What is Von Willebrand disease
Von Willebrand disease is an inherited bleeding disorder. If you have von Willebrand disease, you don’t have enough of a clotting factor called von Willebrand factor (VWF) or the von Willebrand factor doesn’t work properly 1. Most people with Von Willebrand disease are born with it, having inherited it from one or both parents. People with von Willebrand disease often experience bruising, nosebleeds, and prolonged bleeding or oozing following an injury, after surgery, or having a tooth pulled. Affected women may have heavy menstrual bleeding. In severe cases, heavy bleeding occurs after minor injury or even in the absence of injury.
Normally, when one of your blood vessels is injured, you start to bleed. Small blood cell fragments called platelets clump together to plug the hole in the blood vessel and stop the bleeding. Von Willebrand factor acts like glue to help the platelets stick together and a series of actions referred to as activation of the coagulation cascade, resulting in the formation of a stable blood clot.
The von Willebrand factor (VWF) is a large multimeric glycoprotein, and it is susceptible to the shear stress associated with high flow states. Von Willebrand factor also carries clotting Factor 8 (factor VIII), another important protein that helps your blood clot. Von Willebrand factor (VWF) carries Factor 8 (factor VIII) in your blood, increasings its half-life, and releases it as necessary. Factor 8 (factor VIII) is the protein that’s missing or doesn’t work well in people who have hemophilia, another bleeding disorder. The result is that it takes longer than normal for your blood to clot and for bleeding to stop. If the amount of functional von Willebrand factor (VWF) is insufficient, then platelet adherence and aggregation are affected, levels of Factor 8 (factor VIII) could be decreased, blood clot formation takes longer, and therefore bleeding is prolonged. This deficiency causes a condition referred to as von Willebrand disease (VWD). People with von Willebrand disease often experience easy bruising, long-lasting nosebleeds, and excessive bleeding or oozing following an injury, surgery, or dental work. Women with von Willebrand disease typically have heavy or prolonged bleeding during menstruation (menorrhagia), and some may also experience reproductive tract bleeding during pregnancy and childbirth.
However, many people who have von Willebrand disease have no obvious symptoms and are not even aware they have it. Some only find out when a problem is picked up on blood testing for other conditions or when abnormal bleeding occurs following surgery or a serious injury.
Von Willebrand disease might be suspected if you show symptoms such as easy bleeding or bruising, especially if someone in your family is known to have von Willebrand disease. In severe cases of von Willebrand disease, heavy bleeding occurs after minor trauma or even in the absence of injury (spontaneous bleeding). Rarely, the bleeding may even cause death.
Symptoms of von Willebrand disease may change over time. Increased age, pregnancy, exercise, and stress may cause bleeding symptoms to become less frequent.
When symptoms of von Willebrand disease show up, they may include:
- large bruises or bruising easily
- heavy bleeding or bleeding more than normal, for example after an injury or long-lasting bleeding from cuts
- in women, heavy periods and bleeding during or after childbirth
- frequent or long-lasting nosebleeds or gum bleeds
- heavy or long-lasting bleeding after a tooth removal or surgery
- blood in your urine or stools (bleeding in the gut causing bleeding from the bottom)
- bleeding into the joints and muscles (in severe cases).
If you have von Willebrand disease, you might experience different symptoms at different times of your life.
Von Willebrand disease is estimated to affect 1 in 100 to 10,000 individuals 2, 3. According to the Centers for Disease Control and Prevention (CDC) 3.2 million people (or about 1 in every 100) people in the United States have von Willebrand disease 4. Because people with mild signs and symptoms may not come to medical attention, it is thought that this condition is underdiagnosed. Most researchers agree that von Willebrand disease is the most common genetic bleeding disorder. Von Willebrand disease affects both males and females, while hemophilia mainly affects males. However, women are more likely to experience symptoms of von Willebrand disease because of the increased bleeding it causes during their menstrual periods, during pregnancy, and after childbirth. Between 2012 and 2016, more than 14,600 men, women, and children were seen at hemophilia treatment centers for treatment of von Willebrand disease. About 2/3 were women and girls. And von Willebrand disease is more common and usually milder than hemophilia.
Von Willebrand disease can’t be cured. Treatment for von Willebrand disease depends on the type of von Willebrand disease and how severe it is. In mild cases, treatment might not be needed at all, unless you have surgery or dental work, or sustain an injury that causes bleeding.
Your doctor might suggest one or more of the following treatments to increase your von Willebrand factor (VWF), strengthen blood clots or control heavy menstrual bleeding:
- Desmopressin. Desmopressin is available as an injection (DDAVP) or nasal spray (Stimate). Desmopressin is a synthetic hormone that controls bleeding by stimulating your body to release more of the von Willebrand factor (VWF) stored in the lining of your blood vessels. Many doctors consider DDAVP the first treatment for managing von Willebrand disease. It can be used before minor surgical procedures to help control bleeding. You might be given a trial of desmopressin to make sure it’s effective for you.
- Replacement therapies. These include infusions of concentrated blood-clotting factors containing von Willebrand factor (VWF) and Factor 8 (factor VIII) 5, 6.. Your doctor might recommend them if DDAVP isn’t an option for you or has been ineffective. Another replacement therapy approved by the Food and Drug Administration (FDA) for treating adults 18 and older is a genetically engineered (recombinant) von Willebrand factor (rVWF) product 7. Because recombinant factor is made without plasma, it can reduce the risk of a viral infection or allergic reaction.
- Oral contraceptives. In addition to preventing pregnancy, these drugs can help control heavy bleeding during menstrual periods. The estrogen hormones in birth control pills can boost von Willebrand factor and Factor 8 (factor VIII) activity.
- Clot-stabilizing medications. These anti-fibrinolytic medications — such as aminocaproic acid (Amicar) and tranexamic acid (Cyklokapron, Lysteda) — can help stop bleeding by slowing the breakdown of blood clots. Doctors often prescribe these drugs before or after a surgical procedure or tooth extraction.
- Drugs applied to cuts. A fibrin sealant (Tisseel) placed on a cut helps curtail bleeding. This is applied like glue using a syringe. There are also over-the-counter products to stop nosebleeds.
If your condition is mild, your doctor might recommend treatment only when you’re having surgery or dental work or when you’ve had a trauma, such as a car accident.
Treatments for von Willebrand disease can be given when needed, including:
- medicines to help your blood clot properly
- treatments to help wounds stop bleeding
- hormones to stimulate the production of von Willebrand factor in your blood.
Some minor bleeding can be managed at home, while more serious bleeding may require expert help.
To reduce the chances of having problems during pregnancy and after delivery, a woman with von Willebrand disease should:
- Talk to her doctor about her bleeding disorder before becoming pregnant.
- Think about seeing a doctor who specializes in high-risk pregnancies and a hospital that has a hematologist (a doctor who specializes in bleeding disorders) on staff for prenatal care and delivery.
- Talk to her doctor before having any prenatal tests or medical procedures (for example, amniocentesis) to find out whether anything needs to be done to prevent serious blood loss.
- Have blood tests done during her third trimester to measure the levels of von Willebrand factor (VWF) and Factor 8 (factor VIII) in her blood to help plan for delivery 8.
- Meet with an anesthesiologist (a doctor who specializes in giving patients medicines for pain relief) to review her options for pain medicine and to discuss taking medicine to lower her risk of bleeding.
Figure 1. Blood clotting factors
Figure 2. Blood clotting process
Should I tell my other doctors I have von Willebrand disease?
Yes. This is important information for your health care providers, including your dentist, to have. They will need to plan ahead for any surgeries, childbirths, or dental procedures you may have.
Can I have von Willebrand disease and not know it?
Yes. Some people experience no or few symptoms, even though they have quantitative or qualitative VWF deficiencies.
Are there other causes of von Willebrand factor (VWF) deficiency besides inherited causes?
Yes, a deficiency in von Willebrand factor (VWF) may be due to another disease or condition (also known as Acquired von Willebrand disease), where there is no family or personal bleeding history up to the point when signs and symptoms develop, but this rarely occurs. Acquired von Willebrand disease is sometimes seen in people with (see Table 1 below):
- Conditions that cause the breakdown of von Willebrand factor (VWF), such as increased pressure in the arteries leading from the heart to the lungs (pulmonary hypertension) and structural defects of the heart (e.g., aortic valve stenosis)
- Lymphoma, myeloma, or autoimmune disorders (such as lupus) that cause the production of von Willebrand factor (VWF) antibodies
- Myeloproliferative neoplasms associated with increased platelet production that cause increased binding of von Willebrand factor (VWF) to platelets
- Hypothyroidism (underactive thyroid), which can decrease von Willebrand factor (VWF) production
- Wilms tumor and other disorders that bind to von Willebrand factor (VWF) and remove it from the blood
- Certain medications such as valproic acid, ciprofloxacin and hetastarch.
Von Willebrand disease types
Von Willebrand disease is divided into three types, with type 2 being further divided into four subtypes (2A, 2B, 2M, and 2N). Type 1 is the mildest and most common of the three types, accounting for 75 percent of affected individuals. Type 3 is the most severe and rarest form of the condition. The four subtypes of type 2 von Willebrand disease (2A, 2B, 2M, and 2N) are intermediate in severity. Another form of the disorder, acquired von Willebrand syndrome, is not caused by inherited gene mutations. Acquired von Willebrand syndrome is typically seen along with other disorders, such as diseases that affect bone marrow or immune cell function. This rare form of the condition is characterized by abnormal bleeding into the skin and other soft tissues, usually beginning in adulthood.
Von Willebrand disease can have different inheritance patterns.
Most cases of type 1 and type 2 von Willebrand disease are inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. The chances of inheriting type 1 von Willebrand disease can also be affected by other things, including blood group – people with blood group O are more often affected than people with blood group A or B. This means it’s not always easy to predict whether a child might inherit it from their parents.
Type 3, some cases of type 2, and a small number of type 1 cases of von Willebrand disease are inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. Most often, the parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they do not show signs and symptoms of the condition.
Parents who are carriers of a faulty VWF gene may not have symptoms themselves.
Speak to your specialist if you have von Willebrand disease and are thinking of having a baby. If you have a family history of von Willebrand disease and think you might be affected, tests should ideally be done before getting pregnant.
Figure 3. Type 1 and type 2 von Willebrand disease are inherited in an autosomal dominant pattern
Figure 4. Type 3 and some type 2 von Willebrand disease are inherited in an autosomal recessive pattern
Von Willebrand disease Type 1
People who have type 1 von Willebrand disease have low levels of von Willebrand factor (VWF) but the von Willebrand factor (VWF) functions normally and may have low levels of Factor 8 (factor VIII). Type 1 is the mildest and most common form of Von Willebrand disease. About 3 out of 4 people who have Von Willebrand disease have type 1.
Von Willebrand disease Type 1 tends to cause bruising and mild to moderate bleeding, such as persistent nosebleeds, heavy menstrual periods, and prolonged bleeding following childbirth, trauma, dental procedures, and surgeries. Symptoms and the severity of bleeding will vary from person to person and from episode to episode.
Von Willebrand disease Type 2
Type 2 von Willebrand disease is associated with a normal amount of von Willebrand factor (VWF) , but the von Willebrand factor (VWF) doesn’t work well. Type 2 is divided into subtypes: 2A, 2B, 2M, and 2N. Different gene mutations (changes) cause each type, and each is treated differently. Thus, it’s important to know the exact type of Von Willebrand disease that you have.
- Type 2A: Absent Multimers. VWF-dependent platelet adhesion is decreased with selective deficiency of high molecular weight multimers. Intermediate multimers may also be missing. This can be due to decreased assembly or increased proteolysis of multimers. Von Willebrand factor antigen (VWF:Ag) levels (this test measures the amount of the von Willebrand factor protein present in the blood) and Factor 8 (FVIII) coagulant activity (FVIII:C) levels may be normal or slightly decreased. Von Willebrand factor ristocetin cofactor activity (VWF:RCo) (this test determines whether the von Willebrand factor protein is functioning properly) is moderately decreased. Multimer analysis shows decreased or absent high and intermediate molecular weight multimers.
- Type 2B: Binding of platelets increased. VWF binding at the platelet GPIb binding site for VWF is increased, leading to increased platelet clumping and decreased VWF multimers and platelet numbers. VWF:Ag levels can be normal or slightly decreased, while von Willebrand factor ristocetin cofactor activity (VWF:RCo) levels are moderately decreased. Multimer analysis shows a decrease of large multimers. There may be thrombocytopenia present in times of stress such as surgery or pregnancy. Laboratory analysis may be similar to type 2A or 2M. Further analysis by platelet aggregation testing will show abnormally increased Ristocetin-Induced Platelet Aggregation (RIPA) at low doses of ristocetin.
- Type 2M: Multimers normal. VWF – dependent platelet adhesion is decreased due to abnormal binding of VWF to platelets at the platelet binding site GPIb. There can also be decreased binding of VWF to collagen. VWF:Ag levels can be normal or slightly decreased. VWF:RCo levels are moderately decreased. Multimer analysis can be normal with the high molecular weight multimers present.
- Type 2N: Normandy (after the province of origin of one of the first families identified with the disease). VWF binding to FVIII:C is impaired. FVIII:C levels are affected and may be less than 10%. Normal VWF:Ag and VWF:RCo levels are seen. To determine the difference between Type 2N and mild hemophilia A, assays of FVIII-VWF binding are performed. In addition, an autosomal recessive family history may be present.
Von Willebrand disease Type 3
People who have type 3 von Willebrand disease usually have no von Willebrand factor and low levels of Factor 8 (factor VIII). Type 3 is the most serious form of Von Willebrand disease, but it’s very rare. Bleeding from the mouth, nose and gut is common, and you can have joint and muscle bleeds after an injury.
Acquired von Willebrand disease
Acquired von Willebrand disease is a rare condition that occurs when secondary (acquired) processes lead to a functional impairment of von Willebrand factor, either by decreasing its available quantity or interfering with the physiological hemostasis pathway 9. Acquired von Willebrand disease is associated with a multitude of conditions, including lymphoproliferative disorders (most common: 48%), myeloproliferative disorders (chronic granulocytic leukemia, essential thrombocythemia, and polycythemia vera), neoplasms (Wilm’s tumor and gastric cancer), immunological disorders, cardiovascular diseases (such as aortic stenosis, ventricular septal defects (VSD), ventricular assist devices (VAD), extracorporeal membrane oxygenation (ECMO), or metallic cardiac valves), hypothyroidism, hemoglobinopathies, drugs (valproate, ciprofloxacin, and hydroxyethyl starch), and infections 10, 11. Among lymphoproliferative disorders, monoclonal gammopathy of unknown significance (MGUS) is the most commonly associated with acquired von Willebrand disease, including in 23% of registered patients 11. Other lymphoproliferative disorders associated with acquired von Willebrand disease are multiple myeloma, Waldenstrom macroglobulinemia, chronic lymphocytic leukemia, hairy cell leukemia, non Hodgkin lymphoma, and lymphosarcoma 12.
There are two proposed mechanisms for acquired von Willebrand disease. Immune mechanism is believed to be the responsible mechanism in patients with lymphoproliferative or autoimmune diseases. Nonspecific antibodies bind to von Willebrand factor; this complex gets cleared by FC-bearing cells or autoantibodies directed against the von Willebrand factor 10. In monoclonal gammapathy of undetermined significance (MGUS), paraproteins bind to von Willebrand factor resulting in accelerated clearance and low circulating levels 13. Immune-mediated cause most likely mediates the disease process, as patients often had significant response to intravenous immunoglobulin (IVIG). Nonimmune-mediated mechanisms are thought to be due to loss of large von Willebrand factor multimers under high shear stress conditions (congenital heart defects, aortic stenosis, artificial heart valves, or left ventricular assist device), absorption of von Willebrand factor onto tumor cells, decreased synthesis (hypothyroidism and valproic acid) or release from endothelial cells, or increased proteolysis of von Willebrand factor (ciprofloxacin) 13.
Presentation in acquired von Willebrand disease is similar to congenital von Willebrand disease. However, acquired von Willebrand disease presents later in life with no previous or family history of bleeding 14. Routine recommended tests in acquired von Willebrand disease are vWF:Ag assay, vWF:Ag activity assay, and ristocetin cofactor assay (vWF:RCo/Ag ratio) (normal = 1) 13. Among them, ristocetin cofactor assay is the recommended test 15. vWF:RCo/Ag ratio < 0.6–0.7 indicates inhibitory antibodies or a selective loss or decrease in high molecular weight multimers 15. Circulating inhibitors are rarely detected in this condition 16. vWF multimer analysis is the gold standard test. It is particularly useful if other tests are negative 15. A multimeric pattern with decreased levels of high molecular weight vWF multimers is seen because the inhibitors tend to attack the large multimers of von Willebrand factor. Serum protein electrophoresis or immunofluorescence tests and thyroid function test can be done to establish etiology 16. Congenital von Willebrand disease and acquired von Willebrand disease can be differentiated by measurement of von Willebrand factor propeptide (vWFAg II). Von Willebrand factor propeptide is a marker of von Willebrand factor synthesis. Since acquired von Willebrand disease is associated with clearance of von Willebrand factor, von Willebrand factor propeptide will be normal 16.
Table 1. Disorders associated with Acquired von Willebrand disease
| Primary underlying conditions | Examples |
|---|---|
| Lymphoproliferative disorders | Multiple myeloma Monoclonal gammapathy of undetermined significance (MGUS) Waldenström macroglobulinemia Chronic lymphocytic leukemia Hairy cell leukemia Non-Hodgkin lymphomas Acute lymphoblastic leukemia |
| Myeloproliferative disorders | Essential thrombocythemia Polycythemia vera Spontaneous myelofibrosis Chronic myeloid leukemia |
| Non-hematological malignancies | Wilms’ tumors Cancers/solid tumors Primitive neuroectodermal tumors |
| Autoimmune/endocrine disorders | Systemic lupus erythematosus (SLE) Other connective tissue disorders Graft versus host disease (GVHD) Hypothyroidism |
| Cardiovascular diseases (inherited, acquired) | Ventricular septal defects (VSD) Atrial septal defects (ASD) Aortic stenosis Mitral valve prolapse Endocarditis Angiodysplasia Systemic atherosclerosis |
| Drugs and other therapeutic agents: antibiotics antiepileptic agents plasma volume expanders coagulation factors | ciprofloxacin, griseofulvin, tetracycline valproic acid hydroxyethyl starch (hes) recombinant factor III |
| Other | Uremia Infections (viral, parasitic) Diabetes mellitus Hemoglobinopathies Sarcoidosis Ehlers-danlos syndrome Telangiectasia Ulcerative colitis Liver cirrhosis Turner syndrome Lactoferrin deficiency Myelodysplastic syndrome |
Living with von Willebrand disease
If you have von Willebrand disease, you can take steps to prevent bleeding and stay healthy.
For example, avoid over-the-counter medicines that can affect blood clotting, such as aspirin, ibuprofen, and other nonsteroidal anti-inflammatory drugs (NSAIDs). Always check with your doctor before taking any medicines.
Tell your doctor, dentist, and pharmacist that you have von Willebrand disease. Your dentist can ask your doctor whether you need medicine before dental work to reduce bleeding.
You also may want to tell other people about your condition, like your employee health nurse, gym trainer, and sports coach. Making them aware will allow them to act quickly if you have an injury.
Consider wearing a medical ID bracelet or necklace if you have a serious form of von Willebrand disease (for example, type 3). In case of a serious accident or injury, the health care team treating you will know that you have von Willebrand disease.
Be physically active and maintain a healthy weight. Physical activity helps keep muscles flexible. It also helps prevent damage to muscles and joints. Always stretch before exercising.
Some safe physical activities are swimming, biking, and walking. Football, hockey, wrestling, and lifting heavy weights are not safe activities if you have bleeding problems. Always check with your doctor before starting any exercise program.
Your parents, brothers and sisters, and children also may have von Willebrand disease. Talk with them about your diagnosis and suggest that they get tested too.
Pregnancy and von Willebrand Disease
Pregnancy can be a challenge for women who have von Willebrand disease. However, with proper care, women with von Willebrand disease can have a successful pregnancy and deliver a healthy child. Blood levels of von Willebrand factor and Factor 8 (factor VIII) tend to increase during pregnancy. However, the high levels of clotting factors during pregnancy drop back to lower levels after delivery. Women who have von Willebrand disease can have bleeding problems during delivery or surgery (for example, following a Cesarean section). They also are likely to have heavy bleeding for an extended time after delivery. Some women have bleeding from the birth canal that lasts a long time. This is called postpartum hemorrhage and can require treatment to stop the bleeding. A woman who has von Willebrand disease should be monitored closely throughout her pregnancy by her doctors.
You can take steps to lower the risk of complications during pregnancy. If possible, talk with a hematologist and an obstetrician who specializes in high-risk pregnancies before you become pregnant.
A hematologist is a doctor who specializes in diagnosing and treating blood disorders. An obstetrician is a doctor who provides treatment and care for pregnant women.
Consider using a medical center that specializes in high-risk obstetrics and has a hematologist on staff for prenatal care and delivery (e.g., hemophilia treatment center). Hemophilia Treatment Centers search (https://dbdgateway.cdc.gov/HTCDirSearch.aspx)
Before you have any invasive procedure, such as amniocentesis, discuss with your doctor whether you need to take steps to prevent serious blood loss.
During your third trimester, you should have blood tests to measure von Willebrand factor and Factor 8 (factor VIII) to help plan for delivery.
You also should meet with an anesthesiologist to review your choices for anesthesia and to discuss taking medicine to reduce your bleeding risk. The term “anesthesia” refers to a loss of feeling and awareness. Some types of anesthesia temporarily put you to sleep, while others only numb certain areas of your body.
With these steps for safety, most women who have von Willebrand disease can have successful pregnancies.
You may also want to speak to your specialist about genetic testing to see if your baby is at risk of being born with von Willebrand disease.
Children and von Willebrand Disease
If your child has von Willebrand disease that’s severe enough to cause bleeding, anyone who cares for him or her should be told about the condition.
For example, the school nurse, teacher, daycare provider, coach, or any leader of after school activities should know, especially if your child has severe von Willebrand disease. This information will help them handle the situation if your child has an injury.
Von Willebrand disease complications
Complications of von Willebrand disease may include:
- Anemia. Women who experience heavy menstrual bleeding can develop iron deficiency anemia.
- Swelling and pain. If abnormal bleeding occurs in the joints or soft tissue, swelling and severe pain can result.
- Death from bleeding. Rarely, someone with von Willebrand disease may experience uncontrolled bleeding that can be life-threatening and needs emergency medical attention.
In a CDC study of 102 women with all types of von Willebrand disease compared to 88 controls 18:
- The most commonly reported bleeding symptoms among women with von Willebrand disease were:
- Heavy menstrual bleeding (95%)
- Bleeding after minor injuries (92%)
- Excessive gum bleeding (76%)
- 74% of women with von Willebrand disease reported excessive bleeding from several sites (e.g. nose, gum and uterus) or following several procedures or injuries (e.g. dental, surgical, childbirth and minor injury) compared to 6% of controls.
- 41% of women with von Willebrand disease reported a diagnosis of migraine headaches compared with 13% of controls.
- 37% of women with von Willebrand disease reported a diagnosis of arthritis compared with 15% of controls.
- 37% of women with von Willebrand disease compared with 10% of controls indicated that their menstrual period limited routine work, social activities and had a negative effect on life.
- More women with von Willebrand disease than controls in this study had undergone hysterectomy (25% vs. 9%).
In studies of 42 men and 38 women with Type 1 von Willebrand disease (the most common form) 19:
- The most common bleeding symptoms were heavy menstrual bleeding in women (93%) and nosebleeds in men (53%).
- 45% of women and 50% of men with von Willebrand disease reported excessive bruising.
- 40% of women and 47% of men with von Willebrand disease reported excessive bleeding with surgery.
- 34% of women and 29% of men with von Willebrand disease reported dental bleeding.
- 21% of women and 26% of men with von Willebrand disease had received a blood transfusion.
- 76% of men with von Willebrand disease had been diagnosed by age 10, but 50% of women with von Willebrand disease were not diagnosed until after age 12.
Von Willebrand disease causes
Von Willebrand disease can be inherited or acquired 20, 21. However, von Willebrand disease is almost always inherited. “Inherited” means that the disorder is passed from parents to children though genes.
You can inherit type 1 or type 2 von Willebrand disease (autosomal dominant disease) if only one of your parents passes the gene on to you (see Figure 3 above). You usually inherit type 3 von Willebrand disease (autosomal recessive disease) only if both of your parents pass the gene on to you (see Figure 4 above). Your symptoms may be different from your parents’ symptoms.
Some people have the genes for the disorder but don’t have symptoms. However, they still can pass the genes on to their children.
Some people get von Willebrand disease later in life as a result of other medical conditions. This type of von Willebrand disease is called acquired von Willebrand syndrome.
Mutations in the VWF gene cause von Willebrand disease. More than 300 mutations in the VWF gene have been found to cause von Willebrand disease. The VWF gene provides instructions for making a blood clotting protein called von Willebrand factor, which is essential for the formation of blood clots. After an injury, clots protect the body by sealing off damaged blood vessels and preventing further blood loss. Von Willebrand factor acts as a glue to hold blood clots together and prevents the breakdown of other blood clotting proteins. If von Willebrand factor does not function normally or too little of the protein is available, blood clots cannot form properly. Abnormally slow blood clotting causes the prolonged bleeding episodes seen in von Willebrand disease.
The three types of von Willebrand disease are based upon the amount of von Willebrand factor that is produced. Mutations in the VWF gene that reduce the amount of von Willebrand factor cause type 1 von Willebrand disease. People with type 1 have varying amounts of von Willebrand factor in their bloodstream. Some people with a mild case of type 1 never experience a prolonged bleeding episode. Mutations that disrupt the function of von Willebrand factor cause the four subtypes of type 2 von Willebrand disease. People with type 2 von Willebrand disease have bleeding episodes of varying severity depending on the extent of von Willebrand factor dysfunction, but the bleeding episodes are typically similar to those seen in type 1. Mutations that result in an abnormally short, nonfunctional von Willebrand factor generally cause type 3 von Willebrand disease. Because there is no functional protein, people with type 3 von Willebrand disease usually have severe bleeding episodes.
Many people with von Willebrand disease also have low levels of Factor 8 (factor VIII), another protein that helps in clotting. Factor 8 (factor VIII) is involved in another inherited clotting disorder called hemophilia. But unlike hemophilia, which mainly affects males, von Willebrand disease affects males and females and is usually milder.
Rarely, von Willebrand disease can develop later in life in people who didn’t inherit an affected gene from a parent. This is known as acquired von Willebrand syndrome, and it’s likely caused by an underlying medical condition.
Von Willebrand disease pathophysiology
Von Willebrand factor is a multimer formed from a basic dimer subunit. It is produced in megakaryocytes and endothelial cells. The size of the multimer determines the physiological hemostatic effect. Bigger multimers are more active and even prothrombic. They are cleaved by circulating proteases into smaller units. These larger multimers are stored in cytoplasmic granules and released in response to a trigger such as thrombin, fibrin, and histamine.
Larger multimers have more available sites for binding to platelets and endothelium. Von Willebrand factor increases factor VIII half-life by preventing its degradation. Regarding the subtypes, type I is characterized by a mild decrease in von Willebrand factor antigen (Ag), von Willebrand factor activity, and VIII:C.
Of note, von Willebrand factor levels of less than 30% are required for a diagnosis of Von Willebrand disease. Conversely, type III is characterized by a significant decrease in the parameters above.
A qualitative decrease with specific variations characterizes type 2 von Willebrand disease:
- Type 2A: variable decrease in von Willebrand factor Ag and VIII:C with a significant decrease in von Willebrand factor activity and absence of large and intermediate size multimers.
- Type 2B: variable decrease in von Willebrand factor Ag and VIII:C and a significant decrease in von Willebrand factor activity and absence of large multimers. However, most importantly, this type is hypersensitive to ristocetin-induced platelet aggregation (RIPA).
- Type M: vWF activity is decreased relative to Ag and multimers are present.
- Type N: this is characterized variably by a decrease in vWF Ag and activity but is distinguished from the other types by the significant decrease in VIII: C, albeit usually more than 5%. This specific subtype can be confused with hemophilia A.
Von Willebrand disease prevention
Because von Willebrand disease is usually an inherited disorder, consider having genetic counseling if you have a family history of this condition and you’re planning to have children. If you carry the defective gene for von Willebrand disease, you can pass it on to your offspring, even if you don’t have symptoms.
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Von Willebrand disease symptoms
The signs and symptoms of von Willebrand disease depend on which type of the disorder you have. They also depend on how serious the disorder is. Many people have such mild symptoms that they don’t know they have von Willebrand disease.
If you have type 1 or type 2 von Willebrand disease, you may have the following mild-to-moderate bleeding symptoms:
- Frequent, large bruises from minor bumps or injuries
- Frequent or hard-to-stop nosebleeds. Nosebleeds that don’t stop within 10 minutes
- Prolonged bleeding from the gums after a dental procedure
- Heavy or prolonged menstrual bleeding in women
- Blood in your stools from bleeding in your intestines or stomach
- Blood in your urine from bleeding in your kidneys or bladder
- Heavy bleeding after a cut or other accident
- Heavy bleeding after surgery
People who have type 3 von Willebrand disease may have all of the symptoms listed above and severe bleeding episodes for no reason. These bleeding episodes can be fatal if not treated right away. People who have type 3 von Willebrand disease also may have bleeding into soft tissues or joints, causing severe pain and swelling.
Heavy menstrual bleeding often is the main symptom of von Willebrand disease in women. Doctors call this menorrhagia. They define it as:
- Bleeding with clots larger than about 1-inch (2.5 centimeters) in diameter
- Anemia (low red blood cell count) or low blood iron
- The need to change pads or tampons more than every hour
- The need to use double sanitary protection to control menstrual flow
However, just because a woman has heavy menstrual bleeding doesn’t mean she has von Willebrand disease.
Von Willebrand disease diagnosis
The accurate and timely diagnosis of von Willebrand disease remains a challenge for clinicians and patients. Mild forms of von Willebrand disease can be difficult to diagnose because bleeding is common, and, for most people, doesn’t indicate a disease. However, if your doctor suspects you have a bleeding disorder, he or she might refer you to a blood disorders specialist (hematologist).
Early diagnosis of von Willebrand disease is important to make sure that you’re treated and can live a normal, active life.
Sometimes von Willebrand disease is hard to diagnose. People who have type 1 or type 2 von Willebrand disease may not have major bleeding problems. Thus, they may not be diagnosed unless they have heavy bleeding after surgery or some other trauma.
On the other hand, type 3 von Willebrand disease can cause major bleeding problems during infancy and childhood. So, children who have type 3 von Willebrand disease usually are diagnosed during their first year of life.
To find out whether you have von Willebrand disease, your doctor will review your medical history and the results from a physical exam and tests.
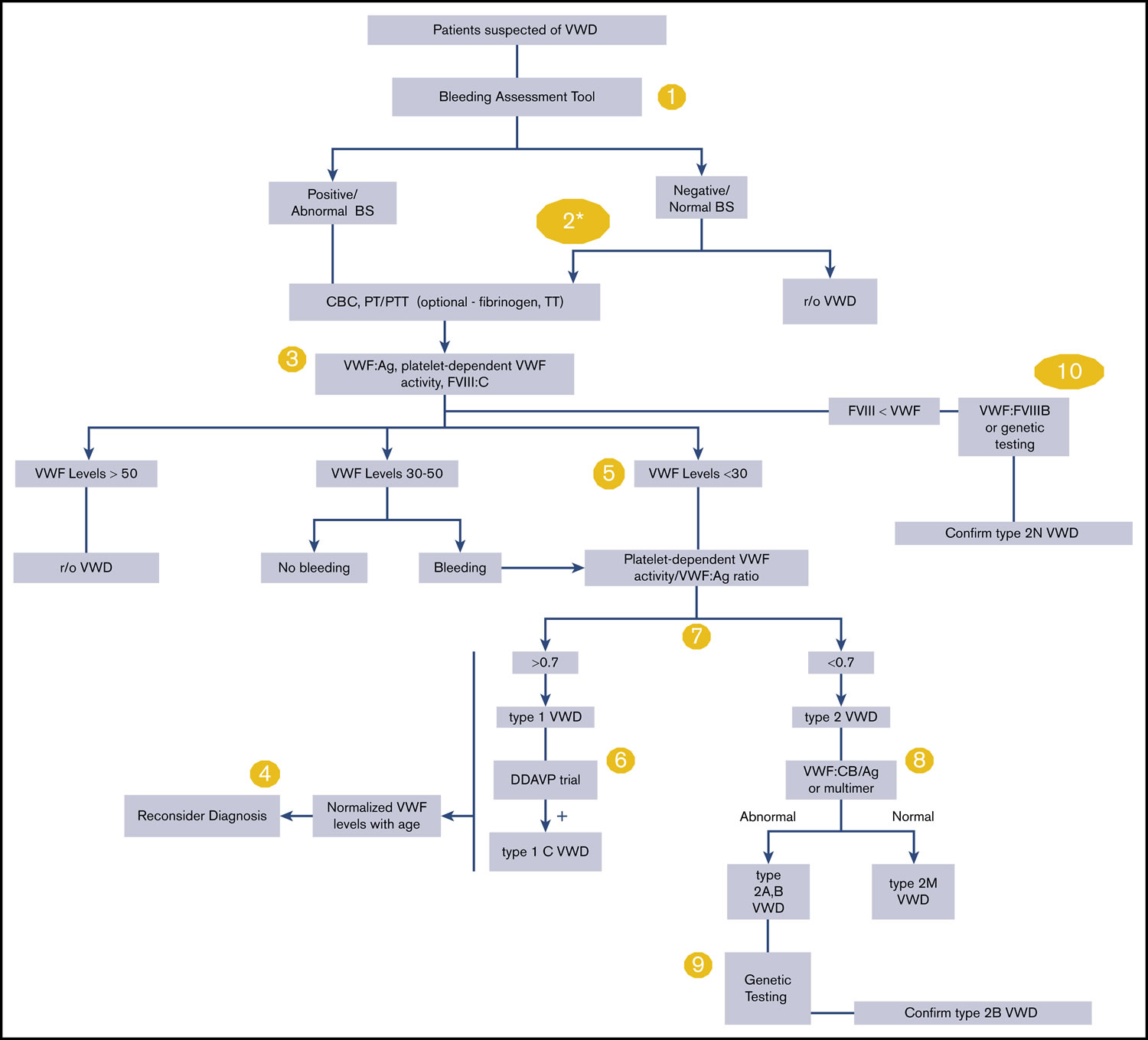
Figure 5. Von Willebrand disease diagnostic algorithm
Footnotes: The numbers in the yellow circles correspond to guideline questions. von Willebrand factor (VWF) levels refer to VWF antigen (VWF:Ag) and/or platelet-dependent VWF activity. The algorithm says von Willebrand factor (VWF) level 30 to 50 for simplicity; this refers to VWF levels of 0.30 to 0.50 IU/mL, with the caveat that the lower limit of the normal range as determined by the local laboratory should be used if it is <0.50 IU/mL.
*Men and children, referred to a hematologist and/or first-degree relative affected with von Willebrand disease.
Abbreviations: BS = bleeding score; CBC = complete blood count; DDAVP = desmopressin; FVIII = Factor 8; FVIII:C = Factor 8 coagulant activity; PT = prothrombin time; PTT = partial thromboplastin time; r/o = rule out; TT = thrombin time; VWF:CB/Ag = ratio of VWF collagen binding to antigen; VWD = von Willebrand disease; VWF:FVIIIB = VWF Factor 8 binding.
[Source 1 ]Medical History
Your doctor will likely ask questions about your medical history and your family’s medical history. He or she may ask about:
- Any bleeding from a small wound that lasted more than 15 minutes or started up again within the first 7 days following the injury.
- Any prolonged, heavy, or repeated bleeding that required medical care after surgery or dental extractions.
- Any bruising with little or no apparent trauma, especially if you could feel a lump under the bruise.
- Any nosebleeds that occurred for no known reason and lasted more than 10 minutes despite pressure on the nose, or any nosebleeds that needed medical attention.
- Any blood in your stools for no known reason.
- Any heavy menstrual bleeding (for women). This bleeding usually involves clots or lasts longer than 7 to 10 days.
- Any history of muscle or joint bleeding.
- Any medicines you’ve taken that might cause bleeding or increase the risk of bleeding. Examples include aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), clopidogrel, warfarin, or heparin.
- Any history of liver or kidney disease, blood or bone marrow disease, or high or low blood platelet counts.
Physical Exam
Your doctor will do a physical exam to look for unusual bruising or other signs of recent bleeding. He or she also will look for signs of liver disease or anemia (a low red blood cell count).
Diagnostic Tests
No single test can diagnose von Willebrand disease. Your doctor may recommend one or more blood tests to diagnose the disorder. These tests may include:
- Von Willebrand factor antigen (VWF:Ag). This test measures the amount of von Willebrand factor in your blood.
- Von Willebrand factor ristocetin cofactor activity (VWF:RCo). This test shows how well your von Willebrand factor works.
- Factor 8 (factor VIII) clotting activity. This test checks the clotting activity of Factor 8 (factor VIII). Some people who have von Willebrand disease have low levels of factor VIII activity, while others have normal levels.
- Von Willebrand factor multimers. This test is done if one or more of the first three tests are abnormal. This test evaluates the structure of von Willebrand factor in your blood, its protein complexes and how its molecules break down. The test helps your doctor diagnose what type of von Willebrand disease you have.
- Platelet function test. This test measures how well your platelets are working.
You may have these tests more than once to confirm a diagnosis because the results of these tests can fluctuate in the same person over time due to factors such as stress, exercise, infection, pregnancy and medications. So you might need to repeat some tests.
Your doctor also may refer you to a hematologist to confirm the diagnosis and for followup care. A hematologist is a doctor who specializes in diagnosing and treating blood disorders.
If you have von Willebrand disease, your doctor might suggest that family members undergo tests to determine if this condition runs in your family.
Von Willebrand disease treatment
Treatment for von Willebrand disease is based on the type of von Willebrand disease you have and how severe it is including how you’ve responded to previous therapy, your other medications and conditions. Most cases of von Willebrand disease are mild, and you may need treatment only if you have surgery, tooth extraction, or an accident.
Medicines are used to:
- Increase the amount of von Willebrand factor and Factor 8 (factor VIII) released into the bloodstream
- Replace von Willebrand factor
- Prevent the breakdown of blood clots
- Control heavy menstrual bleeding in women
Desmopressin
One treatment for von Willebrand disease is a man-made hormone called desmopressin, similar to the natural hormone vasopressin. You usually take this hormone by injection or nasal spray. Desmopressin is available as an injection (DDAVP) or nasal spray (Stimate). It controls bleeding by stimulating your body to release more von Willebrand factor and factor VIII into your bloodstream that are already stored in the lining of your blood vessels. DDAVP is usually effective in people with type 1 von Willebrand disease and some subtypes of type 2 von Willebrand disease.
Many doctors consider DDAVP the first treatment to use in the management of von Willebrand disease. Some women use the nasal spray (Stimate) at the beginning of their menstrual periods to control excessive bleeding. It can also be effective when used before a minor surgical procedure.
Replacement therapies
Another type of treatment is von Willebrand factor replacement therapy. This involves an infusion of concentrated von Willebrand factor and factor VIII into a vein in your arm. This treatment may be used if you:
- Can’t take desmopressin or need extended treatment
- Have type 1 von Willebrand disease that doesn’t respond to desmopressin
- Have type 2 or type 3 von Willebrand disease
Recombinant von Willebrand factor (such as Vonvendi®) and medicines rich in von Willebrand factor (VWF) and factor VIII (for example, Humate P®, Wilate®, Alphanate®, or Koate DVI®) are used to treat people with more severe forms of von Willebrand disease or people with milder forms of von Willebrand disease who do not respond well to the nasal spray 7. These medicines are injected into a vein in the arm to replace the missing factor in the blood.
Clot-stabilizing medications
Antifibrinolytic medicines (for example, aminocaproic acid, tranexamic acid) also are used to treat von Willebrand disease. These medicines help prevent the breakdown of blood clots. They’re mostly used to stop bleeding after minor surgery, tooth extraction, or an injury. These medicines may be used alone or with desmopressin and replacement therapy.
Drugs applied to cuts
A fibrin sealant (Tisseel VHSD) placed directly on a cut helps curtail bleeding. Fibrin glue is medicine that’s placed directly on a wound using syringes to stop bleeding.
Treatments for Women
Treatments for women who have von Willebrand disease with heavy menstrual bleeding include:
- Birth control pills. The hormones in these pills can increase the amount of von Willebrand factor and factor VIII in your blood. The hormones also can reduce menstrual blood loss. Birth control pills are the most recommended birth control method for women who have von Willebrand disease.
- A levonorgestrel intrauterine device. This is a birth control device that contains the hormone progestin. The device is placed in the uterus (womb).
- Aminocaproic acid or tranexamic acid. These antifibrinolytic medicines can reduce bleeding by slowing the breakdown of blood clots.
- Desmopressin nasal spray.
For some women who are done having children or don’t want children, endometrial ablation is done. This procedure destroys the lining of the uterus. It has been shown to reduce menstrual blood loss in women who have von Willebrand disease.
If you need a hysterectomy (surgical removal of the uterus) for another reason, this procedure will stop menstrual bleeding and possibly improve your quality of life. However, hysterectomy has its own risk of bleeding complications.
Home remedies
These self-care tips can help you manage your condition:
- Switch pain relievers. To help prevent bleeding episodes, talk with your doctor before taking blood-thinning medications — such as aspirin, ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, Anaprox). Your doctor may instead recommend pain and fever relievers such as acetaminophen (Tylenol, others).
- Tell your doctors and dentist. Let your doctors or dentist know that you have von Willebrand disease before you have any type of surgery, start a new medication or give birth. Also mention whether anyone in your family has a history of excessive bleeding.
- Consider wearing a medical ID bracelet. Make sure it notes that you have von Willebrand disease, which will be helpful to medical personnel if you’re ever in an accident or taken to an emergency room. Also carry a medical alert card in your wallet.
- Be active and safe. Exercise as part of attaining or maintaining a healthy weight. Avoid activities that could cause bruising, such as football, wrestling and hockey.
von Willebrand disease prognosis
For most affected individuals, von Willebrand disease is a mild, manageable bleeding disorder in which clinically severe bleeding only seen with trauma or invasive procedures. However, significant variability of symptomatology exists among family members.
In individuals with von Willebrand disease types 2 and 3, bleeding episodes may be severe and potentially life threatening. Individuals with type 3 disease who have correspondingly low Factor 8 (factor VIII) levels may develop joint complications, as more commonly seen in hemophilia A patients with comparably decreased Factor 8 (factor VIII) levels.
Levels of von Willebrand factor (VWF) normally increase with age. However, Sanders and colleagues 22 found that although von Willebrand factor (VWF) levels increased with aging in patients with type 1 von Willebrand disease, elderly patients with type 1 reported no change in their pattern of bleeding did not change. In patients with type 2 von Willebrand disease, von Willebrand factor (VWF) levels did not increase with aging, and eldelry patients reported significantly more bleeding symptoms 22.
References- Paula D. James, Nathan T. Connell, Barbara Ameer, Jorge Di Paola, Jeroen Eikenboom, Nicolas Giraud, Sandra Haberichter, Vicki Jacobs-Pratt, Barbara Konkle, Claire McLintock, Simon McRae, Robert R. Montgomery, James S. O’Donnell, Nikole Scappe, Robert Sidonio, Veronica H. Flood, Nedaa Husainat, Mohamad A. Kalot, Reem A. Mustafa; ASH ISTH NHF WFH 2021 guidelines on the diagnosis of von Willebrand disease. Blood Adv 2021; 5 (1): 280–300. doi: https://doi.org/10.1182/bloodadvances.2020003265
- Rodeghiero F, Castaman G, Dini E. Epidemiological investigation of the prevalence of von Willebrand’s disease. Blood. 1987 Feb;69(2):454-9. https://doi.org/10.1182/blood.V69.2.454.454
- Werner EJ, Broxson EH, Tucker EL, Giroux DS, Shults J, Abshire TC. Prevalence of von Willebrand disease in children: a multiethnic study. J Pediatr. 1993 Dec;123(6):893-8. doi: 10.1016/s0022-3476(05)80384-1
- What is von Willebrand Disease? https://www.cdc.gov/ncbddd/vwd/facts.html
- Laffan MA, Lester W, O’Donnell JS, Will A, Tait RC, Goodeve A, Millar CM, Keeling DM. The diagnosis and management of von Willebrand disease: a United Kingdom Haemophilia Centre Doctors Organization guideline approved by the British Committee for Standards in Haematology. Br J Haematol. 2014 Nov;167(4):453-65. doi: 10.1111/bjh.13064
- The Diagnosis, Evaluation, and Management of von Willebrand Disease. Bethesda, Md: National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/diagnosis-evaluation-and-management-of-von-willebrand-disease/von-willebrand-disease-full-report
- Gill JC, Castaman G, Windyga J, Kouides P, Ragni M, Leebeek FW, Obermann-Slupetzky O, Chapman M, Fritsch S, Pavlova BG, Presch I, Ewenstein B. Hemostatic efficacy, safety, and pharmacokinetics of a recombinant von Willebrand factor in severe von Willebrand disease. Blood. 2015 Oct 22;126(17):2038-46. doi: 10.1182/blood-2015-02-629873
- O’Brien, SH, Stanek, JR, Kaur, D, McCracken, K, Vesely, SK. Laboratory monitoring during pregnancy and post-partum hemorrhage in women with von Willebrand disease. J Thromb Haemost. 2020; 18: 604– 608. https://doi.org/10.1111/jth.14696
- Basnet S, Lin C, Dhital R, et al. Acquired von Willebrand Disease Associated with Monoclonal Gammopathy of Unknown Significance. Case Reports in Oncological Medicine. 2017;2017:9295780. doi:10.1155/2017/9295780. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5687136/
- Gavva C., Patel P., Shen Y.-M., Frenkel E., Sarode R. A case of autoimmune severe acquired von Willebrand syndrome (type 3-like) Transfusion and Apheresis Sciences. 2017;56(3):431–433. doi: 10.1016/j.transci.2017.04.006. https://www.ncbi.nlm.nih.gov/pubmed/28512017
- Federici A. B., Rand J. H., Bucciarelli P., et al. Subcommittee on von Willebrand factor. Acquired von Willebrand syndrome: data from an international registry. Thrombosis and Haemostasis. 2000;84(2):345–349. https://www.ncbi.nlm.nih.gov/pubmed/10959711
- Mital A. Acquired von Willebrand syndrome. Advances in Clinical and Experimental Medicine. 2016;25(6):1337–1344. doi: 10.17219/acem/64942. https://www.ncbi.nlm.nih.gov/pubmed/28028990
- Tiede A. Diagnosis and treatment of acquired von Willebrand syndrome. Thrombosis Research. 2012;130(2):S2–S6. doi: 10.1016/S0049-3848(13)70003-3. https://www.ncbi.nlm.nih.gov/pubmed/23439003
- Qamar H., Lee A., Valentine K., Skeith L., Jimenez-Zepeda V. H. Acquired von Willebrand syndrome associated to secondary IgM MGUS emerging after autologous stem cell transplantation for AL amyloidosis. Mediterranean Journal of Hematology and Infectious Diseases. 2017;9(1):p. e2017034. doi: 10.4084/MJHID.2017.034. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5419196/
- Tefferi A., Nichols W. L. Acquired von Willebrand disease: concise review of occurrence, diagnosis, pathogenesis, and treatment. American Journal of Medicine. 1997;103(6):536–540. doi: 10.1016/s0002-9343(97)00239-8. https://www.ncbi.nlm.nih.gov/pubmed/9428838
- Nitu-Whalley I. C., Lee C. A. Acquired von Willebrand syndrome–report of 10 cases and review of the literature. Haemophilia. 1999;5(5):318–326. doi: 10.1046/j.1365-2516.1999.00340.x. https://www.ncbi.nlm.nih.gov/pubmed/10583513
- Acquired von Willebrand Syndrome. Adv Clin Exp Med 2016, 25, 6, 1337–1344. http://www.advances.umed.wroc.pl/pdf/2016/25/6/1337.pdf
- Kirtava, A., Drews, C., Lally, C., Dilley, A. and Evatt, B. (2003), Medical, reproductive and psychosocial experiences of women diagnosed with von Willebrand’s disease receiving care in haemophilia treatment centres: a case–control study. Haemophilia, 9: 292-297. https://doi.org/10.1046/j.1365-2516.2003.00756.x
- Data and Statistics on von Willebrand Disease. https://www.cdc.gov/ncbddd/vwd/data.html
- Petricevic M, Knezevic J, Samoukovic G, Bradaric B, Safradin I, Mestrovic M, Papestiev V, Hodalin A, Madzar T, Mihalj M, Rotim A, Biocina B. Diagnosis and Management of Acquired von Willebrand Disease in Heart Disease: A Review of the Literature. Thorac Cardiovasc Surg. 2020 Apr;68(3):200-211. doi: 10.1055/s-0038-1673670
- Mezzano, D, Quiroga, T. Diagnostic challenges of inherited mild bleeding disorders: a bait for poorly explored clinical and basic research. J Thromb Haemost 2019; 17: 257– 70. https://doi.org/10.1111/jth.14363
- Sanders, YV, Giezenaar, MA, Laros-van Gorkom, BAP, Meijer, K, van der Bom, JG, Cnossen, MH, Nijziel, MR, Ypma, PF, Fijnvandraat, K, Eikenboom, J, Mauser-Bunschoten, EP, Leebeek, FWG, for the WiN study group. von Willebrand disease and aging: an evolving phenotype. J Thromb Haemost 2014; 12: 1066– 75. https://doi.org/10.1111/jth.12586