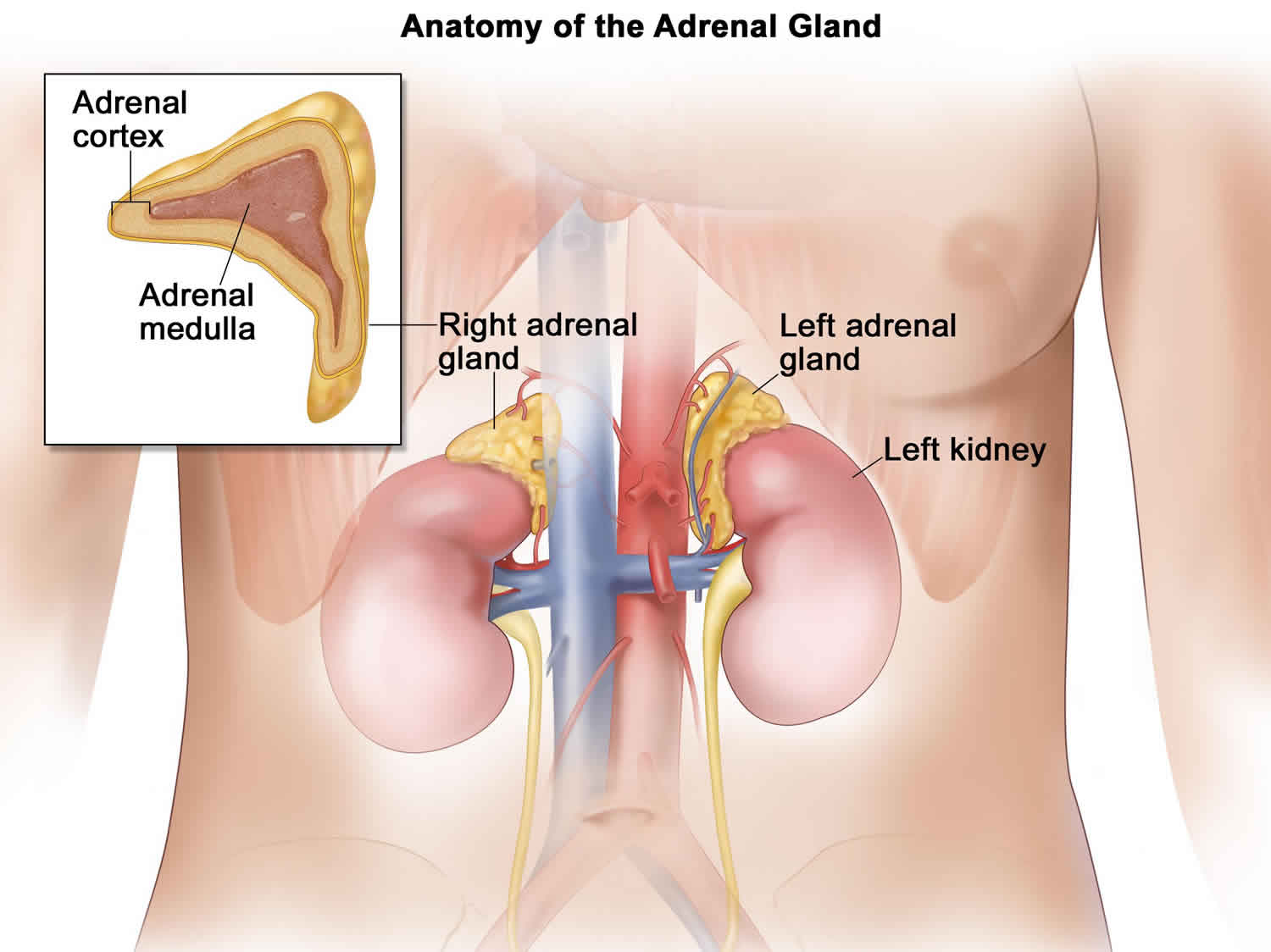
What is adrenal incidentaloma
Adrenal incidentaloma is an unsuspected tumor in one or both of your adrenal glands. Adrenal incidentaloma tumor is usually found by chance during an imaging test, such as an ultrasound or CT scan, for another condition. Usually, the patient has no signs of hormonal excess or obvious underlying malignancy. Adrenal incidentaloma incidence has been increasing proportionally to the use of radiographic imaging 1. Less commonly, adrenal incidentalomas are discovered as part of the clinical workup for suspected adrenal disease (eg, Cushing syndrome) 2.
Adrenal incidentaloma causes
Adrenal incidentaloma has a number of causes. Some causes can make your adrenal glands produce too much of a hormone. This type of tumor is called a hormonally active or functional tumor. Hormonally active causes include:
- Cushing syndrome or subclinical hypercortisolism: Conditions caused by too much cortisol
- Hyperaldosteronism: too much aldosterone: A pheochromocytoma: a rare tumor in the adrenal glands that leads to too much epinephrine and norepinephrine
- Congenital adrenal hyperplasia: An inherited condition in which the adrenal glands make too little cortisol and aldosterone, and too much androgen
- Cancer of the adrenal gland with too much cortisol, adrenal androgens, and/or aldosterone
Other types of causes do not result in excess hormone production. This type of tumor is called a non-functional tumor. Causes include:
- Adrenal adenoma (a non-cancerous tumor in the adrenal glands). Adrenal cortical adenoma is a common benign tumor arising from the cortex of the adrenal gland. It commonly occurs in adults, but it can be found in persons of any age. Adrenal cortical adenomas are not considered to have the potential for malignant transformation.
- Cancer of the adrenal gland or spread of cancer from elsewhere in the body. Because adrenal metastases may be found in as many as 25% of patients with known primary lesions, radiologists frequently face the task of determining whether an adrenal mass is benign or malignant. The question can directly affect the clinical management of the case. For instance, the workup for an otherwise resectable lung cancer may reveal the presence of an adrenal mass and suggest the possibility of metastatic disease.
- Cysts in or on the adrenal glands
- Other less common conditions, such as tumors filled with fat and blood cells
Adrenal incidentaloma symptoms
Even when discovered incidentally, adrenal tumors may cause symptoms. Symptoms vary depending on whether the tumor is non-functional or functional, and which, if any, hormones are produced in excess.
Symptoms of too much cortisol can include:
- Weight loss or weight gain (especially around the face and abdomen)
- Purplish skin stretch marks or skin that’s easily bruised
- Acne
- Muscle weakness
- Depression, anxiety, fatigue, and sleep disturbances
- In women, excess facial and body hair and/or irregular periods
High levels of cortisol can also cause high blood pressure, high blood sugar, and low bone density (when the tissue inside your bones starts to thin).
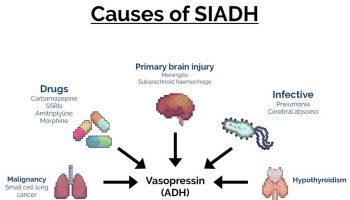
Symptoms of too much norepinephrine or epinephrine can include:
- Fast or irregular heartbeat
- Sweating
- Severe headaches
- Shakiness
- Pale face
- High blood pressure .
High levels of aldosterone can cause high blood pressure, which can be life-threatening if not treated, and sometimes muscle weakness.
Adrenal incidentaloma diagnosis
Your doctor will evaluate your tumor to identify its cause and hormone production. This may include:
- Your medical history
- A review of your symptoms
- A physical exam: a check of your blood pressure, pulse rate, body weight, and other signs
- Blood and/or urine tests to check hormone levels and to rule out hormone excess
- Results of genetic tests (rarely)
Your doctor also will need to know your family history of adrenal tumors, other kinds of tumors, syndromes that come with tumors, high blood pressure, or Cushing syndrome.
Adrenal incidentaloma treatment
About 85% of adrenal incidentalomas are non-functioning and may not need treatment. The treatment for a hormonally active (functional) adrenal tumor is surgery. Sometimes surgery is needed to remove the tumor, or one or both adrenal glands. Your medical team will decide whether you need surgery based on your type of tumor (benign or cancerous) and whether it is producing hormones. The treatment for a malignancy depends on the cell type, spread, and location of the primary tumor 3. Nonfunctional adrenal cortical adenomas are not premalignant, and surgical excision is not indicated. Some people may need hormone treatment. If you have an inherited tumor syndrome, you may need genetic counseling.
If you’ve had an adrenal incidentaloma, you may need regular follow-up, perhaps for several years.
Adrenal incidentaloma prognosis
Generally, adrenal incidentaloma prognosis is excellent, but it depends on the type of underlying adrenal disease.
Approximately 85% of AIs are nonfunctional (hormonally silent) and benign. The other 15% of AIs are either functional (hormonally active) or malignant and require further evaluation and treatment to avoid medical complications 4.
Patients with a previous history of cancer have a clinical course dictated by the primary tumor. Patients with adrenal cortical carcinomas have poor clinical outcomes, usually a 2- to 5-year 50% overall survival rate.
Approximately 3-7 percent of AIs prove to be pheochromocytomas 5. Pheochromocytomas may result in substantial complications, including death if not recognized. A 1981 series reported that less than one quarter of pheochromocytomas found post mortem were diagnosed ante mortem 6. More than 90% of these patients had characteristic symptoms suggesting the unrecognized tumors were not silent. Many of the patients died of causes possibly related to the pheochromocytoma. Approximately 29% died unexpectedly during surgery, 27% died from cardiovascular causes, and 17% died from cerebrovascular causes.
References- Terzolo M, Bovio S, Pia A, Reimondo G, Angeli A. Management of adrenal incidentaloma. Best Pract Res Clin Endocrinol Metab. 2009 Apr. 23(2):233-43.
- Adrenal incidentaloma. https://emedicine.medscape.com/article/116587-overview
- Yener S, Ertilav S, Secil M, et al. Prospective evaluation of tumor size and hormonal status in adrenal incidentalomas. J Endocrinol Invest. 2010 Jan. 33(1):32-6.
- Patrova J, Jarocka I, Wahrenberg H, Falhammar H. CLINICAL OUTCOMES IN ADRENAL INCIDENTALOMA: EXPERIENCE FROM ONE CENTER. Endocr Pract. 2015 Aug. 21 (8):870-7.
- Nieman LK. Approach to the patient with an adrenal incidentaloma. J Clin Endocrinol Metab. 2010 Sep. 95(9):4106-13.
- Sutton MG, Sheps SG, Lie JT. Prevalence of clinically unsuspected pheochromocytoma. Review of a 50-year autopsy series. Mayo Clin Proc. 1981 Jun. 56(6):354-60.