What are ACE inhibitors
ACE inhibitors is short for angiotensin-converting enzyme inhibitors, are blood pressure drugs or antihypertensive medications that are widely used to treat high blood pressure (hypertension). ACE inhibitors medications help relax blood vessels by blocking the formation of a natural chemical that narrows blood vessels. ACE inhibitors may be especially important in treating high blood pressure in people with coronary artery disease, heart failure or kidney failure caused by diabetes. The ACE inhibitors are considered first line drugs for the therapy of hypertension and are considered particularly helpful in preventing the kidney complications of diabetes and high blood pressure. ACE inhibitors are sometimes used even in patients with relatively normal blood pressure for treatment of heart failure and prevention of diabetic nephropathy. For diabetic nephropathy, start ACE inhibitors at onset of microalbuminuria in all diabetic patients 1. Some small studies have shown slowing of onset of microalbuminuria in nonalbuminuric patients; whether this affects outcome is not known.
Clinical outcomes of ACE inhibition include decreases in heart attack (fatal and non-fatal), reinfarction (another heart attack), angina, stroke, end-stage kidney failure, and morbidity and mortality associated with heart failure 1.
Most people who have heart failure take ACE inhibitors medicines. ACE inhibitors have been shown to be beneficial with increased benefit in those with more severe systolic dysfunction 1. ACE inhibitors reduce mortality, rate of progression of heart failure, rate of sudden death or fatal myocardial infarction, and rate of hospital admission. Target dosages should be those used in the therapeutic trials. Several studies suggest that higher dosages produce greater hemodynamic and prognostic benefit than lower dosages 2.
ACE inhibitors medicines treat high blood pressure, strokes, or heart attacks. They may help lower your risk for stroke or heart attack.
ACE inhibitors are also used to treat diabetes and kidney problems. This can help keep your kidneys from getting worse. If you have these problems, ask your health care provider if you should be taking ACE inhibitors.
ACE inhibitors generally don’t work as well in people of African heritage when prescribed alone, but they may be effective when combined with other blood pressure medications.
Currently, there are 10 ACE inhibitors approved for use in the United States: captopril (Capoten: 1981), enalapril (Vasotec: 1985), lisinopril (Prinivil, Zestril: 1987), benazepril (Lotensin: 1991), fosinopril (Monopril: 1991), quinapril (Accupril: 1991), ramipril (Altase: 1991), perindopril (Aceon: 1993), moexipril (Univasc: 1995), and trandolapril (Mavik: 1996).
Possible side effects include dizziness and a cough, and these medications aren’t recommended during pregnancy.
Do not take an ACE inhibitor if you are pregnant or plan to become pregnant. If you become pregnant while taking an ACE inhibitor, call your doctor immediately. ACE inhibitor may harm the fetus.
ACE inhibitors are not considered teratogenic if they are discontinued during the first trimester (class C), but they are considered teratogenic in the second and third trimesters (class D).
FDA Pregnancy Category C
Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
FDA Pregnancy Category D
There is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
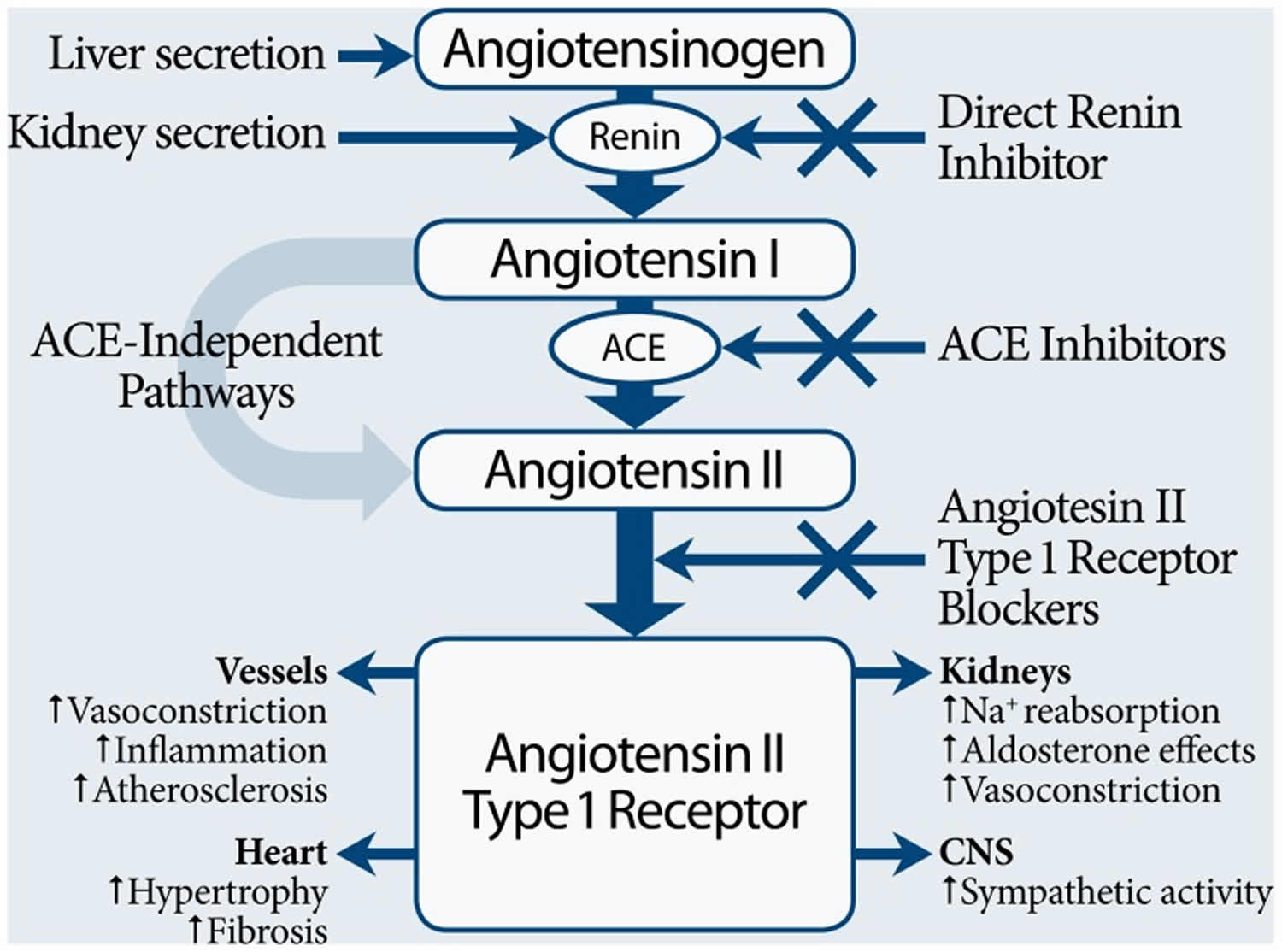
What do ACE inhibitors do
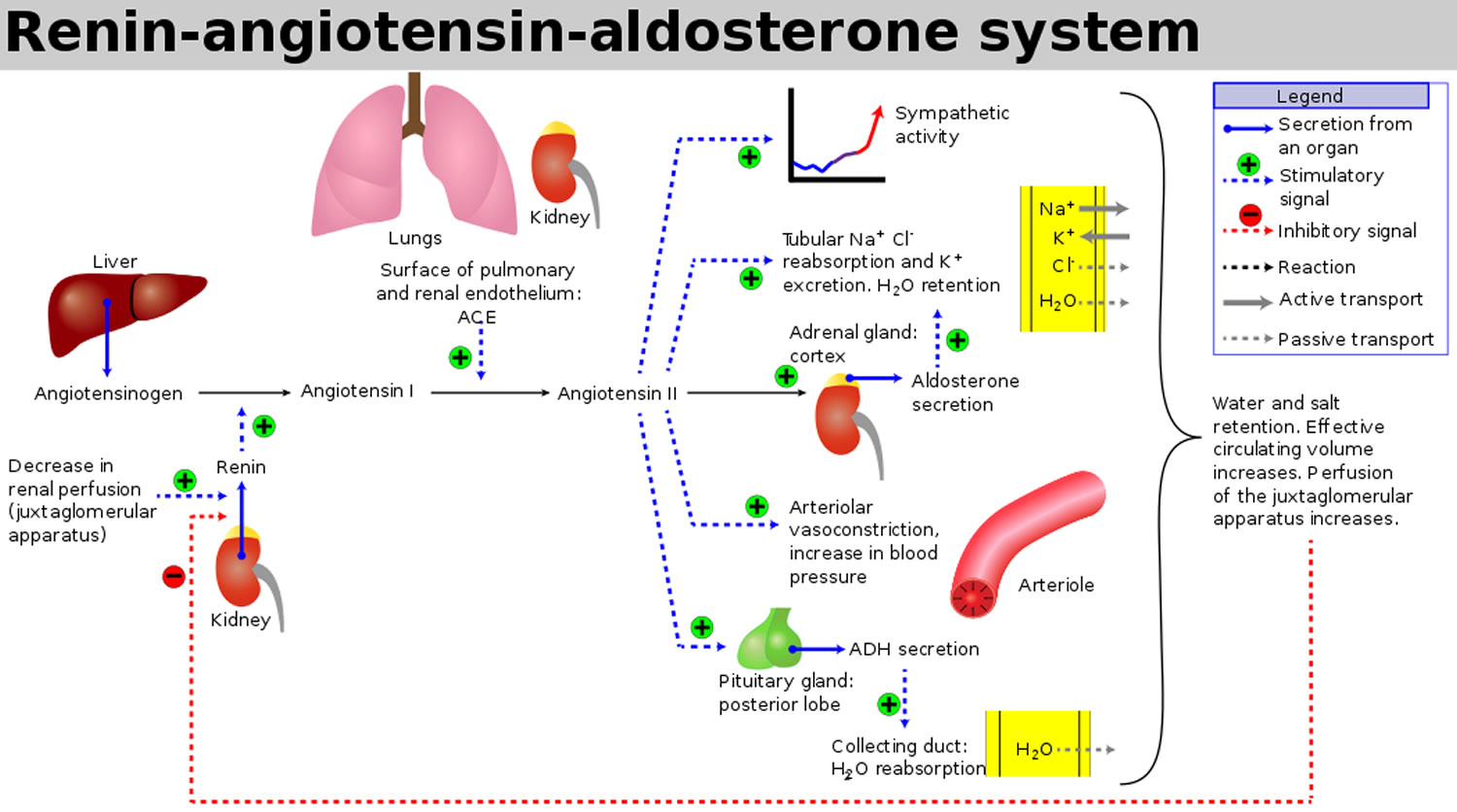
ACE inhibitors act by blocking the conversion of angiotensin 1 to angiotensin 2, the active peptide that causes the blood vessels to become narrower (vasoconstriction) and sodium retention induced by activation of the renin-angiotensin pathway, thus inhibiting an intermediate step in the renin-angiotensin pathway. ACE inhibitors have been shown to reduce morbidity or mortality in congestive heart failure, heart attack (myocardial infarction), diabetes mellitus, chronic renal insufficiency, and atherosclerotic cardiovascular disease. Angiotensin 2 contributes to endothelial dysfunction, altered renal hemodynamics, and vascular and cardiac hypertrophy. ACE inhibitors attenuate these effects.
Figure 1. Angiotensin 1 and Angiotensin 2 production
Figure 2. Renin angiotensin aldosterone system
ACE inhibitors mechanism of action
Ten ACE inhibitors presently approved for use in the United States work by competitive inhibition of angiotensin-converting enzymes (ACE). Captopril (Capoten) and enalapril (Vasotec) are off-patent, which makes them more economical. Enalapril is the only one available in intravenous form, which is called enalaprilat (Vasotec-IV). Drug formularies may dictate which ACE inhibitor a physician is able to prescribe because they are thought to be interchangeable. If a choice is possible, physicians should use those agents that have been proved by clinical trials to reduce morbidity and mortality for the condition being treated and work toward target dosages or clinical end points (Table 1) 2.
Table 1. Comparison of ACE inhibitors
| Agent | Availability | Dosages* | Considerations | Cost (generic)† | |
|---|---|---|---|---|---|
Benazepril (Lotensin) | 5, 10, 20, 40 mg | Hypertension | — | $ 27 | |
Start: 10 mg daily | |||||
Target: 20 to 40 mg daily | |||||
Maximum: 80 mg daily | |||||
Captopril (Capoten) | 12.5, 25, 50, 100 mg | Hypertension | Food decreases absorption, but blood levels do not correlate with blood pressure response | $59 to 88 (20 to 68) | |
25 to 50 mg two or three times daily | |||||
Congestive heart failure | $151 (100 to 118) | ||||
Start: 6.25 to 25 mg three times daily | |||||
Target: 50 to 100 mg three times daily | |||||
Left ventricular dysfunction after myocardial infarction | |||||
Start: 6.25 mg daily | |||||
Target: 50 mg three times daily | |||||
Diabetic nephropathy‡ | $88 (58 to 68) | ||||
25 mg three times daily | |||||
Maximum: 450 mg daily | |||||
Enalapril (Vasotec) | 2.5§, 5§, 10, 20 mg | Hypertension | — | $36 (31 to 32) | |
Start: 5 mg daily | |||||
Range: 10 to 40 mg once daily or in two divided doses | |||||
Congestive heart failure | $101 (88 to 91) | ||||
Start: 2.5 mg daily | |||||
Target: 40 mg daily in two divided doses | |||||
Asymptomatic left ventricular dysfunction | $72 (62 to 64) | ||||
Start: 2.5 mg twice daily | |||||
Target: 20 mg daily in two divided doses | |||||
Maximum: 40 mg daily | |||||
Fosinopril (Monopril) | 10§, 20, 40 mg | Hypertension | May cause false low serum digoxin levels Patients with impaired liver function may have elevated plasma levels | $29 | |
Start: 10 mg daily | |||||
Target: 40 mg daily | |||||
Congestive heart failure | $29 | ||||
Start: 10 mg daily | |||||
Target: 20 to 40 mg daily | |||||
Maximum: 80 mg daily | |||||
Lisinopril (Prinivil§, Zestril) | 2.5, 5§, 10, 20, 30, 40 mg | Hypertension | — | $30 | |
Start: 10 mg daily | |||||
Target: 20 to 40 mg daily | |||||
Congestive heart failure | $30 | ||||
Start: 5 mg daily | |||||
Target: 20 mg daily | |||||
Acute myocardial infarction | $29 | ||||
Start: 5 mg daily for two days, then 10 mg daily for six weeks, then re-evaluate | |||||
Maximum: 40 mg daily | |||||
Moexipril (Univasc) | 7.5§, 15§ mg | Hypertension | — | $20 | |
Start: 7.5 mg daily one hour before meals | |||||
Target: 7.5 to 30 mg in one dose or two divided doses one hour before meals | |||||
Maximum: 30 mg daily | |||||
Perindopril (Aceon) | 2§, 4§, 8§ mg | Hypertension | Cautious administration with gentamicin|| | $30 | |
Start: 4 mg daily | |||||
Target: 4 to 8 mg daily | |||||
Maximum: 16 mg daily | |||||
Quinapril (Accupril) | 5§, 10, 20, 40 mg | Hypertension | Food decreases absorption | $32 | |
Start: 10 mg daily | |||||
Target: 80 mg daily | |||||
| Congestive heart failure | $64 | ||||
Start: 5 mg twice daily, titrate weekly to 20 to 40 mg in divided doses | |||||
Maximum: 80 mg daily | |||||
Ramipril (Altace) | 1.25, 2.5, 5, 10 mg | Hypertension | Patients with impaired liver function may have elevated plasma levels | $30 | |
Start: 2.5 mg daily | |||||
Target: 2.5 to 20 mg daily in one dose or two divided dose | |||||
Heart failure after myocardial infarction | $33 | ||||
Start: 2.5 mg twice daily | |||||
Target: 5 mg twice daily | |||||
Risk reduction of cardiovascular events in at-risk patients: 10 mg daily¶ | |||||
Maximum: 20 mg daily | |||||
Trandolapril (Mavik) | 1§, 2, 4 mg | Hypertension | Food decreases absorption | $24 | |
Start: 1 mg daily (2 mg daily in black patients) | |||||
Target: 2 to 4 mg per day | |||||
Heart failure after myocardial infarction | $24 | ||||
Start: 1 mg daily | |||||
Target: 4 mg daily | |||||
Left ventricular dysfunction after myocardial infarction | $24 | ||||
Start: 1 mg daily | |||||
Target: 4 mg daily | |||||
Maximum: 8 mg daily | |||||
Footnote: Recommendations assume reduction in dosing if hypotension occurs, if the patient is hyponatremic, or if the patient is taking a diuretic.
*—If the patient is taking a diuretic or the creatinine clearance is less than 30 to 40 mL per minute, reduce the starting dose by one half or hold the same dosage for three days before starting ACE inhibitor therapy.
†—Estimated cost to the pharmacist based on average wholesale prices for lowest target dosage level and 30 days of therapy (except where noted), in Red book.
Montvale, N.J.: Medical Economics Data, 2001. Cost to the patient will be higher, depending on prescription filling fee.
‡—Off-label use.
§—Tablet is scored.
∥—Animal studies only.
¶—Heart Outcomes Prevention Evaluation (HOPE) trial 3
[Source 1 ]ACE inhibitors for heart failure
ACE inhibitors are first-line therapy in patients with left ventricular systolic dysfunction, as confirmed in multiple trials and meta-analyses 1. Decreases in dyspnea (shortness of breath), emergency department visits, hospitalizations, disease progression, death, and the need for diuretics have been proved, as well as increases in ejection fraction and exercise tolerance 4. All patients with systolic dysfunction, even if they are asymptomatic, should be considered for treatment with an ACE inhibitor. This consideration mandates wide use of cardiac imaging to identify the presence and type of heart failure.
Target dosages used in the clinical trials that showed reduced morbidity and mortality are listed in Table 1 above. Starting doses should be determined individually and based on clinical status (i.e., blood pressure, serum sodium level) and comorbidities (i.e., age, renal insufficiency). When the dosage is titrated up, the diuretic dosage will probably need to be decreased.
Diuretics, while essential for controlling volume overload, do not confer mortality reduction like the first-line therapies of ACE inhibition and beta blockade. The one exception to this is spironolactone (Aldactone), which has shown mortality reduction in Class III and IV heart failure 5.
ACE inhibitors other uses
High blood pressure
Guidelines for the pharmacologic management of hypertension issued by the World Health Organization and the International Society of Hypertension place ACE inhibitors with diuretics and beta blockers as first-line therapy. The Sixth Report of the Joint National Committee (1997) removed ACE inhibitors as first-line therapy because they had not been shown in clinical trials to reduce all-cause mortality as had diuretics and beta blockers 6.
In 1999, the Captopril Prevention Project19 randomized trial compared the three agents. Captopril and conventional treatment did not differ in cardiovascular end points overall; all events except for stroke were lower in the captopril group. Improper randomization has been cited as a possible reason for increased stroke rates 7. The results of the Swedish Trial in Old Patients with Hypertension-2 study 8 showed equal outcomes between the three drug classes.
ACE inhibitors have a side effect profile that may place them above thiazides and beta blockers. They do not affect lipid, calcium, or uric acid levels, and are less likely to cause erectile dysfunction than other antihypertensive agents 9. There is evidence from several trials that fasting glucose levels, glycosylated hemoglobin levels, and rates of new diagnoses of type 2 diabetes are lower in patients randomized to ACE inhibitor therapy than in those taking placebo. The Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication (DREAM) trial will evaluate prospectively whether this ACE inhibitor prevents diabetes 10. Treatment goals for blood pressure include 140/90 mm Hg (or less) in patients without comorbidities, 130/80 mm Hg (or less) in patients with diabetes (2001 American Diabetes Association [ADA] Guidelines) and 125/75 mm Hg (or less) in those with end organ damage.
Heart attack
In 1996 and 1999, the American Heart Association advocated the administration of an ACE inhibitor to all patients presenting with acute anterior myocardial infarction and/or clinical heart failure in the absence of hypotension or other contraindications. The guidelines recommend starting within the first 24 hours and continuing therapy indefinitely for anterior infarctions and left ventricular dysfunction 11.
A pragmatic approach is to give ACE inhibitors to all patients with acute myocardial infarction who are clinically stable and to continue that therapy indefinitely in those with anterior myocardial infarction or systolic dysfunction. Others should be re-evaluated for continuation of therapy at four to six weeks 12.
Diabetes
ACE inhibitors slow the onset of diabetic nephropathy in patients with microalbuminuria and type 1 diabetes 13. Normotensive, nonalbuminuric diabetics also have a slower onset of nephropathy; however, the American Diabetes Association [ADA] currently does not recommend ACE inhibitors as primary prevention in these patients, and there is no evidence that this practice affects outcomes 14.
In the MICRO-HOPE trial, patients with diabetes and one cardiac risk factor were studied; subjects were titrated to 10 mg a day of ramipril or placebo. The study was stopped prematurely because of the significant decrease in combined primary outcomes in patients taking ramipril. Total cardiovascular end points were reduced by 25 percent; these included myocardial infarction (22 percent), cerebrovascular accident (33 percent), cerebrovascular death (37 percent), total mortality (24 percent), revascularization (17 percent) and overt nephropathy (24 percent) 3. Ramipril was approved by the U.S. Food and Drug Administration in November 2000 for primary prevention of cardiovascular events in at-risk patients.
A meta-analysis of four trials including 1,123 patients with type 2 diabetes showed improved outcomes in those taking ACE inhibitors as opposed to other antihypertensive agents 15. The authors noted in their conclusions that atenolol (Tenormin) may be equivalent to captopril and that further studies are needed in regard to these two agents 15. It will be rare for a patient with diabetes not to meet the criteria for ACE inhibition in the year 2002.
Renal insufficiency
The Kidney Disease: Improving Global Outcomes guideline 16 recommends ACE inhibitors or angiotensin receptor blockers (ARBs) for adults with chronic kidney disease (CKD) with or without diabetes who have a urinary albumin excretion rate of 30 to 300 mg per 24 hours and in whom blood pressure medications are indicated. The guideline recommends a blood pressure goal of 130/80 mm Hg or less in these patients 16. The American Diabetes Association recommends ACE inhibitors or angiotensin receptor blockers (ARBs) for nonpregnant patients with diabetes and microalbuminuria, but it makes no specific recommendations for blood pressure beyond its standard goals 17. The National Kidney Foundation recommends an ACE inhibitor or angiotensin receptor blocker (ARB) in normotensive patients with diabetes and an albumin level greater than 30 mg per g who are at high risk of chronic kidney disease (CKD) or progression 18. The National Kidney Foundation guideline does not provide recommendations for normotensive patients without diabetes.
ACE inhibitors in nondiabetic patients with nephropathy are more effective than other antihypertensives at slowing progression to end-stage renal disease 19. The Ramipril Efficacy in Nephropathy (REIN) study 19 (treatment goal: diastolic blood pressure less than 90 mm Hg) and the Angiotensin-Converting Enzyme Inhibition in Progressive Renal Insufficiency (AIPRI) study 19 (treatment: benazepril, in a dosage of 10 mg daily) demonstrated improved renal survival. Even in normotensive patients with nondiabetic proteinuria, the EUCLID study group demonstrated slowing of progression of renal disease 20. Unless contraindicated, ACE inhibitors should be used in patients with renal insufficiency of any cause with a goal blood pressure of 125/75 mm Hg in those with more than 1,000 mg per 24 hours (1 g per 24 hours) proteinuria 19.
ACE inhibitors also reduce the risk of progression to macroalbuminuria in normotensive patients with microalbuminuria and type 1 diabetes mellitus 21. ACE inhibitors and angiotensin receptor blockers (ARBs) reduce the risk of progression to macroalbuminuria in normotensive patients with microalbuminuria and type 2 diabetes 21. ACE inhibitors and angiotensin receptor blockers (ARBs) do not reliably affect serum creatinine levels. Recommendations are not available for normotensive patients without diabetes who have microalbuminuria 21.
ACE inhibitors contraindications
ACE inhibitors are contraindicated in patients who are hypersensitive to any other ACE inhibitor (e.g., a patient who has experienced angioedema during therapy with any other ACE inhibitor). Angioneurotic edema, which occurs in 0.1 to 0.2 percent of patients, usually develops within the first week of therapy but can occur at any time 1. This potentially life-threatening adverse effect also occurs with angiotensin 2 receptor blockers but to a lesser extent 9. Any patient with a history of angioneurotic edema, whether related to an ACE inhibitor, angiotensin receptor blockers, or another cause, should not be given an ACE inhibitor. Other contraindications include pregnancy, renal artery stenosis, and previous allergy to ACE inhibitors.
ACE inhibitors side effects
Side effects from ACE inhibitors are rare.
You may have a dry cough. This may go away after a while. If it does not, tell your provider. Sometimes reducing your dose helps. But sometimes, your provider will switch you to a different medicine. DO NOT lower your dose without talking with your provider first.
You may feel dizzy or lightheaded when you start taking these medicines, or if your provider increases your dose. Standing up slowly from a chair or your bed may help. If you have a fainting spell, call your provider right away.
Other side effects include:
- Headache
- Fatigue
- Loss of appetite
- Upset stomach
- Diarrhea
- Numbness
- Fever
- Skin rashes or blisters
- Joint pain
If your tongue or lips swell, call your provider right away, or go to the emergency room. You may be having a serious allergic reaction to the medicine. This is very rare.
See your doctor if you are having any of the side effects listed above. Also see your doctor if you are having any other unusual symptoms.
Angioedema
Presumably because ACE inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors may be subject to a variety of adverse reactions, some of them serious.
Angioedema is swelling underneath the skin. It’s usually a reaction to a trigger, such as a medication ACE inhibitors for high blood pressure – this is known as “drug-induced angioedema” or something you’re allergic to. Angioedema occurring with ACE inhibitors was first reported in 1980 22 and may account for 40% of angioedema presentations to hospital 23. An incidence of 0.68% over six months has been reported, so annual incidence may be greater than 1% 24. Rates in people of African origin are even higher, at 1.62% over six months, so may be over 3% annually 24.
Angioedema isn’t normally serious, but it can be a recurring problem for some people and can very occasionally be life-threatening if it affects breathing.
Treatment can usually help keep the swelling under control.
Symptoms of angioedema
The swelling most often affects the:
- hands
- feet
- area around the eyes
- lips and tongue
- genitals
Many people also have a raised, itchy rash called urticaria (hives).
In more serious cases, angioedema can also cause breathing difficulties, tummy (abdominal) pain and dizziness.
Treatments for angioedema
The swelling will usually get better by itself in a few days, but there are treatments that can help it settle faster and reduce the risk of it happening again.
The treatments recommended depend on the type of angioedema you have. For example:
- allergic and idiopathic angioedema are usually treated with antihistamines or occasionally steroid medication to reduce the swelling
- drug-induced angioedema will usually resolve if you change to a different medication – your doctor will advise you about this. This is usually all that needs to be done. Tell your doctor if your symptoms continue or come back after switching medication.
- hereditary angioedema can’t be cured, but medications can help prevent swelling and quickly treat swelling when it occurs
Angioedema can usually be treated at home, although treatment in hospital may be necessary in serious cases. If you have a particularly serious allergy, you may be given adrenaline auto-injectors to use if you experience a severe allergic reaction (anaphylaxis). There are several types of auto-injector, which are used in slightly different ways.
ACE inhibitors hyperkalemia
Hyperkalemia (high blood potassium) does not usually occur in patients with normal kidney function, but those who have renal insufficiency or diabetes. Patients who are taking potassium, salt substitutes, potassium-sparing diuretics, beta blockers, and NSAIDs (nonsteroidal anti-inflammatory drugs) are susceptible. Most clinicians discontinue potassium and potassium-sparing diuretics when starting patients on ACE inhibitor therapy. Potassium levels should be monitored carefully in patients at risk. Up to 5 percent of patients experience serum potassium levels greater than 5.7 mEq per L (5.7 mmol per L), and if levels remain higher than that on repeat testing, ACE inhibitor therapy should be discontinued.
Cough
Cough occurs in 5 to 20 percent of patients. It is not dose- or brand-related, is more frequent in women than men, and is more frequent in blacks than whites. It develops within one week to six months and resolves within four days of cessation. Physicians should be aware of a confounding congestive heart failure cough and remember that changing to another formulation sometimes helps. Cough is not a reason to discontinue treatment unless the patient cannot tolerate it. A few studies have looked at the use of nonsteroidal anti-inflammatory drugs (NSAIDs), nifedipine (Procardia), cromolyn (Intal), or nebulized bupivacaine (Marcaine) for managing cough, but further studies are needed 25.
Renal insufficiency
In patients with renal insufficiency, no creatinine level is an absolute contraindication to ACE inhibitor therapy. ACE inhibitors are not nephrotoxic. Baseline serum creatinine levels of up to 3.0 mg per dL (27 μmol per L) are generally considered safe. The manufacturers make recommendations for initiating treatment and suggest titrating the dosage slowly. An increase of 20 percent in the serum creatinine level is not uncommon and is not a cause for discontinuing the medication. For any higher increase, the family physician should consider a nephrologist. During the first four weeks of treatment, serum potassium and creatinine levels should be monitored closely.
Hypotension
Hypotension can occur in patients with volume depletion or hyponatremia (sodium <130 mEq per L [<130 mmol per L]), those taking vasodilators, those in acute congestive heart failure, and those on dialysis. The underlying problem should be corrected, starting with a low dosage and titrating slowly. Any patient with a high plasma renin level is vulnerable to first-dose hypotension, but this effect is transient and unpredictable 26. Hypotension is not a reason to discontinue ACE inhibition. Patients should be rechallenged at one half the previous dosage. If they are taking a diuretic, the dosage should be reduced or held for three days before reattempting therapy.
Other Considerations
Neutropenia occurs rarely and tends to occur in patients with renal impairment and concurrent collagen vascular disease. Lithium toxicity is also rare, but lithium levels should be monitored if the patient is on concurrent lithium therapy. Aortic stenosis and hypertropic cardiomyopathies are considered relative contraindications because of the risk of hypotension from fixed outlet obstruction.
References- Using ACE Inhibitors Appropriately. Am Fam Physician. 2002 Aug 1;66(3):461-469. https://www.aafp.org/afp/2002/0801/p461.html
- Physicians’ desk reference, 2001. 55th ed. Montvale, N.J.: Medical Economics, 2001.
- The Heart Outcomes Prevention Evaluation Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet. 2000;355:253–9.
- American College of Cardiology. Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Am J Cardiol. 1999;83:1A–38A.
- Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999;341:709–17.
- The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. McLean, Va.: International Medical Publishing, 1997; NIH publication no. 98-4080.
- Fournier A, Pruna A, Esper NE, Makdassi R, Oprisiu R, West-eel PF, et al. Captopril prevention project—what shall we do about captopril and the risk of stroke?. Nephrol Dial Transplant. 2000;15:2–5.
- Hansson L, Lindholm LH, Ekbom T, Dahlof B, Lanke J, Schersten B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354:1751–6.
- Gifford RW Jr. Antihypertensive therapy. Angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists, and calcium antagonists. Med Clin North Am. 1997;81:1319–33.
- Yusef S, Gerstein H, Hoogwerf B, Pogue J, Bosch J, Wolffen-buttel BH, et al. Ramipril and the development of diabetes. JAMA. 2001;286:1882–5.
- Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, et al. 1999 update: ACC/AHA guidelines for the management of patient with acute myocardial infarction: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation. 1999;100:1016–30.
- Gersh BJ. Optimal management of acute myocardial infarction at the dawn of the next millennium. Am Heart J. 1999;138(2 pt 2):S188–202.
- American Diabetes Association Clinical Practice Recommendations 2001. Diabetes Care. 2001;24(suppl 1):S1–133.
- Ravid M, Brosh D, Levi Z, Bar-Dayan Y, Ravid D, Rachmani R. Use of enalapril to attenuate decline in renal function in normotensive, normoalbuminuric patients with type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med. 1998;128(12 pt 1):982–8.
- Pahor M, Psaty BM, Alderman MH, Applegate WB, Williamson JD, Furberg CD. Therapeutic benefits of ACE inhibitors and other antihypertensive drugs in patients with type 2 diabetes. Diabetes Care. 2000:23:888–92.
- Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012;2(5):337–414.
- American Diabetes Association. Microvascular complications and foot care. Diabetes Care. 2015;38(suppl):S58–S66.
- National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 update [published correction appears in Am J Kidney Dis. 2013;61(6):1049]. Am J Kidney Dis. 2012;60(5):850–886.
- Bakris GL. Improving prognosis of nondiabetic chronic renal insufficiency: the role of ACE inhibitors. Kidney Int (In press).
- Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. The EUCLID study group. Lancet. 1997;349:1787–92.
- ACE Inhibitors or ARBs to Prevent CKD in Patients with Microalbuminuria. Am Fam Physician. 2016 Oct 15;94(8):652-653. https://www.aafp.org/afp/2016/1015/p652.html
- Wilkins JK, Hammond JJ, Kirkendall WM. The captopril-induced eruption. A possible mechanism: cutaneous kinin potentiation. Arch Dermatol 1980;116:902-5
- Banerji A, Clark S, Blanda M, LoVecchio F, Snyder B, Camargo CA Jr. Multicenter study of patients with angiotensin-converting enzyme inhibitor-induced angioedema who present to the emergency department. Ann Allergy Asthma Immunol 2008;100:327-32.
- Kostis JB, Packer M, Black HR, Schmieder R, Henry D, Levy E. Omapatrilat and enalapril in patients with hypertension: the Omapatrilat Cardiovascular Treatment vs Enalapril (OCTAVE) trial. Am J Hypertens 2004;17:103-11.
- Drug facts and comparisons. St. Louis: Facts and Comparisons, 2001:504–9.
- Katzung BG. Basic & clinical pharmacology. 8th ed. Stamford, Conn.: Appleton & Lange, 2001:172–4.