How to treat an open wound
A wound is any damage or break in the surface of the skin. Wounds include cuts, scrapes, scratches, and punctured skin. They often happen because of an accident, but surgery, sutures, and stitches also cause wounds. Minor wounds usually aren’t serious, but it is important to clean them. Serious and infected wounds may require first aid followed by a visit to your doctor. You should also seek attention if the wound is deep, you cannot close it yourself, you cannot stop the bleeding or get the dirt out, or it does not heal.
Types of wounds:
- Acute wounds are wounds that can include minor cuts, lacerations, bites, abrasions and surgical wounds.
- Chronic wounds are wounds that can become slow to heal including ulcers on the legs and feet. In the United States, chronic wounds affect around 6.5 million patients 1. It is claimed that an excess of US$25 billion is spent annually on treatment of chronic wounds and the burden is growing rapidly due to increasing health care costs, an aging population and a sharp rise in the incidence of diabetes and obesity worldwide 1.
Any wound is at risk of becoming infected because the skin opening can allow germs or dirt to enter the bloodstream. Infections can cause tenderness or pain, fever, redness, swelling and/or discharge. These infections can lead to further complications or surgery or even death if not treated properly. Applying appropriate first aid to a wound can speed up the healing process and reduce the risk of infection. As your skin heals, a scar may form, as this is a natural part of the healing process. The appearance of a scar often depends on how well the wound heals. While scars from surgery or over joints like the knees and elbows are hard to avoid, scars caused by minor cuts and scrapes can become less noticeable by properly treating the wound at home.
Wounds including minor cuts, lacerations, bites and abrasions can be treated with first aid.
Table 1. Treatment Options for Minor Wounds
| Wound type | Description | Clinical features | Treatment options |
|---|---|---|---|
Laceration | Straight or jagged skin tear; caused by blunt trauma (e.g., fall, collision) | Little to profuse bleeding; ragged edges may not readily align | Sutures, stapling, tissue adhesive, bandage, or skin closure tape |
Abrasion | Scraped skin caused by friction against a rough surface | Minimal bleeding; first- (epidermis only), second- (to dermis), or third-degree (to subcutaneous skin) injury | Skin irrigation and removal of foreign bodies, topical antibiotic, occlusive dressing; third-degree injuries may require topical and oral antibiotics and consultation with plastic surgeon for skin grafting |
Bite or puncture wound | Broken skin caused by penetration of sharp object | Typically more bleeding internally than externally, causing skin discoloration | High-pressure irrigation and removal of foreign bodies, tetanus prophylaxis with possible antibiotics; human bites to the hand require prophylactic antibiotics; plantar puncture wounds are susceptible to pseudomonal infection |
Burn | Thermal injury | Dynamic injury, may progress two to three days after initial injury | Depends on degree and size; in general, first-degree burns do not require therapy (topical nonsteroidal anti-inflammatory drugs and aloe vera can be helpful); deep second- and third-degree burns require topical antimicrobials and referral to burn subspecialist |
How to clean a wound
You can look after most cuts and wounds yourself. You can:
- Stop any bleeding by holding a clean cloth or bandage on it and apply firm pressure. Use a clean towel to apply light pressure to the area until bleeding stops (this may take a few minutes). Minor cuts and scrapes usually stop bleeding on their own. Be aware that some medicines (e.g. aspirin and warfarin) will affect bleeding, and may need pressure to be applied for a longer period of time. If needed, apply gentle pressure with a clean bandage or cloth and elevate the wound until bleeding stops.
- Wash your hands well. Prior to cleaning or dressing the wound, ensure your hands are washed to prevent contamination and infection of the wound.
- Clean the wound by rinsing it with clean water and picking out any dirt (e.g. gravel) or debris with tweezers (don’t use antiseptic cream), as this will reduce the risk of infection. Keeping the wound under running tap water will reduce the risk of infection. Wash around the wound with soap.
- Dry the wound. Gently pat dry the surrounding skin with a clean pad or towel.
- Replace any skin flaps if possible. If there is a skin flap and it is still attached, gently reposition the skin flap back over the wound as much as possible using a moist cotton bud or pad.
- To help the injured skin heal, use an antibiotic ointment (e.g., Neosporin, Polysporin) or petroleum jelly to keep the wound moist. Petroleum jelly prevents the wound from drying out and forming a scab; wounds with scabs take longer to heal. This will also help prevent a scar from getting too large, deep or itchy. As long as the wound is cleaned daily, it is not necessary to use anti-bacterial ointments. However, several studies have supported the use of prophylactic topical antibiotics for minor wounds. An randomized controlled trial of 426 patients with uncomplicated wounds found significantly lower infection rates with topical bacitracin, neomycin/bacitracin/polymyxin B, or silver sulfadiazine (Silvadene) compared with topical petrolatum (5.5%, 4.5%, 12.1%, and 17.6%, respectively) 3. Certain ingredients in some ointments can cause a mild rash in some people. If a rash appears, stop using the ointment.
- Cover the wound (small wounds can be left uncovered) 4. Use a non-stick or gentle dressing and lightly bandage in place; try to avoid using tape on fragile skin to prevent further trauma on dressing removal. Dressings protect the wound by acting as a barrier to infection and absorbing wound fluid. A moist wound bed stimulates epithelial cells to migrate across the wound bed and resurface the wound 5. A dry environment leads to cell desiccation and causes scab formation, which delays wound healing. Older studies in animals and humans suggest that moist wounds had faster rates of re-epithelialization compared with dry wounds 6.
- Manage pain. Wounds can be painful, so consider pain relief while the wound heals. Talk to your doctor or pharmacist about options for pain relief.
- Change the dressing every day or whenever the bandage becomes wet or dirty.
- Get a tetanus shot. Get a tetanus shot if you haven’t had one in the past five years and the wound is deep or dirty.
- Watch for signs of infection. See a doctor if you see signs of infection on the skin or near the wound, such as redness, increasing pain, drainage, warmth or swelling.
- It’s also important to care for yourself, as this helps wounds heal faster. So eat fresh food, get some exercise, avoid smoking, and avoid drinking too much and drink plenty of water (unless you have liquid intake restrictions) to maintain supple, healthy skin.
See a doctor or nurse for a tetanus immunization within a day if you have had any cut or abrasion and any of the following apply:
- It is more than 10 years since your last tetanus shot or you can’t remember when you last had a tetanus shot 7. The Centers for Disease Control and Prevention (CDC) recommends that tetanus toxoid be administered as soon as possible to patients who have no history of tetanus immunization, who have not completed a primary series of tetanus immunization (at least three tetanus toxoid–containing vaccines), or who have not received a tetanus booster in the past 10 years.
- It is more than five years since your last tetanus shot and there was dirt in in the cut or abrasion, or the cut is deep.
- You should have the tetanus booster shot within 48 hours of the injury.
- Besides a tetanus shot, your doctor may also give you an injection of something called tetanus immune globulin, which acts fast to prevent infection 8. There is a small window of opportunity for the tetanus immune globulin to work, so don’t delay seeking medical care.
- Be aware of the first signs of tetanus infection. Also known as lockjaw, tetanus causes stiffness of the neck, difficulty swallowing, rigidity of abdominal muscles, spasms, sweating and fever. Symptoms usually begin eight days after the infection, but occur anywhere within three days to three weeks.
Severe bleeding first aid
For severe bleeding, take these first-aid steps and reassure the injured person.
- Remove any clothing or debris on the wound. Don’t remove large or deeply embedded objects. Don’t probe the wound or attempt to clean it yet. Your first job is to stop the bleeding. Wear disposable protective gloves if available.
- Stop the bleeding. Place a sterile bandage or clean cloth on the wound. Press the bandage firmly with your palm to control bleeding. Apply constant pressure until the bleeding stops. Maintain pressure by binding the wound with a thick bandage or a piece of clean cloth. Don’t put direct pressure on an eye injury or embedded object. Secure the bandage with adhesive tape or continue to maintain pressure with your hands. If possible, raise an injured limb above the level of the heart.
- Help the injured person lie down. If possible, place the person on a rug or blanket to prevent loss of body heat. Calmly reassure the injured person.
- Don’t remove the gauze or bandage. If the bleeding seeps through the gauze or other cloth on the wound, add another bandage on top of it. And keep pressing firmly on the area.
- Tourniquets: A tourniquet is effective in controlling life-threatening bleeding from a limb. Apply a tourniquet if you’re trained in how to do so. When emergency help arrives, explain how long the tourniquet has been in place.
- Immobilize the injured body part as much as possible. Leave the bandages in place and get the injured person to an emergency room as soon as possible.
Call your local emergency services number for emergency medical help for severe bleeding that you can’t control.
Puncture wounds first aid
A puncture wound, such as from stepping on a nail, doesn’t usually cause excessive bleeding. But these wounds are often deep and can be dangerous because of the risk of infection. To reduce the risk of infection, prompt treatment and close monitoring for signs of infection are important.
To take care of a puncture wound:
- Wash your hands. This helps avoid infection.
- Stop the bleeding. Apply gentle pressure with a clean bandage or cloth.
- Clean the wound. Rinse the wound with clear water for five to 10 minutes. If dirt or debris remains in the wound after washing, use tweezers cleaned with alcohol to remove the particles. See a doctor if you can’t remove all of the debris. Clean the skin around the wound with soap and a washcloth.
- Apply an antibiotic. Apply a thin layer of an antibiotic cream or ointment (Neosporin, Polysporin). Certain ingredients in some ointments can cause a mild rash in some people. If a rash appears, stop using the ointment and seek medical care.
- Cover the wound. Bandages help keep the wound clean.
- Change the dressing. Do this at least once a day or whenever the bandage becomes wet or dirty.
- Watch for signs of infection. See a doctor if the wound isn’t healing or you notice any redness, increasing pain, drainage, warmth or swelling.
You should see a doctor if:
- you are unsure how to manage the wound, or have any concerns.
- you can’t properly clean the dirt, glass, a thorn or other foreign body in the wound
- you have cut your hand from punching something or the cut is over a joint
- the wound is more than a few millimeters deep and/or the sides of the cut don’t sit together well by themselves (i.e. the wound “gapes”). These may need to be closed with stitches, tissue glue or staples
- the wound is deep, dirty or caused by a metal object
- the wound is in, or near, your eye
- the pain gets worse
- the redness and swelling is increasing
- you develop a temperature
- the wound is the result of an animal or human bite
- the cut or abrasion was sustained in dirty water
- you have diabetes
- you have an underlying medical condition
- the wound shows signs of infection
- the wound continues to bleed after a few minutes of direct pressure
- you are unable to realign the skin
- the wound seems large or deep
- the wound is not healing, or is very slow to heal (e.g. not healed after 4 weeks)
- you have another injury or hit your head at the time of the injury (you may have a concussion or fracture)
- there is a risk of further injury
- the wound was caused by a cat or a dog, try to confirm that its rabies vaccination is up to date. If it was caused by a wild animal, seek advice from your doctor about which animals are most likely to carry rabies.
Bacterial infections will have the following signs, ranked in order of severity, and should be treated by your physician:
- Area around the wound is warm/hot
- Area becomes red and swollen
- Pus or white/yellow drainage
- Red lines running up the extremity from the wound
- Sudden increase in pain
- Severe tenderness
- Fever.
Any of the following signs of infection require emergency attention to prevent it from spreading to your entire body and jeopardizing your life:
- Circulation decreases; the extremity feels cool/cold
- Wound or area smells bad
- Swollen glands in groin or armpits
- Wound has thick, brown/gray discharge
- Skin around the wound turns black or gangrenous.
When does a wound require hospitalization?
Most wounds can be managed by primary care clinicians in the outpatient setting. However, there are several reasons for hospitalization or referral to a wound care specialist 2:
Indications for Hospitalization and Referral for Wounds
- Hospitalization
- Failure of outpatient treatment
- Necrotizing fasciitis
- Nonadherence to outpatient therapy
- Poorly controlled diabetes mellitus or peripheral vascular disease; immunocompromised
- Severe cellulitis
- Systemic infection
- Worsening of wound
- Referral to a wound care specialist
- Severe or circumferential burns, or burns to the face or appendages
- Wounds affecting joints, bones, tendons, or nerves
- Wounds to large areas of the body
- Wounds to the face
Patients with severe wound infections may require treatment with intravenous antibiotics, with possible referral for exploration, incision, drainage, imaging, or plastic surgery 9.
Patients with severe, full-thickness, or circumferential burns, or those that affect the appendages or face should be referred to a burn center, if available.
What is a puncture wound?
Puncture wounds are not the same as cuts. A puncture wound has a small entry hole caused by a pointed object, such as a nail that you have stepped on. In contrast, a cut is an open wound that produces a long tear in the skin. Puncture wounds require different treatment from cuts because these small holes in the skin can disguise serious injury.
Puncture wounds are common in the foot, especially in warm weather when people go barefoot. But even though they occur frequently, puncture wounds of the foot are often inadequately treated. If not properly treated, infection or other complications can develop.
Proper treatment within the first 24 hours is especially important with puncture wounds because they carry the danger of embedding the piercing object (foreign body) under the skin. Research shows that complications can be prevented if the patient seeks professional treatment right away.
Foreign bodies in puncture wounds
A variety of foreign bodies can become embedded in a puncture wound. Nails, glass, toothpicks, sewing needles, insulin needles and seashells are some common ones. In addition, pieces of your own skin, sock and shoe can be forced into the wound during a puncture, along with dirt and debris from the object. All puncture wounds are dirty wounds because they involve penetration of an object that is not sterile. Anything that remains in the wound increases your chance of developing other problems, either in the near future or later.
Severity of wounds
There are different ways of determining the severity of a puncture wound. Depth of the wound is one way to evaluate it. The deeper the puncture, the more likely it is that complications, such as infection, will develop. Many patients cannot judge how far their puncture extends into the foot. Therefore, if you have stepped on something and the skin was penetrated, seek treatment as soon as possible.
The type and cleanliness of the penetrating object also determine the severity of the wound. Larger or longer objects can penetrate deeper into the tissues, possibly causing more damage. The dirtier an object, such as a rusty nail, the more dirt and debris are dragged into the wound, increasing the chance of infection.
Another thing that can determine wound severity is if you were wearing socks and shoes, particles of which can get trapped in the wound.
Avoiding complications
Follow the foot and ankle surgeon’s instructions for care of the wound to prevent complications.
- Infection is a common complication of puncture wounds that can lead to serious consequences.
- Sometimes a minor skin infection evolves into a bone or joint infection, so you should look for these signs:
- A minor skin infection may develop two to five days after injury.
- The signs of a minor infection that show up around the wound include soreness, redness and possibly drainage, swelling and warmth. You may also develop a fever.
- If these signs have not improved, or if they reappear in 10 to 14 days, a serious infection in the joint or bone may have developed.
- Other complications that may arise from inadequate treatment of puncture wounds include painful scarring in the area of the wound or a hard cyst where the foreign body has remained in the wound.
- Although the complications of puncture wounds can be quite serious, early and proper treatment can play a crucial role in preventing them.
Puncture wound treatment
A puncture wound must be thoroughly cleaning and monitored throughout the healing process to avoid complications. The sooner you do this, the better—within 24 hours after injury, if possible. The surgeon will make sure the wound is properly cleaned and no foreign body remains. He or she may numb the area, thoroughly clean inside and outside the wound, and monitor your progress. In some cases, x-rays may be ordered to determine whether something remains in the wound or if bone damage has occurred. Antibiotics may be prescribed if necessary.
Prophylactic antibiotic use may reduce the incidence of infection in human bite wounds 11. Prophylactic oral antibiotics are generally prescribed for deep puncture wounds and wounds involving the palms and fingers 2.
How to clean an infected wound
Wounds often become colonized by normal skin flora (gram-positive cocci, gram-negative bacilli, and anaerobes), but most immunocompetent patients will not develop an infection 2. An infected wound will disrupt tissue granulation and delay healing. Superficial mild infections can be treated with topical antibiotics; other infections require oral or intravenous antibiotics. Penetrating wounds from bites or other materials may introduce other types of bacteria. The goal of treatment is to eliminate the bacteria without further damage to the underlying tissue.
Symptoms of infection may include redness, swelling, warmth, fever, pain, lymphangitis, lymphadenopathy, and purulent discharge 12. The treatment of wound infections depends on the severity of the infection, type of wound, and type of pathogen involved. Treatment may include debridement and wound dressings that promote granulation, tissue preservation, and moisture. Empiric antibiotic treatment should be based on the potentially causative organism. Superficial mild infections can be treated with topical agents, whereas mild and moderate infections involving deeper tissues should be treated with oral antibiotics. Most severe infections, and moderate infections in high-risk patients, require initial parenteral antibiotics 13. Cultures should be obtained for wounds that do not respond to empiric therapy, and in immunocompromised patients 13.
Evaluating the extent and severity of the infection will help determine the proper treatment course. The Infectious Diseases Society of America 14 uses several clinical indicators to help stage the severity of wounds: those without purulence or inflammation are considered noninfected, and infected wounds are classified as mild, moderate, or severe based on their size and depth, surrounding cellulitis, tissue involvement, and presence of systemic or metabolic findings (Table 2).
Table 2. Classification of Wound Severity and Treatment Strategies
| Severity | Signs and symptoms | Treatment | Special considerations |
|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MRSA = methicillin-resistant Staphylococcus aureus.
Treatment for an infected wound should begin with cleansing the area with sterile saline. Debridement can be performed using surgical techniques or topical agents that lead to enzymatic breakdown or autolysis of necrotic tissue. Five randomized controlled trials with a total of 159 patients found weak evidence that enzymatic debridement leads to faster results compared with saline-soaked dressings 15. Elevation of the affected area and optimal treatment of underlying predisposing conditions (e.g., diabetes mellitus) will help the healing process 13.
Antibiotic Selection
Superficial mild infections (e.g., impetigo, mild cellulitis from abrasions or lacerations) are usually caused by staphylococci and streptococci and can be treated with topical antimicrobials, such as bacitracin, polymyxin B/bacitracin/neomycin, and mupirocin (Bactroban) 16. Metronidazole gel 0.75% can be used alone or in combination with other antibiotics if anaerobes are suspected. There is limited evidence to suggest one topical agent over another, except in the case of suspected methicillin-resistant Staphylococcus aureus (MRSA) infection, in which mupirocin 2% cream or ointment is superior to other topical agents and certain oral antibiotics 15.
Empiric oral antibiotics should be considered for nonsuperficial mild to moderate infections 13. Most infections in nonpuncture wounds are caused by staphylococci and streptococci and can be treated empirically with a five-day course of a penicillinase-resistant penicillin, first-generation cephalosporin, macrolide, or clindamycin. Consensus guidelines recommend trimethoprim/sulfamethoxazole or tetracycline if methicillin-resistant S. aureus infection is suspected 13, although a Cochrane review found insufficient evidence that one antibiotic was superior for treating methicillin-resistant S. aureus–colonized nonsurgical wounds 17.
Moderate wound infections in immunocompromised patients and severe wound infections usually require parenteral antibiotics, with possible transition to oral agents 13. The choice of agent should be based on the potentially causative organism, history, and local antibiotic resistance patterns. For severe infections with potential methicillin-resistant S. aureus involvement, treatment should start with linezolid (Zyvox), daptomycin (Cubicin), or vancomycin 13.
Puncture Wounds
Serious complications from infected animal or human bites include septic arthritis, osteomyelitis, subcutaneous abscess, tendinitis, and bacteremia 13. Common organisms in domestic animal bite wounds include Pasteurella multocida, S. aureus, Bacteroides tectum, and Fusobacterium, Capnocytophaga, and Porphyromonas species. Human bite wounds may include streptococci, S. aureus, and Eikenella corrodens, in addition to many anaerobes 13. For mild to moderate infections, a five- to 10-day course of oral amoxicillin/clavulanate (Augmentin) is preferred. Doxycycline, tri-methoprim/sulfamethoxazole, or a fluoroquinolone plus clindamycin should be used in patients who are allergic to penicillin 13. For severe infections, parenteral ampicillin/sulbactam (Unasyn), cefoxitin, or ertapenem (Invanz) should be used. Because E. corrodens is resistant to most oral antibiotics, clenched-fist bite wounds should be treated with parenteral ampicillin/sulbactam 13.
Burns
Secondary infections from burns may progress rapidly because of loss of epithelial protection. These infections require broad-spectrum antibiotics that are active against gram-positive and gram-negative organisms, including S. aureus, Streptococcus pyogenes, Pseudomonas, Acinetobacter, and Klebsiella. Widespread fungal infection is a rare but serious complication of broad-spectrum antibiotic use in burns. In these cases, systemic antifungals with coverage of Candida, Aspergillus, and Zygomycetes should be considered 18.
Stages of wound healing
Wound healing is classically divided into four stages: hemostasis, inflammation, proliferation and tissue remodeling. In these four stages, there are complicated interactions within a complex network of profibrotic and antifibrotic molecules, such as growth factors, proteolytic enzymes and extracellular matrix proteins 19. Each molecule has its own function in the different phases of the wound healing process. As soon as an injury occurs, the process of hemostasis begins and the bleeding is controlled by the aggregation of platelets at the site of injury. The subsequent formation of a fibrin clot helps to stop the bleeding and provides a scaffold for the attachment and proliferation of cells. Growth factors and cytokines are mainly secreted by inflammatory cells and contribute to the initiation of the proliferative phase of wound healing. Later, angiogenesis and collagen synthesis, followed by tissue remodeling complete the stages of the wound healing process.
Wounds heal at different rates, and may depend on a number of factors such as:
- general state of health
- age – older skin repairs itself at a slower rate than younger skin
- pre-existing medical conditions, such as diabetes
- some types of vascular disease, immune diseases and cancer
- diet – skin needs good nutrition to repair
- stress and wellbeing
- medications – some may slow healing (discuss with doctor or pharmacist)
- further trauma to the wound, such as friction/rubbing or pressure
- smoking
- alcohol excess
- whether or not the wound becomes infected.
Most minor acute wounds heal well and can be managed at home with appropriate first aid.
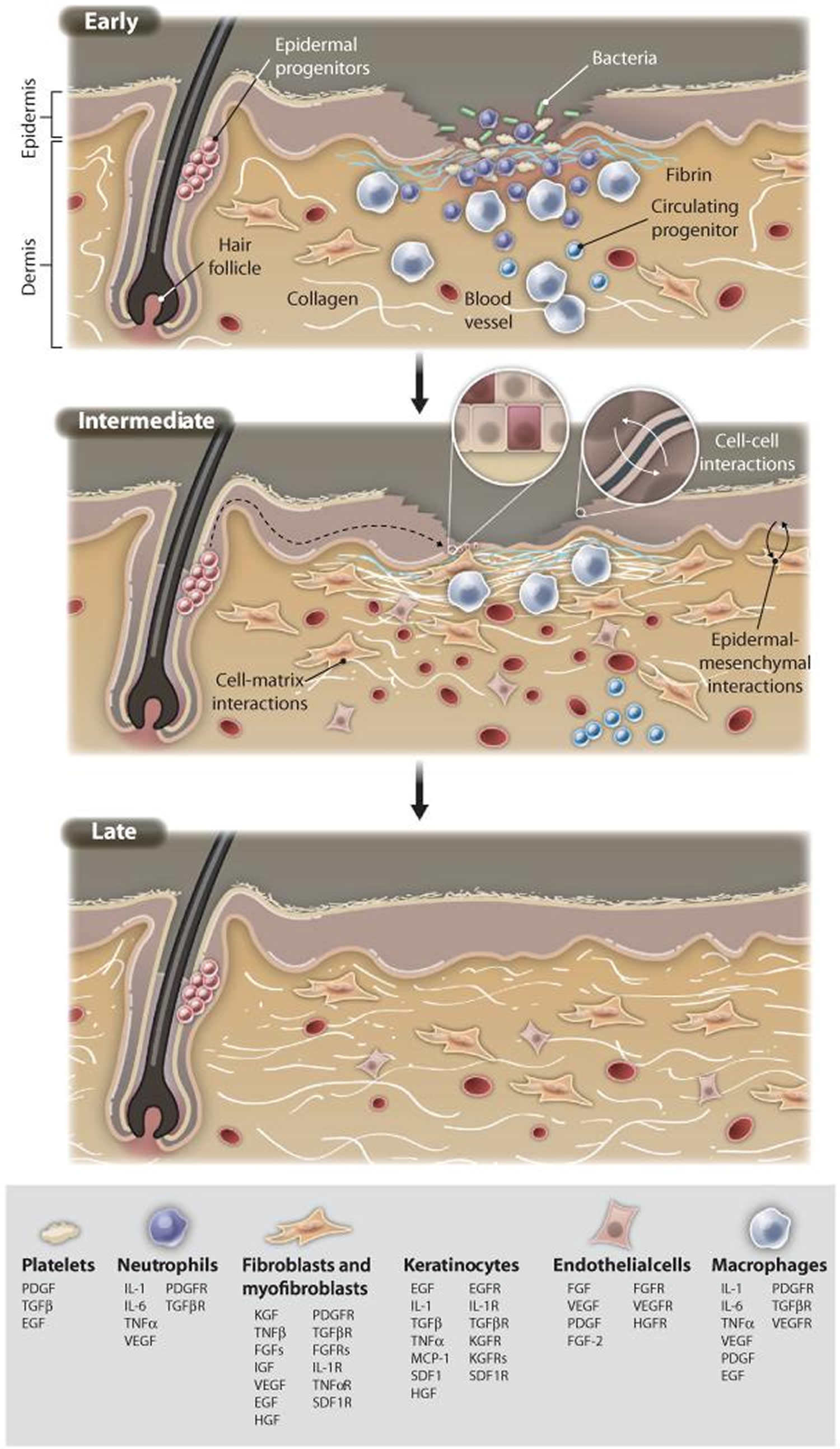
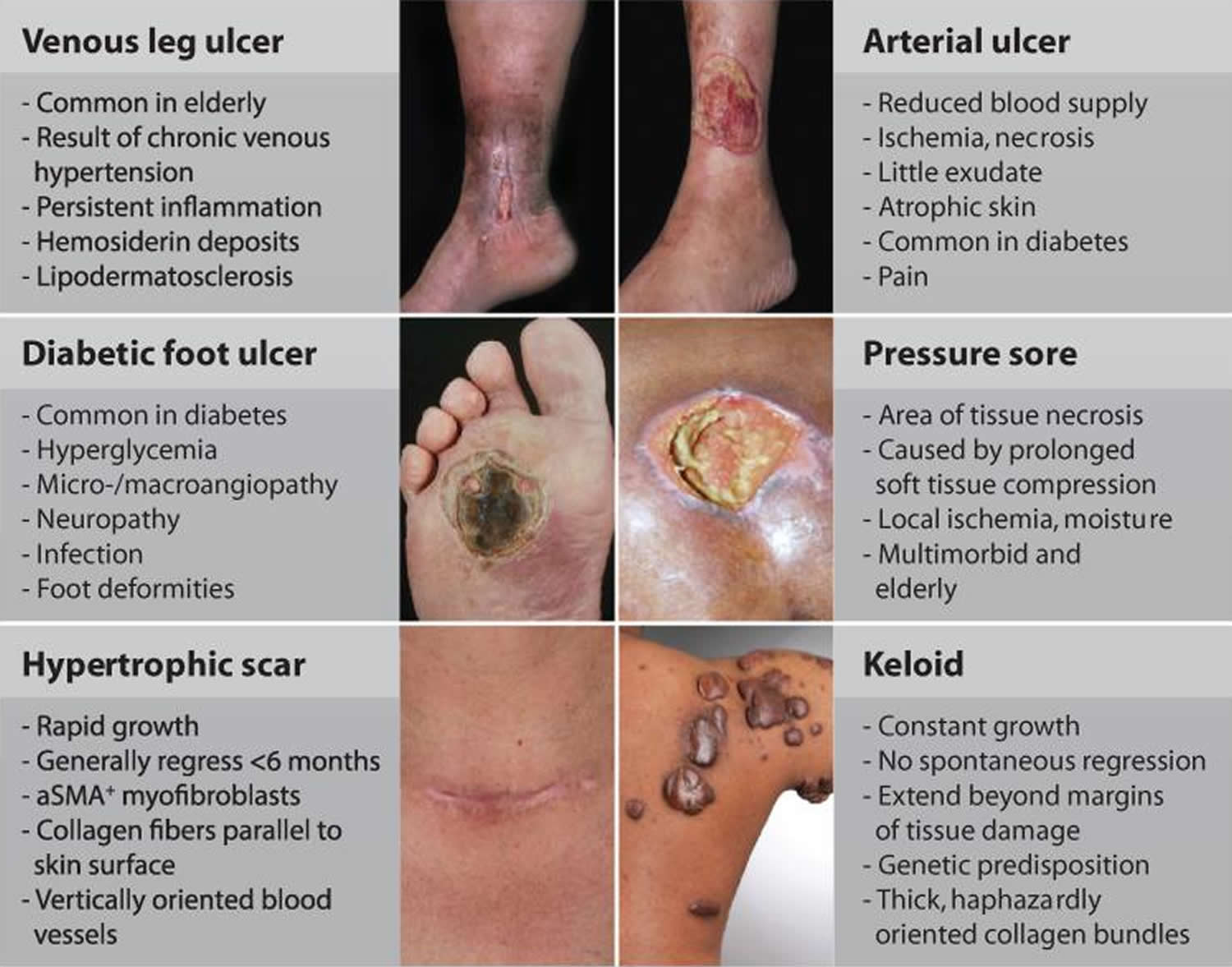
Wound healing after skin injury involves extensive communication between the different cellular constituents of the diverse compartments of the skin and its extracellular matrix (ECM). In normal physiological conditions, restoration of a functional epidermal barrier is highly efficient (Figure 1), whereas repair of the deeper dermal layer is less so and results in scar formation with a substantial loss of original tissue structure and function. When the normal repair response goes awry, there are two major outcomes: either an ulcerative skin defect (chronic wound) or an excessive formation of scar (hypertrophic scar or keloid) (see Figure 2).
The wound healing process is usually characterized as four sequential but overlapping stages 1:
- Hemostasis (0–several hours after injury),
- Inflammation (1–3 days),
- Proliferation (4–21 days) and
- Remodelling (21 days–1 year).
Deregulation of any of these steps results in impaired healing, e.g., chronic hard-to-heal ulcers or excessive scarring, which presents a major and increasing health and economic burden to our society 20. Current treatments for impaired wound healing focus mainly on optimization of controllable healing factors, e.g., clearance of infection, mechanical protection and nutritional support. Few targeted approaches have been developed to date, including mainly topical application of growth factors, unfortunately with limited clinical efficacy 21. Identification of new therapeutic targets and development of more effective treatments are needed.
Transition from the inflammatory to the proliferative stage represents a key step during wound healing. The inflammatory stage is essential leading to hemostasis and recruitment of the innate immune system, which defends us against the attack of invading pathogens and help remove dead tissues 1. However, prolonged inflammation is detrimental and may result in deregulated differentiation and activation of keratinocytes, impeding the progress through the normal stages of wound healing [2]. Severe inflammation has also been associated with excessive scarring [5]. Compared with the process of initiation and amplification of the inflammatory response, we know much less about how inflammation is resolved during normal wound healing, which is prerequisite for understanding the pathogenesis of persistent inflammation in chronic wounds [6]. Moreover, the next step, proliferation, is tightly connected with the inflammatory response, and also plays an important role in resolving inflammation. This review will focus on the inflammation-proliferation transition in normal physiologic as well as in impaired wound healing and highlight factors that can regulate this process at cellular and molecular levels.
Figure 1. Normal skin repair
Footnote: Illustrations show molecular and cellular mechanisms pivotal for progression of wound healing. Early stages of wound healing include hemostasis and activation of keratinocytes and inflammatory cells. The intermediate stage involves proliferation and migration of keratinocytes, proliferation of fibroblasts, matrix deposition, and angiogenesis. Late-stage healing involves remodeling of extracellular matrix (ECM), resulting in scar formation and restoration of barrier. This spatiotemporal process is tightly controlled by multiple cell types that secrete numerous growth factors, cytokines, and chemokines (listed below) to achieve closure and functional restoration of the barrier.
[Source 22]What is a chronic wound
Chronic wounds are rarely seen in individuals who are otherwise healthy. Chronic wounds are those that have failed to proceed through an orderly and timely reparative process to produce anatomic and functional integrity of the injured site 23. Any skin lesion has the potential to become chronic, and hence, chronic wounds are classified on the basis of their underlying cause. Vascular insufficiency, diabetes mellitus, and local-pressure effects are the major causes and categories of nonhealing skin wounds, although systemic factors, including compromised nutritional or immunological status, advanced age, chronic mechanical stress, and other comorbidities, contribute to poor wound healing. In fact, chronic wound patients frequently suffer from “highly branded” diseases such as diabetes and obesity 1.
Most chronic skin wounds occur on the lower extremities. Venous leg ulcers (Figure 2A) are the most common form of leg ulcers with an increasing incidence among the elderly of up to 3 to 4% 24. Venous leg ulcers are the most severe symptom of chronic venous disease 24.
Atherosclerotic disease represents the second most common underlying cause for nonhealing skin wounds of the lower leg. Arterial ulcerations are a consequence of reduced arterial blood supply resulting in tissue hypoxia and tissue damage (Figure 2C). Diabetes mellitus is the most common metabolic disease associated with impaired wound-healing conditions. Currently, the prevalence of type 2 diabetes is 6.4% in the world population and is anticipated to increase to close to 8% in the year 2030 25. It is not clear to what extent impaired healing is due to direct effects of insulin deficiency or its complications, including hyperglycemia, hyperlipidemia, peripheral neuropathy, and/or obesity. The most common clinical indication of impaired wound healing associated with diabetes is the diabetic foot ulcer (Figure 2B) 26. Among diabetic patients, 2 to 3% will develop a foot ulcer each year, and 15% will develop a foot ulcer during their lifetime.
Pressure ulcers (Figure 2D) are areas of tissue necrosis caused by unrelieved pressure to soft tissue compressed between a bony prominence and an external surface for a prolonged period of time. Major etiologic factors involved in their development are biomechanical forces (confined pressure, shearing forces, and friction), moisture, and local ischemia. Pressure ulcers particularly affect multimorbid and elderly patients, especially those that are bed- or wheelchair-bound. In spite of high mortality rates, predominantly for advanced-stage pressure ulcers, there is no efficacious therapy yet approved for their treatment.
Demographically, the number of patients suffering from chronic wounds and impaired healing conditions is reaching epidemic proportions and will become even more burdensome in both human health and economic terms 1. In developed countries, it has been estimated that 1 to 2% of the population will experience a chronic wound during their lifetime 27. In the United States alone, chronic wounds affect 6.5 million patients 28. In the Scandinavian countries, the associated costs account for 2–4% of the total health care expenses 29.
The burden of treating chronic wounds is growing rapidly due to increasing health care costs, an aging population and, in the United States and beyond, a sharp rise in the incidence of diabetes and obesity worldwide. It is claimed that an excess of US$25 billion is spent annually on treatment of chronic wounds 30. At present, over 1000 outpatient wound centers are in operation in the United States, not including all the wound care rendered by clinicians in their offices, by inpatient acute care hospitals, long term facilities and nursing homes 31. According to a new report by Global Industry Analysts, the annual wound care products market would reach $15.3 billion by 2010. The United States represents the world’s largest and the fastest growing market 32. The amount of money spent on wound care, the loss of productivity for afflicted individuals and the families that care for them and their diminished quality of life come at great cost to the society.
Incomplete understanding of the underlying molecular basis of tissue repair and its failure, as well as a lack of preclinical animal models that properly recapitulate human conditions 21, has led to a lack of therapies for treating nonhealing wounds or for speeding up the repair of acute wounds and reducing scar formation. Clinical research is hampered by a multimorbid and complex patient population, contributing to a paucity of high-quality and large-scale clinical trials for even demonstrating the efficacy of current products. In addition, heterogeneous reimbursement politics and an increasingly cautious climate for industrial investment, limited research funding sources 21, and lack of public awareness have also contributed to slow progress. Hence, there is a strong medical and social need to improve therapeutic approaches enhancing the endogenous tissue regenerative capacity.
Figure 2. Chronic wounds and clinical features of most common wound-healing pathologies
Footnote: The repair response can be disturbed by a multitude of local and systemic factors leading to diverse wound-healing pathologies. (A) Medial aspect of lower leg with venous leg ulcer (VLU). (B) Diabetic foot ulcer (DFU). (C) Lateral aspect of lower leg with an arterial ulcer. (D) Pressure sore. (E) Hypertrophic scar after thyroid surgery. (F) Keloid.
[Source 22] References- Sen CK, Gordillo GM, Roy S, et al. Human Skin Wounds: A Major and Snowballing Threat to Public Health and the Economy. Wound repair and regeneration : official publication of the Wound Healing Society [and] the European Tissue Repair Society. 2009;17(6):763-771. doi:10.1111/j.1524-475X.2009.00543.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2810192/
- Common Questions About Wound Care. Am Fam Physician. 2015 Jan 15;91(2):86-92. https://www.aafp.org/afp/2015/0115/p86.html
- Dire DJ, Coppola M, Dwyer DA, Lorette JJ, Karr JL. Prospective evaluation of topical antibiotics for preventing infections in uncomplicated soft-tissue wounds repaired in the ED. Acad Emerg Med. 1995;2(1):4–10.
- Sibbald RG, Goodman L, Woo KY, et al. Special considerations in wound bed preparation 2011: an update. Adv Skin Wound Care. 2011;24(9):415–436.
- Okan D, Woo K, Ayello EA, Sibbald G. The role of moisture balance in wound healing. Adv Skin Wound Care. 2007;20(1):39–53.
- Agren MS, Karlsmark T, Hansen JB, Rygaard J. Occlusion versus air exposure on full-thickness biopsy wounds. J Wound Care. 2001;10(8):301–304.
- Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(1):13–15.
- Immunization Action Coalition. Ask the experts: diseases & vaccines. Diphtheria, tetanus, and pertussis. http://www.immunize.org/askexperts/experts_per.asp
- Presutti RJ. Prevention and treatment of dog bites. Am Fam Physician. 2001;63(8):1567–1572.
- O’Dell ML. Skin and wound infections: an overview. Am Fam Physician. 1998;57(10):2424–2432.
- Medeiros I, Saconato H. Antibiotic prophylaxis for mammalian bites. Cochrane Database Syst Rev. 2001;(2):CD001738.
- Lloyd EC, Rodgers BC, Michener M, Williams MS. Outpatient burns: prevention and care [published correction appears in Am Fam Physician; 2012;85(12):1127]. Am Fam Physician. 2012;85(1):25–32.
- Stevens DL, Bisno AL, Chambers HF, et al.; Infectious Diseases Society of America. Practice guidelines for the diagnosis and management of skin and soft-tissue infections [published corrections appear in Clin Infect Dis. 2005;41(12):1830, and Clin Infect Dis. 2006;42(8):1219]. Clin Infect Dis. 2005;41(10):1373–1406.
- Lavery LA, Armstrong DG, Murdoch DP, Peters EJ, Lipsky BA. Validation of the Infectious Diseases Society of America’s diabetic foot infection classification system. Clin Infect Dis. 2007;44(4):562–565.
- Smith F, Dryburgh N, Donaldson J, Mitchell M. Debridement for surgical wounds. Cochrane Database Syst Rev. 2013;9):CD006214.
- Lipsky BA, Berendt AR, Deery HG, et al.; Infectious Diseases Society of America. Diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2004;39(7):885–910.
- Gurusamy KS, Koti R, Toon CD, Wilson P, Davidson BR. Antibiotic therapy for the treatment of methicillin-resistant Staphylococcus aureus (MRSA) in non surgical wounds. Cochrane Database Syst Rev. 2013;(11):CD010427.
- Struck MF, Gille J. Fungal infections in burns: a comprehensive review. Ann Burns Fire Disasters. 2013;26(3):147–153
- Tredget EE. Pathophysiology and treatment of fibroproliferative disorders following thermal injury. Ann N Y Acad Sci. 1999;888:165–82.
- Reish RG, Eriksson E. Scars: A review of emerging and currently available therapies. Plast. Reconstr. Surg. 2008;122:1068–1078.
- Richmond NA, Lamel SA, Davidson JM, Martins-Green M, Sen CK, Tomic-Canic M, Vivas AC, Braun LR, Kirsner RS. US–National Institutes of Health-funded research for cutaneous wounds in 2012. Wound Repair Regen. 2013;21:789–792.
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: Mechanisms, signaling, and translation. Science translational medicine. 2014;6(265):265sr6. doi:10.1126/scitranslmed.3009337. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4973620/
- Lazarus GS, Cooper DM, Knighton DR, Percoraro RE, Rodeheaver G, Robson MC. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994;2:165–70.
- Bergan JJ, Schmid-Schönbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease. N. Engl. J. Med. 2006;355:488–498.
- Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: From pathophysiology to prevention and management. Lancet. 2011;378:169–181.
- Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J. Clin. Invest. 2007;117:1219–1222.
- Gottrup F. A specialized wound-healing center concept: importance of a multidisciplinary department structure and surgical treatment facilities in the treatment of chronic wounds. Am J Surg. 2004;187:38S–43S.
- Crovetti G, Martinelli G, Issi M, Barone M, Guizzardi M, Campanati B, Moroni M, Carabelli A. Platelet gel for healing cutaneous chronic wounds. Transfus Apher Sci. 2004;30:145–51.
- Gottrup F, Holstein P, Jorgensen B, Lohmann M, Karlsmar T. A new concept of a multidisciplinary wound healing center and a national expert function of wound healing. Arch Surg. 2001;136:765–72.
- Brem H, Stojadinovic O, Diegelmann RF, Entero H, Lee B, Pastar I, Golinko M, Rosenberg H, Tomic-Canic M. Molecular markers in patients with chronic wounds to guide surgical debridement. Mol Med. 2007;13:30–9.
- https://www.todayswoundclinic.com/2007/06/getting-started/
- Global Industry Analysts I. Wound Care Products: A Global Strategic Business Report . Global Industry Analysts; 2008.