What is luteinizing hormone
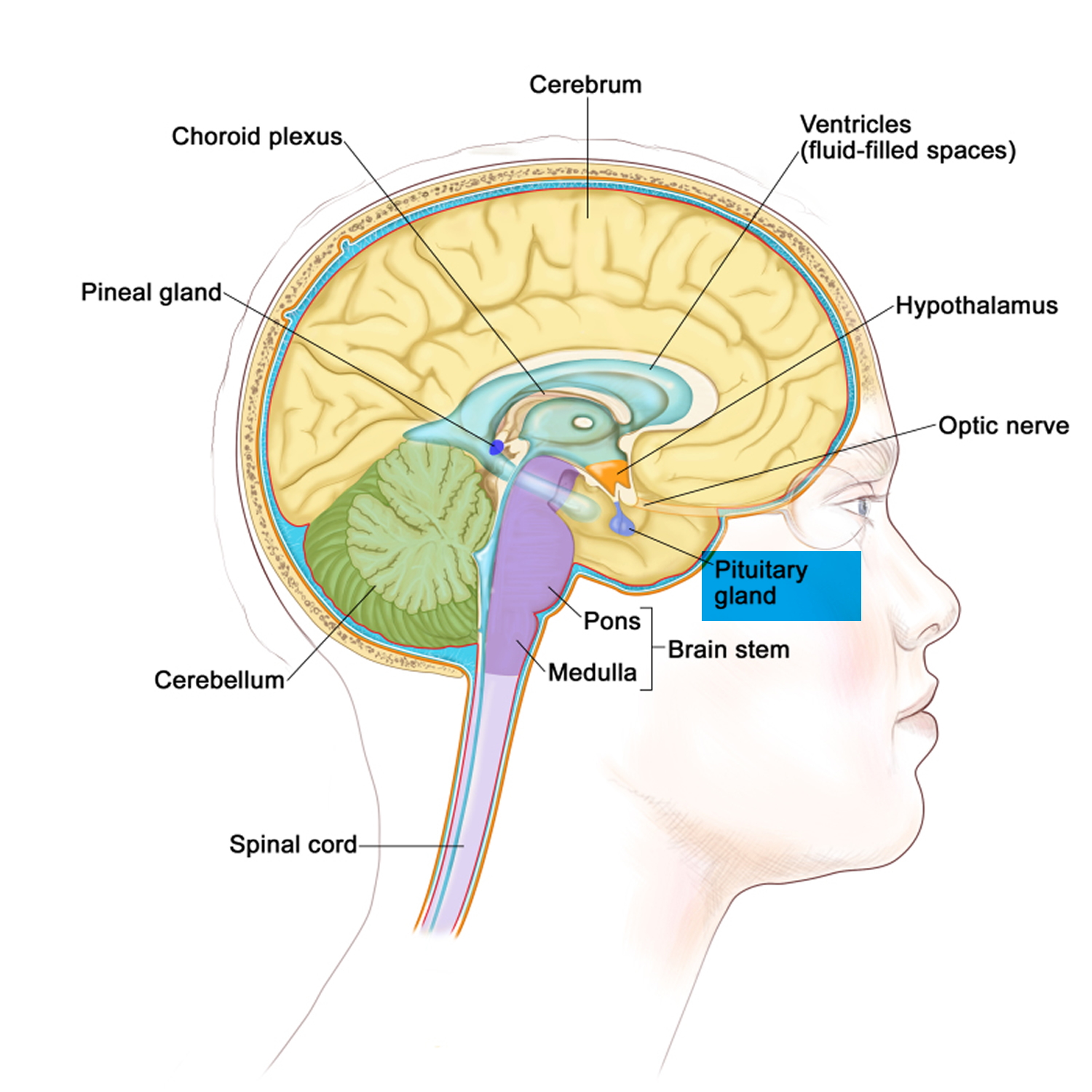
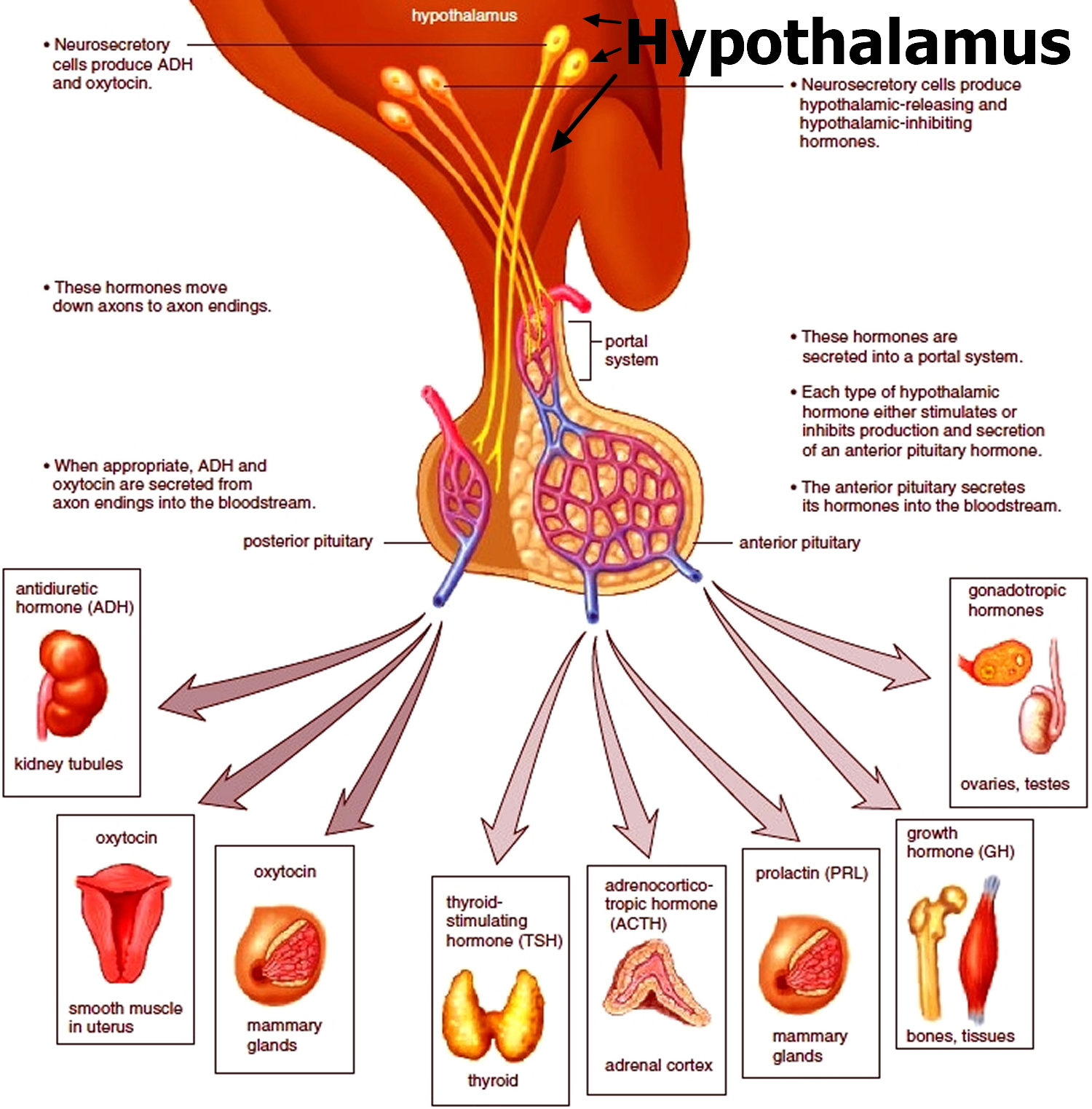
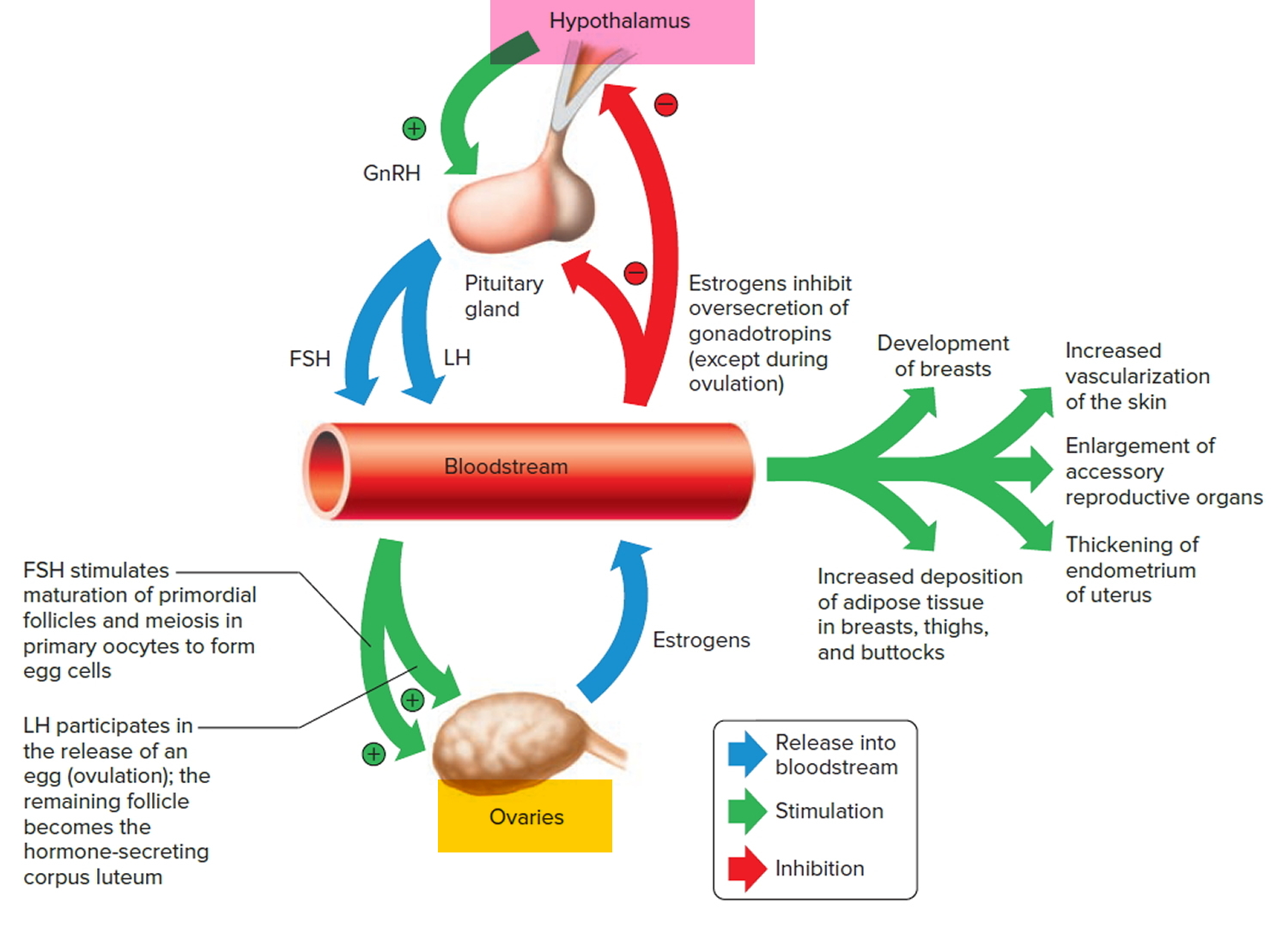
Luteinizing hormone (LH) is a hormone associated with reproduction and the stimulation of the release of an egg from the ovary (ovulation) in women and testosterone production in men. Luteinizing hormone is produced and released by the anterior pituitary gland, a grape-sized organ found at the base of your brain (see Figures 1 and 2). Control of luteinizing hormone (LH) production is a complex system involving the hypothalamus in the brain, the pituitary gland, and the hormones produced by the ovaries and testicles (see Figures 3 and 4). Luteinizing hormone (LH) is considered a gonadotrophic hormone because of its role in controlling the function of ovaries in females and testes in males, which are known as the gonads.
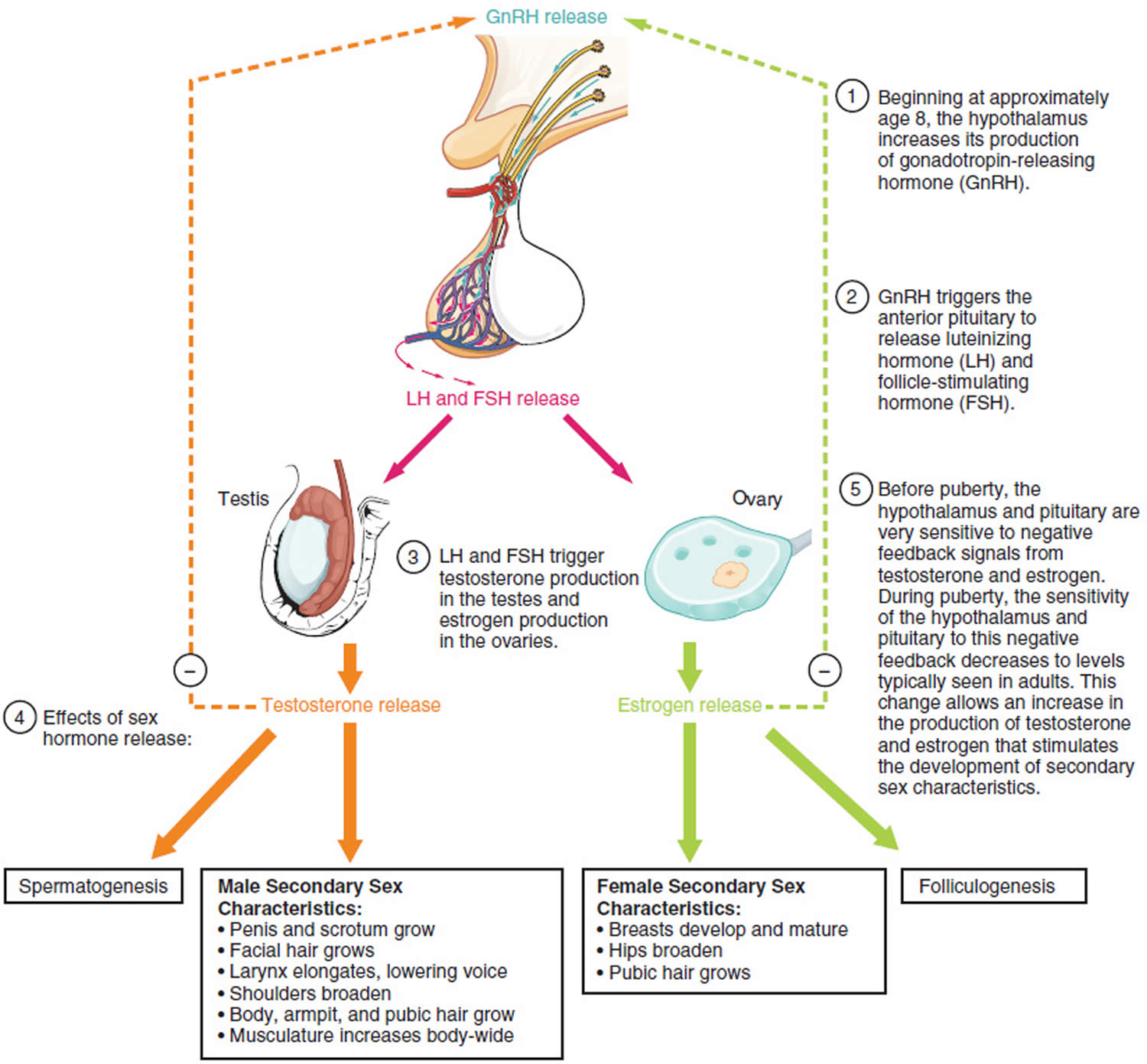
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) control the production of the sex hormones. Synthesis and release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are stimulated mainly by gonadotropin-releasing hormone (GnRH) and suppressed by estrogen and testosterone (see Figures 3 and 4). One factor controlling gonadotropin-releasing hormone (GnRH) release is kisspeptin, a hypothalamic peptide that is triggered by increased leptin levels at puberty. Two gonadal hormones, activin and inhibin, affect only FSH; activin is stimulative, and inhibin is inhibitory.
In women, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) stimulate ovarian follicular development and ovulation. In men, follicle-stimulating hormone (FSH) acts on Sertoli cells and is essential for spermatogenesis; luteinizing hormone (LH) acts on Leydig cells of the testes to stimulate testosterone biosynthesis.
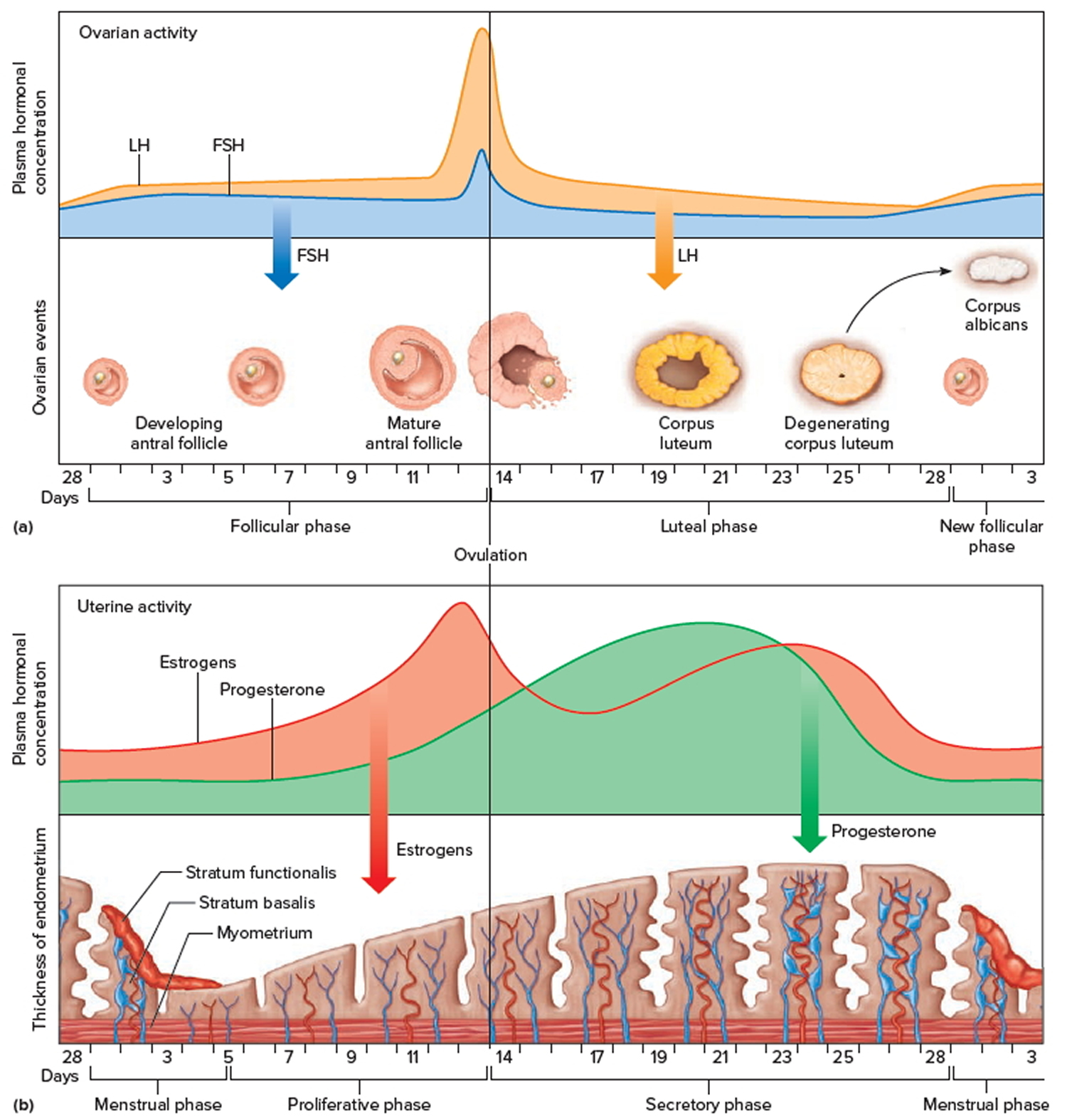
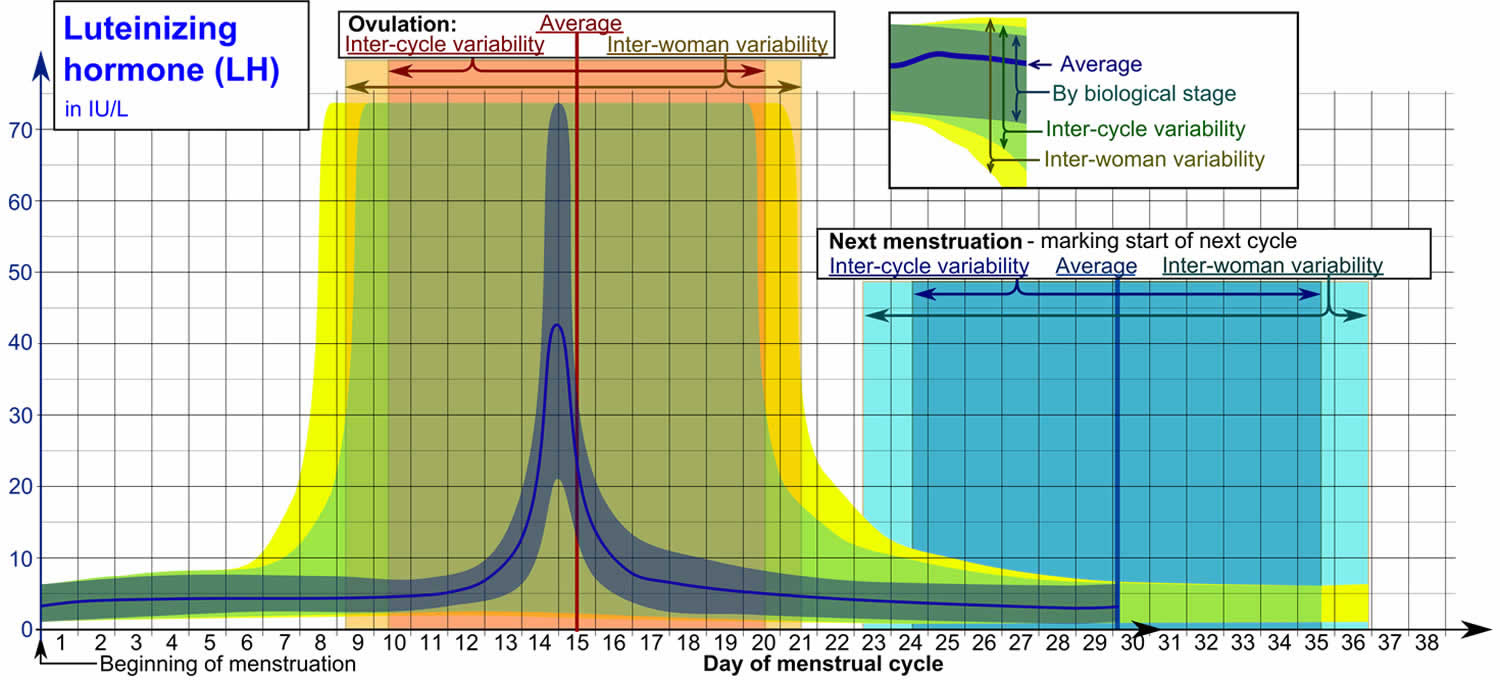
In premenopausal women, several hormones rise and fall in a specific sequence during each menstrual cycle. During the menstrual cycle, luteinizing hormone stimulates ovulation and the production of other hormones, estradiol and progesterone (see Figure 6). Womens’ menstrual cycles are divided into follicular and luteal phases, with each phase lasting about 14 days. Near the end of the follicular phase, there is a mid-cycle surge of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). This surge triggers ovulation, causing the rupture of the egg follicle on the ovary and the release of the egg and also initiating the conversion of the residual follicle into a “corpus luteum”. Luteinizing hormone secretion stimulates the corpus luteum to start producing progesterone to prepare the endometrium for a possible implantation. Luteinizing hormone (LH) is necessary to maintain luteal function for the first 2 weeks of pregnancy. In case of pregnancy, luteal function will be further maintained by the action of hCG (human chorionic gonadotropin) from the newly established pregnancy. Follicle-stimulating hormone (FSH) and luteinizing hormone levels decline, while progesterone and estradiol concentrations increase. These hormone levels decrease in turn after several days if the egg is not fertilized. Menstruation starts and when it ends, the cycle begins again.
As a woman ages and menopause approaches, ovarian function wanes and eventually ceases. As this occurs, follicle-stimulating hormone (FSH) and luteinizing hormone levels rise.
Luteinizing hormone is sometimes referred to as interstitial cell stimulating hormone in males. In men, luteinizing hormone stimulates Leydig cells in the testicles to produce testosterone. Luteinizing hormone levels are relatively constant in men after puberty. A high testosterone level provides negative feedback to the pituitary gland and the hypothalamus, thus decreasing the amount of luteinizing hormone secreted.
In infants and children, luteinizing hormone levels rise shortly after birth and then fall to very low levels (by 6 months in boys and 1-2 years in girls). At about 6-8 years, levels again rise before the beginning of puberty and the development of secondary sexual characteristics.
Figure 1. The pituitary gland location
Figure 2. The hypothalamus and pituitary gland (anterior and posterior) endocrine pathways and target organs
Figure 3. Gonadotropins (FSH and LH)
Figure 4. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
Figure 5. Ovarian activity during the Menstrual cycle
Figure 6. Luteinizing hormone levels
I’m having a hard time getting pregnant. What tests do I need?
Basic tests for infertility in women often include measuring luteinizing hormone and follicle-stimulating hormone (FSH) levels. Your healthcare provider may also ask you to keep track of your body temperature, which rises slightly during ovulation. Other hormonal tests as well as a postcoital (after intercourse) examination may also be done. A hysterosalpingogram (image of fallopian tubes) may be ordered to see whether your fallopian tubes are blocked. Your partner may be asked to give a specimen of semen for analysis.
Can the luteinizing hormone test be used to tell if I have ovulated?
The luteinizing hormone test is often used to predict ovulation by detecting a woman’s monthly pre-ovulation luteinizing hormone surge. It indicates ovulation but cannot, however, be used to confirm that ovulation has occurred.
Why would a man need a test for FSH and luteinizing hormone; I thought these were female hormones?
Men also produce follicle-stimulating hormone (FSH) and luteinizing hormone. These hormone levels are important for the male reproduction process, whereby FSH stimulates the testes to produce sperm. This is analogous to FSH stimulation of the ovaries to produce eggs. In men, luteinizing hormone may be measured if testosterone levels are low, because luteinizing hormone stimulates Leydig cells in the testicles to produce testosterone.
Is there a home test for luteinizing hormone?
Yes, there is a home test that uses a urine sample to help predict ovulation. For more information, visit the following FDA web site (https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/HomeUseTests/ucm126065.htm). This home-use test kit measure luteinizing hormone (LH) in your urine. This helps detect the luteinizing hormone surge that happens in the middle of your menstrual cycle, about 1-1½ days before your ovulation. Some tests also measure another hormone — estrone-3-glucuronide (E3G). A positive result indicates an “luteinizing hormone surge.” This is a sign that ovulation may soon occur.
Estrone-3-glucuronide (E3G) is produced when estrogen breaks down in your body. It accumulates in your urine around the time of ovulation and causes your cervical mucus to become thin and slippery. Sperm may swim more easily in your thin and slippery cervical mucus, increasing your chances of getting pregnant.
Why should I do this home test?
You should do this test if you want to know when you expect to ovulate and be in the most fertile part of your menstrual cycle. This test can be used to help you plan to become pregnant. You should not use this test to help prevent pregnancy, because it is not reliable for that purpose.
How accurate is this home test?
How well this test will predict your fertile period depends on how well you follow the instructions. These tests can detect luteinizing hormone and estrone-3-glucuronide (E3G) reliably about 9 times out of 10, but you must do the test carefully.
How do I prepare for this home test?
DO NOT drink large amounts of fluids before using the test.
Drugs that can decrease luteinizing hormone levels include estrogens, progesterone, and testosterone. Estrogens and progesterone may be found in birth control pills and hormone replacement therapy.
The drug clomiphene citrate (Clomid) can increase LH levels. This drug is used to help trigger ovulation.
How do I do this test?
You add a few drops of your urine to the test kit, hold the tip of the test in your urine stream, or dip the test in a cup of your urine. You either read the test by looking for colored lines on the test or you put the test device into a monitor. You can get results in about 5 minutes. The details of what the color looks like, or how to use the monitor varies among the different brands.
Most kits come with multiple tests to allow you to take measurements over several days. This can help you find your most fertile period, the time during your cycle when you can expect to ovulate based on your hormone levels. Follow the instructions carefully to get good results. You will need to start your testing at the proper time during your cycle, otherwise the test will be unreliable, and you will not find your hormonal surges or your fertile period.
Is this test similar to the one my doctor uses?
The fertility tests your doctor uses are automated, and they may give more consistent results. Your doctor may use other tests that are not yet available for home use (i.e., blood and urine laboratory tests) and information about your history to get a better view of your fertility status.
What does luteinizing hormone do?
In women, luteinizing hormone stimulates the ovaries to produce estradiol. Two weeks into a woman’s cycle, a surge in luteinizing hormone causes the ovaries to release an egg during ovulation. If fertilization occurs, luteinizing hormone will stimulate the corpus luteum, which produces progesterone to sustain the pregnancy.
For men, luteinizing hormone stimulates the production of testosterone from Leydig cells in the testes. Testosterone, in turn, stimulates sperm production and helps accentuate male characteristics — like a deep voice or growth of facial hair.
What problems can occur with luteinizing hormone?
People who have high levels of luteinizing hormone may experience infertility, because the hormone directly impacts the reproductive system. In women, luteinizing hormone levels that are too high are often connected to polycystic ovary syndrome (PCOS), which creates inappropriate testosterone levels. Some genetic conditions, like Turner syndrome or Klinefelter syndrome, can cause high levels of the hormone, as well. People with these conditions are often unable to reproduce.
Low levels of luteinizing hormone can also cause infertility, because insufficient levels will limit the production of sperm or the ovulation process. Too little luteinizing hormone stops ovulation in women or creates a deficiency in gonadotrophin-releasing hormone (GnRH) secretion in men.
Luteinizing hormone test
The luteinizing hormone test, a hormone associated with reproduction and the stimulation of the release of an egg from the ovary (ovulation) in women and testosterone production in men, has several uses.
In both women and men, luteinizing hormone is often used in conjunction with other tests (FSH, testosterone, estradiol and progesterone):
- In the workup of infertility
- To aid in the diagnosis of pituitary disorders that can affect luteinizing hormone production
- To help diagnose conditions associated with dysfunction of the ovaries or testicles
In women, luteinizing hormone levels are useful:
- In the investigation of menstrual irregularities
- To evaluate luteinizing hormone levels during the menstrual cycle; multiple urine luteinizing hormone tests may be ordered for this purpose. These luteinizing hormone “spot tests” can be performed at home and used to detect the surge in luteinizing hormone that indicates that ovulation will occur in the next 1-2 days. The tests can help determine when a woman is likely to be the most fertile.
In children, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are used to diagnose delayed and precocious (early) puberty. Irregular timing of puberty may be an indication of a more serious problem involving the hypothalamus, the pituitary gland, the ovaries or testicles, or other systems. The measurement of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) may differentiate between benign symptoms and true disease. Once it is established that symptoms are a result of true disease, further testing can be done to discern the underlying cause.
In persons with evidence of poor ovarian or testicular function, luteinizing hormone (LH) is sometimes measured in response to administration of gonadotropin releasing hormone (GnRH) to distinguish between disorders involving the hypothalamus or pituitary gland. GnRH is the hormone produced by the hypothalamus that stimulates the pituitary to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). For this test, a baseline blood sample is drawn and then the person is given an injection of gonadotropin releasing hormone (GnRH). Subsequent blood samples are drawn at specified times and the level of luteinizing hormone is measured. This test can help differentiate between a disorder of the pituitary (secondary), when luteinizing hormone will not respond to GnRH, or hypothalamus (tertiary), when luteinizing hormone responds to gonadotropin releasing hormone (GnRH). It is also often helpful in the evaluation of precocious or delayed puberty.
When is luteinizing hormone test ordered?
In adults, luteinizing hormone (LH) (and FSH) tests may be ordered when:
- A woman is having difficulty getting pregnant or has irregular or an absence of menstrual periods
- When it is suspected that a women has entered menopause and her menstrual cycle has stopped or become irregular
- When a man’s partner cannot get pregnant, when he has a low testosterone level, or when he has low muscle mass or decreased sex drive, for example.
- When a health practitioner suspects that a pituitary disorder is present; a pituitary disorder can affect the production of several different hormones so there may be signs and symptoms in addition to infertility that can include fatigue, weakness, unexplained weight loss, and decreased appetite to name a few.
In children, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) may be ordered when a boy or girl does not appear to be entering puberty at an appropriate age (either too late or too soon). Signs of puberty may include:
- Breast enlargement in girls
- Growth of pubic hair
- Growth of testicles and penis in boys
- Beginning of menstruation in girls
Luteinizing hormone normal levels
Males
- Age < or =4 weeks: Not established
- Age >1 month to 12 months: < or =0.4 IU/L
- Age >12 months to 6 years: < or =1.3 IU/L
- Age >6 to 11 years: < or =1.4 IU/L
- Age >11 to 14 years: 0.1-7.8 IU/L
- Age >14 to 18 years: 1.3-9.8 IU/L
- Age >18 years: 1.3-9.6 IU/L
Females
- Age < or =4 weeks: Not established
- Age >1 to 12 months: < or =0.4 IU/L
- Age >12 months to 6 years: < or =0.5 IU/L
- Age >6 to 11 years: < or =3.1 IU/L
- Age >11 to 14 years: < or =11.9 IU/L
- Age >14 to 18 years: 0.5-41.7 IU/L
Premenopausal:
- Follicular: 1.9-14.6 IU/L
- Midcycle: 12.2-118.0 IU/L
- Luteal: 0.7-12.9 IU/L
- Postmenopausal: 5.3-65.4 IU/L
What does abnormal luteinizing hormone levels mean?
Some drugs can cause luteinizing hormone to increase, such as anticonvulsants, clomiphene, and naloxone, while others cause luteinizing hormone to decrease, such as digoxin, oral contraceptives, and hormone treatments.
A recent nuclear medicine scan may interfere with results of the luteinizing hormone test if it is measured by a radioimmunoassay, which is seldom used any more.
Some patients who have been exposed to animal antigens, either in the environment or as part of treatment or imaging procedures, may have circulating antianimal antibodies present. These antibodies may interfere with the assay reagents to produce unreliable results.
In Women
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels can help to differentiate between primary ovarian failure (failure of the ovaries themselves or lack of ovarian development) and secondary ovarian failure (failure of the ovaries due to disorders of either the pituitary or the hypothalamus).
Increased levels of luteinizing hormone and FSH are seen in primary ovarian failure. Some causes of primary ovarian failure are listed below.
Developmental defects:
- Failure to develop ovaries (ovarian agenesis)
- Chromosomal abnormality, such as Turner syndrome
- Defect in steroid production by the ovaries, such as 17 alpha hydroxylase deficiency
Premature ovarian failure due to:
- Exposure to radiation
- Chemotherapy
- Autoimmune disease
Chronic failure to ovulate (anovulation) due to:
- Polycystic ovary syndrome (PCOS)
- Adrenal disease
- Thyroid disease
- Ovarian tumor
In women who are trying to become pregnant, multiple luteinizing hormone tests can be used to detect the surge that precedes ovulation. An luteinizing hormone surge indicates that ovulation has occurred (see Figure 5 above).
During menopause, a woman’s ovaries cease to function; thus luteinizing hormone levels will rise. Postmenopausal luteinizing hormone levels are generally above 40 IU/L. (Note: FSH (follicle-stimulating hormone) is the preferred test to confirm menopausal status).
Low levels of luteinizing hormone and follicle-stimulating hormone (FSH) are seen in secondary ovarian failure and indicate a problem with the pituitary or hypothalamus.
In Men
High luteinizing hormone levels may indicate primary testicular failure. This can be due to developmental defects in testicular growth or to testicular injury, as described below.
Developmental defects:
- Failure to develop gonads (gonadal agenesis)
- Chromosomal abnormality, such as Klinefelter syndrome
Testicular failure:
- Viral infection (mumps)
- Trauma
- Exposure to radiation
- Chemotherapy
- Autoimmune disease
- Germ cell tumor
Low levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are seen in secondary failure of the testicles and indicate a problem with the pituitary or hypothalamus.
In Both Men and Women
In both males and females, primary hypogonadism results in an elevation of basal follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels.
Luteinizing hormone response to gonadotropin releasing hormone (GnRH) can help differentiate between secondary dysfunction (failure of the pituitary) and tertiary disorder (a problem involving the hypothalamus). Once the baseline level of luteinizing hormone has been measured, a dose of GnRH is given by injection. A subsequent increase in the level of luteinizing hormone indicates that the pituitary responded to the GnRH and points to a disorder involving the hypothalamus. A reduced level of luteinizing hormone shows that the pituitary did not respond to the gonadotropin releasing hormone (GnRH) and suggests a disease involving the pituitary.
In Children
In young children, high levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) with the development of secondary sexual characteristics at an unusually young age are an indication of precocious puberty. This is much more common in girls than in boys. This premature development is usually due to a problem with the central nervous system and can have a few different underlying causes. Examples include:
- Central nervous system tumor
- Brain injury, trauma
- Inflammation within the central nervous system (e.g., meningitis, encephalitis)
- Brain surgery
Normal prepubescent levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in children exhibiting some signs of pubertal changes may indicate a condition call “precocious pseudopuberty.” The signs and symptoms are brought on by elevated levels of the hormones estrogen or testosterone. This may be caused by:
- Hormone-secreting tumors
- Adrenal gland tumors
- Ovarian tumors or cysts
- Testicular tumors
Normal luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels with a few signs of puberty can also be a benign form of precocious puberty with no underlying or discernable cause or may just be a normal variation of puberty. In delayed puberty, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels can be normal or below what is expected for a youth within this age range. The test for luteinizing hormone response to GnRH in addition to other testing may help to diagnose the reason for the delayed puberty. Some of the causes for delayed puberty can include:
- Failure of the ovaries or testicles
- Hormone deficiency
- Turner syndrome
- Klinefelter syndrome
- Chronic infections
- Cancer
- Eating disorder (anorexia nervosa)