Black piedra
Black piedra also known as trichomycosis nodosa, tinea nodosa or trichosporosis, is Piedraia hortae fungus infection of the hair shafts resulting in the formation of small black nodules 1. The fungal elements are attached to the hair shaft to form nodules along the hair shaft. Piedra refers to colonization of the hair shaft that results in firm, irregular nodules. If the nodule is dark, the infection is black piedra and is due to Piedraia hortae fungus. If the nodule is white, the infection is White Piedra and is due to Trichosporon beigelii. Though piedra can occur at any age, its incidence usually drops off after middle age 2.
- Black piedra (Piedraia hortae fungus): firmly adherent, black, firm, oval or elongated papules, composed of a mass of fungus cells; scalp most common site of involvement, but also seen in the beard and pubic areas
- White piedra (Trichosporon beigelii fungus): soft, white or light-brown papules loosely adherent to or within the hair shaft; scalp most common site of involvement, but also seen in the beard and pubic areas; increased carriage rate in HIV-positive patients; may be sexually transmitted
Black piedra is characterized by formation of brown to black nodules that are very firmly attached to the hair shaft. Black piedra predominantly affects scalp hair, although involvement of the beard, mustache and pubic hairs is also known. The nodules are composed of ascostromata which are the fruiting body of the fungus containing asci (sexual spore-bearing cell produced in ascomycete fungi) and ascospores. Most of the cases are asymptomatic and may remain so for years. However, breaks due to weakness of the hair shaft may occur eventually in severe cases. Black piedra mostly involves individuals who live in tropical areas (particularly in South America and Southeast Asian countries) and use oily substances for hair care 3. Black piedra is rare in Europe. Mixed infections both black piedra (Piedraia hortae) and white piedra (Trichosporon beigelii) may occur simultaneously in a patient, but is extremely rare 4.
The exact mode of spread of piedra is not clear. The use of an infected comb or sharing of pillows and bedsheets may be the possible factors for transmission 5. There are also reports of sexual transmission.
Shaving the head of all the hair is the best way to get rid of this fungal infection. However, this option may not be acceptable to females for aesthetic reasons.
Black piedra treatment options 1:
- 2% ketoconazole or 2% miconazole shampoo or 1 to 1.5% ciclopirox shampoo applied once-to-twice-a-week for 3 to 4 weeks
- Oral terbinafine 250 mg once daily for 6 weeks
- Oral itraconazole 100 mg twice-a-day after a meal, with a citrus drink for 1 to 2 weeks
- Counseling on the maintenance of good scalp hygiene, avoidance of sharing combs, etc.
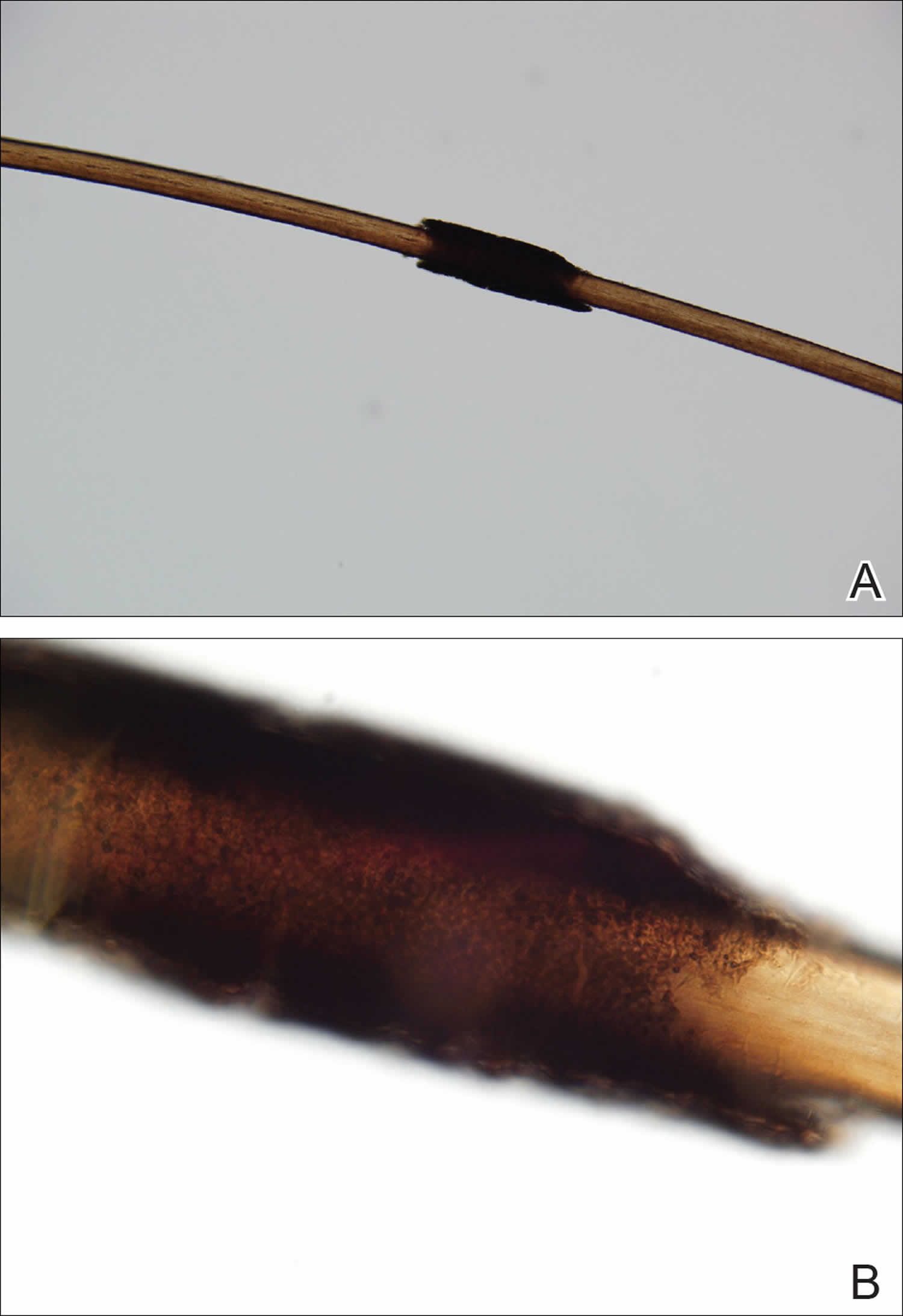
Figure 1. Black piedra hair
Footnote: Black piedra findings on microscopic examination (original magnifications ×100 and ×400) of the hair shafts under light microscopy including brown to black firmly adherent concretions (A and B).
Figure 2. White piedra (whitish nodule attached to the hair shaft)
Black piedra causes
Black piedra results from a particular fungal species called Piedraia hortae. This fungal disease results from poor personal hygiene. Black piedra is commonly seen in people having long hair and with the excessive use of different hair oils. The exact mode of spread of piedra is not clear. Practices like prolonged wearing of veils or tight hats may contribute to its development and progression. The use of an infected comb or sharing of pillows and bedsheets may be the possible factors for transmission 5. There are also reports of sexual transmission. The incidence of fungal infections is on the rise due to the opportunistic nature of the fungal organisms and the prevalence of immunodeficient conditions 6.
The soil appears to be the primary source of infection in black piedra, although Piedraia hortae, has also been traced in stagnant water and crops. Piedraia hortae can produce sexual spores in the parasitic phase, which is a unique feature of this fungus among other pathogenic fungi.
Hairs with black piedra isolated from Brazilian Indians were investigated by studying serial sections with light and transmission electron microscopy 7. Piedraia hortae showed strong keratolytic activity; it was able to destroy both the cuticle and the hair cortex. Two well-defined types of cortex digestion appeared. The first one was parallel to the axis of hair and was produced by fungal cells that grew separating the external layers of the outer cortex. The second type was produced by active boring hyphae, forming channels as they penetrated vertical to the axis of hair.
In vivo and in vitro studies using electron microscopy and x-ray microanalysis have shown elements like phosphorus, sulfur, and calcium in the nodules that develop on hair and in culture colonies. These elements are part of the extracellular material that compacts the pseudoparenchymatous organization of the fungus. Their presence is due to the capacity of melanin-like pigments to sequester ions. They may form part of the mucopolysaccharides that constitute the extracellular material. Researchers detected contaminants such as aluminum, silicon, and iron on the surface of the nodule; these have links to the residual molecules produced during the breakdown of the cuticular keratin 8.
In Piedraia hortae, the cementing extracellular material that holds the nodule together is probably the main factor responsible for preserving the fungus against environmental attack and desiccation. Moreover, this compact organization can also impair successful treatment, which may explain why an untreated black piedra may run a very chronic course.
Black piedra signs and symptoms
Black piedra is asymptomatic, except for the unsightly nodes visible on hair strands. On examination, the hair shaft shows firmly attached brown-black nodules, which are less than 1mm in size. These nodules are gritty on palpation. The nodules are usually multiple and vary in size from microscopic to 1 mm or more in diameter. They are oval or elongated in shape with their thickness tapering from one end to the other or from the middle to the edge. They are composed of a compact cellular substance that surrounds the hair shaft. Hair shafts affected by these nodules become weak and often break at the point of infection. Black piedra is chronic and can last for months or even years.
Black piedra complications
There are no serious complications of black piedra infection. In the absence of treatment, patients with comorbidities (diabetes, immunodeficiency, and malignant tumors) may develop alopecia.
Reports exist of secondary pediculosis (head lice), as well as mixed piedra (black piedra plus white piedra in the same individual) in patients with poor scalp hygiene 9.
Black piedra diagnosis
Trichoscopy: Hair examination using trichoscopy may provide useful information for the correct diagnosis by differentiating pseudonits from nits 10. It shows multiple oval or elongate-shaped brown-black nodules on the hair shaft.
Direct microscopic examination: The microscopic examination of the colonies shows round, dark brown, globus ascus with ascospores. Direct microscopic examination of the crushed nodules under 10% potassium hydroxide (KOH) shows branched hyphae (4 to 8 microns) held together by a cement-like substance. The dematiaceous filamentous hyphae appear as chains of stout thick-walled cells resembling arthrospores. Visualization enhancement can be via lactophenol cotton blue and other colored dyes.
Fungal Culture: The culture on Sabouraud dextrose agar (SDA) medium at room temperature shows a smooth greenish-black colony with a raised and cerebriform center. The reverse side of the colonies is blackish. While performing the culture, it is noteworthy that cycloheximide does not inhibit this fungus.
Histopathology: In histological sections or 10% potassium hydroxide (KOH) mounts, the nodules are observed to be made up of closely packed brown hyphae held in a mass by a viscous or cement-like substance. At the edges of the nodules, regularly aligned hyphae and arthroconidia, 4 to 8 microns in diameter, can be seen. In the thicker parts, club-shaped asci containing elongated ascospores may be formed. A crushed nodule reveals asci containing two to eight single-celled fusiform ascospores with a single polar filament at each end.
Black piedra treatment
Shaving the head of all the hair is the best way to get rid of this fungal infection. However, this option may not be acceptable to females for aesthetic reasons.
Topical antifungal agents in the form of cream or shampoos are effective; 2% ketoconazole or 2% miconazole shampoo applied once a week for three weeks is effective. Non-surfactant based leave-on lotions are also an option. Ciclopirox (0.77%) lotion or 1 to 1.5% shampoo have also been used successfully.
Older treatments include benzoic acid compound ointment or a 1 to 2000 solution of mercury perchloride act as antifungal preparations for application to the hair after shampooing.
Oral antifungals such as terbinafine and itraconazole have been used successfully in cases resistant to topical medications 11. 250 mg of oral terbinafine once daily for 6 weeks was also found to be effective in the treatment of black piedra 12.
Topical keratolytics such as 1% salicylic acid may also be added in cases non-responsive to monotherapy with antifungal shampoos.
Black piedra prognosis
The low spread of infection outside of its endemic habitat and the harmlessness of this disease indicates the good prognosis of this fungal infection. With the right treatment, black piedra has a favorable prognosis- patients recover fully with the restoration of normal hair.
References- Sharma P, Nassereddin A, Sonthalia S. Black Piedra. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545178
- FISCHMAN O. BLACK PIEDRA IN BRAZIL. A CONTRIBUTION TO ITS STUDY IN MANAUS (STATE OF AMAZONAS). Mycopathol Mycol Appl. 1965 Mar 25;25:201-4. doi: 10.1007/BF02049624
- Desai DH, Nadkarni NJ. Piedra: an ethnicity-related trichosis? Int J Dermatol. 2014 Aug;53(8):1008-11.
- Kupiec PM, Green AN, Marks KC. Black adherence nodules on the scalp hair shaft. Cutis. 2017 Jul;100(1):14;38;39.
- Schwartz RA. Superficial fungal infections. Lancet. 2004 Sep 25-Oct 1;364(9440):1173-82. doi: 10.1016/S0140-6736(04)17107-9
- Elewski BE, Hazen PG. The superficial mycoses and the dermatophytes. J Am Acad Dermatol. 1989 Oct;21(4 Pt 1):655-73. doi: 10.1016/s0190-9622(89)70234-6
- Figueras MJ, Guarro J, Zaror L. Ultrastructural aspects of hair digestion in black piedra infection. J Med Vet Mycol. 1997 Jan-Feb;35(1):1-6. doi: 10.1080/02681219780000791
- Figueras MJ, Guarro J. X-ray microanalysis of black piedra. Antonie Van Leeuwenhoek. 1997 Nov;72(4):275-81. doi: 10.1023/a:1000409311166
- Vijay A, Gupta S, Rawat S, Jain SK. A Rare Case of Coinfection with White Piedra and Pediculosis Capitis. Indian Dermatol Online J. 2017 Jul-Aug;8(4):279-280. doi: 10.4103/idoj.IDOJ_353_16
- Lacarrubba F, Verzì AE, Micali G. Trichoscopy in the Differential Diagnosis of Pseudonits. Skin Appendage Disord. 2019;5(3):142-145. doi:10.1159/000493741 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6489062
- Khandpur S, Reddy BS. Itraconazole therapy for white piedra affecting scalp hair. J Am Acad Dermatol. 2002 Sep;47(3):415-8. doi: 10.1067/mjd.2002.124072
- Gip L. Black piedra: the first case treated with terbinafine (Lamisil). Br J Dermatol. 1994 Apr;130 Suppl 43:26-8. doi: 10.1111/j.1365-2133.1994.tb06090.x