What is Angelman syndrome
Angelman syndrome is a rare genetic condition that primarily affects the central nervous system, causing physical and intellectual disability. Although Angelman syndrome can’t be cured, there are a range of therapies that can improve the quality of life of those affected. And the life expectancy of people with this condition appears to be nearly normal 1.
The prevalence of Angelman syndrome is one in 12,000-24,000 population 2.
Characteristic features of Angelman syndrome include:
- developmental delay,
- intellectual disability,
- severe speech impairment,
- problems with movement and balance (ataxia),
- epilepsy, and
- a small head size.
Individuals with Angelman syndrome typically have a happy, excitable demeanor with frequent smiling, laughter, and hand-flapping movements. Many of the characteristic features of Angelman syndrome result from the loss of function or faulty gene called UBE3A. When this gene is faulty or missing, nerve cells in the brain are unable to work properly, causing a range of physical and intellectual problems. Most cases of Angelman syndrome are not inherited that usually happens by chance, around the time of conception, although in rare cases a genetic change responsible for Angelman syndrome can be inherited from a parent 3.
Several different genetic mechanisms can inactivate or delete the maternal copy of the UBE3A gene. Most cases of Angelman syndrome (about 70 percent) occur when a segment of the maternal chromosome 15 containing this gene is deleted 1. In other cases (about 11 percent), Angelman syndrome is caused by a mutation in the maternal copy of the UBE3A gene 1.
In a small percentage of cases, Angelman syndrome results when a person inherits two copies of chromosome 15 from his or her father (paternal copies) instead of one copy from each parent. This phenomenon is called paternal uniparental disomy. Rarely, Angelman syndrome can also be caused by a chromosomal rearrangement called a translocation, or by a mutation or other defect in the region of DNA that controls activation of the UBE3A gene. These genetic changes can abnormally turn off (inactivate) UBE3A or other genes on the maternal copy of chromosome 15.
The causes of Angelman syndrome are unknown in 10 to 15 percent of affected individuals. Changes involving other genes or chromosomes may be responsible for the disorder in these cases.
In some people who have Angelman syndrome, the loss of a gene called OCA2 is associated with light-colored hair and fair skin. The OCA2 (Oculocutaneous Albinism Type 2) gene is located on the segment of chromosome 15 that is often deleted in people with this disorder. However, loss of the OCA2 (Oculocutaneous Albinism Type 2) gene does not cause the other signs and symptoms of Angelman syndrome. The protein produced from this gene helps determine the coloring (pigmentation) of the skin, hair, and eyes.
Most affected children also have recurrent seizures (epilepsy) and a small head size (microcephaly). Delayed development becomes noticeable by the age of 6 to 12 months, and other common signs and symptoms usually appear in early childhood.
Children with Angelman syndrome typically have a happy, excitable demeanor with frequent smiling, laughter, and hand-flapping movements. Hyperactivity, a short attention span, and a fascination with water are common. Most affected children also have difficulty sleeping and need less sleep than usual.
With age, people with Angelman syndrome become less excitable, and the sleeping problems tend to improve. However, affected individuals continue to have intellectual disability, severe speech impairment, and seizures throughout their lives. Adults with Angelman syndrome have distinctive facial features that may be described as “coarse.” Other common features include unusually fair skin with light-colored hair and an abnormal side-to-side curvature of the spine (scoliosis).
Treatment is aimed at addressing each individual’s symptoms and may include antiepileptics for seizures; physical, occupational, and speech therapy; and special education services 4.
Although there’s no cure for Angelman syndrome, early intervention services can improve outcomes for your child and treat his symptoms. Through these services, you can work with health professionals to support your child and help him reach his full potential.
The team of professionals involved in supporting you and your child might include physiotherapists, speech pathologists and occupational therapists, as well as paediatricians, who will look after your child’s overall health and development, and prescribe medication if your child needs it for epilepsy.
Together, you and your team can choose treatment and therapy options to best help your child.
Most babies with Angelman syndrome don’t show signs or symptoms at birth. The first signs of Angelman syndrome are usually developmental delays, such as lack of crawling or babbling, between 6 and 12 months.
If your child seems to have developmental delays or if your child has other signs or symptoms of Angelman syndrome, make an appointment with your child’s doctor.
Coping and support
Finding out that your child has Angelman syndrome can be overwhelming. You may not know what to expect. You may worry about your ability to care for your child’s medical concerns and developmental disabilities. There are resources that can help.
- Angelman Syndrome Foundation. https://www.angelman.org/
Work with a team
Find a team of doctors and therapists you trust to help you with important decisions about your child’s care and treatment. These professionals can also help you find local resources.
Consider a support group
Connecting with other families facing similar challenges may help you feel less alone. Ask your child’s doctor for information about local support groups and other helpful organizations.
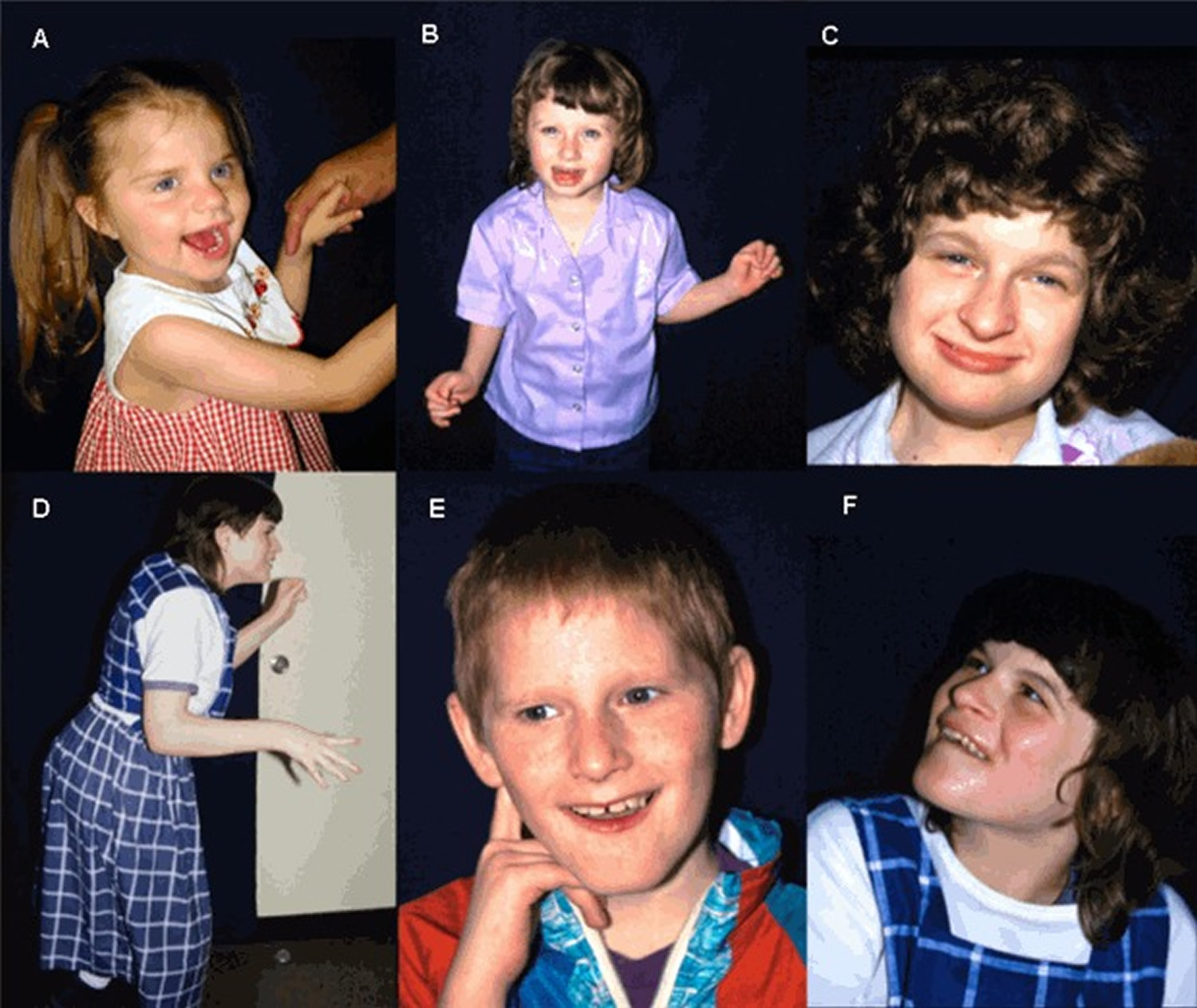
Figure 1. Angelman syndrome
Note: Individuals depicted have a genetically confirmed diagnosis of Angelman syndrome. Happy expression and an unstable gait accompanied by uplifted arms are commonly observed. At times, the facial appearance can suggest the diagnosis, but usually facial features are not distinctive.
[Source 4]Angelman syndrome complications
Complications associated with Angelman syndrome include:
- Feeding difficulties. Difficulty coordinating sucking and swallowing may cause feeding problems in infants. Your pediatrician may recommend a high-calorie formula to help your baby gain weight.
- Hyperactivity. Children with Angelman syndrome often move quickly from one activity to another, have a short attention span, and keep their hands or a toy in their mouths. Hyperactivity often decreases with age, and medication usually isn’t necessary.
- Sleep disorders. People with Angelman syndrome often have abnormal sleep-wake patterns and need less sleep than most people. Sleep difficulties may improve with age. Medication and behavior therapy may help control sleep disorders.
- Curving of the spine (scoliosis). Some people with Angelman syndrome develop an abnormal side-to-side spinal curvature over time.
- Obesity. Older children with Angelman syndrome tend to have large appetites, which may lead to obesity.
Angelman syndrome clinical description
Prenatal history, birth weight, and head circumference at birth are usually normal. Young infants with Angelman syndrome may have difficulties with breast feeding or bottle feeding (as a result of sucking difficulties) and muscular hypotonia. Gastroesophageal reflux may occur.
Some infants have an apparent happy affect with excessive chortling or paroxysms of laughter. 50% of children develop microcephaly by age 12 months. Strabismus may also occur. Tremulous movements may be noted prior to age 12 months, associated with increased deep-tendon reflexes.
Angelman syndrome may first be suspected in a toddler because of delayed gross motor milestones, muscular hypotonia, and/or speech delay 5.
Seizures typically occur between ages one and three years and can be associated with generalized, somewhat specific EEG changes: runs of high-amplitude delta activity with intermittent spike and slow-wave discharges (at times observed as a notched delta pattern); runs of rhythmic theta activity over a wide area; and runs of rhythmic sharp theta activity of 5-6/s over the posterior third of the head, forming complexes with small spikes. These are usually facilitated by or seen only with eye closure 6.
Seizure types can be quite varied and include both major motor and minor motor types (e.g., petit mal, atonic) 7. Infantile spasms are rare. Non-convulsive status epilepticus may occur 8. Brain MRI may show mild atrophy and mild dysmyelination, but no structural lesions 9.
The average child with Angelman syndrome walks between ages 2.5 and six years 10 and at that time may have a jerky, robot-like, stiff gait, with uplifted, flexed, and pronated forearms, hypermotoric activity, excessive laughter, protruding tongue, drooling, absent speech, and social-seeking behavior. 10% of children are nonambulatory.
Sleep problems are well known in individuals with Angelman syndrome; frequent awakening at night is common 11. Dyssomnias (difficulties in initiating or maintaining sleep), irregular sleep-wake cycles, disruptive night behaviors such as periods of laughter, and sleep-related seizures have been reported 12.
Essentially all young children with Angelman syndrome have some component of hyperactivity; males and females appear equally affected. Infants and toddlers may have seemingly ceaseless activity, constantly keeping their hands or toys in their mouth, and/or moving from object to object. Some behaviors may suggest an autism spectrum problem but social engagement is typically good and stereotypic behaviors such as lining up of toys or fascination with spinning objects or flashing lights rarely occur 13.
Language impairment is severe. Appropriate use of even one or two words in a consistent manner is rare. Receptive language skills are always more advanced than expressive language skills 14. Most older children and adults with Angelman syndrome are able to communicate by pointing and using gestures and by using communication boards. Effective fluent use of sign language does not occur 15. Relatively higher language skills can be seen in those with mosaic imprinting defects.
Pubertal onset and development are generally normal in Angelman syndrome. Fertility appears to be normal; procreation appears possible for both males and females. Lossie & Driscoll 16 reported transmission of an Angelman syndrome deletion to a fetus by the affected mother.
Young adults appear to have generally good physical health, although seizures continue to be present throughout adulthood. Constipation is common. Many are treated for gastroesophageal reflux symptoms. Scoliosis becomes more common with advancing age 17.
Independent living is not possible for adults with Angelman syndrome; many live at home or in home-like placements.
Life span data are not available, but life span appears to be nearly normal.
Genotype-Phenotype Correlations
All genetic mechanisms that give rise to Angelman syndrome lead to a somewhat uniform clinical picture of severe-to-profound intellectual disability, movement disorder, characteristic behaviors, and severe limitations in speech and language. However, some clinical differences correlate with genotype 18. These correlations are broadly summarized below:
- The 5- to 7-Mb deletion class results in the most severe phenotype with microcephaly, seizures, motor difficulties (e.g., ataxia, muscular hypotonia, feeding difficulties), and language impairment. They also have lower body mass index compared to individuals with uniparental disomy or imprinting defects 19. There is some suggestion that individuals with larger deletions (e.g., BP1-BP3 [class I; ISCA-37404] break points) may have more language impairment or autistic traits than those with BP2-BP3 (class II; ISCA-37478) break points 20.
- Individuals with uniparental disomy have better physical growth (e.g., less likelihood of microcephaly), fewer movement abnormalities, less ataxia, and a lower prevalence (but not absence) of seizures than do those with other underlying molecular mechanisms 18.
- Individuals with imprinting defects or uniparental disomy have higher developmental and language ability than those with other underlying molecular mechanisms. Individuals who are mosaic for the nondeletion imprinting defect (approximately 20% of the imprinting defect group) have the most advanced speech abilities 21; they may speak up to 50-60 words and use simple sentences.
- Individuals with chromosome deletions encompassing OCA2 (Oculocutaneous Albinism Type 2) frequently have hypopigmented irides, skin, and hair. OCA2 (Oculocutaneous Albinism Type 2) encodes a protein important in tyrosine metabolism that is associated with the development of pigment in the skin, hair, and irides (see Oculocutaneous Albinism Type 2). However, other factors in addition to haploinsufficiency of OCA2 (Oculocutaneous Albinism Type 2) appear to account for the relative hypopigmentation in individuals with Angelman syndrome, as UBE3A has now been shown to modulate melanocortin 1 receptor (MC1R) activity in somatic tissues 22.
Uniparental disomy is a situation in which both members of a chromosome pair or segments of a chromosome pair are inherited from one parent and neither is inherited from the other parent; uniparental disomy can result in an abnormal phenotype in some instances.
Imprinting defect is the process by which maternally and paternally derived chromosomes are uniquely chemically modified (usually by methylation), leading to different expression of a certain gene or genes on those chromosomes depending on their parental origin. Patterns of gene expression and repression vary between imprinted regions.
Imprinting center is the process by which maternally and paternally derived chromosomes are uniquely chemically modified (usually by methylation), leading to different expression of a certain gene or genes on those chromosomes depending on their parental origin. Patterns of gene expression and repression vary between imprinted regions.
Proband is index case or the affected individual through whom a family with a genetic disorder is ascertained; may or may not be the individual presenting for genetic counseling.
Angelman syndrome causes
Angelman syndrome is a genetic disorder. It’s usually caused by problems with a gene located on chromosome 15 called the ubiquitin protein ligase E3A (UBE3A) gene.
A missing or defective gene
You receive your pairs of genes from your parents — one copy from your mother (maternal copy) and the other from your father (paternal copy).
Your cells typically use information from both copies, but in a small number of genes, only one copy is active.
Normally, only the maternal copy of the UBE3A gene is active in the brain. Most cases of Angelman syndrome occur when part of the maternal copy is missing or damaged.
In a few cases, Angelman syndrome is caused when two paternal copies of the gene are inherited, instead of one from each parent.
Risk factors for Angelman syndrome
Angelman syndrome is rare. Researchers usually don’t know what causes the genetic changes that result in Angelman syndrome. Most people with Angelman syndrome don’t have a family history of the disease.
Occasionally, Angelman syndrome may be inherited from a parent. A family history of the disease may increase a baby’s risk of developing Angelman syndrome.
Angelman syndrome prevention
In rare cases, Angelman syndrome may be passed from an affected parent to a child through defective genes. If you’re concerned about a family history of Angelman syndrome or if you already have a child with Angelman syndrome, consider talking to your doctor or a genetic counselor for help planning future pregnancies.
Angelman syndrome signs and symptoms
Parents often notice their child isn’t developing properly at the age of 6 to 12 months. But it can take a while to pin down the source of the problems.
People with Angelman syndrome often:
- laugh and smile for no apparent reason
- speak very little, or not at all
- have severe intellectual disability and delayed development
- have problems with balance and movement, such as difficulty sitting up without support, walking with stiff legs and making jerky arm movements
- are restless and excitable
- need less sleep than most people, especially as children.
Some people with Angelman syndrome have:
- seizures
- a small head, which is flat at the back
- certain facial features, such as widely spaced teeth and eyes that look in different directions.
Diagnosing Angelman syndrome
A paediatrician would examine the child and his or her behavior. A blood sample would also be taken for genetic testing.
If testing is able to show the genetic cause of the syndrome, parents can find out if it is likely to happen again with any future children they may have.
Consensus criteria for the clinical diagnosis of Angelman syndrome have been developed in conjunction with the Scientific Advisory Committee of the US Angelman Syndrome Foundation 5.
The diagnosis of Angelman syndrome may be suggested by the following clinical and/or laboratory findings.
Clinical Findings of Angelman syndrome
Newborns typically have a normal phenotype. Developmental delays are first noted at around age six months. However, the unique clinical features of AS do not become manifest until after age one year, and it can take several years before the correct clinical diagnosis is obvious.
Findings typically present in affected individuals 5
- Normal prenatal and birth history, normal head circumference at birth, no major birth defects
- Normal metabolic, hematologic, and chemical laboratory profiles
- Structurally normal brain by MRI or CT, although mild cortical atrophy or dysmyelination may be observed
- Delayed attainment of developmental milestones without loss of skills
- Evidence of developmental delay by age six to 12 months, eventually classified as severe
- Speech impairment, with minimal to no use of words; receptive language skills and nonverbal communication skills higher than expressive language skills
- Movement or balance disorder, usually ataxia of gait and/or tremulous movement of the limbs
- Behavioral uniqueness, including any combination of frequent laughter/smiling; apparent happy demeanor; excitability, often with hand-flapping movements and hypermotoric behavior
Findings in more than 80% of affected individuals
- Delayed or disproportionately slow growth in head circumference, usually resulting in absolute or relative microcephaly by age two years
- Seizures, usually starting before age three years
- Abnormal EEG, with a characteristic pattern of large-amplitude slow-spike waves
Findings in fewer than 80% of affected individuals
- Flat occiput
- Occipital groove
- Protruding tongue
- Tongue thrusting; suck/swallowing disorders
- Feeding problems and/or muscle hypotonia during infancy
- Prognathia
- Wide mouth, widely spaced teeth
- Frequent drooling
- Excessive chewing/mouthing behaviors
- Strabismus
- Hypopigmented skin, light hair and eye color (compared to family); seen only in those with a deletion
- Hyperactive lower-extremity deep-tendon reflexes
- Uplifted, flexed arm position especially during ambulation
- Wide-based gait with pronated or valgus-positioned ankles
- Increased sensitivity to heat
- Abnormal sleep-wake cycles and diminished need for sleep
- Attraction to/fascination with water; fascination with crinkly items such as certain papers and plastics
- Abnormal food-related behaviors
- Obesity (in the older child; more common in those who do not have a deletion)
- Scoliosis
- Constipation
Laboratory Findings
A combination of genetic tests can reveal the chromosome defects related to Angelman syndrome. These tests may review:
- Parental DNA pattern. This test, known as a DNA methylation test, screens for three of the four known genetic abnormalities that cause Angelman syndrome.
- Missing chromosomes. Either a fluorescence in situ hybridization (FISH) test or a comparative genomic hybridization test (CGH) can show if portions of chromosomes are missing.
- Gene mutation. Rarely, Angelman syndrome may occur when a person’s maternal copy of the UBE3A gene is active, but mutated. If results from a DNA methylation test are normal, your child’s doctor may order a UBE3A gene sequencing test to look for a maternal mutation.
Abnormality of 15q11.2-q13 detected by chromosomal microarray (CMA) or by karyotype performed for nonspecific clinical findings is suggestive of Angelman syndrome.
Establishing the Diagnosis
The diagnosis of Angelman syndrome is established in a proband who meets the consensus clinical diagnostic criteria and/or who has findings on molecular genetic testing that suggest deficient expression or function of the maternally inherited UBE3A allele through one of the following mechanisms:
- Abnormal methylation at 15q11.2-q13 due to one of the following:
- Deletion of the maternally inherited 15q11.2-q13 locus (which includes UBE3A)
- Uniparental disomy of the paternal chromosome 15
- An imprinting defect of the maternal chromosome 15q11.2-q13 locus
- A pathogenic variant in the maternally derived UBE3A
Molecular genetic testing approaches to establish the diagnosis can be based on either the clinical findings or the laboratory findings that suggested the diagnosis of Angelman syndrome.
Based on clinical findings in a symptomatic individual who has not had any prior molecular genetic testing:
- DNA methylation analysis is typically the first test ordered. Individuals with Angelman syndrome caused by a 5- to 7-Mb deletion of 15q11.2-q13, uniparental disomy (UPD), or an imprinting defect (ID) have only an unmethylated (i.e., “paternal”) contribution (i.e., an abnormal parent-specific DNA methylation imprint). DNA methylation analysis identifies approximately 80% of individuals with Angelman syndrome.
Note: Most commercially available DNA methylation analysis tests cannot distinguish between AS resulting from a deletion, UPD, or an ID. Further testing is required to identify the underlying molecular mechanism. - If DNA methylation analysis is normal:
- Testing of UBE3A may be considered. Sequence analysis is performed first. If a pathogenic variant is not identified, gene-targeted deletion/duplication analysis can be considered.
- Use of a multigene panel that includes UBE3A and other genes of interest (see Differential Diagnosis) may be considered in individuals who have features of AS and normal DNA methylation analysis. Note: The genes included and sensitivity of multigene panels vary by laboratory and over time.
- More comprehensive genomic testing (when available) including exome sequencing, genome sequencing, and mitochondrial sequencing may be considered if testing of UBE3A (and/or use of a multigene panel) fails to confirm a diagnosis in an individual with features of Angelman syndrome.
Based on laboratory findings in an individual who has been found to have a deletion of 15q11.2-q13 through chromosomal microarray (CMA), fluorescent in situ hybridization (FISH), or karyotype*, perform DNA methylation analysis to determine if the deletion is on the maternally derived chromosome 15.
*Fewer than 1% of individuals with Angelman syndrome have a cytogenetically visible chromosome rearrangement (i.e., translocation or inversion) of one number 15 chromosome involving 15q11.2-q13.
Possible explanations for the failure to detect Angelman syndrome-causing genetic abnormalities in the 11% or more of individuals with clinically diagnosed Angelman syndrome:
- Incorrect clinical diagnosis
- Undetected pathogenic variants in the regulatory region(s) of UBE3A
- Other unidentified mechanisms or gene(s) involved in UBE3A function.
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with Angelman syndrome, the following evaluations focused on neurologic assessment and good preventive practice are recommended:
- Baseline brain MRI and EEG. Note: Typically, management of seizures (or assessment of risk for seizures) is not significantly helped by repetitive EEG or MRI testing.
- Musculoskeletal examination for scoliosis and gait impairment (e.g., extent of foot pronation or ankle subluxation; tight Achilles tendons) and the extent of muscular hypotonia; orthopedic referral as needed
- Ophthalmology examination for strabismus, evidence of ocular albinism (in deletion-positive AS), and visual acuity
- Developmental evaluation focused on: (1) nonverbal language ability and related educational and teaching strategies; and (2) physical therapy to enable optimal ambulation
- Evaluation for gastroesophageal reflux in infants and young children; dietary evaluation to assure optimal nutritional status
- Consultation with a clinical geneticist and/or genetic counselor
Angelman syndrome treatment
There’s no cure for Angelman syndrome. Research is focusing on targeting specific genes for treatment. Current treatment focuses on managing the medical and developmental issues.
A team of health care professionals will likely work with you to manage your child’s condition. Depending on your child’s signs and symptoms, treatment for Angelman syndrome may involve:
- Anti-seizure medication to control seizures
- Physical therapy to help with walking and movement problems
- Communication therapy, which may include sign language and picture communication
- Behavior therapy to help overcome hyperactivity and a short attention span and to aid in development
Feeding problems in newborns may require special nipples and other strategies to manage weak or uncoordinated sucking.
Gastroesophageal reflux can be associated with poor weight gain and emesis; the customary medical treatment (i.e., upright positioning, motility drugs) is usually effective; sometimes fundoplication as required.
Many antiepileptic drugs have been used to treat seizures in individuals with Angelman syndrome; no one drug has proven superior. Medications used for minor motor seizures (e.g., valproic acid, clonazepam, topiramate, lamotrigine, ethosuximide) are more commonly prescribed than medications for major motor seizures (e.g., diphenylhydantoin, phenobarbital) 23. Carbamezapine, although not contraindicated, is less frequently used than other common anticonvulsants. Single medication use is preferred, but seizure breakthrough is common. A few individuals with Angelman syndrome have infrequent seizures and are not on antiepileptic drugs. Some with uncontrollable seizures have benefited from a ketogenic or low glycemic diet 24.
Hypermotoric behaviors are typically resistant to behavioral therapies; accommodation by the family and provision of a safe environment are important.
Most children with Angelman syndrome do not receive drug therapy for hyperactivity, although some may benefit from the use of stimulant medications such as methylphenidate (Ritalin®).
Behavioral modification is effective in treating undesirable behaviors that are socially disruptive or self-injurious.
A full range of educational training and enrichment programs should be available.
Unstable or nonambulatory children may benefit from physical therapy. Occupational therapy may help improve fine motor and oral-motor control. Special adaptive chairs or positioners may be required, especially for extremely ataxic children.
Speech therapy is essential and should focus on nonverbal methods of communication. Augmentative communication aids such as picture cards or communication boards should be used at the earliest appropriate time. Attempts to teach signing should begin as soon as the child is sufficiently attentive.
Individualization and flexibility in the school are important educational strategies.
Special physical provisions in the classroom, along with teacher aides or assistants, may be needed for effective class integration. Children with Angelman syndrome with excessive hypermotoric behaviors need an accommodating classroom space.
Many families construct safe but confining bedrooms to accommodate disruptive nighttime wakefulness. Administration of 0.3 mg melatonin one hour before sleep may be helpful in some, but should not be given in the middle of the night if the child awakens.
Strabismus may require surgical correction.
Constipation often requires regular use of laxatives such as high fiber or lubricating agents.
Orthopedic problems, particularly subluxed or pronated ankles or tight Achilles tendons, can be corrected by orthotic bracing or surgery.
Thoraco-lumbar jackets may be needed for scoliosis, and individuals with severe curvature may benefit from surgical rod stabilization.
Excessive tongue protrusion causes drooling; available surgical or medication treatments (e.g., surgical reimplantation of the salivary ducts or use of local scopolamine patches) are generally not effective.
Prevention of Secondary Complications
Children with Angelman syndrome are at risk for medication overtreatment because their movement abnormalities can be mistaken for seizures and because EEG abnormalities can persist even when seizures are controlled.
The behavioral phenotype of Angelman syndrome includes hyperexcitability, hypermotoric behaviors, and deficits in social communication. These limitations place them at risk for social disruptions. On occasion, the use of risperidone (Risperdal®) or other atypical antipsychotic drugs provides some but often limited benefit. When such drugs are needed, care must be taken to avoid over-sedation and other side effects.
Older adults tend to become less mobile and less active; attention to activity schedules may be helpful in reducing the extent of scoliosis and obesity.
Surveillance
The following are appropriate:
- Annual clinical examination for scoliosis
- For older children, evaluation for the development of obesity associated with excessive appetite and decreased physical activity
Agents/Circumstances to Avoid
Carbamezapine, although not contraindicated, is less frequently used than other common anticonvulsants.
Vigabatrin and tigabine (anticonvulsants that increase brain GABA levels) are contraindicated in individuals with Angelman syndrome. For unknown reasons, carbamazapine, vigabatrine, and tigabine can cause development of other seizure types or non-convulsive status epilepticus. This paradoxic seizure development is not limited to individuals with Angelman syndrome 8.
Therapies Under Investigation
Clinical trials involving oral administration of folate, vitamin B12, creatine, and betaine have been undertaken in an attempt to augment DNA methylation pathways and possibly increase expression of the paternal UBE3A allele in the central nervous system; however, the initial trial did not demonstrate significant clinical benefit 25. More recent therapeutic efforts have focused on activating the otherwise silenced paternal UBE3A allele by use of telomerase inhibitors 26 and antisense oligonucleotides 27.
Living with Angelman syndrome
People with Angelman syndrome have a near-normal life expectancy, but need life-long care to help them achieve the best possible quality of life. Ideally, this care is provided by a team of health professionals.
Some treatments and therapies that may help include:
- medications, such as anti-epilepsy drugs
- physical supports, such as back or leg braces
- therapy to improve posture, balance and movement
- therapy to develop communication skills
- therapy to help behavioral problems such as hyperactivity.
Family planning
- The optimal time for determination of genetic risk and discussion of the availability of prenatal testing is before pregnancy.
- It is appropriate to offer genetic counseling (including discussion of potential risks to offspring and reproductive options) to young adults who are at risk of having children with Angelman syndrome.
DNA banking is the storage of DNA (typically extracted from white blood cells) for possible future use. Because it is likely that testing methodology and our understanding of genes, allelic variants, and diseases will improve in the future, consideration should be given to banking DNA of affected individuals.
Prenatal Testing and Preimplantation Genetic Diagnosis
Prenatal diagnosis and preimplantation genetic diagnosis for high-risk pregnancies require prior identification of the disease-causing mechanism in the family.
High risk. Prenatal detection of all the known molecular genetic alterations (i.e., molecular classes Ia, Ib, IIa, IIb, IIIa, IIIb, IV; see Table 2) in the 15q11.2-q13 region that give rise to Angelman syndrome is possible through DNA and/or chromosome/FISH analysis of fetal cells obtained by chorionic villus sampling (usually performed at ~10-12 weeks’ gestation) or amniocentesis (usually performed at ~15-18 weeks’ gestation) 28.
DNA methylation analysis (for 5- to 7-Mb deletions, uniparental disomy, and imprinting center defects) on cells obtained by chorionic villus sampling (CVS) is theoretically possible 29. However, the few clinical laboratories doing prenatal testing using DNA methylation analysis prefer using amniocytes because of the relative hypomethylation of cells derived from the placenta. FISH analysis, IC deletion analysis, and sequence analysis of UBE3A should be technically possible for chorionic villus sampling.
Prenatal testing should be undertaken only after the genetic mechanism in the index case has been established and the couple has been counseled regarding the risk to their unborn child, as the risks and the type of molecular genetic testing used vary according to the type of molecular defect in the proband.
- Parents with normal chromosomes who have had one child with Angelman syndrome caused by either deletion or uniparental disomy, have a low recurrence risk but may be offered prenatal testing for reassurance.
- Parents who have had one child with Angelman syndrome caused by a UBE3A pathogenic variant should be offered prenatal testing even if the mother does not have a UBE3A pathogenic variant because of the possibility of germline mosaicism.
- Prenatal testing for an inherited translocation involving chromosome 15 is relevant because of the increased recurrence risk. FISH analysis and parent-of-origin (DNA methylation and/or polymorphism) studies should be considered if an inherited translocation involving chromosome 15 is present.
Note: Gestational age is expressed as menstrual weeks calculated either from the first day of the last normal menstrual period or by ultrasound measurements.
Low risk. For low-risk pregnancies with no family history of Angelman syndrome, Angelman syndrome needs to be considered in the following instances:
- If a 15q11.2-q13 deletion is suspected on cytogenetic studies from chorionic villus sampling (CVS) or amniocentesis, FISH analysis or chromosomal microarray analysis (CMA) is indicated to confirm the deletion. If the deletion is confirmed, parent-of-origin studies 29 can be performed to determine if the deletion is maternally derived (fetus has Angelman syndrome) or paternally derived (fetus has Prader-Willi syndrome).
- If trisomy 15 or mosaic trisomy 15 is detected on chorionic villus sampling, and if subsequent amniocentesis reveals 46 chromosomes, the possibility of trisomy rescue leading to Angelman syndrome (paternal uniparental disomy) or Prader-Willi syndrome (maternal uniparental disomy) through the loss of a parental chromosome 15 must be considered. In this instance, parent-of-origin (DNA) studies on amniocytes can be performed.
- If a de novo translocation involving chromosome 15 or a supernumerary chromosome 15 marker is detected, FISH analysis or CMA and parent-of-origin studies should be considered to evaluate for a possible deletion (of variable size) or uniparental disomy.
Preimplantation genetic diagnosis may be an option for families in which the underlying mechanism has been identified in the proband to be UBE3A pathogenic variants or imprinting center deletions. (The relative hypomethylation of the early embryo makes preimplantation genetic diagnosis problematic for DNA methylation testing.)
Other
Assisted reproductive technology (ART). In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) have been demonstrated to increase the chance of certain imprinting disorders, like Beckwith-Wiedemann syndrome, in offspring. However, recent studies demonstrate that there is no significant association between Angelman syndrome and IVF or ICSI 30.
Fertility. Research from the Netherlands and Germany demonstrate an association between fertility issues and incidence of Angelman syndrome. The percent of couples who experienced fertility issues before having a child with Angelman syndrome ranged from 19% to 25%. There was no positive association with fertility issues and Angelman syndrome in families queried in the United Kingdom 30.
References- Angelman syndrome. https://ghr.nlm.nih.gov/condition/angelman-syndrome
- Mertz LG, Christensen R, Vogel I, Hertz JM, Nielsen KB, Gronskov K, Ostergaard JR. Angelman syndrome in Denmark. birth incidence, genetic findings, and age at diagnosis. Am J Med Genet A. 2013;161A:2197–203. https://www.ncbi.nlm.nih.gov/pubmed/23913711
- Angelman syndrome. Genetics Home Reference. https://ghr.nlm.nih.gov/condition/angelman-syndrome
- Dagli AI, Mueller J, Williams CA. Angelman Syndrome. 1998 Sep 15 [Updated 2017 Dec 21]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1144/
- Williams, C. A., Beaudet, A. L., Clayton-Smith, J., Knoll, J. H., Kyllerman, M., Laan, L. A., Magenis, R. E., Moncla, A., Schinzel, A. A., Summers, J. A. and Wagstaff, J. (2006), Angelman syndrome 2005: Updated consensus for diagnostic criteria. Am. J. Med. Genet., 140A: 413–418. doi:10.1002/ajmg.a.31074 http://onlinelibrary.wiley.com/doi/10.1002/ajmg.a.31074/full
- Korff CM, Kelley KR, Nordli DR Jr. Notched delta, phenotype, and Angelman syndrome. J Clin Neurophysiol. 2005;22:238–43. https://www.ncbi.nlm.nih.gov/pubmed/16093895
- Fiumara A, Pittalà A, Cocuzza M, Sorge G. Epilepsy in patients with Angelman syndrome. Ital J Pediatr. 2010;36:31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2865483
- Pelc K, Boyd SG, Cheron G, Dan B. Epilepsy in Angelman syndrome. Seizure. 2008a;17:211–7. https://www.ncbi.nlm.nih.gov/pubmed/17904873
- Castro-Gago M, Gómez-Lado C, Eirís-Puñal J, Rodríguez-Mugico VM. Abnormal myelination in Angelman syndrome. Eur J Paediatr Neurol. 2010;14:292. http://www.ejpn-journal.com/article/S1090-3798(09)00151-2/fulltext
- Lossie AC, Whitney MM, Amidon D, Dong HJ, Chen P, Theriaque D, Hutson A, Nicholls RD, Zori RT, Williams CA, Driscoll DJ. Distinct phenotypes distinguish the molecular classes of Angelman syndrome. J Med Genet. 2001;38:834–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1734773
- Bruni O, Ferri R, D’Agostino G, Miano S, Roccella M, Elia M. Sleep disturbances in Angelman syndrome: a questionnaire study. Brain Dev. 2004;26:233–40. https://www.ncbi.nlm.nih.gov/pubmed/15130689
- Pelc K, Cheron G, Boyd SG, Dan B. Are there distinctive sleep problems in Angelman syndrome? Sleep Med. 2008b;9:434–41. https://www.ncbi.nlm.nih.gov/pubmed/17765640
- Walz NC. Parent report of stereotyped behaviors, social interaction, and developmental disturbances in individuals with Angelman syndrome. J Autism Dev Disord. 2007;37:940–7. https://www.ncbi.nlm.nih.gov/pubmed/17019625
- Gentile JK, Tan WH, Horowitz LT, Bacino CA, Skinner SA, Barbieri-Welge R, Bauer-Carlin A, Beaudet AL, Bichell TJ, Lee HS, Sahoo T, Waisbren SE, Bird LM, Peters SU. A neurodevelopmental survey of Angelman syndrome with genotype-phenotype correlations. J Dev Behav Pediatr. 2010;31:592–601. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2997715/
- Clayton-Smith J. Clinical research on Angelman syndrome in the United Kingdom: observations on 82 affected individuals. Am J Med Genet. 1993;46:12–15. https://www.ncbi.nlm.nih.gov/pubmed/7684188
- Lossie AC, Driscoll DJ. Transmission of Angelman syndrome by an affected mother. Genet Med. 1999;1:262–6. https://www.nature.com/articles/gim1999181.pdf
- Giroud M, Daubail B, Khayat N, Chouchane M, Berger E, Muzard E, Medeiros de Bustos E, Thauvin-Robinet C, Faivre L, Masurel A, Darmency-Stamboul V, Huet F, Bejot Y, Giroud M, Moulin T. Angelman syndrome: a case series assessing neurological issues in adulthood. Eur Neurol. 2015;73:119–25. https://www.karger.com/Article/Abstract/369454
- Valente KD, Varela MC, Koiffmann CP, Andrade JQ, Grossmann R, Kok F, Marques-Dias MJ. Angelman syndrome caused by deletion: a genotype-phenotype correlation determined by breakpoint. Epilepsy Res. 2013;105:234–9. https://www.ncbi.nlm.nih.gov/pubmed/23352739
- Tan WH, Bacino CA, Skinner SA, Anselm I, Barbieri-Welge R, Bauer-Carlin A, Beaudet AL, Bichell TJ, Gentile JK, Glaze DG, Horowitz LT, Kothare SV, Lee HS, Nespeca MP, Peters SU, Sahoo T, Sarco D, Waisbren SE, Bird LM. Angelman syndrome: Mutations influence features in early childhood. Am J Med Genet A. 2011;155A:81–90. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3563320/
- Sahoo T, Peters SU, Madduri NS, Glaze DG, German JR, Bird LM, Barbieri-Welge R, Bichell TJ, Beaudet AL, Bacino CA. Microarray based comparative genomic hybridization testing in deletion bearing patients with Angelman syndrome: genotype-phenotype correlations. J Med Genet. 2006;43:512–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2564536/
- Nazlican H, Zeschnigk M, Claussen U, Michel S, Boehringer S, Gillessen-Kaesbach G, Buiting K, Horsthemke B. Somatic mosaicism in patients with Angelman syndrome and an imprinting defect. Hum Mol Genet. 2004;13:2547–55. https://www.ncbi.nlm.nih.gov/pubmed/15385437
- Low D, Chen KS. UBE3A regulates MC1R expression: a link to hypopigmentation in Angelman syndrome. Pigment Cell Melanoma Res. 2011;24:944–52. https://www.ncbi.nlm.nih.gov/pubmed/21733131
- Thibert RL, Conant KD, Braun EK, Bruno P, Said RR, Nespeca MP, Thiele EA. Epilepsy in Angelman syndrome: a questionnaire-based assessment of the natural history and current treatment options. Epilepsia. 2009;50:2369–76. https://www.ncbi.nlm.nih.gov/pubmed/19453717
- Thibert RL, Pfeifer HH, Larson AM, Raby AR, Reynolds AA, Morgan AK, Thiele EA. Low glycemic index treatment for seizures in Angelman syndrome. Epilepsia. 2012;53:1498–502. https://www.ncbi.nlm.nih.gov/pubmed/22779920
- Peters SU, Bird LM, Kimonis V, Glaze DG, Shinawi LM, Bichell TJ, Barbieri-Welge R, Nespeca M, Anselm I, Waisbren S, Sanborn E, Sun Q, O’Brien WE, Beaudet AL, Bacino CA. Double-blind therapeutic trial in Angelman syndrome using betaine and folic acid. Am J Med Genet A. 2010;152A:1994–2001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3172130/
- Huang HS, Allen JA, Mabb AM, King IF, Miriyala J, Taylor-Blake B, Sciaky N, Dutton JW Jr, Lee HM, Chen X, Jin J, Bridges AS, Zylka MJ, Roth BL, Philpot BD. Topoisomerase inhibitors unsilence the dormant allele of Ube3a in neurons. Nature. 2011;481:185–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257422/
- Meng L, Ward AJ, Chun S, Bennett CF, Beaudet AL, Rigo F. Towards a therapy for Angelman syndrome by targeting a long non-coding RNA. Nature. 2015;518:409–12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4351819
- Chang CW, Hsu HK, Kao CC, Huang JY, Kuo PL. Prenatal diagnosis of Prader-Willi syndrome and Angelman syndrome for fetuses with suspicious deletion of chromosomal region 15q11-q13. Int J Gynaecol Obstet. 2014;125:18–21. https://www.ncbi.nlm.nih.gov/pubmed/24434231
- Glenn CC, Deng G, Michaelis RC, Tarleton J, Phelan MC, Surh L, Yang TP, Driscoll DJ. DNA methylation analysis with respect to prenatal diagnosis of the Angelman and Prader-Willi syndromes and imprinting. Prenat Diagn. 2000;20:300–6. https://www.ncbi.nlm.nih.gov/pubmed/10740202
- Vermeiden JP, Bernardus RE. Are imprinting disorders more prevalent after human in vitro fertilization or intracytoplasmic sperm injection? Fertil Steril. 2013;99:642–51. https://www.ncbi.nlm.nih.gov/pubmed/23714438