What are bisphosphonates
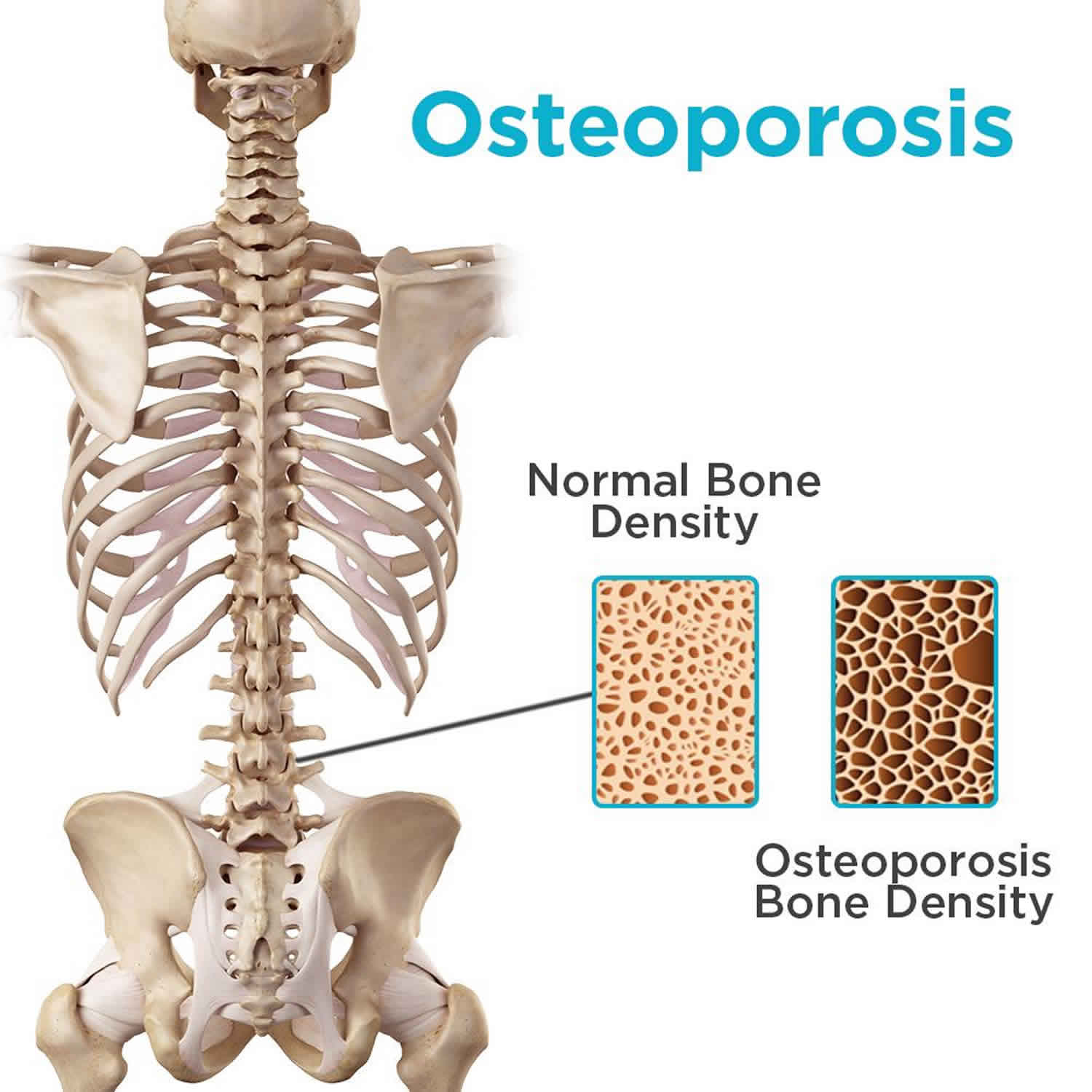
Bisphosphonates are pyrophosphate analogues that become incorporated into bone matrix and suppress osteoclastic activity, thereby reducing bone turnover and increasing bone mass, which makes them valuable agents for the prevention and therapy of osteoporosis. Bisphosphonates are a group of medicines that slow down or prevent bone loss, strengthening bones. Bisphosphonates inhibit osteoclasts which are responsible for breaking down and reabsorbing minerals such as calcium from bone (the process is known as bone resorption). Bisphosphonates allow osteoblasts (bone building cells) to work more effectively, improving bone mass. Bisphosphonates are used in the treatment of osteoporosis, Paget’s disease of bone, and may be used to lower high calcium levels in people with cancer. When used to treat osteoporosis, the optimal duration of treatment is not yet known; however, the majority of benefits appear to happen within the first five years of treatment and long-term use has been associated with atypical femur fractures, osteonecrosis of the jaw and esophageal cancer. Experts recommend the need for bisphosphonate treatment should be reviewed every three to five years.
Bisphosphonates have been shown to be effective in treating malignant hypercalcemia and in preventing and treating osteoporosis. Six bisphosphonates have been approved for use in the United States (year of approval given in parentheses) and they differ in formulation, recommended dose regimen, spectrum of activity and clinical indications.
- Alendronate (1995) is available in tablets of 5 and 10 mg for daily use, 35, 40 and 70 mg (with and without vitamin D) for weekly use, and as a suspension for oral use in several generic forms and under the brand name Fosamax. Indications include prevention and treatment of osteoporosis and treatment of Paget disease of bone.
- Etidronate (1977) is available in tablets of 200 and 400 mg for daily use in generic forms and under the trade name Didronel. Indications include Paget disease of bone and heterotopic ossification, but it has also been used off label for therapy of osteoporosis.
- Ibandronate (2003) is available in tablets of 2.5 mg for daily and 150 mg for monthly use and as an intravenous formulation under the trade name Boniva. Indications include prevention and treatment of osteoporosis.
- Pamidronate (1991) is available as an intravenous formulation generically and under the trade name Aredia. Indications include hypercalcemia of malignancy, multiple myeloma and Paget disease of bone.
- Risedronate (1998) is available in tablets of 5 mg for daily use, 30 and 35 mg for weekly use, and 75 and 150 mg for monthly use in generic forms and under the trade name Actonel. Indications include osteoporosis and Paget disease of bone.
- Zoledronic acid (2001) is available as several intravenous formulations generically and under the brand names Zometa and Reclast. Indications and dosage vary by preparation, but include prevention and treatment of osteoporosis, Paget disease of bone, hypercalcemia of malignancy and multiple myeloma.
Alendronate, risedronate, and ibandronate are given orally, most commonly at weekly (alendronate, risedronate) or monthly (risedronate and ibandronate) intervals. Zoledronic acid and pamidronate are administered intravenously, and there is also an intravenous preparation of ibandronate that may be used. Intravenous preparations are beneficial in patients who cannot tolerate oral bisphosphonates or in whom oral bisphosphonates are contraindicated such as the presence or history of esophageal stricture 1.
Alendronate is given as 35 mg once weekly for the prophylaxis of osteoporosis in postmenopausal females and as 70 mg once weekly for the treatment of osteoporosis in men and women. For Paget disease of bone in males and females, alendronate is given orally as 40 mg once daily for 6 months, and risedronate is given 30 mg orally daily for 2 months. Risedronate is given as 35 mg once weekly and 150 mg once a month. Ibandronate sodium is given as 150 mg orally once a month or 3 mg intravenously every month. Zoledronic acid is given as 4 mg to 5 mg intravenously over at least 15 to 30 minutes every 12 months for the treatment of osteoporosis. Pamidronate is given as 30 mg to 60 mg by slow intravenous infusion every 3 to 6 months for the treatment of hypercalcemia of malignancy, Paget disease, and bone metastasis.
Patients should receive supplemental calcium 1000 to 1200 mg/day and vitamin D 800 to 1000 international units/day if dietary intake is inadequate. Bisphosphonates should be taken as first medication in the morning and more than 30 minutes before the first food intake, beverage (except water), or any other medication. Patients should be instructed to stay erect, not to lay down for at least thirty minutes or until the first food intake of the day to reduce esophageal irritation/ulceration. Milk and milk products, coffee, orange juice, and food may reduce the absorption of alendronate.
The side effects of the bisphosphonates vary by route of administration, but are largely class specific. The oral formulations are generally well tolerated, but are recommended to be given on an empty stomach and with care that they enter the stomach (by drinking water and remaining upright) to avoid esophageal irritation and potential ulceration. Common side effects of oral formulations include headache, abdominal discomfort, dyspepsia, nausea and hypocalcemia. The intravenous formulations of the bisphosphonates can be associated with local infusion reactions and in an acute phase reaction in up to 30% of patients. This is characterized by a flu-like syndrome primarily with the initial infusion. Symptoms arise within 10 to 20 hours after the infusion and are accompanied by increases in C reactive protein, decreases in serum zinc and, in some instances, minor elevations in serum enzymes several days later. Severe side effects of the bisphosphanates are rare, but have included esophageal ulcer, gastrointestinal bleeding, atrial fibrillation and, with long-term treatment, osteonecrosis of the jaw and atypical femoral fractures.
Bisphosphonate therapy
Bisphosphonates define a class of drugs which are widely indicated since the 1990s to treat osteoporosis both in men and women 2. Bisphosphonates effectiveness to treat osteoporosis and other conditions is related to their ability to inhibit bone resorption 3.
- U.S. Food and Drug Administration (FDA)-approved indications for bisphosphonates include treatment of osteoporosis in postmenopausal women, osteoporosis in men, glucocorticoid-induced osteoporosis, hypercalcemia of malignancy, Paget disease of the bone, and malignancies with metastasis to the bone.
- Non-FDA-approved indications include treatment of osteogenesis imperfecta in children as well as adults and prevention of glucocorticoid-induced osteoporosis.
Bisphosphonates contraindications
Widely documented contraindications include hypersensitivity to the bisphosphonate, hypocalcemia, abnormalities of the esophagus such as achalasia, esophageal stricture, esophageal varices, Barrett’s esophagus, inability to stand or sit upright for at least 30 minutes, history of bariatric surgery (Roux-en-Y gastric bypass) and in chronic kidney disease with glomerular filtration rate (GFR) less than 30 to 35 mL/min 2.
How do bisphosphonates work?
Bisphosphonates are pyrophosphate analogues that have two phosphonate groups attached to a central carbon atom that replaces the oxygen present in pyrophosphate. The bisphosphonates bind calcium and are rapidly taken up in bone matrix where they suppress osteoclastic activity and change the balance between bone resorption and bone formation, thus increasing bone mass.
Monitoring
Bone mineral density should be evaluated 1 to 2 years after initiating therapy and every two years or more frequently in patients deemed high risk. Annual measurements of height, weight, serum calcium, 25- hydroxyvitamin D and assessment of back pain for the development of compression fractures should be done.
In some circumstances, monitoring of biochemical markers of bone resorption such as N-telopeptide of type-1 collagen, C-terminal telopeptide of type 1-collagen and pyridinoline cross-links, and markers of bone formation such as bone-specific alkaline phosphatase, osteocalcin, and N-terminal propeptide of type 1 procollagen before and after 3 months after bisphosphonate initiation can be helpful in monitoring the effectiveness of the medication in inhibiting bone resorption and measuring compliance. However, these assays are fraught with significant variability within individual patients and poor standardization, so they are not routinely used.
Alkaline phosphatase should be monitored at 6 to 12 weeks after the treatment initiation in patients with a history of Paget disease and should be repeated at 6-month to 12-month intervals 4.
Bisphosphonates mechanism of action
Bisphosphonates have a structure similar to native pyrophosphate and are divided into two groups: nitrogen-containing and non-nitrogen containing bisphosphonates. Nitrogen-containing bisphosphonates include alendronate, risedronate, ibandronate, pamidronate, and zoledronic acid. Non-nitrogen containing bisphosphonates include etidronate, clodronate, and tiludronate. All bisphosphonates inhibit bone resorption by attaching to hydroxyapatite binding sites on the bone, particularly in areas with active resorption. As bone is resorbed by osteoclasts, the bisphosphonate that is embedded in the bone in released and impairs the osteoclast’s ability to continue bone resorption 3.
Nitrogen-containing bisphosphonates work by inhibiting farnesyl pyrophosphate synthase, which is important in promoting attachment of the osteoclast to the bone. As a result, the osteoclast detaches from the bone surface, thus inhibiting bone resorption.
Non-nitrogen containing bisphosphonates, on the other hand, are metabolized within the cell to substrates that replace the terminal pyrophosphate moiety of adenosine triphosphate, forming a nonfunctional molecule which competes with adenosine triphosphate in the energy metabolism of the cell. This initiates osteoclast apoptosis which in turn leads to an overall decrease in the bone breakdown.
Nitrogen-containing bisphosphonates are much more potent antiresorptive agents than the non-nitrogen-containing bisphosphonates. In addition, non-nitrogen containing bisphosphonates are found to have high potential to inhibit bone mineralization and can cause osteomalacia. For this reason, they are no longer used widely.
Bisphosphonate medication list
Alendronate
Alendronate is used to treat and prevent osteoporosis (a condition in which the bones become thin and weak and break easily) in women who have undergone menopause (”change of life,” end of menstrual periods) and to treat osteoporosis in men. Alendronate is also used to treat osteoporosis in men and women who are taking corticosteroids (a type of medication that may cause osteoporosis in some patients). Alendronate is also used to treat Paget’s disease of bone (a condition in which the bones are soft and weak and may be deformed, painful, or easily broken). Alendronate works by preventing bone breakdown and increasing bone density (thickness).
Alendronate comes as a tablet and a solution (liquid) to take by mouth. The solution is usually taken on an empty stomach once a week in the morning. The 5-mg and 10-mg tablets are usually taken on an empty stomach once a day in the morning, and the 35-mg and 70-mg tablets are usually taken on an empty stomach once a week in the morning. The 40-mg tablets are usually taken once a day in the morning for six months to treat Paget’s disease of bone. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take alendronate exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Alendronate may not work properly and may damage the esophagus (tube between the mouth and stomach) or cause sores in the mouth if it is not taken according to the following instructions. Tell your doctor if you do not understand, you do not think you will remember, or you are unable to follow these instructions:
- You must take alendronate just after you get out of bed in the morning, before you eat or drink anything. Never take alendronate at bedtime or before you wake up and get out of bed for the day.
- Swallow alendronate tablets with a full glass (6 to 8 ounces [180 to 240 mL]) of plain water. Drink at least a quarter of a cup (2 ounces [60 mL]) of plain water after you take alendronate solution. Never take alendronate tablets or solution with tea, coffee, juice, milk, mineral water, sparkling water, or any liquid other than plain water.
- Swallow the tablets whole; do not split, chew or crush them. Do not suck on the tablets.
- After you take alendronate, do not eat, drink, or take any other medications (including vitamins or antacids) for at least 30 minutes. Do not lie down for at least 30 minutes after you take alendronate. Sit upright or stand upright until at least 30 minutes have passed and you have eaten your first food of the day.
Alendronate controls osteoporosis and Paget’s disease of bone but does not cure these conditions. It may take 3 months or longer before your bone density begins to increase. Alendronate helps to treat and prevent osteoporosis only as long as it is taken regularly. Continue to take alendronate even if you feel well. Do not stop taking alendronate without talking to your doctor, but talk to your doctor from time to time about whether you still need to take alendronate.
Ask your pharmacist or doctor for a copy of the manufacturer’s information for the patient.
Alendronate special precautions
Before taking alendronate:
- tell your doctor and pharmacist if you are allergic to alendronate or any other medications.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: angiogenesis inhibitors such as bevacizumab (Avastin), everolimus (Afinitor, Zortress), pazopanib (Votrient), sorafenib (Nexavar), or sunitinib (Sutent); aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Ibu-Tab, Motrin, others) and naproxen (Aleve, Naprelan, Naprosyn, others); cancer chemotherapy; or oral steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
if you are taking any other medications including supplements, vitamins, or antacids by mouth, take them at least 30 minutes after you take alendronate. - tell your doctor if you are unable to sit upright or stand upright for at least 30 minutes and if you have or have ever had a low level of calcium in your blood or any problems with your esophagus. Your doctor may tell you that you should not take alendronate.
- tell your doctor if are undergoing radiation therapy and if you have or have ever had anemia (condition in which the red blood cells do not bring enough oxygen to all the parts of the body); a low level of vitamin D in your body; difficulty swallowing; heartburn; ulcers or other stomach problems;cancer; any type of infection, especially in your mouth; problems with your mouth, teeth, or gums any condition that stops your blood from clotting normally; or dental or kidney disease.
- tell your doctor if you are pregnant or are breast-feeding. Also tell your doctor if you plan to become pregnant at any time in the future, because alendronate may remain in your body for years after you stop taking it. Call your doctor if you become pregnant during or after your treatment.
- you should know that alendronate may cause osteonecrosis of the jaw (ONJ, a serious condition of the jaw bone), especially if you have dental surgery or treatment while you are taking the medication. A dentist should examine your teeth and perform any needed treatments, including cleaning or fixing ill-fitted dentures, before you start to take alendronate. Be sure to brush your teeth and clean your mouth properly while you are taking alendronate. Talk to your doctor before having any dental treatments while you are taking this medication.
- you should know that alendronate may cause severe bone, muscle, or joint pain. You may begin to feel this pain within days, months, or years after you first take alendronate. Although this type of pain may begin after you have taken alendronate for some time, it is important for you and your doctor to realize that it may be caused by alendronate. Call your doctor right away if you experience severe pain at any time during your treatment with alendronate. Your doctor may tell you to stop taking alendronate and your pain may go away after you stop taking the medication.
- talk to your doctor about other things you can do to prevent osteoporosis from developing or worsening. Your doctor will probably tell you to avoid smoking and drinking large amounts of alcohol and to follow a regular program of weight-bearing exercise.
You should eat and drink plenty of foods and drinks that are rich in calcium and vitamin D while you are taking alendronate. Your doctor will tell you which foods and drinks are good sources of these nutrients and how many servings you need each day. If you find it difficult to eat enough of these foods, tell your doctor. In that case, your doctor can prescribe or recommend a supplement.
Alendronate side effects
Alendronate may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- stomach pain
- constipation
- diarrhea
- gas
- bloating or fullness in the stomach
- change in ability to taste food
- headache
- dizziness
- swelling of the joints, hands, or legs
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately before you take any more alendronate:
- new or worsening heartburn
- difficulty swallowing
- pain on swallowing
- chest pain
- bloody vomit or vomit that looks like coffee grounds
- black, tarry, or bloody stools
- fever
- blisters or peeling skin
- rash (may be made worse by sunlight)
- itching
- hives
- swelling of eyes, face, lips, tongue, or throat
- difficulty breathing
- hoarseness
- painful or swollen gums
- loosening of the teeth
- numbness or heavy feeling in the jaw
- poor healing of the jaw
- eye pain
- dull, aching pain in the hips, groin, or thighs
Taking a bisphosphonate medication such as alendronate for osteoporosis may increase the risk that you will break your thigh bone(s). You may feel pain in your hips, groin, or thighs for several weeks or months before the bone(s) break, and you may find that one or both of your thigh bones have broken even though you have not fallen or experienced other trauma. It is unusual for the thigh bone to break in healthy people, but people who have osteoporosis may break this bone even if they do not take alendronate. Talk to your doctor about the risks of taking alendronate.
Alendronate may cause other side effects. Call your doctor if you have any unusual problems while taking alendronate.
Symptoms of alendronate overdose may include the following:
- heartburn
- nausea
- stomach pain
- bloody vomit or vomit that looks like coffee grounds
- difficulty swallowing or pain when swallowing
- bloody or black and tarry stools
Etidronate
Etidronate is used to treat Paget’s disease of bone (a condition in which the bones are soft and weak and may be deformed, painful, or easily broken) and to prevent and treat heterotopic ossification (growth of bone tissue in an area of the body other than the skeleton) in people who have had total hip replacement surgery (surgery to replace the hip joint with an artificial joint) or in people who have had an injury to the spinal cord. Etidronate works by slowing the breakdown of old bone and the formation of new bone.
Etidronate comes as a tablet to take by mouth. It is usually taken once a day on an empty stomach. Treatment for Paget’s disease may be repeated if symptoms come back or worsen after some time has passed. Take etidronate at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take etidronate exactly as directed. Do not take more or less of it or take it more often or for a longer period of time than prescribed by your doctor.
Etidronate is also used sometimes to treat and prevent osteoporosis (condition in which the bones become thin and weak and may break easily) caused by corticosteroids (a type of medication that may cause osteoporosis). Talk to your doctor about the possible risks of using this medication for your condition.
Etidronate may not work properly and may damage the esophagus (tube that connects the mouth and stomach) or cause sores in the mouth if it is not taken according to the following instructions. Tell your doctor if you do not understand, you do not think you will remember, or you are unable to follow these instructions:
- Swallow the tablets with a full glass (6 to 8 ounces [180 to 240 mL]) of plain water while you are sitting or standing.
- Sit or stand upright after taking etidronate.
- Do not eat, drink, or take any other medications (including vitamins or antacids) for 2 hours before and 2 hours after you take etidronate.
If you are taking etidronate to treat Paget’s disease of bone or to prevent or treat heterotopic ossification, it may take some time for your condition to improve. Do not stop taking etidronate without talking to your doctor.
Etidronate special precautions
Before taking etidronate:
- tell your doctor and pharmacist if you are allergic to etidronate, any other medications, or any of the ingredients in etidronate tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: angiogenesis inhibitors such as bevacizumab (Avastin), everolimus (Afinitor, Zortress), pazopanib (Votrient), sorafenib (Nexavar), or sunitinib (Sutent); anticoagulants (‘blood thinners’) such as warfarin (Coumadin, Jantoven); cancer chemotherapy; and oral steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- if you are taking vitamin and mineral supplements such as iron, or if you are taking antacids containing calcium, magnesium, or aluminum (Maalox, Mylanta, Tums, others), take them 2 hours before or 2 hours after you take etidronate.
- tell your doctor if you have or have ever had problems with your esophagus such as an esophageal stricture (narrowing of the esophagus that causes swallowing difficulties) or achalasia (disorder which affects the ability of the esophagus to move food toward the stomach), or osteomalacia (softening of bones due to a lack of minerals). Your doctor may tell you not to take etidronate.
- tell your doctor if you are unable to sit or stand upright and if you have or have ever had anemia (condition in which the red blood cells do not bring enough oxygen to all the parts of the body); a low level of calcium in your blood; difficulty swallowing, heartburn, ulcers, or other stomach problems; cancer; enterocolitis (swelling in the intestines); any type of infection, especially in your mouth; problems with your mouth, teeth, or gums; any condition that stops your blood from clotting normally; or kidney disease. Your doctor may need to change the dose of your medications or monitor you carefully for side effects.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. Also tell your doctor if you plan to become pregnant at any time in the future because etidronate may remain in your body for years after you stop taking it. Call your doctor if you become pregnant during or after your treatment with etidronate.
- you should know that etidronate may cause osteonecrosis of the jaw (ONJ, a serious condition of the jaw bone), especially if you have dental surgery or treatment while you are taking the medication. A dentist should examine your teeth and perform any needed treatments, including cleaning or fixing ill-fitted dentures, before you start to take etidronate. Be sure to brush your teeth and clean your mouth properly while you are taking etidronate. Talk to your doctor before having any dental treatments while you are taking this medication.
- you should know that etidronate may cause severe bone, muscle, or joint pain. You may begin to feel this pain within days, months, or years after you first take etidronate. Although this type of pain may begin after you have taken etidronate for some time, it is important for you and your doctor to realize that it may be caused by etidronate. Call your doctor right away if you experience severe pain at any time during your treatment with etidronate. Your doctor may
- tell you to stop taking etidronate and your pain may go away after you stop taking the medication.
It is important that you get enough calcium and vitamin D and eat a balanced diet while you are taking etidronate. Your doctor will tell you which foods are good sources of these nutrients and how many servings you need each day. If you find it difficult to eat enough of these foods, tell your doctor. In that case, your doctor may prescribe or recommend a supplement.
Etidronate side effects
Etidronate may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- diarrhea
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- new or worsening heartburn
- pain when swallowing
- chest pain
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- hoarseness
- difficulty swallowing
- blisters on the skin
Etidronate may cause other side effects. Call your doctor if you have any unusual problems while taking etidronate.
Symptoms of etidronate overdose may include the following:
- vomiting
- stomach cramps
- diarrhea
- pain, burning, numbness, or tingling in the hands or feet
- muscle spasms and cramps
Ibandronate
Ibandronate is used to prevent and treat osteoporosis (a condition in which the bones become thin and weak and break easily) in women who have undergone menopause (”change of life,” end of menstrual periods). Ibandronate works by preventing bone breakdown and increasing bone density (thickness).
Ibandronate comes as a tablet to take by mouth. The 2.5-mg tablet is usually taken once a day in the morning on an empty stomach and the 150-mg tablet is usually taken once a month in the morning on an empty stomach. The 150-mg tablet should be taken on the same date each month. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take ibandronate exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Ibandronate may not work properly and may damage the esophagus (tube between the mouth and stomach) or cause sores in the mouth if it is not taken according to the following instructions. Tell your doctor if you do not understand, you do not think you will remember, or you are unable to follow these instructions:
- You must take ibandronate just after you get out of bed in the morning, before you eat or drink anything. Never take ibandronate at bedtime or before you wake up and get out of bed for the day.
- Swallow the tablets with a full glass (6 to 8 ounces [180 to 240 mL]) of plain water. Never take ibandronate with tea, coffee, juice, milk, mineral water, sparkling water, or any liquid other than plain water.
- Swallow the tablets whole; do not split, chew, or crush them. Do not suck on the tablets.
- After you take ibandronate, do not eat, drink, or take any other medications (including vitamins or antacids) for at least 60 minutes. Do not lie down for at least 60 minutes after you take ibandronate. Sit upright or stand upright for at least 60 minutes.
Ibandronate controls osteoporosis but does not cure it. Ibandronate helps to treat and prevent osteoporosis only as long as it is taken regularly. Continue to take ibandronate even if you feel well. Do not stop taking ibandronate without talking to your doctor, but talk to your doctor from time to time about whether you still need to take ibandronate.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with ibandronate and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (http://www.fda.gov/Drugs/DrugSafety/ucm085729.htm) or the manufacturer’s website to obtain the Medication Guide.
Ibandronate special precautions
Before taking ibandronate:
- tell your doctor and pharmacist if you are allergic to ibandronate, any other medications, or any of the ingredients in ibandronate tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: angiogenesis inhibitors such as bevacizumab (Avastin), everolimus (Afinitor, Zortress), pazopanib (Votrient), sorafenib (Nexavar), or sunitinib (Sutent); aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Ibu-Tab, Motrin, others) and naproxen (Aleve, Naprelan, Naprosyn, others); cancer chemotherapy; and oral steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
if you are taking any oral medications, including supplements, vitamins, or antacids, take them at least 60 minutes after you take ibandronate. - tell your doctor if you are unable to sit upright or stand upright for at least 60 minutes and if you have or have ever had a low level of calcium in your blood. Your doctor may tell you not to take ibandronate.
- tell your doctor if are undergoing radiation therapy and if you have or have ever had anemia (condition in which the red blood cells do not bring enough oxygen to all the parts of the body); difficulty swallowing; heartburn; ulcers or other problems with your stomach or esophagus (tube that connects the throat to the stomach); cancer; any type of infection, especially in your mouth; problems with your mouth, teeth, or gums; any condition that stops your blood from clotting normally; or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. Also tell your doctor if you plan to become pregnant at any time in the future, because ibandronate may remain in your body for years after you stop taking it. Call your doctor if you become pregnant during or after your treatment.
- you should know that ibandronate may cause osteonecrosis of the jaw (ONJ, a serious condition of the jaw bone), especially if you have dental surgery or treatment while you are taking the medication. A dentist should examine your teeth and perform any needed treatments, including cleaning or fixing ill-fitted dentures, before you start to take ibandronate. Be sure to brush your teeth and clean your mouth properly while you are taking ibandronate. Talk to your doctor before having any dental treatments while you are taking this medication.
- you should know that ibandronate may cause severe bone, muscle, or joint pain. You may begin to feel this pain within days, months, or years after you first take ibandronate. Although this type of pain may begin after you have taken ibandronate for some time, it is important for you and your doctor to realize that it may be caused by ibandronate. Call your doctor right away if you experience severe pain at any time during your treatment with ibandronate. Your doctor may tell you to stop taking ibandronate and your pain may go away after you stop taking the medication.
- talk to your doctor about other things you can do to prevent osteoporosis from developing or worsening. Your doctor will probably tell you to avoid smoking and drinking large amounts of alcohol and to follow a regular program of weight-bearing exercise.
You should eat and drink plenty of foods and drinks that are rich in calcium and vitamin D while you are taking ibandronate. Your doctor will tell you which foods and drinks are good sources of these nutrients and how many servings you need each day. If you find it difficult to eat enough of these foods, tell your doctor. In that case, your doctor may prescribe or recommend a supplement.
Ibandronate side effects
Ibandronate may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- stomach pain
- diarrhea
- constipation
- weakness
- dizziness
- headache
- fever, sore throat, chills, cough, and other signs of infection
- frequent or urgent need to urinate
- painful urination
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately before you take any more ibandronate:
- new or worsening heartburn
- difficulty swallowing
- pain on swallowing
- upper chest pain
- rash
- painful or swollen gums
- loosening of the teeth
- numbness or heavy feeling in the jaw
- poor healing of the jaw
- dull, aching pain in the hips, groin, or thighs
Ibandronate may cause other side effects. Call your doctor if you have any unusual problems while taking ibandronate.
Taking a bisphosphonate medication such as ibandronate for osteoporosis may increase the risk that you will break your thigh bone(s). You may feel pain in your hips, groin, or thighs for several weeks or months before the bone(s) break, and you may find that one or both of your thigh bones have broken even though you have not fallen or experienced other trauma. It is unusual for the thigh bone to break in healthy people, but people who have osteoporosis may break this bone even if they do not take ibandronate. Talk to your doctor about the risks of taking ibandronate.
Symptoms of ibandronate overdose may include the following:
- nausea
- stomach pain
- heartburn
Pamidronate Injection
Pamidronate is used to treat high levels of calcium in the blood that may be caused by certain types of cancer. Pamidronate is also used along with cancer chemotherapy to treat bone damage caused by multiple myeloma (cancer that begins in the plasma cells [a type of white blood cell that produces substances needed to fight infection]) or by breast cancer that has spread to the bones. Pamidronate is also used to treat Paget’s disease (a condition in which the bones are soft and weak and may be deformed, painful, or easily broken). Pamidronate injection works by slowing bone breakdown, increasing bone density (thickness) and decreasing the amount of calcium released from the bones into the blood.
Pamidronate injection comes as a solution (liquid) to inject into a vein slowly, over 2 to 24 hours. It is usually injected by a health care provider in a doctor’s office, hospital, or clinic. It may be given once every 3 to 4 weeks, once a day for 3 days in a row, or as a single dose that may be repeated after 1 week or longer. The treatment schedule depends on your condition.
Your doctor may recommend a calcium supplement and a multivitamin containing vitamin D to take during your treatment. You should take these supplements every day as directed by your doctor.
Pamidronate special precautions
Before receiving pamidronate injection:
- tell your doctor and pharmacist if you are allergic to pamidronate injection, alendronate (Fosamax), etidronate (Didronel), risedronate (Actonel), tiludronate (Skelid), zoledronic acid (Zometa), any other medications, or any of the ingredients in pamidronate injection. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: cancer chemotherapy medications; oral steroids such as dexamethasone (Decadron, Dexone), methylprednisolone (Medrol), and prednisone (Deltasone);and thalidomide (Thalomid). Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Many other medications may also interact with pamidronate injection, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list.
- tell your doctor if you are being treated with radiation therapy and if you have or have ever had thyroid surgery, seizures, or liver or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. You should use a reliable method of birth control to prevent pregnancy while you are receiving pamidronate. If you become pregnant while receiving pamidronate, call your doctor immediately. Talk to your doctor if you plan to become pregnant at any time in the future because pamidronate may remain in your body for years after you stop using it.
- you should know that pamidronate may cause serious problems with your jaw, especially if you have dental surgery or treatment while you are taking the medication. A dentist should examine your teeth and perform any needed treatments before you start to receive pamidronate. Be sure to brush your teeth and clean your mouth properly while you are receiving pamidronate. Talk to your doctor before having any dental treatments while you are receiving this medication.
- you should know that pamidronate injection may cause severe bone, muscle, or joint pain. You may begin to feel this pain within days, months, or years after you first receive pamidronate injection. Although this type of pain may begin after you have received pamidronate injection for some time, it is important for you and your doctor to realize that it may be caused by pamidronate. Call your doctor right away if you experience severe pain at any time during your treatment with pamidronate inejction. Your doctor may stop giving you pamidronate injection and your pain may go away after you stop treatment with this medication.
Pamidronate side effects
Pamidronate injection may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- redness, swelling, or pain in the injection spot
- stomach pain
- loss of appetite
- constipation
- nausea
- vomiting
- heartburn
- change in ability to taste food
- sores in the mouth
- fever
- headache
- dizziness
- excessive tiredness
- difficulty falling asleep or staying asleep
- coughing
- difficulty urinating or painful urination
- swelling of the hands, arms, feet, ankles, or lower legs
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately:
- painful or swollen gums
- loosening of the teeth
- numbness or heavy feeling in the jaw
- poor healing of the jaw
- vomit that is bloody or looks like coffee grounds
- bloody or black and tarry stools
- shortness of breath
- fast heartbeat
- fainting
- sudden tightening of muscles
- numbness or tingling around the mouth
- eye pain or tearing
Pamidronate injection may cause other side effects. Call your doctor if you have any unusual problems while taking pamidronate injection.
Symptoms of pamidronate injection overdose may include:
- fever
- change in ability to taste food
- sudden tightening of the muscles
- numbness or tingling around the mouth
Risedronate
Risedronate tablets and delayed-release (long-acting tablets) are used to prevent and treat osteoporosis (a condition in which the bones become thin and weak and break easily) in women who have undergone menopause (”change of life,” end of menstrual periods). Risedronate tablets are also used to treat osteoporosis in men, and in men and women who are taking glucocorticoids (a type of corticosteroid medication that may cause osteoporosis). Risedronate tablets are also used to treat Paget’s disease of bone (a condition in which the bones are soft and weak and may be deformed, painful, or easily broken). Risedronate works by preventing bone breakdown and increasing bone density (thickness).
Risedronate comes as a tablet and a delayed-release tablet to take by mouth. The delayed-release tablets are usually taken once a week in the morning, immediately after breakfast. The tablets are usually taken on an empty stomach once a day in the morning, once a week in the morning, once monthly in the morning, or once monthly for two mornings in a row depending on your condition and the dosage prescribed by your doctor. If you are taking risedronate once a week, once monthly, or once monthly for 2 days in a row, take it on the same day every week or month or the same 2 days in a row every month. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take risedronate exactly as directed. Do not take more or less of it or take it more often or for a longer period of time than prescribed by your doctor.
Risedronate may not work properly and may damage the esophagus (tube that connects the mouth and stomach) or cause sores in the mouth if it is not taken according to the following instructions. Tell your doctor if you do not understand, you do not think you will remember, or you are unable to follow these instructions:
- You must take risedronate tablets immediately after you get out of bed in the morning and before you eat or drink anything. You must take risedronate delayed-release tablets immediately after breakfast. Never take risedronate at bedtime or before you wake up and get out of bed for the day.
- Swallow the tablets with a full glass (6 to 8 ounces [180 to 240 mL]) of plain water while you are sitting or standing. Swallow the delayed-release tablets with at least 4 ounces (120 mL) of plain water while you are sitting or standing. Never take risedronate with tea, coffee, juice, mineral water, milk, other dairy drinks, or any liquid other than plain water.
- Swallow the tablets and delayed-release tablets whole. Do not split, chew, or crush them. Do not suck on the tablets or hold them in your mouth for any length of time.
- After you take risedronate, do not eat, drink, or take any other medications for at least 30 minutes. Do not lie down for at least 30 minutes after you take risedronate. Sit upright or stand upright until at least 30 minutes have passed.
Risedronate controls osteoporosis and Paget’s disease of bone but does not cure these conditions. Risedronate helps to treat and prevent osteoporosis only as long as it is taken regularly. Continue to take risedronate even if you feel well. Do not stop taking risedronate without talking to your doctor, but talk to your doctor from time to time about whether you still need to take risedronate.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with risedronate and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (http://www.fda.gov/Drugs/DrugSafety/ucm085729.htm) or the manufacturer’s website to obtain the Medication Guide.
Risedronate special precautions
Before taking risedronate:
- tell your doctor and pharmacist if you are allergic to risedronate, any other medications, or any of the ingredients in risedronate tablets or delayed-release tablets. Ask your pharmacist or check the Medication Guide for a list of the ingredients
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: angiogenesis inhibitors such as bevacizumab (Avastin), everolimus (Afinitor, Zortress), pazopanib (Votrient), sorafenib (Nexavar), or sunitinib (Sutent); aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Ibu-Tab, Motrin, others) and naproxen (Aleve, Naprelan, Naprosyn, others); cancer chemotherapy; or oral steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos). If you are taking the delayed-release tablets, you should also tell your doctor if you are taking an H2 blocker such as cimetidine, famotidine (Pepcid), nizatidine (Axid), and ranitidine (Zantac) or a proton pump inhibitor such as esomeprazole (Nexium, in Vimovo), lansoprazole (Prevacid), omeprazole (Prilosec, Zegerid), pantoprazole (Protonix), and rabeprazole (AcipHex). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- you should know that Actonel and Atelvia both contain risedronate. You cannot take both of these medications at the same time.
- if you are taking any other oral medications including vitamins, supplements, or antacids, take them at least 30 minutes after you take risedronate.
- tell your doctor if you have or have ever had a low level of calcium in your blood or any problems with your esophagus and if you are unable to sit upright or stand upright for at least 30 minutes. Your doctor may tell you that you should not take risedronate.
- tell your doctor if you are undergoing radiation therapy; if you have or have ever had difficulty swallowing; heartburn; ulcers or other problems with your stomach; anemia (condition in which the red blood cells do not bring enough oxygen to all the parts of the body); cancer; any type of infection, especially in your mouth; problems with your mouth, teeth, or gums; any condition that stops your blood from clotting normally; or dental or kidney disease.
- tell your doctor if you are pregnant or are breastfeeding. Also tell your doctor if you plan to become pregnant at any time in the future, because risedronate may remain in your body for years after you stop taking it. Call your doctor if you become pregnant during or after your treatment with risedronate.
- you should know that risedronate may cause severe bone, muscle, or joint pain. You may begin to feel this pain within days, months, or years after you first take risedronate. Although this type of pain may begin after you have taken risedronate for some time, it is important for you and your doctor to realize that it may be caused by risedronate. Call your doctor right away if you experience severe pain at any time during your treatment with risedronate. Your doctor may tell you to stop taking risedronate and your pain may go away after you stop taking the medication.
- you should know that risedronate may cause osteonecrosis of the jaw (ONJ, a serious condition of the jaw bone), especially if you have dental surgery or treatment while you are taking the medication. A dentist should examine your teeth and perform any needed treatments, including cleaning or fixing ill-fitted dentures, before you start to take risedronate. Be sure to brush your teeth and clean your mouth properly while you are taking risedronate. Talk to your doctor before having any dental treatments while you are taking this medication.
- talk to your doctor about other things you can do to prevent osteoporosis from developing or worsening. Your doctor will probably tell you to avoid smoking and drinking large amounts of alcohol and to follow a regular program of weight-bearing exercise.
You should eat plenty of foods that are rich in calcium and vitamin D while you are taking risedronate. Your doctor will tell you which foods are good sources of these nutrients and how many servings you need each day. If you find it difficult to eat enough of these foods, tell your doctor. In that case, your doctor can prescribe or recommend a supplement.
Risedronate side effects
Risedronate may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- burping
- dry mouth
- stomach pain
- diarrhea
- constipation
- gas
- headache
- dizziness
- weakness
- leg cramps
- back pain
- frequent or urgent need to urinate
- painful urination
Some side effects can be serious. If you experience any of the following side effects, call your doctor immediately before you take any more risedronate:
- difficulty swallowing or pain when swallowing
- new or worsening heartburn
- chest pain
- itching
- rash
- hives
- blisters on skin
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- difficulty breathing
- hoarseness
- muscle spasms, twitching, or cramps
- numbness or tingling around mouth or in hands or feet
- swollen, red, or painful eyes
- sensitivity to light
- painful or swollen gums
- loosening of the teeth
- numbness or heavy feeling in the jaw
- poor healing of the jaw
- dull, aching pain in the hips, groin, or thighs
Risedronate may cause other side effects. Call your doctor if you have any unusual problems while taking risedronate.
Taking a bisphosphonate medication such as risedronate for osteoporosis may increase the risk that you will break your thigh bone(s). You may feel pain in your hips, groin, or thighs for several weeks or months before the bone(s) break, and you may find that one or both of your thigh bones have broken even though you have not fallen or experienced other trauma. It is unusual for the thigh bone to break in healthy people, but people who have osteoporosis may break this bone even if they do not take risedronate. Talk to your doctor about the risks of taking risedronate.
Symptoms of risedronate overdose may include the following:
- numbness or tingling around mouth or in hands or feet
- muscle spasms, cramps, or twitches
- seizures
Zoledronic Acid Injection
Zoledronic acid (Reclast) is used to prevent or treat osteoporosis (condition in which the bones become thin and weak and break easily) in women who have undergone menopause (‘change of life,’ end of regular menstrual periods). Zoledronic acid (Reclast) is also used to treat osteoporosis in men, and to prevent or treat osteoporosis in men and women who are taking glucocorticoids (a type of corticosteroid medication that may cause osteoporosis). Zoledronic acid (Reclast) is also used to treat Paget’s disease of bone (a condition in which the bones are soft and weak and may be deformed, painful, or easily broken). Zoledronic acid (Zometa) is used to treat high levels of calcium in the blood that may be caused by certain types of cancer. Zoledronic acid (Zometa) is also used along with cancer chemotherapy to treat bone damage caused by multiple myeloma [cancer that begins in the plasma cells (white blood cells that produce substances needed to fight infection)] or by cancer that began in another part of the body but has spread to the bones. Zoledronic acid (Zometa) is not cancer chemotherapy, and it will not slow or stop the spread of cancer. However, it can be used to treat bone disease in patients who have cancer. Zoledronic acid works by slowing bone breakdown, increasing bone density (thickness), and decreasing the amount of calcium released from the bones into the blood.
Zoledronic acid comes as a solution (liquid) to inject into a vein over at least 15 minutes. It is usually injected by a healthcare provider in a doctor’s office, hospital, or clinic. When zoledronic acid injection is used to treat high blood levels of calcium caused by cancer it is usually given as a single dose. A second dose may be given at least 7 days after the first dose if blood calcium does not drop to normal levels or does not remain at normal levels. When zoledronic acid injection is used to treat bone damage caused by multiple myeloma or cancer that has spread to the bones, it is usually given once every 3 to 4 weeks. When zoledronic acid injection is used to treat osteoporosis in women who have undergone menopause, or in men, or to treat or prevent osteoporosis in people who are taking glucocorticoids, it is usually given once a year. When zoledronic acid is used to prevent osteoporosis in women who have undergone menopause, it is usually given once every 2 years. When zoledronic acid is used to treat Paget’s disease of bone, it is usually given as a single dose, but additional doses may be given after some time has passed.
Be sure to drink at least 2 glasses of water or another liquid within a few hours before you receive zoledronic acid.
Your doctor may prescribe or recommend a calcium supplement and a multivitamin containing vitamin D to take during your treatment. You should take these supplements every day as directed by your doctor. Tell your doctor if there is any reason that you will not be able to take these supplements during your treatment.
You may experience a reaction during the first few days after you receive a dose of zoledronic acid injection. Symptoms of this reaction may include flu-like symptoms, fever, headache, chills, and bone, joint or muscle pain. These symptoms may begin during the first 3 days after you receive a dose of zoledronic acid injection and may last 3 to 14 days. Your doctor may tell you to take a nonprescription pain reliever/fever reducer after you receive zoledronic acid injection to prevent or treat these symptoms.
If you are receiving zoledronic acid injection to prevent or treat osteoporosis, you must continue to receive the medication as scheduled even if you are feeling well. You should talk to your doctor from time to time about whether you still need to be treated with this medication.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with zoledronic acid injection and each time you receive a dose. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (http://www.fda.gov/Drugs/DrugSafety/ucm085729.htm) or the manufacturer’s website} to obtain the Medication Guide.
Zoledronic acid special precautions
Before receiving zoledronic acid injection:
- tell your doctor and pharmacist if you are allergic to zoledronic acid or any other medications, or any of the ingredients in zoledronic acid injection. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
you should know that zoledronic acid injection is available under the brand names Zometa and Reclast. You should only be treated with one of these products at a time. - tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: aminoglycoside antibiotics such as amikacin (Amikin), gentamicin (Garamycin), kanamycin (Kantrex), neomycin (Neo-Rx, Neo-Fradin), paromomycin (Humatin), streptomycin, and tobramycin (Tobi, Nebcin); aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve, Naprosyn); cancer chemotherapy medications; digoxin (Lanoxin, in Digitek); diuretics (‘water pills’) such as bumetanide (Bumex), ethacrynic acid (Edecrin), and furosemide (Lasix); and oral steroids such as dexamethasone (Decadron, Dexone), methylprednisolone (Medrol), and prednisone (Deltasone). Many other medications may interact with zoledronic acid, so tell your doctor about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had kidney disease or if you have a dry mouth, dark urine, decreased sweating, dry skin, and other signs of dehydration or recently have had diarrhea, vomiting, fever, infection, excessive sweating, or have been unable to drink enough fluids. Your doctor will wait until you are no longer dehydrated before giving you zoledronic acid injection or if you have certain types of kidney disease may not prescribe this treatment for you. Also tell your doctor if you have ever had a low level of calcium in your blood. Your doctor will probably check the level of calcium in your blood before you begin treatment and may not prescribe this medication if the level is too low.
- tell your doctor if you have been treated with zoledronic acid or other bisphosphonates (Actonel, Actonel+Ca, Aredia, Boniva, Didronel, Fosamax, Fosamax+D, Reclast, Skelid, and Zometa) in the past; if you have ever had surgery on your parathyroid gland (small gland in the neck) or thyroid gland or surgery to remove sections of your small intestine; and if you have or have ever had heart failure (condition in which the heart cannot pump enough blood to other parts of the body); anemia (condition in which red blood cells cannot bring enough oxygen to other parts of the body); any condition that stops your blood from clotting normally; low levels of calcium, magnesium, or potassium in your blood; any condition that prevents your body from absorbing nutrients from food; or problems with your mouth, teeth, or gums; an infection, especially in your mouth; asthma or wheezing, especially if it is made worse by taking aspirin; or parathyroid or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. You should use a reliable method of birth control to prevent pregnancy while you are receiving zoledronic acid. If you become pregnant while receiving zoledronic acid, call your doctor. Zoledronic acid may harm the fetus. Talk to your doctor if you plan to become pregnant at any time in the future because zoledronic acid may remain in your body for years after you stop receiving it.
- you should know that zoledronic acid injection may cause severe bone, muscle, or joint pain. You may begin to feel this pain within daysor months after you first receive zoledronic acid injection. Although this type of pain may begin after you have received zoledronic acid injection for some time, it is important for you and your doctor to realize that it may be caused by zoledronic acid. Call your doctor right away if you experience severe pain at any time during your treatment with zoledronic acid injection. Your doctor may stop giving you zoledronic acid injection and your pain may go away after you stop treatment with this medication.
- you should know that zoledronic acid may cause osteonecrosis of the jaw (ONJ, a serious condition of the jaw bone), especially if you have dental surgery or treatment while you are using the medication. A dentist should examine your teeth and perform any needed treatments, including cleaning, before you start to use zoledronic acid. Be sure to brush your teeth and clean your mouth properly while you are using zoledronic acid. Talk to your doctor before having any dental treatments while you are using this medication.
Zoledronic acid side effects
Zoledronic acid may cause side effects. Tell your doctor if any of these symptoms, or those listed in the special precautions sections, are severe or do not go away:
- itching, redness, pain, or swelling in the place where you received your injection
- red, swollen, itchy, or teary eyes or swelling around the eyes
- constipation
- nausea
- vomiting
- diarrhea
- stomach pain
- loss of appetite
- weight loss
- heartburn
- mouth sores
- excessive worry
- agitation
- depression
- difficulty falling asleep or staying asleep
- fever, chills, cough, and other signs of infection
- white patches in the mouth
- swelling, redness, irritation, burning, or itching of the vagina
- white vaginal discharge
- numbness or tingling around the mouth or in fingers or toes
- hair loss
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- rash
- hives
- itching
- swelling of the eyes, face, lips, tongue, throat, hands, arms, feet, ankles, or lower legs
- hoarseness
- difficulty breathing or swallowing
- upper chest pain
- irregular heart beat
- muscle spasms, twitches, or cramps
- unusual bruising or bleeding
- painful or swollen gums
- loosening of the teeth
- numbness or heavy feeling in the jaw
- sore in the mouth or the jaw that does not heal
Zoledronic acid may cause other side effects. Call your doctor if you have any unusual problems while taking zoledronic acid injection.
Being treated with a bisphosphonate medication such as zoledronic acid injection for osteoporosis may increase the risk that you will break your thigh bone(s). You may feel dull, aching pain in your hips, groin, or thighs for several weeks or months before the bone(s) break, and you may find that one or both of your thigh bones have broken even though you have not fallen or experienced other trauma. It is unusual for the thigh bone to break in healthy people, but people who have osteoporosis may break this bone even if they do not receive zoledronic acid injection. Talk to your doctor about the risks of receiving zoledronic acid injection.
Symptoms of zoledronic acid overdose may include the following:
- fever
- weakness
- sudden tightening of muscles or muscle cramps
- fast, pounding, or irregular heart beat
- dizziness
- uncontrollable eye movements
- double vision
- depression
- difficulty walking
- uncontrollable shaking of a part of your body
- seizures
- confusion
- shortness of breath
- pain, burning, numbness or tingling in the hands or feet
- difficulty speaking
- difficulty swallowing
- decreased urination
Bisphosphonates side effects
Side effects of bisphosphonates includes: acute phase reaction (10% to 30%) with transient pyrexia with myalgias, arthralgias, headaches, and influenza-like symptoms, transient hypocalcemia (18%), hypophosphatemia (10%), musculoskeletal paib (less than or equal to 6%), flatulence (less than or equal to 4%), headache and gastroesophageal reflux disease (3%), constipation or diarrhea (less than or equal to 3%), abdominal pain (2% to 7%), esophageal ulcer (2%), acid regurgitation (1% to 5%), abdominal distension, gastric ulcer, gastritis and muscle cramps (less than or equal to 1%) 2.
Other side effects
One of the most severe adverse effects is bisphosphonate-related osteonecrosis of the jaw (BRONJ). Bisphosphonate-related osteonecrosis of the jaw is diagnosed if all the following criteria are met:
- History of treatment with a bisphosphonate;
- Those who had more than 8 weeks of exposed bone in the maxillofacial region
- No radiation therapy to the jaw
The American Association of Oral and Maxillofacial Surgeons has further defined the stages of Bisphosphonate-related osteonecrosis of the jaw (BRONJ) as follows:
- Stage 0: Indicated by no visible bone but nonspecific symptoms. Common treatment includes Symptomatic treatment and conservative management of underlying dental issues; antibiotics are recommended if the infection is present.
- Stage 1: Indicated by exposed, inflamed necrotic bone without symptoms. Common treatment includes antimicrobial rinses (if the infection is not present).
- Stage 2: Indicated by exposed, necrotic bone with local signs or symptoms of infection. Common treatment includes symptomatic treatment, antimicrobial rinses, and systemic antibiotics.
- Stage 3: Indicated by exposed, necrotic bone with pain and infection, pathologic fracture, extraoral fistula and extensive osteolysis. Common treatment includes symptomatic treatment, systemic antibiotics and superficial surgical debridement of the necrotic bone.
Dose modification or preferably stopping oral bisphosphonate therapy should be done in patients exhibiting systemic symptoms since bisphosphonates are known to affect the jaw completely and may lead to progression of bisphosphonate-related osteonecrosis of the jaw.
Another serious adverse effect of bisphosphonates is atypical femoral fracture typically involving diaphysis or sub-trochanteric region of the femur. It is caused by pathophysiological alterations of the bone quality and fracture repair process resulting in over-suppression of bone turnover.
Due to potential serious nature of bisphosphonate-related osteonecrosis of the jaw and atypical femur fracture, a two year drug holiday is recommended after 5 to 10 years for the oral bisphosphonates and 3 to 5 years for zoledronic acid.
References- US Preventive Services Task Force. Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW, Kemper AR, Kubik M, Landefeld CS, Mangione CM, Phipps MG, Pignone M, Silverstein M, Simon MA, Tseng CW, Wong JB. Screening for Osteoporosis to Prevent Fractures: US Preventive Services Task Force Recommendation Statement. JAMA. 2018 Jun 26;319(24):2521-2531
- Ganesan K, Roane D. Bisphosphonate. [Updated 2019 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470248
- Farrell KB, Karpeisky A, Thamm DH, Zinnen S. Bisphosphonate conjugation for bone specific drug targeting. Bone Rep. 2018 Dec;9:47-60
- Aparecida Cariolatto F, Carelli J, de Campos Moreira T, Pietrobon R, Rodrigues C, Bonilauri Ferreira AP. Recommendations for the Prevention of Bisphosphonate-Related Osteonecrosis of the Jaw: A Systematic Review. J Evid Based Dent Pract. 2018 Jun;18(2):142-152