What is nutcracker esophagus
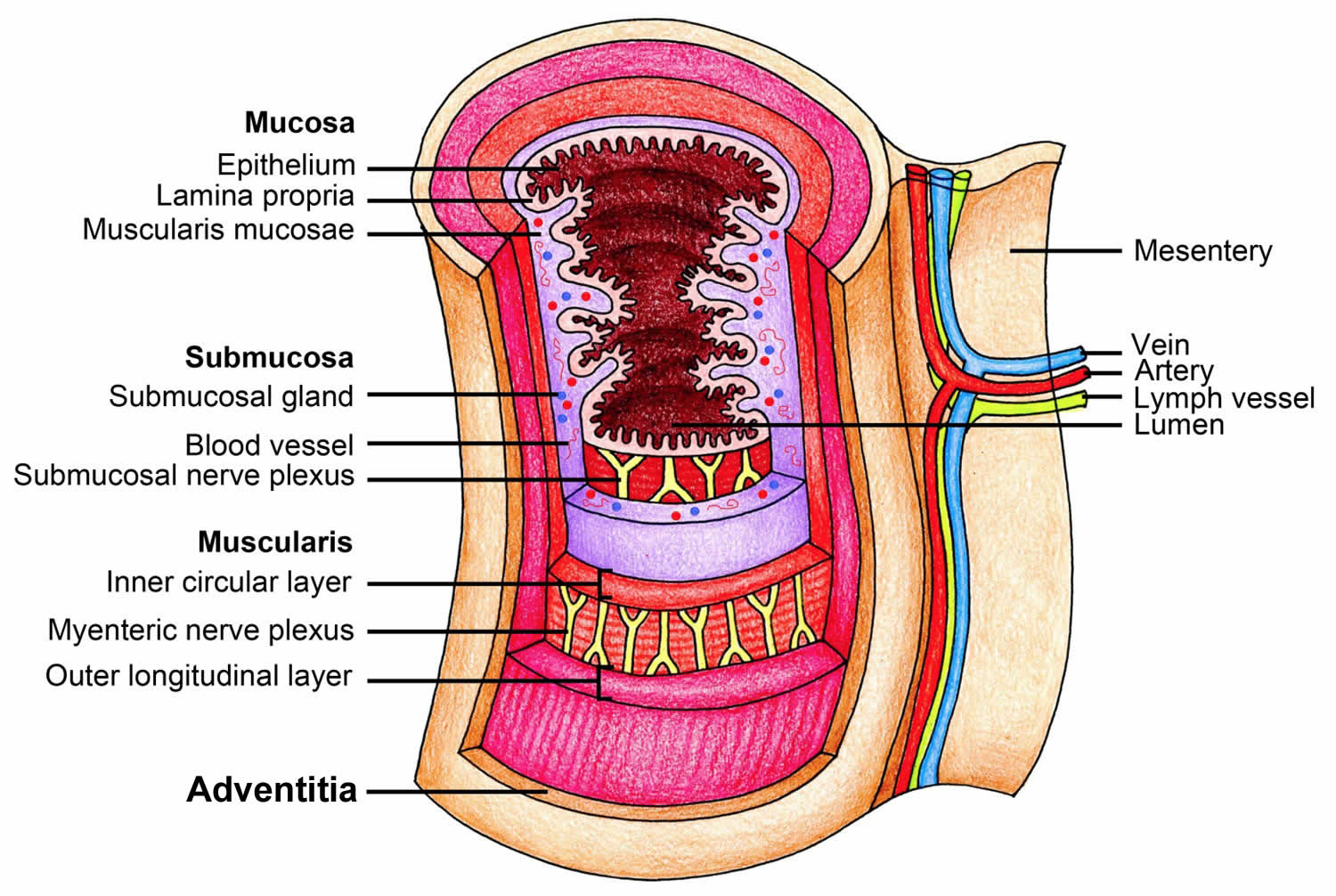
The esophagus is the hollow, muscular tube that moves food and liquid from your mouth to your stomach (see Figure 1). If the muscles in your esophagus don’t squeeze properly, it will be harder for the food and liquids to reach your stomach. This condition is known as an esophageal motility disorder. Esophageal motility disorders make it difficult for you to swallow, cause food to come back up into your mouth, and sometime cause chest pain. One type of esophageal motility disorder is achalasia. Achalasia occurs when the nerves in the esophagus degenerate 1. As a result, the muscles in the esophagus stop working (no peristalsis), and the valve at the bottom of the esophagus doesn’t open. The condition is believed to affect 1-2 people in every 100,000, with about 3,000 new cases diagnosed each year in the United States.
Other less common dysmotility disorders include spastic esophageal motility disorder like “nutcracker esophagus” or hypertensive peristalsis also called “jackhammer esophagus”. The nutcracker esophagus is defined by high amplitude peristaltic contractions in the distal esophagus and can be associated with dysphagia and/or chest pain. Hypertensive esophageal peristaltic contractions (“nutcracker esophagus”) are among the most common reported findings in clinical manometric studies 2. The term, nutcracker esophagus, was coined in conventional manometry (measurement of muscle pressure and movements in the esophagus) with mean distal esophageal peristaltic amplitude (measured 3 cm and 8 cm above the esophagogastric junction) greater than 180 mm Hg in the context of normal lower esophageal sphincter relaxation 3.
There is currently no standardized diagnostic or management plan for these diseases 4. Due to the diagnostic complexity for the nutcracker esophagus the median time patients experienced symptoms prior to diagnosis was 24 months (0–480 months) 5. The median age of patients was 62 years (range 25–87 years), and 63% were female 5. Furthermore, there was no statistically significant correlation between esophageal motility parameters and symptoms.
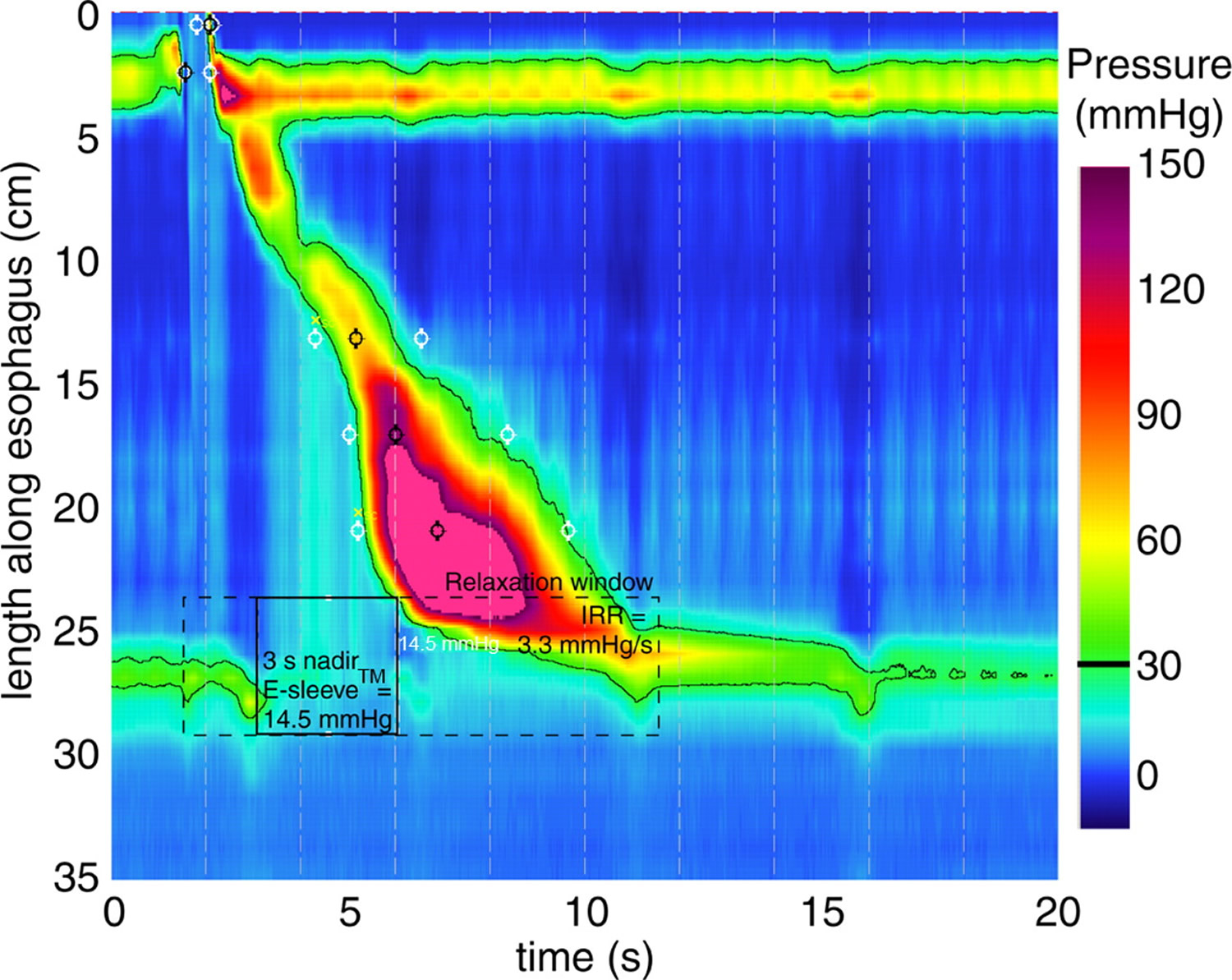
In the case of nutcracker esophagus, there is a pattern of esophageal hypercontractility causally linked to dysphagia or pain that is not consistent with achalasia or esophageal spasm. Unlike the case of esophageal spasm, there were no characteristic fluoroscopic abnormalities. The manometric criterion for nutcracker esophagus were initially an average peristaltic amplitude of greater than 180 mm Hg in the distal esophagus 6. The most recent published criterion for nutcracker esophagus applicable to conventional manometry suggests a mean peristaltic amplitude of 180 mmHg measured 3 and 8 cm proximal to the lower esophageal sphincter measured in 10 test swallows 7. Subsequently, this threshold value was increased to 220 mm Hg in hopes of improving specificity. With the era of high-resolution manometry and high resolution esophageal pressure topography, peristaltic amplitude was replaced by the distal contractile integral as the summary metric of the vigor of the distal esophageal contraction. If the entire distal esophageal contraction is envisioned as a solid with the height of the peaks corresponding to peristaltic amplitude and the footprint corresponding to the length of the involved esophagus and the duration of the contraction, the distal contractile integral (DCI), expressed as Hg-s-cm, is the volume of that solid above a 20–mm Hg minimum. A distal contractile integral mean value of 5000 mm Hg-s-cm (hypertensive peristalsis in the Chicago classification) approximately corresponds to nutcracker esophagus in conventional manometry 6. Even that value is seen in up to 5% of normal subjects, however, making it inherently nonspecific. Alternatively, an extreme observable characteristic of hypertensive contractions was described based on the occurrence of at least one contraction with a distal contractile integral greater than 8000 mm Hg-s-cm, a value never observed in controls 8. This was termed, esophageal hypercontractility or the jackhammer esophagus. Although still somewhat heterogeneous (the pattern is sometimes seen with esophagogastric junction outflow obstruction), this extreme observable characteristic is likely more clinically relevant than hypertensive peristalsis (nutcracker esophagus). Hypercontractility is commonly associated with multipeaked contractions, sometimes resulting in distal contractile integral values in excess of 50,000 mm Hg-s-cm.
Additional manometric features of nutcracker esophagus that may be relevant include prolonged or repetitive contractions 9.
- Esophageal hypercontractility is defined in esophageal pressure topography by the occurrence of a propagated swallow-induced contraction with distal contractile integral > 8,000 mmHg-s-cm, a magnitude never encountered in control subjects
- Hypercontractility, nicknamed Jackhammer esophagus because it is usually associated with multipeaked contractions, is rare (4.1% of a referral practice) and is usually associated with dysphagia
- Subsets of patients with Jackhammer Esophagus had this associated with esophagogastric junction outflow obstruction, reflux disease, or as an apparent primary abnormality of hypercontractility.
High-resolution esophageal manometry
Manometry has long been the test of choice for assessing esophageal motor function, especially for evaluating the common esophageal complaints of dysphagia and noncardiac chest pain. In patients, it also is useful for identifying achalasia and gastroesophageal reflux disease (GERD) and for evaluating swallowing difficulties and esophageal changes in scleroderma.
Two types of manometry systems can be used to evaluate the esophagus.
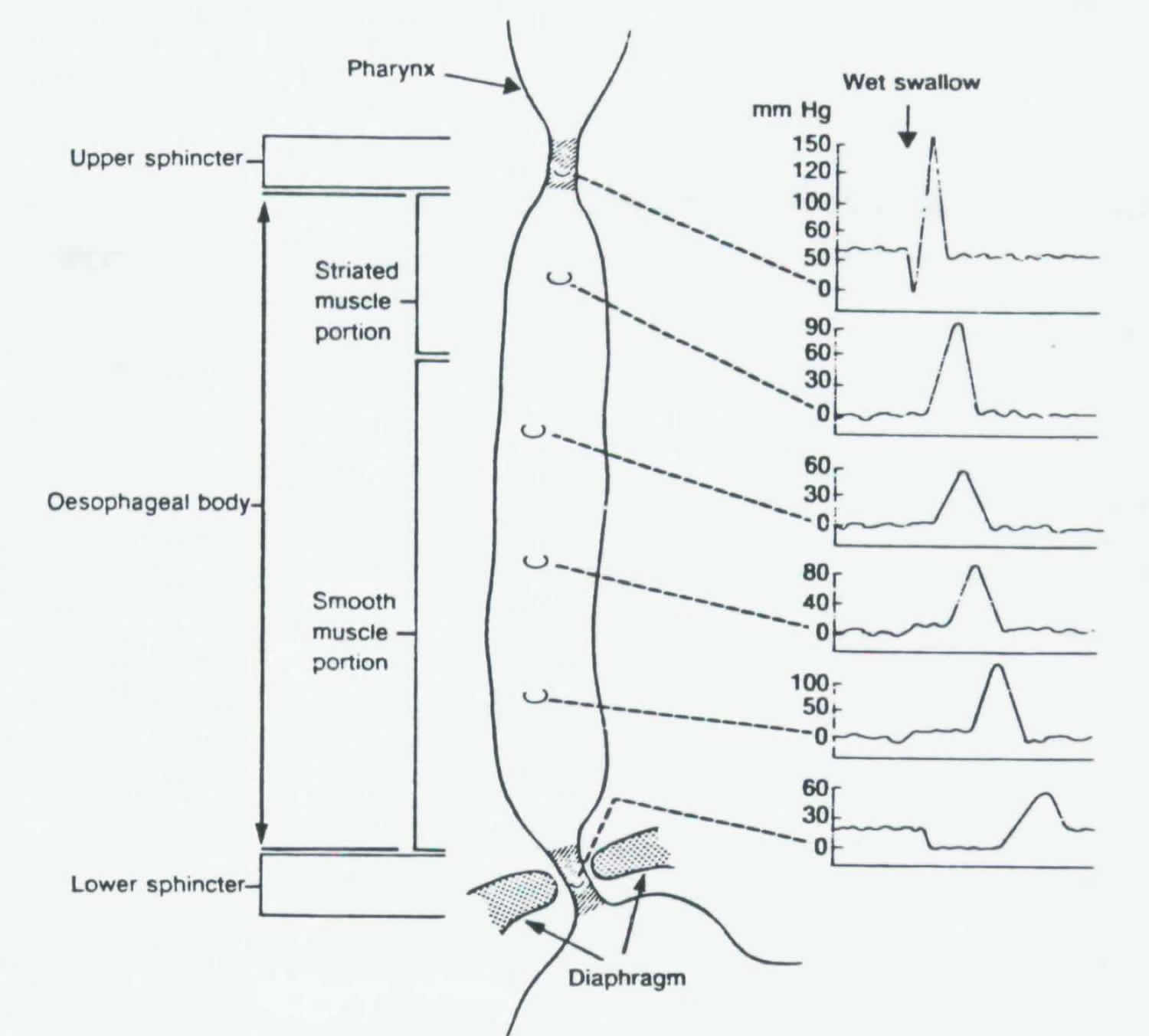
Conventional manometry uses a water perfused catheter with five to eight sensors displaying point pressure in the form of stacked line tracings (see Figure 3). Because of the limited number of sensors and the distance between them, the catheter must be repeatedly repositioned in order to obtain a complete study, making the procedure especially time-consuming and uncomfortable for patients. Further, accurate interpretation of manometry data, even in experienced centers, can be challenging.
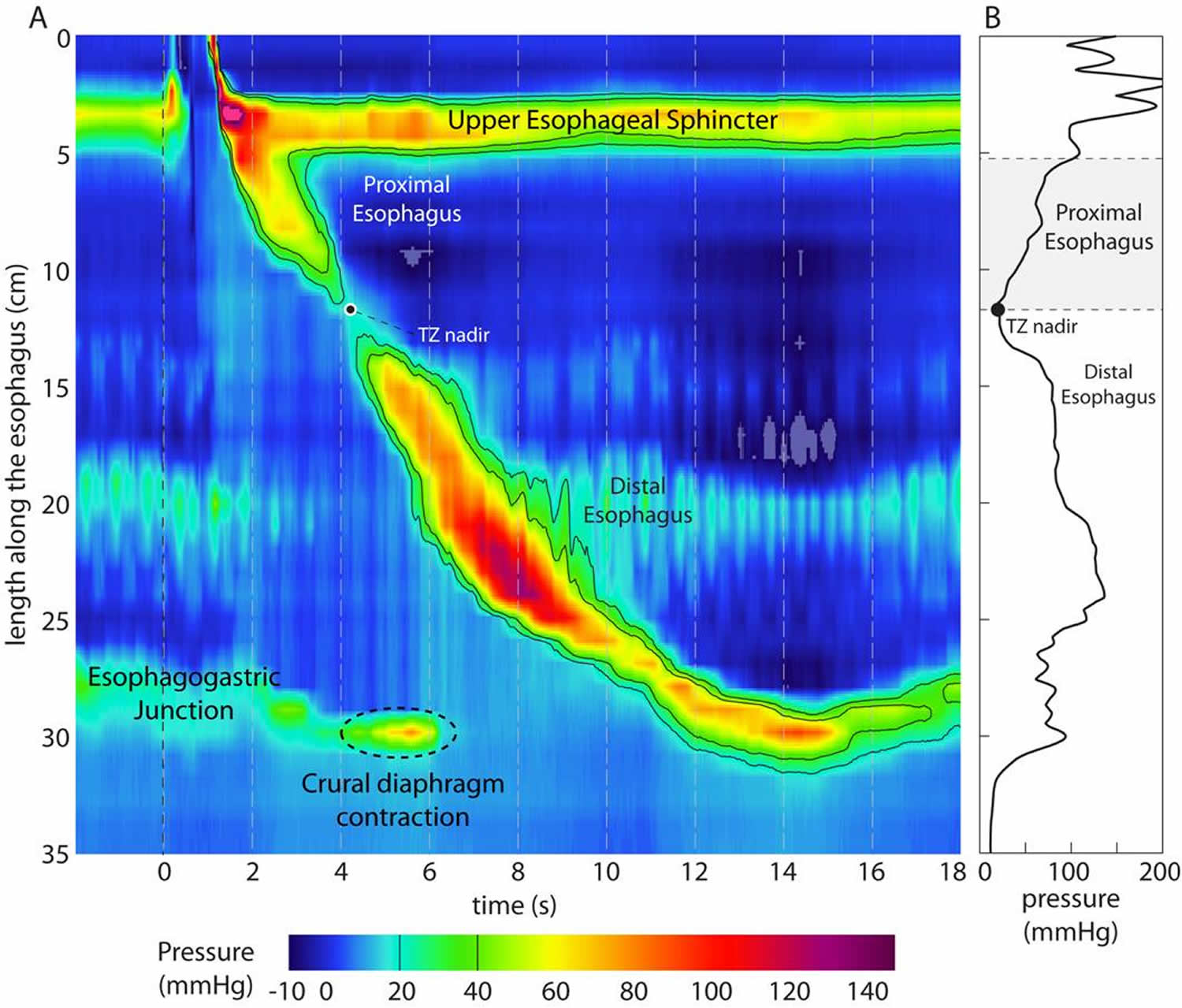
High-resolution manometry (HRM) with esophageal pressure topography (EPT) was designed to overcome these limitations (see Figure 4). High-resolution manometry uses 24 to 36 sensors spaced 1 centimeter apart, allowing readings of both sphincters and the entire esophagus simultaneously in real time. To better visualize this data, esophageal pressure topography (EPT), a 3-D plotting format, represents pressure changes visually, with cool colors (blue and green) signifying low pressure and warm colors (orange and red) denoting higher pressure. Time and location within the esophagus are continuous variables, with pressure magnitude indicated at each coordinate by color. This creates an isobaric contour map that more closely aligns esophageal pressure topography (EPT) with imaging techniques than data analysis. Combined with intraluminal impedance monitoring, which measures the flow of liquids and air in the esophagus, high-resolution manometry and esophageal pressure topography (EPT) provide a far more complete study than can be obtained with conventional manometry.
Both conventional and high-resolution manometry can determine the pressure of the upper and lower esophageal sphincters and whether or not a swallow is peristaltic. But the motor function of the esophagus can be described in greater detail using high-resolution manometry and the Chicago Classification of esophageal motility disorders, which uses an algorithmic scheme to analyze high-resolution manometry studies.
Two commonly used measurements are the integrative relaxation pressure (IRP) and the distal contractile integral (DCI). The integrative relaxation pressure (IRP) measures the effectiveness of the esophagogastric junction (EGJ) relaxation during swallow by measuring the average minimum pressure for four of the 10 seconds following a swallow. The distal contractile integral (DCI) measures the vigor of the esophageal contraction by combining the length of the esophagus with the contractile amplitude and duration.
The Chicago Classification
The Chicago Classification of esophageal motility was developed to facilitate the interpretation of clinical high resolution esophageal pressure topography (EPT) studies, concurrent with the widespread adoption of this technology into clinical practice 10. The Chicago Classification is an algorithmic scheme for diagnosis of esophageal motility disorders from clinical high resolution esophageal pressure topography (EPT) studies. The Chicago Classification continually evolves through the workings of an international working group 11.
The terms necessary to utilize the Chicago Classification of EPT studies are detailed in Table 1.
Note: All pressures referenced to atmospheric pressure except the integrated relaxation pressure (IRP), which is referenced to gastric pressure.
Table 1. Esophageal pressure topography metrics utilized in the Chicago Classification
| Pressure Topography Metrics | |
|---|---|
| Metric | Description |
| IRP (mmHg) Integrated Relaxation Pressure | Mean EGJ pressure measured with an electronic equivalent of a sleeve sensor for 4 contiguous or non-contiguous seconds of relaxation in the ten-second window following deglutitive UES relaxation. |
| DCI (mraHg-s-cm) Distal Contractile Integral | Amplitude × duration × length (mmHg-s-cm) of the distal esophageal contraction greater than 20 mmHg from proximal (P) to distal (D) pressure troughs. |
| CDP (time, position) Contractile Deceleration Point | The inflection point along the 30 mmHg isobaric contour where propagation velocity slows demarcating the tubular esophagus from the phrenic ampulla |
| CFV (cm/s) Contractile Front Velocity | Slope of the tangent approximating the 30 mmHg isobaric contour between P and the CDP |
| DL(s) Distal Latency | Interval between UES relaxation and the CDP |
| Peristaltic breaks (cm) | Gaps in the 20 mmHg isobaric contour of the peristaltic contraction between the UES and EGJ, measured in axial length |
Figure 1. Esophagus
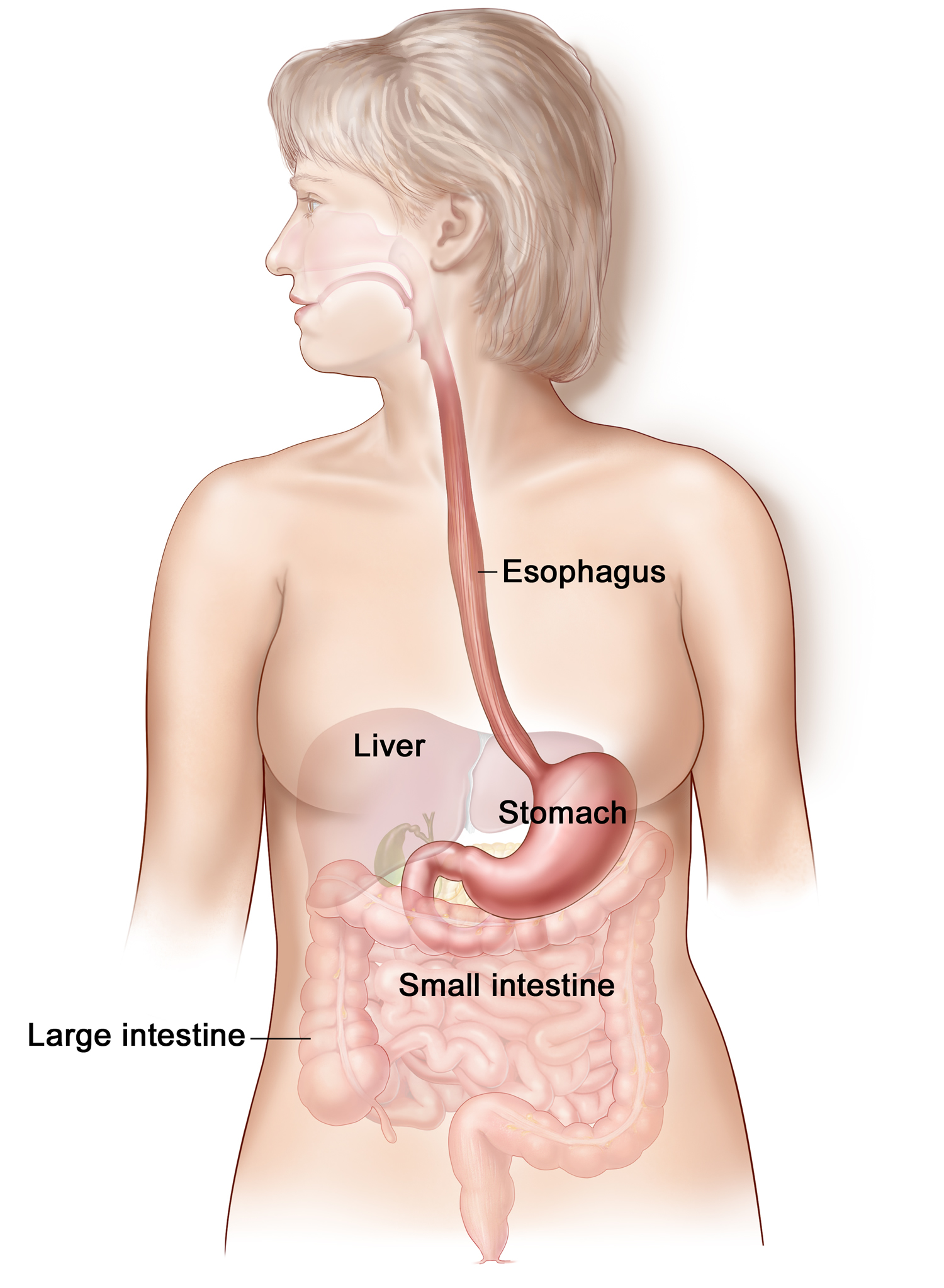
Figure 2. Esophagus anatomy
Figure 3. Esophagus conventional manometry
Figure 4. Esophagus high resolution manometry (HRM)
Figure 5. Nutcracker esophagus manometry
Note: A patient with a spastic nutcracker pattern in the distal esophagus had a shorter relaxation duration resulting in an abnormal integrated relaxation resistance (IRR), whereas the 3-s nadir eSleeve was normal.
[Source 13]It the past it was initially hypothesized that nutcracker esophagus might represent a causal explanation for unexplained chest pain or dysphagia. However subsequent analyses have concluded that, most often, this was not the case 14. The finding lacked specificity, frequently encountered in gastroesophageal reflux patients 15, patients with hypersensitivity 16, and normal controls.
Causes of nutcracker esophagus
The pathophysiology of esophageal hypercontractility likely involves an excess of cholinergic drive 6. Temporal asynchrony between the contractions of circular and longitudinal muscle layers of the muscularis propria have been observed with high-frequency intraluminal ultrasound in patients with nutcracker esophagus 17. This asynchrony was reversed with atropine 18. The observations of Loo and colleagues 19 in diabetics with autonomic neuropathy are also an indirect argument for an excess of cholinergic stimulation. Multipeaked contractions occurred more frequently in diabetics with neuropathy than in control subjects or diabetics without neuropathy. Multipeaked contractions became single-peak contraction after atropine injection. Multipeaked contractions are also a common finding in jackhammer esophagus 20. It remains to be determined if atropine may change the multipeaked pattern in such patients. Finally, as with diffuse esophageal spasm, increased muscle thickness has been observed in patients with nutcracker esophagus and with esophageal hypercontractility 21.
Association with Other Conditions:
Psychiatric comorbidity occurred in 24% with half the patients receiving psychotropic medications 5. Irritable bowel syndrome (IBS) and fibromyalgia co-existed in 15% and 12% of patients, respectively 5.
Gastroesophageal Reflux Disease and Eosinophilic Esophagitis
In a series of 45 patients with nutcracker esophagus (conventional manometry), 47% had abnormal acid exposure time on pH-metry, 4% had endoscopic esophagitis, and 16% positive symptom index 22. Finally, reflux esophagitis has also been observed in patients with jackhammer esophagus and the hypercontractile pattern can resolve with of proton pump inhibitor therapy 23.
Jackhammer esophagus was also associated with eosinophilic esophagitis in 3 of 41 patients (7%) who underwent endoscopy with mucosal biopsies 23.
Nutcracker esophagus symptoms
Presenting symptoms were chest pain (31%) and dysphagia (21%). Gastroesophageal reflux disease (GERD) symptoms were common: heartburn occurred in 51% of patients, 77% had a prior history of GERD, and 78% were receiving acid suppressive medications. GERD was confirmed by testing in at least 35%. Hence, the clinical evaluation needs to prioritize identifying more morbid conditions and more prevalent conditions before pursuing these rare, nonfatal conditions. When chest pain is among the presenting symptoms, the evaluation should first prioritize excluding heart attack owing to its potentially life-threatening nature.
Even within the realm of esophageal chest pain, gastroesophageal reflux (GERD) is a more common cause than spastic disorders. Using the more refined criteria of the Chicago classification, the combined prevalence of diffuse esophageal spasm, spastic achalasia, and jackhammer is even lower, approximately 2% 24. Consequently, evaluation of suspected esophageal spastic disorders requires a thorough evaluation to first identify or exclude other potential causes of esophageal chest pain.
Nutcracker esophagus treatment
In a sham-controlled trial of 22 patients with diffuse esophageal spasm or nutcracker esophagus, thus far reported only in abstract form, injection of toxin botulinum in the distal esophagus was superior to placebo in improving dysphagia 25.
In another study involving 3 patients with nutcracker esophagus using peroral endoscopic myotomy (POEM) 26. Peroral endoscopic myotomy (POEM) was performed under general anesthesia on the distal esophagus and upper stomach. At 3 months, 6 months and 1 year postoperatively all patients had clinical follow-up, barium swallow and high-resolution manometry. All patients displayed marked improvement with a significant reduction in Eckardt score at follow-up after 1 year. However, during follow-up, the patients were diagnosed with increased reflux index and one patient was diagnosed with gastroparesis 26.
- Achalasia and Esophageal Motility Disorders. The Society of Thoracic Surgeons. https://ctsurgerypatients.org/lung-esophageal-and-other-chest-diseases/achalasia-and-esophageal-motility-disorders[↩]
- Esophageal testing of patients with noncardiac chest pain or dysphagia. Results of three years’ experience with 1161 patients. Katz PO, Dalton CB, Richter JE, Wu WC, Castell DO. Ann Intern Med. 1987 Apr; 106(4):593-7. https://www.ncbi.nlm.nih.gov/pubmed/3826958/[↩]
- Classification of oesophageal motility abnormalities. Spechler SJ, Castell DO. Gut. 2001 Jul; 49(1):145-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1728354/[↩]
- Nutcracker and jackhammer esophagus treatment: a three-case survey, including two novel cases of eosinophilic infiltration into the muscularis propria. Endoscopy. 2015 Sep;47(9):855-7. doi: 10.1055/s-0034-1391985. Epub 2015 May 11. https://www.ncbi.nlm.nih.gov/pubmed/25961439[↩]
- R. Lufrano, M. G. Heckman, N. Diehl, K. R. DeVault, S. R. Achem; Nutcracker esophagus: demographic, clinical features, and esophageal tests in 115 patients, Diseases of the Esophagus, Volume 28, Issue 1, 1 January 2015, Pages 11–18, https://doi.org/10.1111/dote.12160[↩][↩][↩][↩]
- Roman S, Kahrilas PJ. Management of Spastic Disorders of the Esophagus. Gastroenterology clinics of North America. 2013;42(1):27-43. doi:10.1016/j.gtc.2012.11.002. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3618975/[↩][↩][↩]
- Classification of oesophageal motility abnormalities. Spechler SJ, Castell DO. Gut. 2001 Jul; 49(1):145-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1728354/pdf/v049p00145.pdf[↩]
- Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Roman S, Pandolfino JE, Chen J, Boris L, Luger D, Kahrilas PJ. Am J Gastroenterol. 2012 Jan; 107(1):37-45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641840/[↩]
- SPECHLER S, CASTELL D. Classification of oesophageal motility abnormalities. Gut. 2001;49(1):145-151. doi:10.1136/gut.49.1.145. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1728354/pdf/v049p00145.pdf[↩]
- Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago Classification Criteria of Esophageal Motility Disorders Defined in High Resolution Esophageal Pressure Topography (EPT). Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society. 2012;24(Suppl 1):57-65. doi:10.1111/j.1365-2982.2011.01834.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3544361/[↩]
- High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ. Neurogastroenterol Motil. 2009 Aug; 21(8):796-806. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892003/[↩]
- Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago Classification Criteria of Esophageal Motility Disorders Defined in High Resolution Esophageal Pressure Topography (EPT). Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society. 2012;24(Suppl 1):57-65. doi:10.1111/j.1365-2982.2011.01834.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3544361/ [↩]
- Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. American Journal of Physiology – Gastrointestinal and Liver Physiology Published 5 October 2007 Vol. 293 no. 4, G878-G885 DOI: 10.1152/ajpgi.00252.2007. http://ajpgi.physiology.org/content/293/4/G878[↩]
- Agrawal A, Hila A, Tutuian R, et al. Clinical relevance of the nutcracker esophagus: suggested revision of criteria for diagnosis. J Clin Gastroenterol. 2006;40:504–9. https://www.ncbi.nlm.nih.gov/pubmed/16825932[↩]
- Borjesson M, Pilhall M, Rolny P, et al. Gastroesophageal acid reflux in patients with nutcracker esophagus. Scand J Gastroenterol. 2001;36:916–20. https://www.ncbi.nlm.nih.gov/pubmed/11521980[↩]
- Mujica VR, Mudipalli RS, Rao SS. Pathophysiology of chest pain in patients with nutcracker esophagus. Am J Gastroenterol. 2001;96:1371–7. https://www.ncbi.nlm.nih.gov/pubmed/11374670[↩]
- Jung HY, Puckett JL, Bhalla V, et al. Asynchrony between the circular and the longitudinal muscle contraction in patients with nutcracker esophagus. Gastroenterology. 2005;128(5):1179–86. https://www.ncbi.nlm.nih.gov/pubmed/15887102[↩]
- Korsapati H, Bhargava V, Mittal RK. Reversal of asynchrony between circular and longitudinal muscle contraction in nutcracker esophagus by atropine. Gastroenterology. 2008;135(3):796–802. https://www.ncbi.nlm.nih.gov/pubmed/18675815[↩]
- Loo FD, Dodds WJ, Soergel KH, et al. Multipeaked esophageal peristaltic pressure waves in patients with diabetic neuropathy. Gastroenterology. 1985;88(2):485–91. https://www.ncbi.nlm.nih.gov/pubmed/3965338[↩]
- Roman S, Pandolfino JE, Chen J, et al. Phenotypes and clinical context of hypercontractility in high resolution pressure topography (EPT) Am J Gastroenterol. 2012;107(1):37–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641840/[↩]
- Dogan I, Puckett JL, Padda BS, et al. Prevalence of increased esophageal muscle thickness in patients with esophageal symptoms. Am J Gastroenterol. 2007;102(1):137–45. https://www.ncbi.nlm.nih.gov/pubmed/17266691[↩]
- Gastroesophageal acid reflux in patients with nutcracker esophagus. Börjesson M, Pilhall M, Rolny P, Mannheimer C. Scand J Gastroenterol. 2001 Sep; 36(9):916-20. https://www.ncbi.nlm.nih.gov/pubmed/11521980/[↩]
- Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Roman S, Pandolfino JE, Chen J, Boris L, Luger D, Kahrilas PJ. Am J Gastroenterol. 2012 Jan; 107(1):37-45. https://www.ncbi.nlm.nih.gov/pubmed/21931377/[↩][↩]
- Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Am J Gastroenterol. 2008 Jan; 103(1):27-37. https://www.ncbi.nlm.nih.gov/pubmed/17900331/[↩]
- Vanuytsel T, Bisschops R, Holvoet L, et al. A sham-control study of injection of botulinum toxin in non achalasia esophageal hypermotility disorder. Gastroenterology. 2009;136(5 Suppl 1):A–152.[↩]
- Peroral endoscopic myotomy (POEM) for nutcracker esophagus. Three cases with 12 months follow-up. Scand J Gastroenterol. 2014 Nov;49(11):1285-9. doi: 10.3109/00365521.2014.958096. Epub 2014 Sep 16. https://www.ncbi.nlm.nih.gov/pubmed/25225846[↩][↩]