What is xanthine
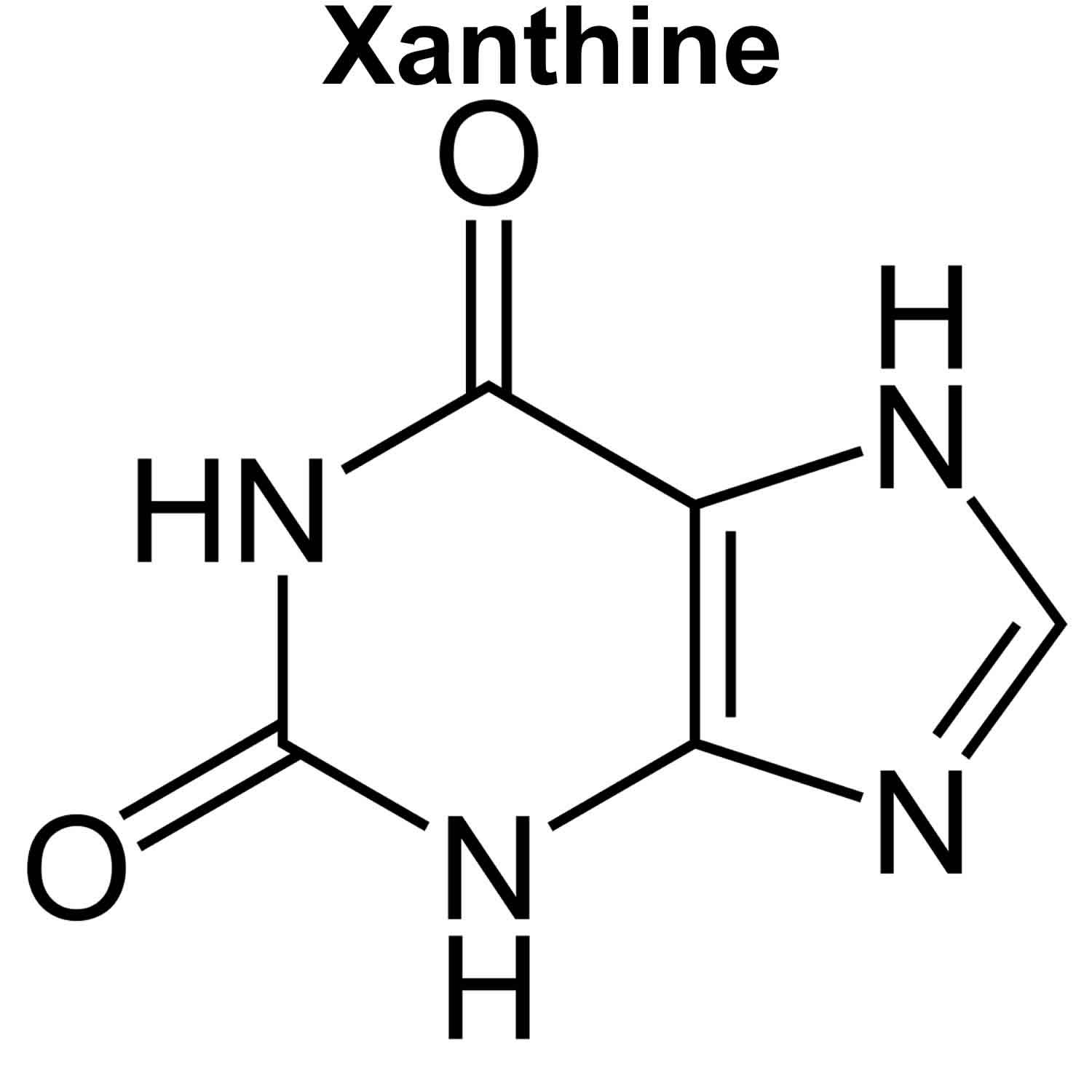
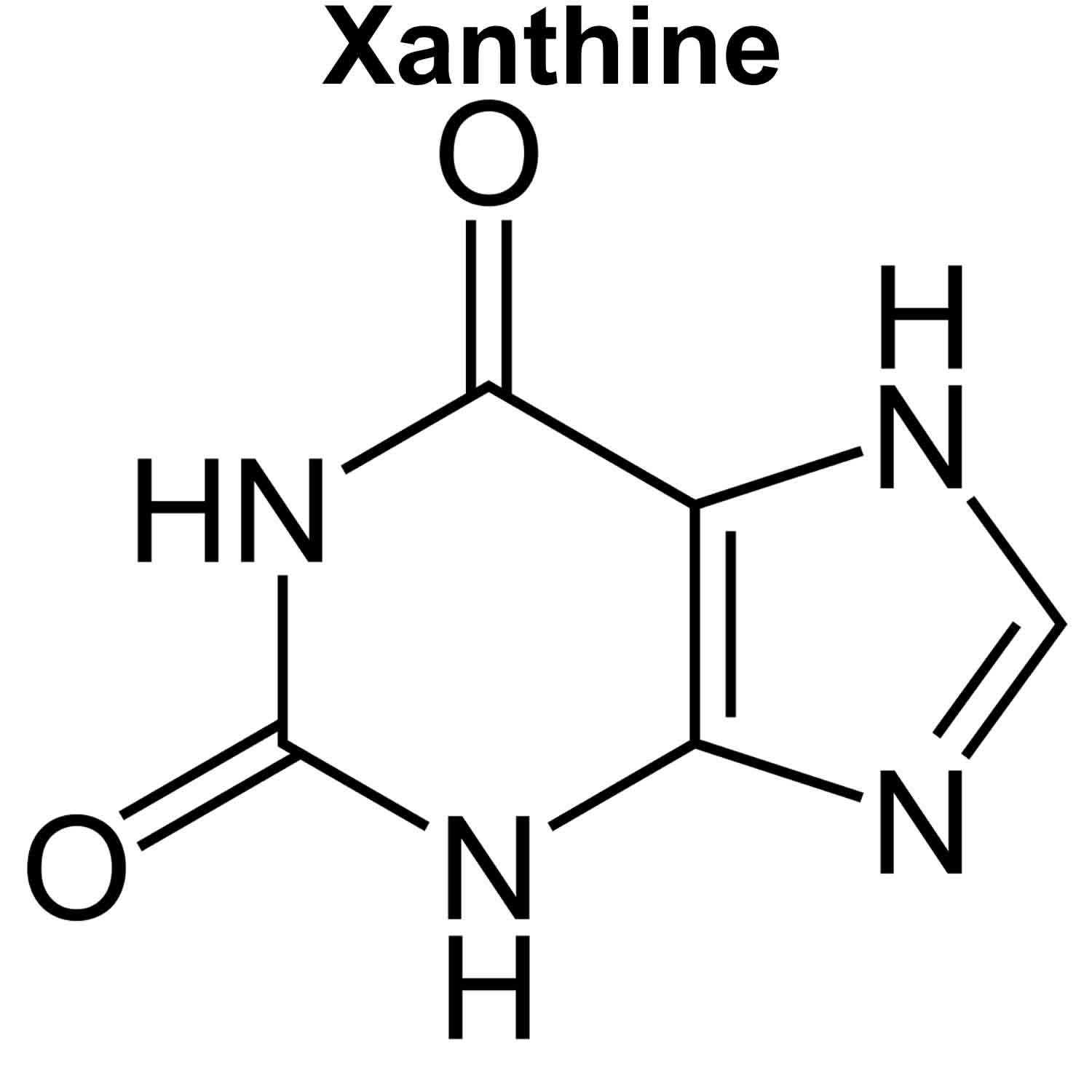
Xanthine is a purine base found in most human body tissues and fluids, certain plants, and some kidney stones. Xanthine is formed following enzymatic degradation of adenine and guanine. The term “xanthines” denotes a wide class of compounds whose central core (3,7-dihydro-purine-2,6-dione) is closely related to the DNA bases guanine and adenine (see Figures 1 and 2) 1. Like nucleobases, xanthines are capable of forming hydrogen bonds, allowing their insertion in duplexes 2 and guanine quadruplexes (G-quadruplexes) 3. Moreover, it has been shown that their self-association can give rise to four-stranded structures 4, which have attracted attention for applications in the field of molecular electronics 5. Moreover, methylxanthines are used as therapeutic agents acting, among others, as stimulants of the nervous system 6. The well-known caffeine, present in coffee and tea and various soft beverages, is none other than 1,3,7-trimethylxanthine (Figure 2). It is also worth noticing that 2′-deoxyxanthosine (dX) has been used in the extension of the genetic alphabet by purine pairing with a 2,4-diaminopyrimidine nucleoside, which has a hydrogen bonding pattern complementary to 2′-deoxyxanthosine (dX) 7.
Xanthine is an intermediate in the degradation of adenosine monophosphate to uric acid, being formed by oxidation of hypoxanthine. The methylated xanthine compounds caffeine, theobromine, and theophylline and their derivatives are used in medicine for their bronchodilator effects. Xanthine is found to be associated with Lesch-Nyhan syndrome and xanthinuria type 1, which are inborn errors of metabolism.
Purine is a heterocyclic aromatic organic compound, consisting of a pyrimidine ring fused to an imidazole ring. Two of the bases in nucleic acids, adenine and guanine, are purines. Purines from food (or from tissue turnover) are metabolized by several enzymes, including xanthine oxidase, into uric acid. High levels of uric acid can predispose to gout when the acid crystalizes in joints; this phenomenon only happens in humans and some animal species (e. g. dogs) that lack an intrinsic uricase enzyme that can further degrade uric acid.
Figure 1. Xanthine
Figure 2. Xanthine derivatives
Xanthine oxidase deficiency
Hereditary xanthinuria is a condition that most often affects the kidneys. It is characterized by high levels of a compound called xanthine and very low levels of another compound called uric acid in the blood and urine. The excess xanthine can accumulate in the kidneys and other tissues. In the kidneys, xanthine forms tiny crystals that occasionally build up to create kidney stones. These stones can impair kidney function and ultimately cause kidney failure. Related signs and symptoms can include abdominal pain, recurrent urinary tract infections, and blood in the urine (hematuria). Less commonly, xanthine crystals build up in the muscles, causing pain and cramping. In some people with hereditary xanthinuria, the condition does not cause any health problems.
Researchers have described two major forms of hereditary xanthinuria, types 1 and 2. The types are distinguished by the enzymes involved; they have the same signs and symptoms.
Classically, Type 1 xanthinuria is caused by a mutation in xanthine dehydrogenase/oxidase (XDH/OX) gene mapped to chromosome 2p23.1, whereas Type 2 xanthinuria is caused by deficits of xanthine dehydrogenase/oxidase (XDH/OX) and aldehyde oxidase (AOX) caused by mutations in molybdenum cofactor sulfurase gene (MOCOS) localized on chromosome 18q12.2 8. These different mutations lead to clinically undistinguishable types.
A third clinically distinct entity, molybdenum cofactor deficiency type A, is characterized by triple deficiency of xanthine dehydrogenase, aldehyde oxidase and sulfite oxidase. This rare lethal autosomal recessive disorder caused by mutations in MOCS1 gene (6p21.1) is characterized by early onset in infancy 9.
The combined incidence of hereditary xanthinuria types 1 and 2 is estimated to be about 1 in 69,000 people worldwide. However, researchers suspect that the true incidence may be higher because some affected individuals have no symptoms and are never diagnosed with the condition. Hereditary xanthinuria appears to be more common in people of Mediterranean or Middle Eastern ancestry. About 150 cases of this condition have been reported in the medical literature.
Hereditary xanthinuria diagnosis is based on estimation of uric acid in blood and urine 10. If hypouricemia is confirmed, detailed purine metabolic investigation follows, and includes measurement of xanthine and hypoxanthine in urine and plasma. High urinary levels of xanthine are then typical for classical hereditary xanthinuria. In about half of patients, ultrasonography reveals the presence of xanthine urolithiasis. Additional methods for diagnostic confirmation and/or identification of the type of xanthinuria include allopurinol loading test, xanthine oxidase assay and molecular analysis.
There is no curative treatment for hereditary xanthinuria. The only recommended treatment for patients with xanthinuria is a low purine diet and high intake of fluids 9. Because the solubility of xanthine is relatively independent of urinary pH, urine alkalinization has no effect (in contrast to patients with uric acid lithiasis) 11. When kidney stones are present, a pyelolithotomy might be necessary.
The overall prognosis for hereditary xanthinuria is favorable, even though, in some cases, the disease progresses to end-stage renal failure 10.
Hereditary xanthinuria type 1
Hereditary xanthinuria type 1 is caused by mutations in the XDH gene that is inherited in autosomal recessive manner. An autosomal recessive pattern means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. The XDH gene provides instructions for making an enzyme called xanthine dehydrogenase. The xanthine dehydrogenase enzyme is involved in the normal breakdown of purines, which are building blocks of DNA and its chemical cousin, RNA. Specifically, xanthine dehydrogenase carries out the final two steps in the process, including the conversion of xanthine to uric acid (which is excreted in urine and feces). Mutations in the XDH gene reduce or eliminate the activity of xanthine dehydrogenase. As a result, the xanthine dehydrogenase enzyme is not available to help carry out the last two steps of purine breakdown. Because xanthine is not converted to uric acid, affected individuals have high levels of xanthine in their blood (hyperxanthinemia) and urine (xanthinuria) and very low levels of uric acid in their blood and urine. The excess xanthine can cause damage to the kidneys and other tissues. Xanthinuria leads to urolithiasis (kidney stones formation), hematuria (blood in urine), renal colic and urinary tract infections (UTIs), while some patients are asymptomatic and others suffer from kidney failure. Approximately 50% of patients with hereditary xanthinuria type 1 present with urinary tract infections, hematuria, renal colic, acute renal failure, and urolithiasis. A small number of patients also develop renal failure, arthropathy, myopathy, or duodenal ulcer 12.
Hereditary xanthinuria type 2
Hereditary xanthinuria type 2 results from mutations in the MOCOS gene that is inherited in autosomal recessive manner. An autosomal recessive pattern means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. The MOCOS gene provides instructions for making an enzyme called molybdenum cofactor sulfurase. The molybdenum cofactor sulfurase enzyme is necessary for the normal function of xanthine dehydrogenase, described above, and another enzyme called aldehyde oxidase. Mutations in the MOCOS gene prevent xanthine dehydrogenase and aldehyde oxidase from being turned on (activated). The loss of xanthine dehydrogenase activity prevents the conversion of xanthine to uric acid, leading to an accumulation of xanthine in the kidneys and other tissues. The loss of aldehyde oxidase activity does not appear to cause any health problems.
Xanthine medications
The xanthines, caffeine and theobromine are the pharmacologically active components of a range of drinks such as coffee, tea, cocoa and soft drinks.
Xanthines also include medicines such as theophylline, used in the treatment of asthma.
Caffeine
Caffeine is a naturally occurring substance which stimulates the central nervous system and can temporarily relieve tiredness and increase alertness 13. While humans have no nutritional requirement for caffeine (caffeine is not an essential part of the human diet), most adults can safely consume moderate amounts of caffeine. Pregnant women can also safely consume caffeine, however they should consume less caffeine than non-pregnant women, to protect the health of their developing fetus.
The caffeine content of a cup of coffee is generally estimated to be approximately 100 mg, and a cup of tea approximately 50 mg but may be greater depending on how the drink is prepared. For instance, an espresso is likely to have a higher caffeine concentration than a cup of instant coffee. Cola drinks contain up to 25 mg of caffeine per 100 mL. Energy drinks are likely to have an even higher caffeine content, and often contain other stimulants. Caffeine is also a component of certain medications, such as analgesic preparations and over the counter cold and flu preparations.
The approximate amounts of caffeine found in food and drinks are:
- one cup of instant coffee: 60 – 80 mg
- one cup (5 oz. cup) of filter coffee: 40 – 180 mg
- one cup (5 oz. cup) of tea: 20 – 90 mg
- one 375g can of cola: 48.75 mg
- one 250ml can of energy drink: 80mg
- Red Bull® energy drink 67 mg
- one 100g bar of milk chocolate: around 20 mg
- 2 tablets of Excedrin® 130 mg
- 1 cup of coffee ice cream 58 mg
- 12 oz. Coke® 46 mg
- Hershey® chocolate bar 10 mg
- 8 oz. hot chocolate 5 mg
Caffeine, as a lipophilic substance, is well absorbed from the gastrointestinal tract, crosses the placenta and can exert its stimulant effects on the fetus resulting in increased fetal activity and heart rate, and in some cases fetal arrhythmia.
Regular use of large amounts of caffeine have been associated with reduced fertility in both women and men 14. A meta-analysis of studies involving approximately 50,000 pregnant women in total suggested a slightly elevated rate of spontaneous abortion amongst women who drank more than 150 mg of caffeine per day during pregnancy 15. Stefanidou 16 reported a dose-response relationship between caffeine ingestion and recurrent miscarriage. After controlling for confounders, the odds ratio for recurrent miscarriage increased with increased daily caffeine intake in the periconceptional period and in early gestation. A prospective Danish study found a slight elevated rate of stillbirth amongst pregnant women who had consumed more than eight cups of coffee a day 17. A follow-up study by the same authors demonstrated that women who drank more than eight cups of coffee per day were at increased risk of a fetal death 18.
A number of studies have demonstrated an increased rate of cryptorchidism, anal atresia and cleft lip/palate amongst infants whose mothers consumed caffeine during pregnancy; however, these studies were limited by retrospective exposure assessment, small sample size and failure to adjust for other potential confounders including maternal smoking and alcohol consumption 19. A study by Schmidt 20 identified an association between infant neural tube defect (NTD) risk and polymorphisms in a fetal and maternal gene involved in caffeine metabolism. The authors suggested that risk of neural tube defects may be increased in genetically susceptible individuals with caffeine consumption.
The data relating to the effects of caffeine on fetal growth in utero are mixed. Numerous studies 21, 22, 23 have suggested a link between intrauterine growth restriction (IUGR) or low infant birth weight and caffeine consumption in pregnancy. A meta-analysis from 1998, which included approximately 50,000 pregnant women, suggested a slightly increased risk of having a baby with IUGR, if the mother had consumed more than 150 mg of caffeine per day 24. More recent studies have also found a positive correlation between caffeine intake and low birth weight 25 found reduced infant birth weight with maternal daily caffeine intake of more than 540 mg, whilst Sengpiel 25 reported that maternal caffeine intake of more than 200 mg to 300 mg/day increased the odds for having a small for gestational age infant. Other studies have suggested that effects of maternal caffeine consumption on birth weight are restricted to male offspring only 26, or to infants of women who are rapid caffeine metabolizers 27. However, a review of the literature in 2000 demonstrated no evidence of an effect of even moderate to high caffeine consumption on in utero growth 28 and another concluded that low infant birth weight cannot be clearly attributed to caffeine and cannot be separated from effects of other exposures such as maternal smoking and alcohol consumption 19.
The hypothesis that the methylxanthine, theobromine, which is found particularly in cocoa, could reduce the rate of preeclampsia, has not been confirmed 29. A meta-analysis of 22 studies found no clear connection between coffee consumption during pregnancy and preterm delivery 30. In a study by Barr 31 no effect on physical development parameters and IQ up to the age of 7.5 years in the children of 500 pregnant women who had consumed more than 150 mg of caffeine daily was found. One prospective study reported a weak association between the occurrence of hyperactivity at 18 months in children whose mothers had consumed caffeine-containing drinks during the pregnancy 32. Another study found no connection between caffeine use during pregnancy and attention deficit disorders 33.
Regular coffee consumption during pregnancy has recently been associated with childhood acute leukemia in the offspring in a single study, with the risk increasing linearly with daily intake 34.
A New Zealand study 35 reported that the babies of women who consumed greater than 400 mg of caffeine per day during pregnancy were 1.65 times more likely to die of sudden infant death syndrome than the babies of women who consumed less caffeine. The New Zealand study 35 also found that infants born to women who consumed high quantities of caffeine whilst pregnant were more likely to experience sleep apnea (difficulty breathing during sleep).
Summary
There is insufficient robust scientific evidence on which to provide a specific recommendation regarding the amount of caffeine that can be consumed during pregnancy without causing harm to the fetus. The data regarding caffeine consumption during pregnancy are contradictory. An association between caffeine intake and increased miscarriage risk, and possibly fetal demise has been reported but remains unproven. Similarly, various structural anomalies have been reported following caffeine exposure in utero but a causal association or consistent embryopathy has not been demonstrated.
Maternal caffeine consumption of less than 150 mg caffeine a day in pregnancy does not appear to affect fetal growth, and although an adverse effect on birth weight has been reported at higher doses by some, these data are inconsistent with respect to identifying a threshold dose for this effect. Single studies have suggested a possible association with childhood acute leukemia and hyperactivity, but these findings remain to be confirmed.
Pregnant women who consume more than 200 mg of caffeine daily (about two cups of brewed coffee) should reduce their caffeine consumption whilst pregnant. Health professionals advise individuals to reduce their caffeine consumption gradually, for example by replacing one caffeinated drink with a non-caffeinated alternative each day, in order to avoid withdrawal symptoms. Decaffeinated varieties are an option which contains little or no caffeine.
Energy drinks are not recommended during pregnancy as they may contain high levels of caffeine, and other ingredients not recommended for pregnant women.
Theobromine
Theobromine is the principal alkaloid (1.5–3%) of the cacao bean (Theobroma cacao); it is usually extracted from the husks of cacao beans, which contain 0.7–1.2% theobromine 36. Theobromine is used principally to make caffeine 37. Formerly, theobromine and its derivatives were used in diuretics, myocardial stimulants, vasodilators and smooth muscle relaxants 38. Theobromine salts (calcium salicylate, sodium salicylate and sodium acetate) were used previously to dilate coronary arteries 39 at doses of 300 to 600 mg per day 40. There is no current therapeutic use of theobromine 41.
Theobromine in foods
Theobromine is found in chocolate, tea and cocoa products 42. Cacao is the major natural source of theobromine; the concentration in whole cacao beans and nibs (cotyledon) increases during the first day of fermentation and that in the shells increases subsequently 43.
Theobromine has been reported in cacao husks and beans at 0.7–1.2% and 1.5–3% (15–30 g/kg) 38. Levels have been reported to be 20 mg/kg in green coffee beans 44, 0.15–0.20% in manufactured tea 45 and 0.3% in dried mate 46.
Dark chocolate contains the largest amount of theobromine per serving of any type of eating chocolate; concentrations vary widely (0.36–0.63%) owing to the initial large difference in the theobromine content in chocolate liquors, but one 1-oz bar of dark chocolate contained 130 mg theobromine, and one 1-oz bar of milk chocolate contained 44 mg theobromine. The theobromine content of chocolate foods prepared from home recipes using standard chocolate sources (i.e., cocoa and baking chocolate) varies widely (24 mg per serving in chocolate brownies to 724 mg in chocolate frostings); chocolate frostings have relatively higher theobromine levels (0.055–0.213%) than chocolate cakes. The methylxanthine (theobromine and caffeine) content of manufactured chocolate foods and beverages varies according to food source and within different brands of the same item 47.
Theobromine side effects
It has been stated that ‘in large doses’ theobromine may cause nausea and anorexia 48 and that daily intake of 50–100 g cocoa (0.8–1.5 g theobromine) by humans has been associated with sweating, trembling and severe headache 49. In a study of 13 volunteers who consumed 200 mg theobromine orally three times during a 24-h period, no clinical symptom or other pharmacological activity was observed 50. Ingestion of theobromine in sweet chocolate at a dose of 6 mg/kg body weight per day had no effect on clinical parameters in 12 human subjects 51.
Theophylline
Theophylline is a bronchodilator. Theophylline is used to prevent and treat symptoms such as wheezing, shortness of breath, and chest tightness caused by asthma, chronic bronchitis, emphysema, and other lung diseases. It relaxes and opens air passages in the lungs, making it easier to breathe.
Theophylline controls symptoms of asthma and other lung diseases but does not cure them. Continue to take theophylline even if you feel well. Do not stop taking theophylline without talking to your doctor.
Theophylline works by relaxing muscles in the lungs and chest, making the lungs less sensitive to allergens and other causes of bronchospasm.
Theophylline comes as a tablet, capsule, solution, and syrup to take by mouth. It usually is taken every 6, 8, 12, or 24 hours. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take theophylline exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Take theophylline with a full glass of water on an empty stomach, at least 1 hour before or 2 hours after a meal. Do not chew or crush the extended-release (long-acting) theophylline tablets; swallow them whole. Extended-release capsules (e.g., Theo-Dur Sprinkles) may be swallowed whole or opened and the contents mixed with soft food and swallowed without chewing.
Theophylline side effects
Theophylline may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away.
- upset stomach
- stomach pain
- diarrhea
- headache
- restlessness
- insomnia
- irritability
If you experience any of the following symptoms, call your doctor immediately:
- vomiting
- increased or rapid heart rate
- irregular heartbeat
- seizures
- skin rash
Xanthine oxidase inhibitor
Allopurinol and Febuxostat are xanthine oxidase inhibitor drugs that is used to treat gout and high levels of uric acid in the blood (hyperuricemia) caused by certain cancer medications, and kidney stones. Xanthine oxidase inhibitor works by causing less uric acid to be produced by the body. High levels of uric acid may cause gout attacks or kidney stones. Allopurinol is used to prevent gout attacks, not to treat them once they occur.
These medicines are available only with your doctor’s prescription.
Allopurinol side effects
Allopurinol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- upset stomach
- diarrhea
- drowsiness
Some side effects can be serious. The following symptoms are uncommon, but if you experience any of them, call your doctor immediately:
- skin rash
- painful urination
- blood in the urine
- irritation of the eyes
- swelling of the lips or mouth
- fever, sore throat, chills, and other signs of infection
- loss of appetite
- unexpected weight loss
- itching
Allopurinol may cause other side effects. Call your doctor if you have any unusual problems while taking this allopurinol.
Febuxostat side effects
Febuxostat may cause side effects. Tell your doctor if either of these symptoms is severe or does not go away:
- nausea
- joint pain
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately:
- rash; skin redness or pain; swelling or blistering of lips, eyes or mouth; skin peeling; or fever and other flu-like symptoms
- chest pain
- shortness of breath
- slow or difficult speech
- dizziness or faintness
- weakness or numbness of an arm or leg
- yellow eyes or skin; dark urine; or pain or discomfort in right upper stomach area
Febuxostat may cause other side effects. Call your doctor if you have any unusual problems while taking this febuxostat.
References- Changenet-Barret P, Kovács L, Markovitsi D, Gustavsson T. Xanthines Studied via Femtosecond Fluorescence Spectroscopy. Molecules. 2016;21(12):1668. Published 2016 Dec 3. doi:10.3390/molecules21121668 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6274292
- Eritja R., Horowitz D.M., Walker P.A., Ziehlermartin J.P., Boosalis M.S., Goodman M.F., Itakura K., Kaplan B.E. Synthesis and properties of oligonucleotides containing 2′-deoxynebularine and 2′-deoxyxanthosine. Nucleic Acids Res. 1986;14:8135–8153. doi: 10.1093/nar/14.20.8135.
- Cheong V.V., Lech C.J., Heddi B., Phan A.T. Inverting the G-tetrad polarity of a G-quadruplex by using xanthine and 8-oxoguanine. Angew. Chem. Int. Ed. 2016;55:160–163. doi: 10.1002/anie.201507034
- Novotny J., Yurenko Y.P., Kulhanek P., Marek R. Tailoring the properties of quadruplex nucleobases for biological and nanomaterial applications. Phys. Chem. Chem. Phys. 2014;16:15241–15248. doi: 10.1039/c4cp00541d
- Livshits G.I., Stern A., Rotem D., Borovok N., Eidelshtein G., Migliore A., Penzo E., Wind S.J., di Felice R., Skourtis S.S., et al. Long-range charge transport in single G-quadruplex DNA molecules. Nat. Nanotechnol. 2014;9:1040–1046. doi: 10.1038/nnano.2014.246
- Monteiro J.P., Alves M.G., Oliveira P.F., Silva B.M. Structure-bioactivity relationships of methylxanthines: Trying to make sense of all the promises and the drawbacks. Molecules. 2016;21:974 doi: 10.3390/molecules21080974
- Lutz M.J., Held H.A., Hottiger M., Hubscher U., Benner S.A. Differential discrimination of DNA polymerases for variants of the non-standard nucleobase pair between xanthosine and 2,4-diaminopyrimidine, two components of an expanded genetic alphabet. Nucleic Acids Res. 1996;24:1308–1313. doi: 10.1093/nar/24.7.1308
- Ichida K, Amaya Y, Okamoto K, Nishino T. Mutations associated with functional disorder of xanthine oxidoreductase and hereditary xanthinuria in humans. Int J Mol Sci 2012;13: 15475–15495. 10.3390/ijms131115475
- Grases F, Costa-Bauza A, Roig J, Rodriguez A. Xanthine urolithiasis: Inhibitors of xanthine crystallization. PLoS One. 2018;13(8):e0198881. Published 2018 Aug 29. doi:10.1371/journal.pone.0198881 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6114289/
- Hereditary xanthinuria. https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=EN&data_id=704&Disease_Disease_Search_diseaseGroup=xanthine&Disease_Disease_Search_diseaseType=Pat&Disease(s)/group%20of%20diseases=Hereditary-xanthinuria&title=Hereditary%20xanthinuria&search=Disease_Search_Simple
- Nicoletta JA, Lande MB. Medical evaluation and treatment of urolithiasis. Pediatr Clin North Am. 2006;53: 479–491. 10.1016/j.pcl.2006.03.001
- Mateos FA, Puig JG, Jimenez ML, Fox IH. Hereditary xanthinuria: Evidence for enhanced hypoxanthine salvage. J Clin Invest 1987;79: 847–852. 10.1172/JCI112893
- Nawrot P, Jordan S, Eastwood J, Rostein J, Hugenholt A, Feeley M. Effects of caffeine on human health. Food Addit Contam. 2003; 20(1): 1-30.
- Caffeine intake and fecundability: a follow-up study among 430 Danish couples planning their first pregnancy. Reprod Toxicol. 1998 May-Jun;12(3):289-95. https://www.ncbi.nlm.nih.gov/pubmed/9628552
- Cnattinguis S, Signorello LB, Anneren G, Clausson B, Ekbom A, Ljunger E, et al. Caffeine intake and the risk of first trimester spontaneous abortion. NEMJ. 2000; 343: 1839-43.
- Maternal caffeine consumption and sine causa recurrent miscarriage. Eur J Obstet Gynecol Reprod Biol. 2011 Oct;158(2):220-4. doi: 10.1016/j.ejogrb.2011.04.024. Epub 2011 Jun 1. https://www.ncbi.nlm.nih.gov/pubmed/21636205
- Wisborg K, Kesmodel U, Bech BH, Hedegaard M, Henriksen TB. Maternal consumption of coffee during pregnancy and stillbirth and infant death in first year of life: prospective study. BMJ. 2003;326(7386):420. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC149440
- K.A. Hahn, L.A. Wise, K.J. Rothman, E.M. Mikkelsen, S.B. Brogly, H.T. Sørensen, A.H. Riis, E.E. Hatch; Caffeine and caffeinated beverage consumption and risk of spontaneous abortion, Human Reproduction, Volume 30, Issue 5, 1 May 2015, Pages 1246–1255, https://doi.org/10.1093/humrep/dev063
- A review of the epidemiologic evidence concerning the reproductive health effects of caffeine consumption: a 2000-2009 update. Food Chem Toxicol. 2010 Oct;48(10):2549-76. doi: 10.1016/j.fct.2010.06.019. Epub 2010 Jun 15. https://www.ncbi.nlm.nih.gov/pubmed/20558227
- Schmidt RJ, Romitti PA, Burns TL, et al. Caffeine, selected metabolic gene variants, and risk for neural tube defects. Birth Defects Res A Clin Mol Teratol. 2010;88(7):560-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2917796/
- Care Study Group. Maternal caffeine intake during pregnancy and risk of fetal growth restriction: A large prospective observational study. BMJ. 2008; 337: 2332.
- Bakker R, Steegers EAP, Obradov A, Raat H, Hoffman A, Jaddoe VWV. Maternal caffeine intake from coffee and tea, fetal growth and the risks of adverse birth outcomes: The Generation R Study. Am J Clin Nutr. 2010; 91(6): 1691-8
- Grosso LM, Triche EW, Belanger K, Benowitz NL, Holford TR, Bracken MB. Caffeine metabolites in umbilical cord blood, cytochrome P-450 1A2 activity and intrauterine growth restriction. Am J Epidemiol. 2006; 163(11): 1035-41.
- Moderate to heavy caffeine consumption during pregnancy and relationship to spontaneous abortion and abnormal fetal growth: a meta-analysis. Reprod Toxicol. 1998 Jul-Aug;12(4):435-44. https://www.ncbi.nlm.nih.gov/pubmed/9717693
- Sengpiel V, Elind E, Bacelis J, et al. Maternal caffeine intake during pregnancy is associated with birth weight but not with gestational length: results from a large prospective observational cohort study. BMC Med. 2013;11:42. Published 2013 Feb 19. doi:10.1186/1741-7015-11-42 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3606471/
- Vik, T. , Bakketeig, L. S., Trygg, K. U., Lund‐Larsen, K. and Jacobsen, G. (2003), High caffeine consumption in the third trimester of pregnancy: gender‐specific effects on fetal growth. Paediatric and Perinatal Epidemiology, 17: 324-331. doi:10.1046/j.1365-3016.2003.00507.x
- CARE Study Group. Maternal caffeine intake during pregnancy and risk of fetal growth restriction: a large prospective observational study. BMJ. 2008;337:a2332. Published 2008 Nov 3. doi:10.1136/bmj.a2332 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2577203
- Brent RL, Christian MS, Diener RM. Evaluation of the reproductive and developmental risks of caffeine. Birth Defects Res B Dev Reprod Toxicol. 2011;92(2):152-87. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121964/
- Maternal serum theobromine and the development of preeclampsia. Epidemiology. 2009 Sep;20(5):727-32. doi: 10.1097/EDE.0b013e3181aba664. https://www.ncbi.nlm.nih.gov/pubmed/19535985
- Maslova E, Bhattacharya S, Lin SW, Michels KB. Caffeine consumption during pregnancy and risk of preterm birth: a meta-analysis. Am J Clin Nutr. 2010;92(5):1120-32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2954446/
- Caffeine use during pregnancy and child outcome: a 7-year prospective study. Neurotoxicol Teratol. 1991 Jul-Aug;13(4):441-8. https://www.ncbi.nlm.nih.gov/pubmed/1921923
- Intrauterine exposure to caffeine and inattention/overactivity in children. Acta Paediatr. 2010 Jun;99(6):925-8. doi: 10.1111/j.1651-2227.2010.01744.x. Epub 2010 Mar 5. https://www.ncbi.nlm.nih.gov/pubmed/20219037
- Linnet, K. M., Wisborg, K. , Secher, N. J., Hove Thomsen, P. , Obel, C. , Dalsgaard, S. and Henriksen, T. B. (2009), Coffee consumption during pregnancy and the risk of hyperkinetic disorder and ADHD: a prospective cohort study. Acta Pædiatrica, 98: 173-179. doi:10.1111/j.1651-2227.2008.00980.x
- Childhood acute leukemia, maternal beverage intake during pregnancy, and metabolic polymorphisms. Cancer Causes Control. 2013 Apr;24(4):783-93. doi: 10.1007/s10552-013-0161-9. Epub 2013 Feb 13. https://www.ncbi.nlm.nih.gov/pubmed/23404349
- Ford RPK, Schuter PJ, Mitchell EA, Taylor BJ, Scragg R, Stewart AW. Heavy caffeine intake in pregnancy and sudden infant death syndrome. Arch Dis Child. 1998; 78: 9-13.
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans. Coffee, Tea, Mate, Methylxanthines and Methylglyoxal. Lyon (FR): International Agency for Research on Cancer; 1991. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 51.) Theobromine. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507032
- McCutheon, G.F. (1969) Caffeine. In: Snell, F.D. & Ettre, L.S., eds, Encyclopedia of Industrial Chemical Analysis, Vol. 8, New York, Interscience, pp. 55–71
- Windholz, M., ed. (1983) The Merck Index, 10th ed., Rahway, NJ, Merck & Co., p. 1327.
- Gennaro, A.R., ed. (1985) Remington’s Pharmaceutical Sciences, 17th ed., Easton, PA, Mack Publishing, pp. 944, 1070, 1135.
- Moffat, A.C., ed. (1986) Clarke’s Isolation and Identification of Drugs, 2nd ed., London, The Pharmaceutical Press, pp. 1010–1011
- Tarka, S.M., Jr (1982) The toxicology of cocoa and methylxanthines: a review of the literature. Crit. Rev. Toxicol. 9, 275–312
- Stavric B. Methyl xanthines: toxicity to humans. 3. Theobromine, paraxanthine and the combined effects of methylxanthines. Food chem. Toxicol. 1988;26:725–733.
- Shively, C.A. & Tarka, S.M., Jr (1984) Methylxanthine composition and consumption patterns of cocoa and chocolate products. In: Spiller, G.A., ed., The Methylxanthine Beverages and Foods: Chemistry, Consumption, and Health Effects, New York, Alan R. Liss, pp. 149–178
- Spiller, M.A. (1984) The chemical components of coffee. In: Spiller, G.A., ed., The Methylxanthine Beverages and Foods: Chemistry, Consumption, and Health Effects, New York, Alan R. Liss, pp. 91–147
- Graham, H.N. (1984a) Tea: the plant and its manufacture: chemistry and conception of the beverage. In: Spiller, G.A., ed., The Methylxanthine Beverages and Foods: Chemistry, Consumption, and Health Effects, New York, Alan R. Liss, pp. 29–74.
- Graham, H.N. (1984b) Mate. In: Spiller, G.A., ed., The Methylxanthine Beverages and Foods: Chemistry, Consumption, and Health Effects, New York, Alan R. Liss, pp. 179–183.
- Shively, C.A. & Tarka, S.M., Jr (1984) Methylxanthine composition and consumption patterns of cocoa and chocolate products. In: Spiller, G.A., ed., The Methylxanthine Beverages and Foods: Chemistry, Consumption, and Health Effects, New York, Alan R. Liss, pp. 149–178.
- Reynolds, J.E.F., ed. (1982) Martindale. The Extra Pharmacopoeia, 28th ed., London, The Pharmaceutical Press, pp. 348–349.
- Czok G. Concerning the question of the biological effectiveness of methylxanthines in cocoa products (Ger.). Z. Ernahrungswiss. 1974;13:165–171.
- Birkett D.J., Dahlqvist R., Miners J.O., Lelo A., Billing B. Comparison of theophylline and theobromine metabolism in man. Drug Metab. Disposition. 1985;13:725–728
- Shively C.A., Tarka S.M. Jr, Arnaud M.J., Dvorchik B.H., Passananti G.T., Vesell E.S. High levels of methylxanthines in chocolate do not alter theobromine disposition. Clin. pharmacol. Ther. 1985;37:415–424.