What is athetosis
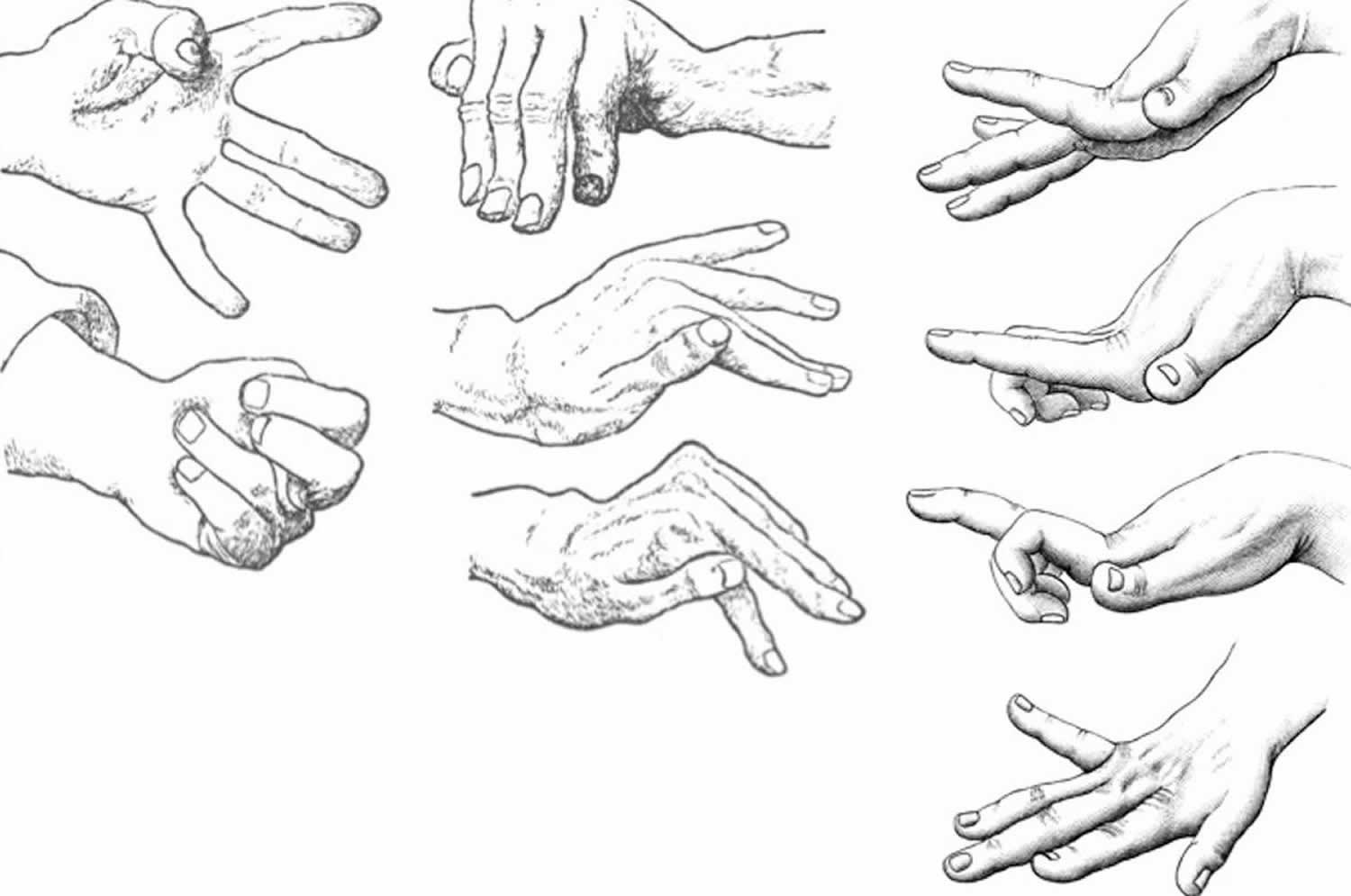
Athetosis is slow, smooth, nonrhythmic, involuntary writhing, sinuous movements of the hands and feet, often alternating with postures of the proximal limbs 1. The term athetosis, comes from a Greek word meaning “without fixed position” or “changing”, is a movement disorder first described by Hammond in 1871 2. In 1983, Foley defined the athetoid syndrome as “a nonprogressive but evolving disorder due to damage to the basal ganglia of the full-term brain … [with] impairment of postural reflexes, arrhythmical involuntary movements, and dysarthria, [but] sparing … sensation, ocular movements and … intelligence” 3. A decade later, “athetoid syndrome” was replaced by “dyskinetic cerebral palsy.” Injury to basal ganglia by various mechanisms, including asphyxia, trauma, perinatal strokes, and kernicterus, is known to cause birth-related athetosis. Athetosis is characterized by the inability to maintain a single position in the fingers and toes, tongue or any other part of the body where no muscle group is respected and movements are slower than in chorea, and with distal predominance 4. This seems to be related to a failure of the striatum to suppress the activity of unwanted muscle groups 5.
Athetosis vs Chorea
Athetosis is also known as slow chorea. Chorea is rapid, nonrhythmic, jerky, dance-like involuntary movement of the body, mostly of the distal muscles and face; movements may be incorporated into semipurposeful acts that mask the involuntary movements.
Chorea is an abnormal involuntary movement disorder, one of a group of neurological disorders called dyskinesias, which are caused by overactivity of the neurotransmitter dopamine in the areas of the brain that control movement. Chorea is characterized by brief, irregular contractions that are not repetitive or rhythmic, but appear to flow from one muscle to the next. Chorea often occurs with athetosis, which adds twisting and writhing movements. Chorea is a primary feature of Huntington’s disease, a progressive, hereditary movement disorder that appears in adults, but it may also occur in a variety of other conditions. Sydenham’s chorea occurs in a small percentage (20 percent) of children and adolescents as a complication of rheumatic fever. Chorea can also be induced by drugs (levodopa, anti-convulsants, and anti-psychotics) metabolic and endocrine disorders, and vascular incidents.
Chorea and athetosis are defined by clinical manifestations; many experts believe that when they occur together (as choreoathetosis), athetosis is a dystonia superimposed on chorea. Chorea and athetosis result from impaired inhibition of thalamocortical neurons by the basal ganglia. Excess dopaminergic activity may be the mechanism.
There is no standard course of treatment for chorea. Treatment depends on the type of chorea and the associated disease. Treatment for Huntington’s disease is supportive, while treatment for Sydenham’s chorea usually involves antibiotic drugs to treat the infection, followed by drug therapy to prevent recurrence. Adjusting medication dosages can treat drug-induced chorea. Metabolic and endocrine-related choreas are treated according to the cause(s) of symptoms.
Athetosis vs Dystonia
Dystonia is a slow involuntary movement or extended spasm in a group of muscles. Dystonia causes involuntary contractions of your muscles such as those in the arms, legs, or neck; or the entire body. These contractions result in twisting and repetitive movements. Sometimes they are painful. Early symptoms may include deterioration in handwriting, foot cramps, or a dragging foot after running or walking some distance. Other possible symptoms are tremor and voice or speech difficulties. Dystonia can occur at any age, but is often described as either early, or childhood, onset versus adult onset.
Dystonia can affect just one muscle, a group of muscles or all of your muscles. Symptoms can include tremors, voice problems or a dragging foot. Symptoms often start in childhood. They can also start in the late teens or early adulthood. Some cases worsen over time. Others are mild.
About half the cases of dystonia have no connection to disease or injury and are called primary or idiopathic dystonia. Of the primary dystonias, many cases appear to be inherited. Others have it because of another disease. Researchers think that dystonia may be due to a problem in the part of the brain that handles messages about muscle contractions. There is no cure. Doctors use medicines, Botox injections, surgery, physical therapy, and other treatments to reduce or eliminate muscle spasms and pain.
No one treatment has been found to be universally effective. Instead, doctors use a variety of therapies (medications, surgery, and other treatments such as physical therapy, splinting, stress management, and biofeedback) aimed at reducing or eliminating muscle spasms and pain. Since response to drugs varies among individuals and even in the same person over time, the most effective therapy is often individualized.
Athetosis causes
Among the causes of athetosis, are postnatal congenital hypoxia, head trauma, and perinatal kernicterus; with neuronal loss and demyelination that affect the basal ganglia in the latter 6. Kernicterus now describes the clinical features of chronic bilirubin encephalopathy, which include an extrapyramidal movement disorder, sensorineural hearing loss, impaired upward gaze, and dental enamel dysplasia. Aggressive treatment of perinatal hyperbilirubinemia has led to a decline in kernicterus so that, today, it is a rare cause of dyskinetic cerebral palsy. In adults, other causes of athetosis have been described, such as hepatic encephalopathy, Wilson disease, Hallervorden-Spatz Syndrome, Leigh disease, and mitochondrial disease 5.
References- Lanska DJ. Early Controversies over Athetosis: I. Clinical Features, Differentiation from other Movement Disorders, Associated Conditions, and Pathology. Tremor Other Hyperkinet Mov (N Y). ;3:tre-03-132-2918-1. doi:10.7916/D8TT4PPH https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3582863
- Vargas Canas A, Rivas M, Guerrero Torrealba R, Francisca Fajre Caamano M. Marchiafava-Bignami’s Disease, as Etiologic Diagnosis of Athetosis. Ann Neurosci. 2017;24(1):57–60. doi:10.1159/000464424 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5448430
- Birth-related syndromes of athetosis and kernicterus. Handb Clin Neurol. 2011;100:387-95. doi: 10.1016/B978-0-444-52014-2.00030-6. https://www.ncbi.nlm.nih.gov/pubmed/21496597
- Vargas A, Court J. Extrapiramidal dictionary: athetosis. Rev Chil Neuro-Psiquiat. 1996;34:215–216.
- Ropper AH, Brown RH. Principios de Neurología de Adams y Victor. ed 8. McGraw Hill; 2007.
- Przekop A, Sanger TD. Weiner WJ, Tolosa E, editors. Birth-related syndromes of athetosis and kernicterus. Hyperkinetic Movement Disorders. 2011;100:387–398.