;36:83–9.
- Matern D, Seydewitz HH, Bali D, Lang C, Chen YT. Glycogen storage disease type I: diagnosis and phenotype/genotype correlation. Eur J Pediatr. 2002;161 Suppl 1:S10–9.
- Iida S, Matsuoka K, Inoue M, Tomiyasu K, Noda S. Calcium nephrolithiasis and distal tubular acidosis in type 1 glycogen storage disease. Int J Urol. 2003;10:56–8.
- Rake JP, Visser G, Labrune P, Leonard JV, Ullrich K, Smit GP. Glycogen storage disease type I: diagnosis, management, clinical course and outcome. Results of the European Study on Glycogen Storage Disease Type I (ESGSD I). Eur J Pediatr. 2002;161 Suppl 1:S20–34.
- Humbert M, Labrune P, Simonneau G. Severe pulmonary arterial hypertension in type 1 glycogen storage disease. Eur J Pediatr. 2002;161 Suppl 1:S93–6.
- Franco LM, Krishnamurthy V, Bali D, Weinstein DA, Arn P, Clary B, Boney A, Sullivan J, Frush DP, Chen YT, Kishnani PS. Hepatocellular carcinoma in glycogen storage disease type Ia: a case series. J Inherit Metab Dis. 2005;28:153–62.
- Beegle RD, Brown LM, Weinstein DA. Regression of hepatocellular adenomas with strict dietary therapy in patients with glycogen storage disease type I. JIMD Rep. 2015;18:23–32.
- Wang DQ, Fiske LM, Carreras CT, Weinstein DA. Natural history of hepatocellular adenoma formation in glycogen storage disease type I. J Pediatr. 2011;159:442–6.
- Melis D, Parenti G, Della Casa R, Sibilio M, Romano A, Di Salle F, Elefante R, Mansi G, Santoro L, Perretti A, Paludetto R, Sequino L, Andria G. Brain damage in glycogen storage disease type I. J Pediatr. 2004;144:637–42.
- Wang DQ, Carreras CT, Fiske LM, Austin S, Boree D, Kishnani PS, Weinstein DA. Characterization and pathogenesis of anemia in glycogen storage disease type Ia and Ib. Genet Med. 2012;14:795–9.
- Banugaria SG, Austin SL, Boney A, Weber TJ, Kishnani PS. Hypovitaminosis D in glycogen storage disease type I. Mol Genet Metab. 2010;99:434–7.
- Austin SL, El-Gharbawy AH, Kasturi VG, James A, Kishnani PS. Menorrhagia in patients with type I glycogen storage disease. Obstet Gynecol. 2013;122:1246–54.
- Weston BW, Lin JL, Muenzer J, Cameron HS, Arnold RR, Seydewitz HH, Mayatepek E, Van Schaftingen E, Veiga-Da-Cunha M, Matern D, Chen YT. Glucose-6-phosphatase mutation G188R confers an atypical glycogen storage disease type Ib phenotype. Pediatr Res. 2000;48:329–34.
- Visser G, Rake JP, Labrune P, Leonard JV, Moses S, Ullrich K, Wendel U, Groenier KH, Smit GP. Granulocyte colony-stimulating factor in glycogen storage disease type 1b. Results of the European Study on Glycogen Storage Disease Type 1. Eur J Pediatr. 2002b;161 Suppl 1:S83–7.
- Melis D, Pivonello R, Parenti G, Della Casa R, Salerno M, Lombardi G, Sebastio G, Colao A, Andria G. Increased prevalence of thyroid autoimmunity and hypothyroidism in patients with glycogen storage disease type I. J Pediatr. 2007;150:300–5.
- Weinstein DA, Wolfsdorf JI. Effect of continuous glucose therapy with uncooked cornstarch on the long-term clinical course of type 1a glycogen storage disease. Eur J Pediatr. 2002;161 Suppl 1:S35–9.
- Ross KM, Brown LM, Corrado MM, Chengsupanimit T, Curry LM, Ferrecchia IA, Porras LY, Mathew JT, Weinstein DA. Safety and Efficacy of Chronic Extended Release Cornstarch Therapy for Glycogen Storage Disease Type I. JIMD Rep. 2016;2016;26:85–90.
- Shieh JJ, Lu YH, Huang SW, Huang YH, Sun CH, Chiou HJ, Liu C, Lo MY, Lin CY, Niu DM. Misdiagnosis as steatohepatitis in a family with mild glycogen storage disease type 1a. Gene. 2012;509:154–7.
- Ferrecchia IA, Guenette G, Potocik EA, Weinstein DA. Pregnancy in women with glycogen storage disease Ia and Ib. J Perinat Neonatal Nurs. 2014;28:26–31.
- Terkivatan T, de Wilt JH, de Man RA, Ijzermans JN. Management of hepatocellular adenoma during pregnancy. Liver. 2000;20:186–7.
- Yamamoto T, Suzuki Y, Kaneko S, Hattori Y, Obayashi S, Suzumori N, Sugiura M. Glycogen storage disease type Ia (GSD Ia) during pregnancy: report of a case complicated by fetal growth restriction and preeclampsia. J Obstet Gynaecol Res. 2010;36:1125–9.
- Dagli AI, Lee PJ, Correia CE, Rodriguez C, Bhattacharya K, Steinkrauss L, Stanley CA, Weinstein DA. Pregnancy in glycogen storage disease type Ib: gestational care and report of first successful deliveries. J Inherit Metab Dis. 2010;33 Suppl 3:S151–7.
- Lewis R, Scrutton M, Lee P, Standen GR, Murphy DJ. Antenatal and Intrapartum care of a pregnant woman with glycogen storage disease type 1a. Eur J Obstet Gynecol Reprod Biol. 2005;118:111–2.